Introduction
Congenital central hypoventilation syndrome (CCHS) is characterized by inadequate respiration during sleep and a lack of responsiveness to CO2 and O2. Many autonomic deficits, however, are also present in the syndrome, and both anecdotal and indirect evidence suggests impaired cerebral autoregulation, including syncope and abnormal cerebral blood oxygenation and volume changes to CO2 and O2 challenges [1]. Inadequate cerebral perfusion could contribute to neural injury and functional deficits present in the syndrome [2, 3]. We took advantage of a recent magnetic resonance imaging technique, arterial spin labeling (ASL [4]), to quantify cerebral blood flow (CBF) throughout the brain in a CCHS and an age- and gender-matched control subject.
Image analysis
We assessed overall and regional absolute blood flow in one CCHS and one control 19-year-old female subject with ASL procedures. Subjects provided written, informed consent, and the studies were approved by the Institutional Review Board at UCLA. A total of 400 whole brain (200 ASL labeled, 200 non-labeled), non-invasive (i.e., no contrast) brain volumes were collected while each subject lay in a magnetic resonance imaging scanner over a period of approximately 25 minutes, and CBF maps in ml/100g/min were calculated using ASL labeled and non-labeled volumes with a standard method, resulting in 200 CBF maps per subject [4]. These 200 CBF maps were averaged to derive a mean whole-brain map of CBF levels for each subject; the repeated measures are required to account for the noisy nature of individual CBF measurement. We also collected high-resolution T1-weighted images for background localization. We used SPM software to calculate global CBF (average over whole brain) and to normalize images in order to perform a subtraction for illustrating regional CBF differences. We used MRIcron software to visualize the regional CBF results.
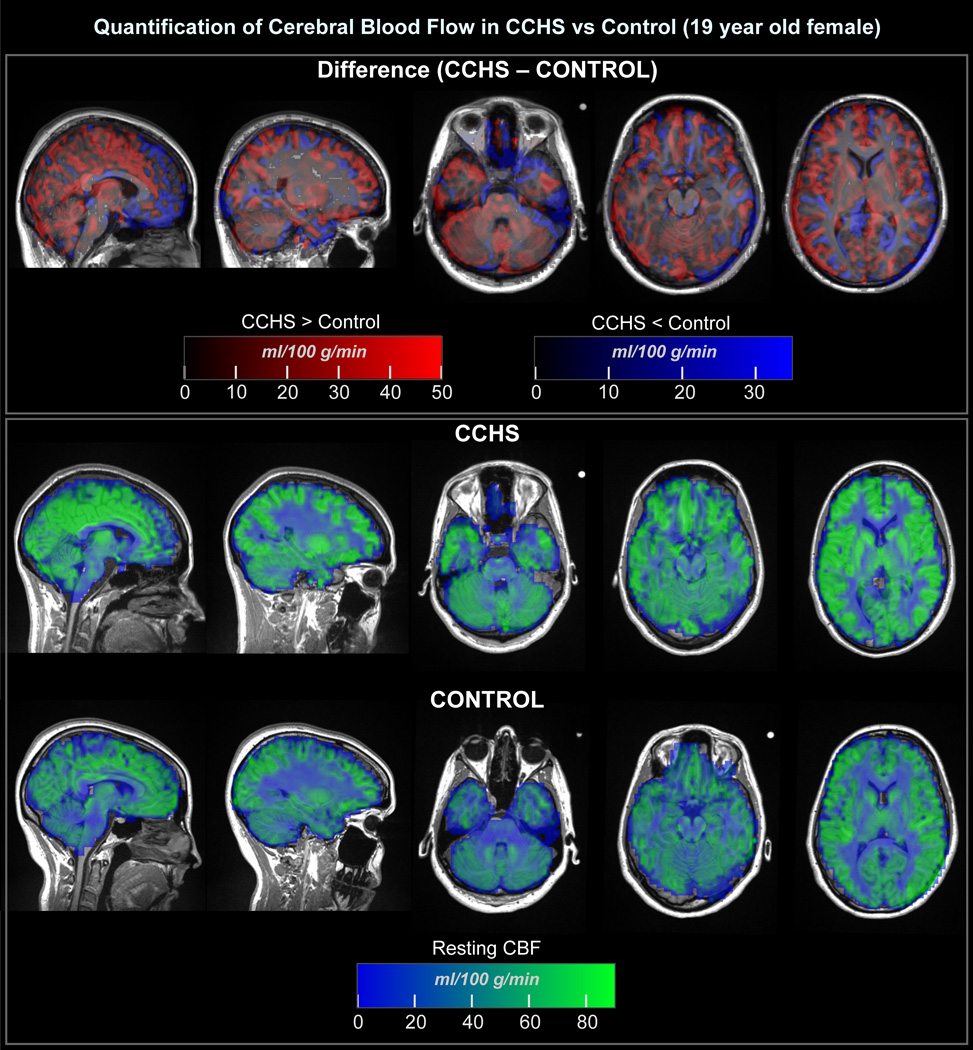
Global baseline blood flow level was higher in CCHS than control (65.8 ± 32.7 vs. 51.3 ± 28.4 ml/100g/min); however, blood flow varied greatly by region (see figure), with the patient showing both increased (red) and decreased (blue) flow over control subject. Notable declines in CCHS appeared in the caudate, bed nucleus of the stria terminalis, ventral medial prefrontal cortex, caudal cerebellum and right temporal cortex. Some of these areas, e.g., ventral medial prefrontal cortex, play significant roles in autonomic regulation.
Figure 1.
Absolute cerebral blood flow in a CCHS patient and age-and gender-matched control subject, as measured using 200 resting-state arterial spin labeling CBF measurements in each subject. Flow quantification is displayed in ml/100g/min according to the color scales, overlaid onto the anatomical background. The CCHS and control patients are in their native space, and the difference images are in normalized space, with the background being the average of the two subjects’ normalized anatomical images.
Discussion
The CCHS patient showed 28% higher overall CBF, but many areas had lower flow than the control subject, suggesting that a combination of processes is operating. The higher overall CBF may relate to high CO2 levels, and the regional variations may reflect previously-demonstrated vascular alterations [5], or impaired autonomic regulation, especially in areas such as the ventral medial prefrontal cortex which plays a major role in blood pressure control. The dramatically altered CBF in the CCHS patient is likely associated with altered tissue perfusion relative to healthy subjects, which may introduce further injury. While this study was performed in a resting condition, it is also possible that the CCHS patient would lack the capacity to respond to autonomic stimuli, such as the orthostatic challenge of standing.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Macey PM, Alger JR, Kumar R, Macey KE, Woo MA, Harper RM. Global BOLD MRI changes to ventilatory challenges in congenital central hypoventilation syndrome. Respir Physiol Neurobiol. 2003 Dec 16;139(1):41–50. doi: 10.1016/j.resp.2003.09.006. [DOI] [PubMed] [Google Scholar]
- 2.Kumar R, Macey PM, Woo MA, Alger JR, Harper RM. Elevated mean diffusivity in widespread brain regions in congenital central hypoventilation syndrome. J Magn Reson Imaging. 2006 Dec;24(6):1252–1258. doi: 10.1002/jmri.20759. [DOI] [PubMed] [Google Scholar]
- 3.Harper RM, Macey PM, Woo MA, Macey KE, Keens TG, Gozal D, et al. Hypercapnic exposure in congenital central hypoventilation syndrome reveals CNS respiratory control mechanisms. J Neurophysiol. 2005 Mar;93(3):1647–1658. doi: 10.1152/jn.00863.2004. [DOI] [PubMed] [Google Scholar]
- 4.Wu WC, Fernandez-Seara M, Detre JA, Wehrli FW, Wang J. A theoretical and experimental investigation of the tagging efficiency of pseudocontinuous arterial spin labeling. Magn Reson Med. 2007 Nov;58(5):1020–1027. doi: 10.1002/mrm.21403. [DOI] [PubMed] [Google Scholar]
- 5.Kumar R, Nguyen HD, Macey PM, Woo MA, Harper RM. Dilated basilar arteries in patients with congenital central hypoventilation syndrome. Neuroscience letters. 2009 Dec 25;467(2):139–143. doi: 10.1016/j.neulet.2009.10.024. [DOI] [PMC free article] [PubMed] [Google Scholar]