Abstract
Corticotropin-releasing factor (CRF) peptides and their receptors have crucial roles in behavioral and endocrine responses to stress. Dysregulation of CRF signaling has been linked to post-traumatic stress disorder, which is associated with increased startle reactivity in response to threat. Thus, understanding the mechanisms underlying CRF regulation of startle may identify pathways involved in this disorder. Here, we tested the hypothesis that both CRF1 and CRF2 receptors contribute to fear-induced increases in startle. Startle responses of wild type (WT) and mice with null mutations (knockout, KO) for CRF1 or CRF2 receptor genes were measured immediately after footshock (shock sensitization) or in the presence of cues previously associated with footshock (ie fear-potentiated startle, FPS). WT mice exhibited robust increases in startle immediately after footshock, which was dependent upon contextual cues. This effect was completely absent in CRF1 KO mice, and significantly attenuated in CRF2 KO mice. In contrast, CRF1 and CRF2 KO mice exhibited normal potentiation of startle by discrete conditioned cues. Blockade of both receptors via CRF1 receptor antagonist treatment in CRF2 KO mice also had no effect on FPS. These results support an additive model of CRF1 and CRF2 receptor activation effects on potentiated startle. These data also indicate that both CRF receptor subtypes contribute to contextual fear but are not required for discrete cued fear effects on startle reactivity. Thus, we suggest that either CRF1 or CRF2 could contribute to the increased startle observed in anxiety disorders with CRF system abnormalities.
Keywords: CRF, startle, conditioned fear, PTSD, fear potentiated startle, context fear
INTRODUCTION
The corticotropin-releasing factor (CRF) family of peptides, including CRF and the urocortins play a critical role in neuroendocrine and behavioral stress responses (for review see Hauger et al, 2006). Some anxiety disorders have been linked to abnormalities in CRF signaling. Post-traumatic stress disorder (PTSD) patients exhibit elevated levels of CRF in cerebrospinal fluid (Sautter et al, 2003; Bremner et al, 1997; Baker et al, 1999). Mutations in the CRF (Smoller et al, 2005) and CRF1 receptor (Keck et al, 2008) genes have been associated with traits predictive for panic disorder and panic disorder diagnoses, respectively. Identifying CRF receptor signaling pathways that subserve anxiety and fear may further our understanding of how CRF pathology could contribute to these disorders.
Corticotropin-releasing factor family peptides activate two known G-protein-coupled receptors, CRF1 and CRF2, which are expressed throughout the mammalian brain (for review see Risbrough and Stein, 2006). CRF1 activation is required for both behavioral and endocrine responses to stress (for review see Hauger et al, 2006), supporting the clinical application of CRF1 antagonists for anxiety and stress-related disorders (Steckler and Dautzenberg, 2006; Zorrilla and Koob, 2004; Holsboer and Ising, 2008). Involvement of CRF2 receptors in stress and anxiety is less clear, and may depend on a number of factors including region of activation, baseline stress level, and type of behavior assessed (see Hauger et al, 2006 and discussion below). CRF receptor activation also modulates fear learning, although again, the specific contribution of CRF2 is less clear. CRF2 activation has been reported to either enhance or attenuate fear learning (Radulovic et al, 1999; Sananbenesi et al, 2003; Todorovic et al, 2007).
The defensive acoustic startle response consists of a series of involuntary reflexes elicited by a sudden, intense auditory or tactile stimulus (Graham, 1975; Yeomans et al, 2002). PTSD and panic disorder subjects exhibit exaggerated startle reactivity (e.g. Butler et al, 1990, Ludewig et al. 2005) predominantly in response to stressful environments or threat (eg oncoming shock, darkness; for review, see Grillon and Baas, 2003), although a direct link between CRF abnormalities and increased startle has not been established. In rodents, exogenous CRF administration increases startle, an effect that can be attenuated by anxiolytic treatment (Swerdlow et al, 1986, 1989). CRF1 is required for exogenous CRF-induced increases in startle, as antagonism or null mutation of CRF1 prevents CRF-induced increases in startle (Risbrough et al, 2003b, 2004). The role of CRF2 in startle is less clear however. CRF2 antagonism attenuates CRF-induced increases in startle; direct CRF2 agonism however has minimal effects (Risbrough et al, 2003b, 2004). We have suggested previously that CRF2 may be additive with CRF1 in mediating CRF-induced potentiation of startle. A critical question remains however, are the functions of CRF1 and CRF2 observed after exogenous CRF treatment reproducible under physiological conditions that better model human anxiety and fear responses?
Contextual and discrete cues associated with an aversive stimulus can elicit exaggerated startle reactivity in humans, a phenomenon that may be exacerbated in PTSD and other anxiety disorders (Grillon and Baas, 2003; Stam, 2007). The enhancing effect of discrete fear cues on startle is termed fear-potentiated startle (FPS) and is found across rodents, primates, and humans (Brown et al, 1951; Winslow et al, 2002; Grillon et al, 1991). Studies examining the role of CRF receptors in FPS have been inconsistent, with CRF receptor antagonist treatment either reducing FPS (Swerdlow et al, 1989; Schulz et al, 1996) or having no effect on FPS (de Jongh et al, 2003). These inconsistencies may be because of a lack of receptor specificity of the pharmacological manipulations. Startle is also exaggerated immediately after footshock in rats and mice, a phenomenon originally termed ‘shock sensitization’ (Davis, 1989; Dirks et al, 2001). In rats, the shock sensitization effect is attributed to contextual fear learning (Richardson, 2000; McNish et al, 1997), and thus ‘sensitization’ may be a misnomer. Humans also exhibit increased startle reactivity after shock (Green-wald et al, 1998) and other stressors (eg social stress, Grillon et al, 2007). In rodents, shock has been shown to induce CRF receptor signaling (Bakshi et al, 2002; Ho et al, 2001; Le et al, 2002; Wang et al, 2005); hence, we reasoned that shock induced increases in startle may be attributable to CRF signaling. Here, we tested the hypothesis that CRF receptors contribute to fear induced increases in startle reactivity. To test our hypothesis, we examined the effect of CRF1 or CRF2 receptor null mutation on startle reactivity under two conditions, either under immediate response to footshock or in response to a discrete cue previously associated with footshock (FPS).
MATERIALS AND METHODS
Subjects
Separate naive cohorts of 2- to 3-month-old male and female CRF1 (Timpl et al, 1998) or CRF2 (Coste et al, 2000) WT and knockout (KO) mice bred in-house by heterozygous mating (backcrossed to C57BL/6J mice for more than 12 generations) were used for each experiment. Male C57BL/6J mice (Jackson Laboratories; 6- to 8-week-old on arrival) were used to test the dependence of shock induced increases in startle on contextual cues. Animals were housed 4 to a cage with food and water provided ad libitum and maintained in a climate-controlled room with a reverse 12-h light/dark cycle (lights on at 1700 hours). Animals were tested during the dark phase between 1000 and 1600 hours. Experiments were conducted in accordance with the ‘Principles of Laboratory Animal Care’ NIH guidelines and with local animal care committee approval.
Apparatus
Startle chambers and footshock apparatus (San Diego Instruments, San Diego, CA) are as described previously (Risbrough et al, 2003a). From startle stimulus onset, 65 consecutive 1 ms readings were recorded to obtain the peak amplitude of the animals’ startle response to acoustic startle stimuli or the average response during the initial 65 ms of the footshock stimuli. Responses to these stimuli are presented in arbitrary units. A light + tone CS was delivered via a bare 5-W incandescent bulb located on the ceiling of the testing chamber (400 lux) and a Sonalert tone generator located at the far wall of the chamber (4 kHz, 70 dB). A 65 dB white-noise background was delivered throughout all sessions. Calibrations of stimuli and response sensitivity were conducted as described elsewhere (Risbrough and Geyer, 2005). Shocks presented outside of the chamber in control experiment 3 were presented in 4 FreezeMonitor chambers (San Diego Instruments). Each acrylic chamber (25 cm wide × 18 cm high × 21 cm deep) was inside a sound-attenuating box. A 15-W house light and small fan in the wall of the sound-attenuating box were on during all sessions. The shock grid floor consisted of 32 stainless steel rods wired to a shock generator for scrambled shock delivery.
Behavioral Testing
Fear-potentiated startle
Mice were tested over 4 consecutive days. On day 1, mice were tested initially with the FPS test session to evaluate any unconditioned effects of the CS on startle before pairing with the US. The session consisted of an initial eight startle pulses without the presence of the cue, four each of 100 and 105 dB 40-ms pulses, with an average ITI of 15 s (range: 7–23 s). This block was used to habituate and stabilize startle responding and was not used in the analysis of FPS. Then eight startle pulses in the presence of the CS and without the CS were presented in a pseudorandom order with an average ITI of 60 s (range: 30–90 s). Half of the startle pulse trials were 100 dB and the other half 105 dB. On days 2 and 3, mice received 10 training trials of CS–US pairings with an average ITI of 180 s (range: 130–230 s). Each training trial consisted of a simultaneous 30 s presentation of the light and tone stimuli (the compound CS), with a 0.4 mA footshock (250 ms) presented immediately at offset of the CS. The FPS test session was then repeated on day 4, 24 h after the last training session.
To test the effects of dual blockade of CRF1 and CRF2 receptors on FPS expression, a second cohort of CRF2 KO mice were trained for FPS using the protocol above. On the pretraining test day, all mice were injected with vehicle to allow for direct comparisons between pretraining and posttraining tests as injection stress may increase unconditioned responses to the CS. On the post-training test day, the selective CRF1 receptor antagonist NBI-30775 (also known as R-121919; a gift from Neurocrine Biosciences Inc., San Diego, CA) or vehicle was administered 30 min before FPS testing (day 4). Mice receiving drug or vehicle were matched for pretraining startle reactivity. NBI-30775 (20 mg/kg) was administered by intraperitoneal (i.p.) injection in a 5 ml/kg volume, using 3% Cremophor/sterile water as the vehicle. This dose and time point was efficacious in blocking exogenous CRF induced increases in startle in mice (Risbrough et al, 2003b, 2004).
Shock-potentiated startle
At least 24h before shock exposure, mice were tested for baseline startle and assigned to Shock and No-Shock groups matched for baseline startle scores. On the test day, mice received a total of five brief startle sessions. After habituation to the startle chamber for 5 min, the first startle session was presented to examine preshock startle reactivity. At 30 s later, mice were presented with a block of five 0.2-mA shocks with an ITI of 60 s (30–90 s range). At 1 min after the last shock, the startle session was presented again. 1 min after the second startle session, a block of five 0.4-mA shocks was presented and followed by the third startle session. At 1 min later, a block of 5–0.8 mA shocks was presented, followed by the fourth startle session. All footshocks were 500 ms in duration.
The startle session consisted of two blocks: the first included nine each of 90, 105, and 120 dB startle pulses (40 ms), given in a pseudorandom order with an average ITI of 15 s (range: 7–23 s). The second block consisted of seven each of 105 and 120 dB pulse alone trials, and five each of four prepulse trials (71 or 75 dB 20 ms prepulse preceding either a 105 or 120 dB 40 ms pulse). The data for this second block (stimuli examining prepulse inhibition) are not presented here because they address different hypotheses. A ‘no stimulus’ trial in which data were recorded without startle stimuli occurred in the middle of each ITI to examine baseline activity.
To aid in interpreting the effects of shock on startle reactivity, we tested if shock induced increases in startle were context dependent. Two matched groups received either shock or no shock in the startle chambers (same-context group) and two matched groups received shock or no shock in fear conditioning chambers in another room (different-context group). All mice were initially tested for startle reactivity using the startle block described above and then immediately removed and placed in holding cages. Mice in the different-context group were then transported to an adjacent room for footshock presentations in fear conditioning chambers, and then immediately returned to the startle chambers for postshock testing. Mice receiving shock in the startle chambers (same context) were kept in holding cages in an adjacent room for 4 min before and after shock presentations to equate handling procedures across context. In both contexts, Shock groups were presented with five 0.4-mA footshocks (500 ms, 30–90 s ITI). No Shock controls underwent the exact same procedures as the shock groups however the shock grids were not activated.
Data Analysis
Fear-potentiated startle
A three-way ANOVA was completed with genotype as a between-subject factor and training (before or after training) and cue (startle trials with and without the presence of the CS) as within-subject factors. Initial analyses with startle intensity as a factor did not reveal any interactions with cue or genotype so this factor was dropped. % FPS was calculated to normalize for differences in startle during the no-cue trials, and analyzed using a two-way ANOVA with genotype as a between-subject factor and training as a within-subject factor (% FPS = ((mean ‘cue’ trial startle magnitude—mean ‘no-cue’ trial startle magnitude)/mean ‘no-cue’ trial startle magnitude) × 100). To assess NBI-30775 effects on FPS in CRF2 WT and KO mice, a three-way ANOVA was completed on % FPS scores with genotype and treatment as between-subject factors and training as a within-subject factor.
Shock-potentiated startle
To examine initial preshock startle baseline across genotype, a three-way ANOVA with gene and shock as between-subject factors and startle intensity (90, 105, 120 dB) as within-subject factors was completed on data collected immediately before footshocks were presented. To assess the effects of the subsequent footshock on startle, a percentage change from preshock baseline scores ((postshock startle block—preshock startle block)/preshock startle block) × 100) was calculated. A four-way ANOVA with genotype and shock as between-subject factors and startle intensity and startle block (after 0.2, 0.4, 0.8 mA) as within-subject factors was completed on the percentage scores, followed by simple ANOVAs as appropriate. To assess context effects on shock induced increases in startle a two-way ANOVA with context exposure (same context vs different context) as a between-subject factor and startle intensity as a within-subject factor was completed.
The ANOVAs reported are collapsed across sex because initial analyses including sex as a factor revealed that, although female mice consistently showed significantly lower startle values than males, sex did not interact with gene, shock, or CS training. Post hoc analyses were completed (significance was considered as α < 0.05) using Tukey’s test or simple ANOVAs as appropriate.
RESULTS
Fear-Potentiated Startle
Experiment 1: fear-potentiated startle in CRF1 WT and KO mice
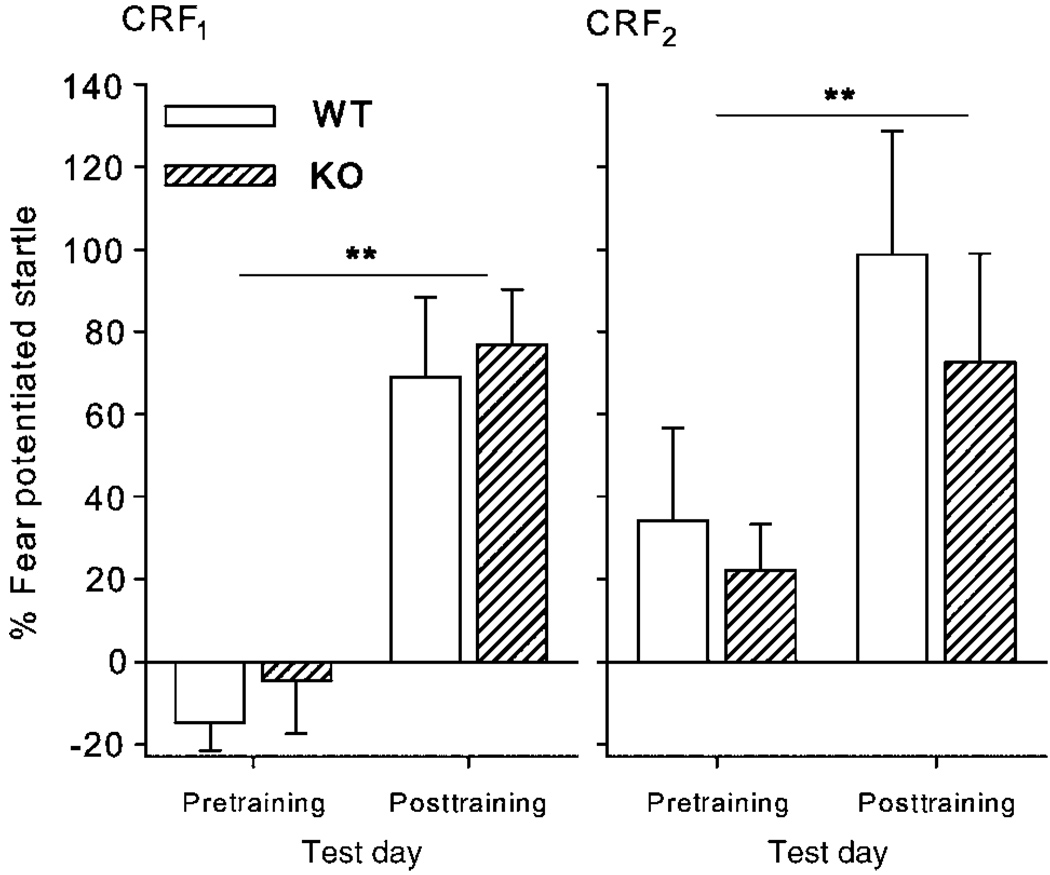
After CS–US paired training, cue trials produced significantly higher startle reactivity compared to no cue trials, as supported by a significant interaction between training (pre vs post-training) and trial type (cue vs no cue) (training × trial type: F(1,20) = 26.2, p < 0.0001; data not shown). Accordingly, % FPS scores were significantly increased after training (Figure 1a, data collapsed across 100 and 105 dB intensities; training: F(1,20) = 33.07, p < 0.0001). There were no significant effects of CRF1 genotype on startle magnitude or % FPS. There was also no significant effect of genotype on average shock reactivity (F(1,20) = 1.2, NS; data not shown).
Figure 1.
Potentiated startle induced by conditioned fear in CRF1 and CRF2 null mutation mice. Mice were tested for startle reactivity with and without the presence of the CS before (pretraining) and after 20 CS–US pairing trials (posttraining). Data are represented as mean ± SEM of % fear-potentiated startle (FPS). N = 8–19, **p<0.01 main effect of training on % FPS.
Experiment 2: fear-potentiated startle in CRF2 WT and KO mice
As in experiment 1, training increased startle reactivity selectively in cue trials (data not shown; training × trial type: F(1,31) = 5.64, p<0.05) and consequently increased % FPS (Figure 1b, data collapsed across 100 and 105 dB intensities; training: F(1,31) = 5.26, p<0.05). CRF2 KO mice exhibited no differences in startle or % FPS compared to WT mice. There was also no significant effect of genotype on average shock reactivity (F(1,32)<1, NS; data not shown).
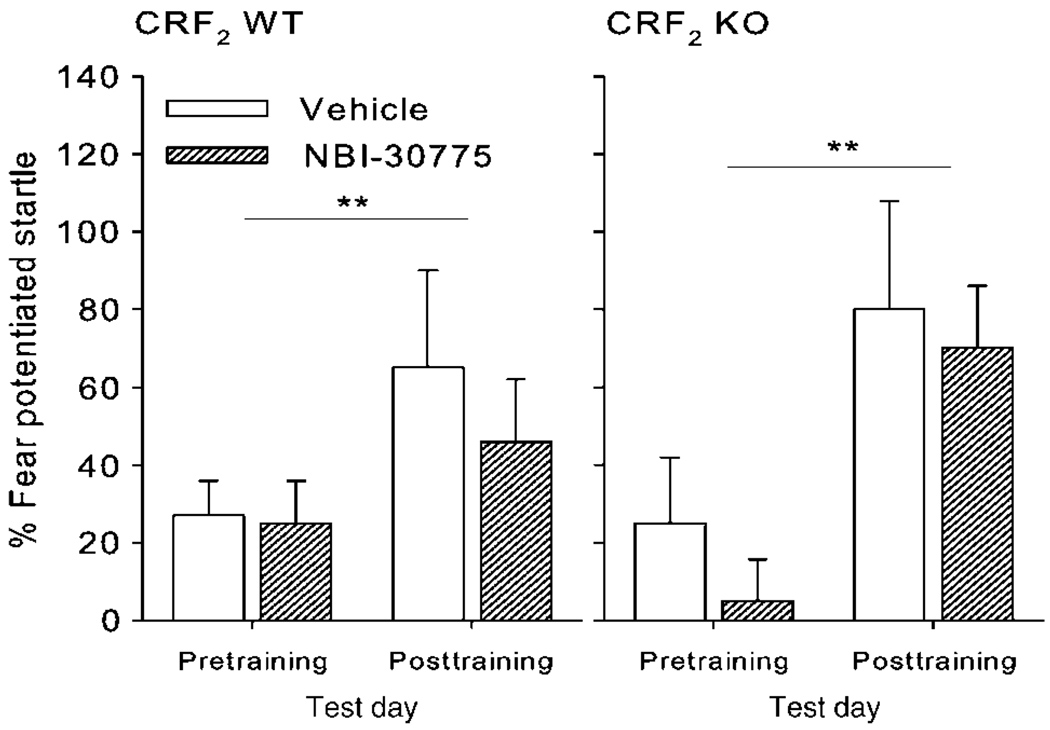
Experiment 3: fear-potentiated startle in CRF2 WT and KO mice with CRF1 receptor antagonist treatment
To test for the possibility that either CRF1 or CRF2 receptors are sufficient for expression of FPS, we treated CRF2 WT and KO mice with the selective CRF1 receptor antagonist NBI-30775 on the post-training test day. NBI-30775 did not significantly alter % FPS in either WT or KO mice (Figure 2; main effect of training: F(1,33) = 10.14, p<0.005, no interactions of training with genotype or drug).
Figure 2.
Effect of pharmacological blockade of CRF1 receptors on potentiated startle induced by conditioned fear in CRF2 null mutation mice. Mice were tested for startle reactivity with and without the presence of the CS before (pretraining) and after 20 CS–US pairing trials (posttraining). NBI-30775 (20 mg/kg, i.p.) or vehicle was administered 30 min before the posttraining test day only. Data are represented as mean ± SEM of % fear-potentiated startle (FPS). N = 7–13, **p<0.01 main effect of training on % FPS.
Shock-Potentiated Startle
Experiment 1: shock-potentiated startle in CRF1 WT and KO mice
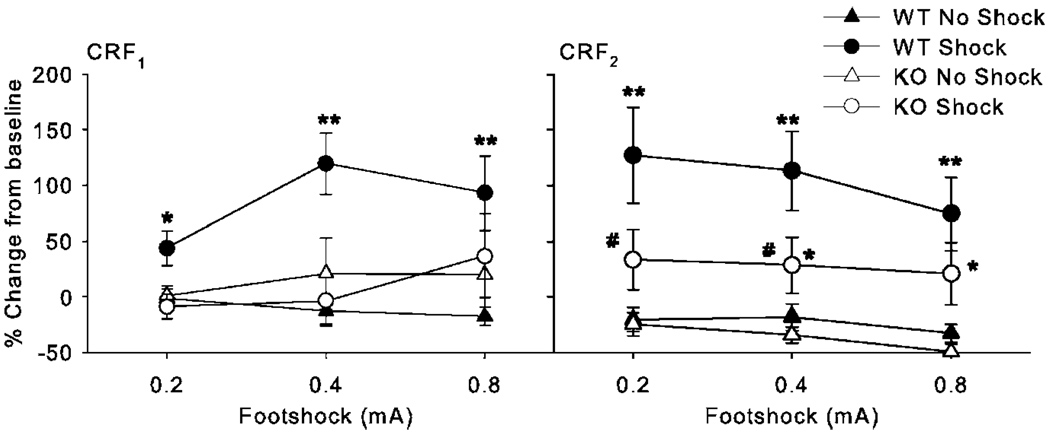
CRF1 WT and KO mice did not differ significantly in preshock baseline startle across the three startle intensities, although KO mice tended to have lower startle magnitude (Table 1; main effect of Genotype: F(1,48) = 3.15, p = 0.08). This preshock baseline was used to calculate a percentage change in startle after footshock to normalize for any small differences in startle reactivity. After shock, significant interactions of genotype with shock and startle intensity were found on % startle potentiation (Intensity × Genotype × Shock: F(2, 96) = 5.11, p<0.01). To dissect the cause of these interactions, we conducted separate analyses for each genotype. As expected, the WT Shock group exhibited shock potentiation compared to the No-Shock group; this effect was most robust at the 90 dB startle intensity, with a peak of 119% increase from preshock baseline at the 0.4 mA block compared to peak increases of 35 and 16% at the 105 and 120 dB startle pulses (Figure 3, left panel; Table 1, Shock × startle intensity: F(2,72) = 8.26, p<0.001). Likely because of ceiling effects at the higher intensities, shock induced increases were most robust at the lowest startle intensity (90 dB), thus data from the 90 dB pulse intensity trials will be presented in figures, percentage change at the 105 and 120 dB pulses are presented in Supplementary Table 1. In CRF1 KO mice however, mice presented with shock showed no differences in startle potentiation compared to the No-Shock group (main effect of shock and interactions F < 1, NS). At the 90 dB intensity, CRF1 KO mice had significantly less shock-potentiated startle than shocked WT mice, independent of shock intensity (Figure 3, left panel; main effect of Genotype: F(1,24) = 4.82, p<0.05). To determine if the lack of potentiation in CRF1 KO mice was because of reduced nociception, we examined jump responses during the shock stimuli. CRF1 WT and KO mice exhibited similar jump responses to the footshock stimuli, with reactivity increasing with increasing current intensities (Table 2; Shock × Intensity: F(2,96) = 3.24, p<0.05; Genotype: F(1,48) < 1, NS).
Table 1.
Baseline Startle Reactivity Immediately Before Footshock Stress
| CRF1 | CRF2 | |||||||
|---|---|---|---|---|---|---|---|---|
| dB | WT no shock | WT shock | KO no shock | KO shock | WT no shock | WT shock | KO no shock | KO shock |
| 90 | 119 ± 22 | 56 ± 13 | 96 ± 11 | 77 ± 12 | 131 ± 28 | 265 ± 61 | 167 ± 34 | 176 ± 44 |
| 105 | 372 ± 57 | 176 ± 28 | 302 ± 36 | 225 ± 69 | 308 ± 58 | 357 ± 52 | 292 ± 63 | 339 ± 73 |
| 120 | 459 ± 62 | 382 ± 118 | 399 ± 41 | 367 ± 117 | 472 ± 66 | 473 ± 64 | 438 ± 86 | 470 ± 87 |
CRF, corticotropin-releasing factor; KO, knock out; WT, wild type.
Measures are mean ± SEM of peak startle magnitude during 90, 105, and 120 dB startle pulses, presented in the startle session immediately before footshock stress.
There was no significant difference between No-Shock and Shock group startle reactivity before footshock stress began. No significant effects of gene were observed; see ‘Results’ for details.
Figure 3.
Potentiated startle induced by footshock in CRF1 and CRF2 null mutation mice. Effects of ascending footshock intensity on startle reactivity were assessed in CRF1 and CRF2 receptor wild-type and knockout mice (WT and KO). Startle reactivity was tested immediately before (preshock baseline) the initial shock block and immediately after each block of footshocks (footshocks were presented in ascending order, 0.2, 0.4, and 0.8 mA, five per block). Half of the animals in each genotype received shock (Shock group) and the other half did not receive shock (No-Shock group). Data are represented as mean ± SEM of % change from initial preshock baseline reactivity to 90 dB startle pulse. N = 7–19, *p<0.05, **p<0.01 vs respective No Shock control, #p<0.05 vs. WT Shock, Tukey’s post hoc test.
Table 2.
Footshock Reactivity in CRF1 and CRF2 WT and KO Mice
| CRF1 | CRF2 | |||
|---|---|---|---|---|
| mA | WT | KO | WT | KO |
| 0.1 | — | — | 111 ± 46 | 130 ± 34 |
| 0.2 | 232 ± 20 | 260 ± 65 | 295 ± 46 | 223 ± 43 |
| 0.4 | 313 ± 23 | 287 ± 21 | 389 ± 52 | 243 ± 52 |
| 0.8 | 263 ± 23 | 326 ± 31 | 344 ± 38 | 254 ± 37 |
CRF, corticotropin-releasing factor; KO, knock out; WT, wild type.
Measures are reported as mean ± SEM of average jump response over the initial 65 ms record window. In experiments 3 and 4, footshocks were varied in intensity (0.2, 0.4, 0.8 mA, 500 ms in duration, given in ascending order). In experiment 5, a separate test using only 0.1 mA (500 ms duration) shock was used in CRF2 KO mice. No significant effects of gene were observed; see ‘Results’ for details.
Experiment 2: shock-potentiated startle in CRF2 WT and KO mice
As seen with CRF1 null mutation, CRF2 null mutation resulted in no significant differences in baseline startle (Table 1; Preshock: Genotype: F(1,45) < 1, NS). As in experiment 1, the shock increased startle reactivity in CRF2 WT mice, with most robust effects at the 90 dB startle intensity (eg at the 0.4mA shock block there was 113, 66, and 32% increase from preshock baseline at the 90, 105, and 120 dB startle intensities, respectively, Intensity × Block × Shock: F(6,270) = 4.31, p<0.001, see Supplementary Table 1 for 105 and 120 dB data). Post hoc analysis at the 90 dB intensity indicated that although both CRF2 WT and KO mice exhibited increases in startle after shock (Figure 3, right panel, p<0.05, Tukey’s post hoc test), the magnitude of the increase in CRF2 KO mice was significantly lower than WT mice (Figure 3, right panel, p<0.05, Tukey’s post hoc test). Because shock effects may cause an inverted U-shaped dose–response curve on startle reactivity (Davis and Astrachan, 1978; Borszcz et al, 1989), a separate experiment using lower shock levels was also conducted to test for the small chance that CRF2 null mutation produced a leftward shift in the inverted shock response curve (ie with lower shock intensities CRF2 null mutation would result in greater shock-potentiated startle). A 0.1 mA footshock intensity produced weak but significant increases in startle (mean ± SEM of % change from baseline at 90 dB: WT/No Shock = −8.3 ± 17.2, KO/No Shock = 16.2 ± 12.8, WT/Shock = 55.3 ± 39.9, KO/Shock = 32.3 ± 20.6) with no interaction with genotype or startle intensity (Shock: F(1,27) = 7.65, p<0.05).
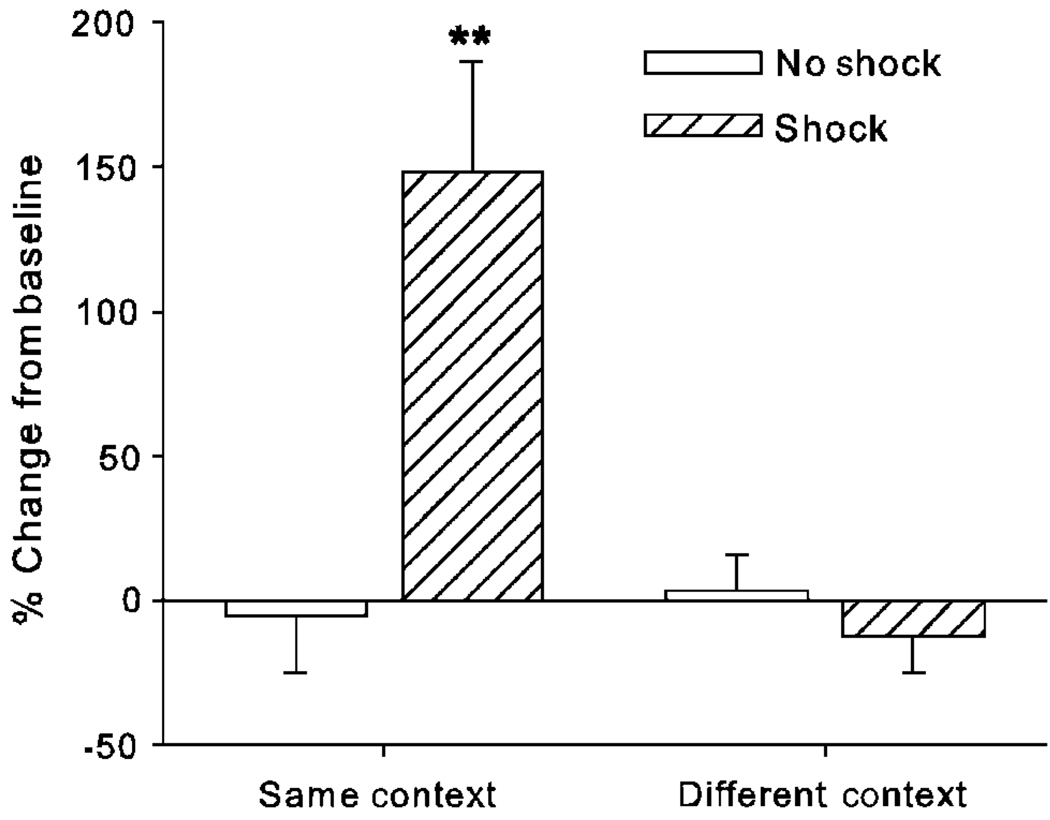
Experiment 3: dependence of shock induced increases in startle reactivity on contextual cues
To test if shock-potentiated startle was because of associative learning to contextual cues, we examined shock-potentiated startle in C57BL6J mice either in the same or different context in which they experienced shock. Unlike mice receiving shock in the startle chambers, mice given similar shock presentations outside of the startle chambers showed no significant increases in startle reactivity compared to No-Shock controls (90 dB pulse shown in Figure 4, 105 and 120 dB data not shown; Context × Shock: F(1,43) = 5.65, p<0.05; Context × Shock × Pulse Intensity: F(2,86) = 9.47, p<0.001).
Figure 4.
Effect of contextual cues on shock-potentiated startle in mice. Mice were initially tested for preshock baseline. Half of the mice were then moved to another room for footshock presentations (different context), whereas half were replaced into the startle chambers for footshock presentations (same context). Half of the mice in each context group received five 0.4-mA shocks (‘Shock’ group) or no footshock (‘No Shock’ group). After shock presentations all mice were replaced into the startle chambers to test postshock reactivity. Data are represented as mean ± SEM of % change from preshock baseline to 90 dB startle pulse. N = 11–12, **p<0.01 vs respective No-Shock control, Tukey’s post hoc test.
DISCUSSION
Here we examined the role of CRF receptors in the potentiation of startle reactivity produced by either discrete or contextual fear cues. Unlike their WT littermates, CRF1 KO mice failed to exhibit shock-potentiated startle. In contrast, CRF2 KO mice exhibited increases in startle after footshock, although these responses were significantly reduced compared to WT mice. Neither CRF1 nor CRF2 KO mice exhibited significant changes in their jump response to footshock or in baseline (preshock) startle reactivity. These results support our hypothesis that CRF1 and CRF2 exert additive influences on startle potentiation. Conversely, both CRF1 and CRF2 KO mice exhibited normal acquisition and expression of FPS. Hence, startle increases elicited by discrete cues do not require either CRF1 or CRF2 signaling. These findings indicate a dissociation between the influences of CRF on context fear learning vs conditioned fear to discrete cues.
In this study, we found that CRF1 and CRF2 KO mice exhibited normal FPS (Figure 1). We also found that blockade of CRF1 receptors in CRF2 KO mice had no significant effects on FPS expression (Figure 2). The dose of NBI-30775 used was found previously to be effective in blocking the effects of exogenous CRF treatment on startle reactivity (Risbrough et al, 2004). These results are consistent with pharmacological studies indicating that non-selective CRF antagonists (de Jongh et al, 2003) and agonists (Risbrough and Geyer, 2005; Walker and Davis, 2002) have no effects on FPS. Others have observed blockade of FPS expression in rats with either α-helical CRF administration (Swerdlow et al, 1989) or the selective CRF1 receptor antagonist CP-154,526 (Schulz et al, 1996). It is not immediately clear what differences could account for these disparate findings, although the previous studies were conducted in rats whereas the present studies are conducted in mice. Swerdlow et al (1989) trained rats with 30 pairing trials per day over 4 days, thus ‘over-training’ the rats in comparison to the present study, resulting in large increases (approximately 200%) in baseline startle. The FPS levels observed in Swerdlow et al (1989) were relatively weak compared to the present study, 21% increase vs 70–100%, respectively, perhaps because of the high baseline startle levels resulting from contextual learning. Schulz et al (1996) had fairly similar training methods as those presented here (20 pairing trials), although the shock level (1.2 mA) was three times stronger than the methods used here. Unfortunately, they did not report % FPS values or startle values, so it is difficult to directly compare our results. It is possible that prolonged training (Swerdlow et al, 1989) or very intense US stimuli (Schulz et al, 1996) result in stronger contextual learning influences on FPS, although these speculations are untested. We report here that context learning is reduced in CRF1 and CRF2 KO mice; hence, paradigms with greater contextual influences may be more sensitive to CRF receptor antagonist effects. We have also observed no effects of CRF1 or CRF2 receptor antagonist treatment on FPS expression in mice (VB Risbrough and MA Geyer, unpublished observations), making it more difficult to claim that compensatory effects alone could account for normal FPS expression in CRF1 and CRF2 KO mice. The present findings are also consistent with a recent report that CRF1 receptor blockade in the amygdala has no effect on conditioned fear as assessed by freezing to discrete cues (Hubbard et al, 2007). Hence, taken together, our data support the hypothesis that neither CRF1 nor CRF2 receptors are required for cued FPS. It should be noted however that these results are not inconsistent with a modulatory role for CRF receptors on fear learning, in particular contextual fear learning (see below). CRF receptor activation before conditioning has been shown previously to influence fear learning, with septal CRF2 receptor activation producing reductions in freezing to conditioned cues (Todorovic et al, 2007). Thus, it is possible that CRF1 or CRF2 null mutation may affect FPS under other protocols, specifically, when animals are stressed or treated with CRF before fear conditioning (Rau et al, 2005; Todorovic et al, 2007; Servatius et al, 2005).
Unlike FPS, mice lacking CRF1 receptors showed a complete absence of shock-potentiated startle (Figure 3). This pattern of results is similar to the total absence of CRF treatment effects on startle reported previously in CRF1 KO mice (Risbrough et al, 2004) or with CRF1 antagonist treatment (Risbrough et al, 2003b). Conversely, CRF2 KO mice exhibited increases in startle after shock; although the magnitude was attenuated significantly compared to WT mice (Figure 3). This overall pattern of effects is similar to findings using pharmacological manipulations. Previously, we showed that CRF2 blockade via the antagonist Antisauvagine-30 attenuated the effects of high doses of rat/human CRF on startle (which activates both CRF1 and CRF2 receptors, but did not reverse the effects of low doses of CRF; Risbrough et al, 2003b), which are more selective for CRF1 receptors. Taken together, our results indicate that shock- or CRF induced increases in startle require CRF2 activation to reach maximal levels (Risbrough et al, 2004). CRF2 activation alone however does not appear to be sufficient to produce robust increases in startle. First, the present data indicate there were no residual increases in startle in shocked CRF1 KO mice. These mice have intact CRF2 receptors that are presumably being activated, as CRF2 KO mice also show altered responses in this task. Second, previous reports indicate that selective CRF2 agonists do not produce robust increases in startle (Risbrough et al, 2003b, 2004). Overall these data are in line with previous results that pharmacological blockade of CRF1 and CRF2 reduces shock-induced freezing (Bakshi et al, 2002). Taken together, these data also support our previous suggestion that startle-increasing effects of CRF2 may require concomitant CRF1 activation (Risbrough et al, 2004). Others have also suggested that anxiogenic effects of CRF2 activation may require concurrent stress (Henry et al, 2006), which presumably activates CRF1 receptors. It is important to note that CRF1 and CRF2 KO mice exhibited normal learning of cue associations with the unconditioned shock stimulus as measured by FPS, indicating that the shock stimulus retained its aversive properties in CRF1 and CRF2 KO mice.
As in rats, we found that shock induced increases in startle reactivity were dependent on the contextual cues, as mice tested immediately after footshock in a different context showed no significant increases in startle reactivity (Figure 4; Richardson, 2000). Because CRF1 and CRF2 null mutation modifies responses in this paradigm, it appears that activation of CRF1 and CRF2 receptors contributes to immediate context fear effects on startle reactivity, although the regions mediating these effects are unknown. Studies in rats suggest that the amygdala plays a permissive role in shock-potentiated startle; hence, the amygdala may be an important modulatory site of action for CRF receptor effects on this behavior as well (Van Nobelen and Kokkinidis, 2006; Sananes and Davis, 1992). Previous reports using freezing behavior support a modulatory role for CRF1 and CRF2 receptors in contextual fear learning when tested at longer time points after training. Stress or CRF-induced activation of hippocampal CRF1 receptors enhances fear learning (Radulovic et al, 1999; Todorovic et al, 2007) whereas amygdala CRF1 receptor activation contributes to long-term consolidation of fear learning (Roozendaal et al, 2002; Hubbard et al, 2007). Hippocampal injections of a CRF2 antagonist block stressed induced increases in contextual fear learning (Sananbenesi et al, 2003). These CRF2 effects were linked to secondary messenger signaling however, which is unlikely to be functioning in the immediate context fear produced by the shock stress. Shock-potentiated startle does not appear to require NMDA receptor activation or protein synthesis, necessary components for long-term (eg 24h) fear memory storage (Van Nobelen and Kokkinidis, 2006). Hence, only tentative comparisons can be made between studies using context-conditioned freezing and startle, as these measures may be probing differential short-and long-term conditioned fear processes, as well as differential neural substrates (eg McNish et al, 1997).
Previous reports have shown consistently that the inactivation of CRF2 receptors in the septum and the raphe produces anxiety-like effects in rodents (Bakshi et al, 2007; Henry et al, 2006; Hammack et al, 2003). Whole-brain inactivation is less consistent however, with pharmacological blockade inducing both anxiolytic (present data Pelleymounter et al, 2002; Takahashi et al, 2001) and anxiogenic-like effects (Kishimoto et al, 2000). Genetic null mutation has been reported to produce no effect or anxiolytic effects (Kishimoto et al, 2000; Bale et al, 2000; Coste et al, 2000) in approach-avoidance tests, and reductions in stress coping behavior, such as increased hypophagia in response to stress and increased immobility in the forced swim test (Coste et al, 2006; Bale and Vale, 2004). The present results are the first to our knowledge to show an anxiolytic-like effect of CRF2 null mutation, thus being more consistent with septal or raphe CRF2 receptor inactivation studies. This interpretation should be made cautiously however, as it is also possible that CRF2 receptor activation mediates the aversive quality of the US (Sahuque et al, 2006) or could disrupt immediate fear learning. Evidence arguing against the latter interpretation is that cued fear learning was not affected by CRF2 gene deletion, which would be expected to be altered if CRF2 activation contributes to the aversive quality of the US. Future studies examining the contribution of CRF2 to other forms of immediate learning are required to fully resolve whether CRF2 is blocking cognition or defensive responding per se. CRF2 receptor blockade also attenuates unconditioned increases in startle reactivity after CRF administration however, thus this contribution of CRF2 effects on startle is observed in both conditioned and unconditioned potentiated startle models. In contrast to rodent approach-avoidance measures of anxiety (eg open field, plus maze, forced swim), defensive startle measures are not confounded by alterations in locomotor activity (Davis, 1990). CRF2 ligands have robust effects on locomotor activity and grooming behavior (Todorovic et al, 2007; Valdez et al, 2003; Bakshi et al, 2007; Zhao et al, 2007), which may account for some inconsistent findings in models that are influenced by activity levels (eg grooming behaviors may compete with approach-avoidance behaviors). Unlike other lines of CRF2 KO mice, this line exhibits normal approach-avoidance behavior (eg elevated plus maze or open field) and normal CRF expression (Bale et al, 2000; Bale and Vale, 2004; Coste et al, 2000). It has been suggested that the anxiety-like phenotype exhibited by other lines of CRF2 KO mice may be in part because of an increased CRF expression in the amygdala (Bale and Vale, 2004). Nevertheless, this explanation seems unlikely to account for the present results, because increased CRF release would be expected to increase rather than decrease startle reactivity, as observed here.
Conclusions
The present data indicate that FPS to contextual cues requires CRF1 activation, and also require CRF2 activation to achieve maximal effects. Conversely, conditioned cue effects on startle using the same US (shock) do not require CRF1 or CRF2 signaling. These results suggest that CRF2 blockade can attenuate immediate context learning effects on startle, but without altering effects of discrete conditioned cues. Although there is still continued controversy over the role of CRF2 in anxiety, the present results provide more evidence that CRF2 receptor activation can mediate increases in certain defensive behaviors.
The shock-potentiated startle task may be particularly relevant to clinical studies of startle reactivity, as human tests of potentiated startle are most commonly conducted over one session and assess immediate responses to threatening or painful stimuli, not long-term learned responses (eg 24 h in-between training and testing; Grillon, 2008). The findings that CRF receptors play a role in contextual FPS may also have relevance to PTSD. Exaggerated startle responses in PTSD subjects are most commonly observed in the laboratory in paradigms using stress or threat manipulations (for review see Grillon and Baas, 2003), and CRF abnormalities have been linked to PTSD (Baker et al, 1999; Bremner et al, 1997; Sautter et al, 2003; for review see Risbrough and Stein, 2006). Although no direct link between CRF pathology and startle abnormalities has been established, our results indicate that excessive CRF1 or CRF2 signaling could contribute to the exaggerated startle reactivity observed in PTSD. These studies support future examination of CRF receptor antagonists in clinical studies of context fear effects on potentiated startle.
ACKNOWLEDGEMENTS
We thank Dr Susan Powell for her helpful comments, Christine Scott and Chelsea Wallace for their technical assistance, and Dr Dimitri Grigoriadis of Neurocrine Biosciences for the gift of NBI-30775. This work was supported by NIH grant MH074697; the San Diego Veteran’s Administration Center of Excellence for Stress and Mental Health (CESAMH), and via a Merit Review grant from the Department of Veterans Affairs. These data were previously presented at the 2007 Biological Psychiatry meeting in San Diego, CA.
Footnotes
DISCLOSURE/CONFLICT OF INTEREST
Drs Hauger, Coste, Stenzel-Poore, Wurst and Holsboer have no potential financial conflicts to report. Over the past 3 years, Dr Geyer has received compensation from Acadia, Addex, Amgen, AstraZeneca, Jazz, Omeros, Organon and Wyeth-Ayerst and holds an equity interest in San Diego Instruments. Over the past 3 years Dr Risbrough has received compensation as a consultant from Arena Pharmaceuticals and San Diego Instruments.
Supplementary Information accompanies the paper on the Neuropsychopharmacology website (http://www.nature.com/npp)
REFERENCES
- Baker DG, West SA, Nicholson WE, Ekhator NN, Kasckow JW, Hill KK, et al. Serial CSF corticotropin-releasing hormone levels and adrenocortical activity in combat veterans with posttraumatic stress disorder. Am J Psychiatry. 1999;156:585–588. doi: 10.1176/ajp.156.4.585. [DOI] [PubMed] [Google Scholar]
- Bakshi VP, Newman SM, Smith-Roe S, Jochman KA, Kalin NH. Stimulation of lateral septum CRF2 receptors promotes anorexia and stress-like behaviors: functional homology to CRF1 receptors in basolateral amygdala. J Neurosci. 2007;27:10568–10577. doi: 10.1523/JNEUROSCI.3044-06.2007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bakshi VP, Smith-Roe S, Newman SM, Grigoriadis DE, Kalin NH. Reduction of stress-induced behavior by antagonism of corticotropin-releasing hormone 2 (CRH2) receptors in lateral septum or CRH1 receptors in amygdala. J Neurosci. 2002;22:2926–2935. doi: 10.1523/JNEUROSCI.22-07-02926.2002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bale TL, Contarino A, Smith GW, Chan R, Gold LH, Sawchenko PE, et al. Mice deficient for corticotropin-releasing hormone receptor-2 display anxiety-like behaviour and are hypersensitive to stress. Nat Genet. 2000;24:410–414. doi: 10.1038/74263. [DOI] [PubMed] [Google Scholar]
- Bale TL, Vale WW. CRF and CRF receptors: role in stress responsivity and other behaviors. Annu Rev Pharmacol Toxicol. 2004;44:525–557. doi: 10.1146/annurev.pharmtox.44.101802.121410. [DOI] [PubMed] [Google Scholar]
- Borszcz GS, Cranney J, Leaton RN. Influence of long-term sensitization on long-term habituation of the acoustic startle response in rats: central gray lesions, preexposure, and extinction. J Exp Psychol Anim Behav Process. 1989;15:54–64. [PubMed] [Google Scholar]
- Bremner JD, Licinio J, Darnell A, Krystal JH, Owens MJ, Southwick SM, et al. Elevated CSF corticotropin-releasing factor concentrations in posttraumatic stress disorder. Am J Psychiatry. 1997;154:624–629. doi: 10.1176/ajp.154.5.624. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brown JS, Kalish HI, Farber IE. Conditioned fear as revealed by magnitude of startle response to an auditory stimulus. J Exp Psychol. 1951;41:317–328. doi: 10.1037/h0060166. [DOI] [PubMed] [Google Scholar]
- Butler RW, Braff DL, Rausch JL, Jenkins MA, Sprock J, Geyer MA. Physiological evidence of exaggerated startle response in a subgroup of Vietnam veterans with combat-related PTSD. Am J Psychiatry. 1990;147:1308–1312. doi: 10.1176/ajp.147.10.1308. [DOI] [PubMed] [Google Scholar]
- Coste SC, Heard AD, Phillips TJ, Stenzel-Poore MP. Corticotropin-releasing factor receptor type 2-deficient mice display impaired coping behaviors during stress. Genes Brain Behav. 2006;5:131–138. doi: 10.1111/j.1601-183X.2005.00142.x. [DOI] [PubMed] [Google Scholar]
- Coste SC, Kesterson RA, Heldwein KA, Stevens SL, Heard AD, Hollis JH, et al. Abnormal adaptations to stress and impaired cardiovascular function in mice lacking corticotropin-releasing hormone receptor-2. Nat Genet. 2000;24:403–409. doi: 10.1038/74255. [DOI] [PubMed] [Google Scholar]
- Davis M. Sensitization of the acoustic startle reflex by footshock. Behav Neurosci. 1989;103:495–503. [PubMed] [Google Scholar]
- Davis M. Animal models of anxiety based on classical conditioning: the conditioned emotional response (CER) and the fear-potentiated startle effect. Pharmacol Ther. 1990;47:147–165. doi: 10.1016/0163-7258(90)90084-f. [DOI] [PubMed] [Google Scholar]
- Davis M, Astrachan DI. Conditioned fear and startle magnitude: effects of different footshock or backshock intensities used in training. J Exp Psychol Anim Behav Process. 1978;4:95–103. doi: 10.1037//0097-7403.4.2.95. [DOI] [PubMed] [Google Scholar]
- de Jongh R, Groenink L, van der Gugten J, Olivier B. Light-enhanced and fear-potentiated startle: temporal characteristics and effects of alphα-helical corticotropin-releasing hormone. Biol Psychiatry. 2003;54:1041–1048. doi: 10.1016/s0006-3223(03)00468-2. [DOI] [PubMed] [Google Scholar]
- Dirks A, Pattij T, Bouwknecht JA, Westphal TT, Hijzen TH, Groenink L, et al. 5-HT1B receptor knockout, but not 5-HT1A receptor knockout mice, show reduced startle reactivity and footshock-induced sensitization, as measured with the acoustic startle response. Behav Brain Res. 2001;118:169–178. doi: 10.1016/s0166-4328(00)00326-0. [DOI] [PubMed] [Google Scholar]
- Graham FK. Presidential Address, 1974. The more or less startling effects of weak prestimulation. Psychophysiology. 1975;12:238–248. doi: 10.1111/j.1469-8986.1975.tb01284.x. [DOI] [PubMed] [Google Scholar]
- Greenwald MK, Bradley MM, Cuthbert BN, Lang PJ. Startle potentiation: shock sensitization, aversive learning, and affective picture modulation. Behav Neurosci. 1998;112:1069–1079. doi: 10.1037//0735-7044.112.5.1069. [DOI] [PubMed] [Google Scholar]
- Grillon C. Models and mechanisms of anxiety: evidence from startle studies. Psychopharmacology. 2008;199:421. doi: 10.1007/s00213-007-1019-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grillon C, Ameli R, Woods SW, Merikangas K, Davis M. Fear-potentiated startle in humans: effects of anticipatory anxiety on the acoustic blink reflex. Psychophysiology. 1991;28:588–595. doi: 10.1111/j.1469-8986.1991.tb01999.x. [DOI] [PubMed] [Google Scholar]
- Grillon C, Baas J. A review of the modulation of the startle reflex by affective states and its application in psychiatry. Clin Neurophysiol. 2003;114:1557–1579. doi: 10.1016/s1388-2457(03)00202-5. [DOI] [PubMed] [Google Scholar]
- Grillon C, Duncko R, Covington MF, Kopperman L, Kling MA. Acute stress potentiates anxiety in humans. Biol Psychiatry. 2007;62:1183. doi: 10.1016/j.biopsych.2007.06.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hammack SE, Schmid MJ, LoPresti ML, Der-Avakian A, Pellymounter MA, Foster AC, et al. Corticotropin releasing hormone type 2 receptors in the dorsal raphe nucleus mediate the behavioral consequences of uncontrollable stress. J Neurosci. 2003;23:1019–1025. doi: 10.1523/JNEUROSCI.23-03-01019.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hauger RL, Risbrough V, Brauns O, Dautzenberg FM. Corticotropin releasing factor (CRF) receptor signaling in the central nervous system: new molecular targets. CNS Neurol Disord Drug Targets. 2006;5:453–479. doi: 10.2174/187152706777950684. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Henry B, Vale W, Markou A. The effect of lateral septum corticotropin-releasing factor receptor 2 activation on anxiety is modulated by stress. J Neurosci. 2006;26:9142–9152. doi: 10.1523/JNEUROSCI.1494-06.2006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ho SP, Takahashi LK, Livanov V, Spencer K, Lesher T, Maciag C, et al. Attenuation of fear conditioning by antisense inhibition of brain corticotropin releasing factor-2 receptor. Brain Res Mol Brain Res. 2001;89:29–40. doi: 10.1016/s0169-328x(01)00050-x. [DOI] [PubMed] [Google Scholar]
- Holsboer F, Ising M. Central CRH system in depression and anxiety—evidence from clinical studies with CRH1 receptor antagonists. Eur J Pharmacol. 2008;583:350. doi: 10.1016/j.ejphar.2007.12.032. [DOI] [PubMed] [Google Scholar]
- Hubbard DT, Nakashima BR, Lee I, Takahashi LK. Activation of basolateral amygdala corticotropin-releasing factor 1 receptors modulates the consolidation of contextual fear. Neuroscience. 2007;150:818. doi: 10.1016/j.neuroscience.2007.10.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Keck ME, Kern N, Erhardt A, Unschuld PG, Ising M, Salyakina D, et al. Combined effects of exonic polymorphisms in CRHR1 and AVPR1B genes in a case/control study for panic disorder. Am J Med Genet B Neuropsychiatr Genet. 2008;147B:1196–1204. doi: 10.1002/ajmg.b.30750. [DOI] [PubMed] [Google Scholar]
- Kishimoto T, Radulovic J, Radulovic M, Lin CR, Schrick C, Hooshmand F, et al. Deletion of Crhr2 reveals an anxiolytic role for corticotropin-releasing hormone receptor-2. Nat Genet. 2000;24:415–419. doi: 10.1038/74271. [DOI] [PubMed] [Google Scholar]
- Le AD, Harding S, Juzytsch W, Fletcher PJ, Shaham Y. The role of corticotropin-releasing factor in the median raphe nucleus in relapse to alcohol. J Neurosci. 2002;22:7844–7849. doi: 10.1523/JNEUROSCI.22-18-07844.2002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ludewig S, Geyer MA, Ramseier M, Vollenweider FX, Rechsteiner E, Cattapan-Ludewig K. Information-processing deficits and cognitive dysfunction in panic disorder. J Psychiatry Neurosci. 2005;30:37–43. [PMC free article] [PubMed] [Google Scholar]
- McNish KA, Gewirtz JC, Davis M. Evidence of contextual fear after lesions of the hippocampus: a disruption of freezing but not fear-potentiated startle. J Neurosci. 1997;17:9353–9360. doi: 10.1523/JNEUROSCI.17-23-09353.1997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pelleymounter MA, Joppa M, Ling N, Foster AC. Pharmacological evidence supporting a role for central corticotropin-releasing factor(2) receptors in behavioral, but not endocrine, response to environmental stress. J Pharmacol Exp Ther. 2002;302:145–152. doi: 10.1124/jpet.302.1.145. [DOI] [PubMed] [Google Scholar]
- Radulovic J, Ruhmann A, Liepold T, Spiess J. Modulation of learning and anxiety by corticotropin-releasing factor (CRF) and stress: differential roles of CRF receptors 1 and 2. J Neurosci. 1999;19:5016–5025. doi: 10.1523/JNEUROSCI.19-12-05016.1999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rau V, DeCola JP, Fanselow MS. Stress-induced enhancement of fear learning: an animal model of posttraumatic stress disorder. Neurosci Biobehav Rev. 2005;29:1207–1223. doi: 10.1016/j.neubiorev.2005.04.010. [DOI] [PubMed] [Google Scholar]
- Richardson R. Shoc sensitization of startle: learned or unlearned fear? Behav Brain Res. 2000;110:109–117. doi: 10.1016/s0166-4328(99)00189-8. [DOI] [PubMed] [Google Scholar]
- Risbrough VB, Brodkin JD, Geyer MA. GABA-A and 5-HT1A receptor agonists block expression of fear-potentiated startle in mice. Neuropsychopharmacology. 2003a;28:654–663. doi: 10.1038/sj.npp.1300079. [DOI] [PubMed] [Google Scholar]
- Risbrough VB, Geyer MA. Anxiogenic treatments do not increase fear-potentiated startle in mice. Biol Psychiatry. 2005;57:33–43. doi: 10.1016/j.biopsych.2004.10.006. [DOI] [PubMed] [Google Scholar]
- Risbrough VB, Hauger RL, Pelleymounter MA, Geyer MA. Role of corticotropin releasing factor (CRF) receptors 1 and 2 in CRF-potentiated acoustic startle in mice. Psychopharmacology (Berl) 2003b;170:178–187. doi: 10.1007/s00213-003-1535-6. [DOI] [PubMed] [Google Scholar]
- Risbrough VB, Hauger RL, Roberts AL, Vale WW, Geyer MA. Corticotropin-releasing factor receptors CRF1 and CRF2 exert both additive and opposing influences on defensive startle behavior. J Neurosci. 2004;24:6545–6552. doi: 10.1523/JNEUROSCI.5760-03.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Risbrough VB, Stein MB. Role of corticotropin releasing factor in anxiety disorders: a translational research perspective. Horm Behav. 2006;50:550–561. doi: 10.1016/j.yhbeh.2006.06.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Roozendaal B, Brunson KL, Holloway BL, McGaugh JL, Baram TZ. Involvement of stress-released corticotropin-releasing hormone in the basolateral amygdala in regulating memory consolidation. Proc Natl Acad Sci USA. 2002;99:13908–13913. doi: 10.1073/pnas.212504599. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sahuque L, Kullberg E, McGeehan A, Kinder J, Hicks M, Blanton M, et al. Anxiogenic and aversive effects of corticotropin-releasing factor (CRF) in the bed nucleus of the stria terminalis in the rat: role of CRF receptor subtypes. Psychopharmacology. 2006;186:122–132. doi: 10.1007/s00213-006-0362-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sananbenesi F, Fischer A, Schrick C, Spiess J, Radulovic J. Mitogen-activated protein kinase signaling in the hippocampus and its modulation by corticotropin-releasing factor receptor 2: a possible link between stress and fear memory. J Neurosci. 2003;23:11436–11443. doi: 10.1523/JNEUROSCI.23-36-11436.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sananes CB, Davis M. N-methyl-d-aspartate lesions of the lateral and basolateral nuclei of the amygdala block fear-potentiated startle and shock sensitization of startle. Behav Neurosci. 1992;106:72–80. doi: 10.1037//0735-7044.106.1.72. [DOI] [PubMed] [Google Scholar]
- Sautter FJ, Bissette G, Wiley J, Manguno-Mire G, Schoenbachler B, Myers L, et al. Corticotropin-releasing factor in posttrau-matic stress disorder (PTSD) with secondary psychotic symptoms, nonpsychotic PTSD, and healthy control subjects. Biol Psychiatry. 2003;54:1382–1388. doi: 10.1016/s0006-3223(03)00571-7. [DOI] [PubMed] [Google Scholar]
- Schulz DW, Mansbach RS, Sprouse J, Braselton JP, Collins J, Corman M, et al. CP-154,526: a potent and selective nonpeptide antagonist of corticotropin releasing factor receptors. Proc Natl Acad Sci USA. 1996;93:10477–10482. doi: 10.1073/pnas.93.19.10477. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Servatius RJ, Beck KD, Moldow RL, Salameh G, Tumminello TP, Short KR. A stress-induced anxious state in male rats: corticotropin-releasing hormone induces persistent changes in associative learning and startle reactivity. Biol Psychiatry. 2005;57:865–872. doi: 10.1016/j.biopsych.2005.01.015. [DOI] [PubMed] [Google Scholar]
- Smoller JW, Yamaki LH, Fagerness JA, Biederman J, Racette S, Laird NM, et al. The corticotropin-releasing hormone gene and behavioral inhibition in children at risk for panic disorder. Biol Psychiatry. 2005;57:1485–1492. doi: 10.1016/j.biopsych.2005.02.018. [DOI] [PubMed] [Google Scholar]
- Stam R. PTSD and stress sensitisation: a tale of brain and body Part 1: human studies. Neurosci Biobehav Rev. 2007;31:530–557. doi: 10.1016/j.neubiorev.2006.11.010. [DOI] [PubMed] [Google Scholar]
- Steckler T, Dautzenberg FM. Corticotropin-releasing factor receptor antagonists in affective disorders and drug dependence—an update. CNS Neurol Disord Drug Targets. 2006;5:147–165. doi: 10.2174/187152706776359619. [DOI] [PubMed] [Google Scholar]
- Swerdlow NR, Britton KT, Koob GF. Potentiation of acoustic startle by corticotropin-releasing factor (CRF) and by fear are both reversed by alphα-helical CRF (9–41) Neuropsychopharmacology. 1989;2:285–292. doi: 10.1016/0893-133x(89)90033-x. [DOI] [PubMed] [Google Scholar]
- Swerdlow NR, Geyer MA, Vale WW, Koob GF. Corticotropin-releasing factor potentiates acoustic startle in rats: blockade by chlordiazepoxide. Psychopharmacology (Berl) 1986;88:147–152. doi: 10.1007/BF00652231. [DOI] [PubMed] [Google Scholar]
- Takahashi LK, Ho SP, Livanov V, Graciani N, Arneric SP. Antagonism of CRF(2) receptors produces anxiolytic behavior in animal models of anxiety. Brain Res. 2001;902:135–142. doi: 10.1016/s0006-8993(01)02405-2. [DOI] [PubMed] [Google Scholar]
- Timpl P, Spanagel R, Sillaber I, Kresse A, Reul JM, Stalla GK, et al. Impaired stress response and reduced anxiety in mice lacking a functional corticotropin-releasing hormone receptor 1. Nat Genet. 1998;19:162–166. doi: 10.1038/520. [DOI] [PubMed] [Google Scholar]
- Todorovic C, Radulovic J, Jahn O, Radulovic M, Sherrin T, Hippel C, et al. Differential activation of CRF receptor subtypes removes stress-induced memory deficit and anxiety. Eur J Neurosci. 2007;25:3385–3397. doi: 10.1111/j.1460-9568.2007.05592.x. [DOI] [PubMed] [Google Scholar]
- Valdez GR, Zorrilla EP, Rivier J, Vale WW, Koob GF. Locomotor suppressive and anxiolytic-like effects of urocortin 3, a highly selective type 2 corticotropin-releasing factor agonist. Brain Res. 2003;980:206–212. doi: 10.1016/s0006-8993(03)02971-8. [DOI] [PubMed] [Google Scholar]
- Van Nobelen M, Kokkinidis L. Amygdaloid GABA, not glutamate neurotransmission or mRNA transcription controls footshock-associated fear arousal in the acoustic startle paradigm. Neuroscience. 2006;137:707. doi: 10.1016/j.neuroscience.2005.08.061. [DOI] [PubMed] [Google Scholar]
- Walker DL, Davis M. Light-enhanced startle: further pharmacological and behavioral characterization. Psychopharmacology (Berl) 2002;159:304–310. doi: 10.1007/s002130100913. [DOI] [PubMed] [Google Scholar]
- Wang J, Fang Q, Liu Z, Lu L. Region-specific effects of brain corticotropin-releasing factor receptor type 1 blockade on footshock-stress- or drug-priming-induced reinstatement of morphine conditioned place preference in rats. Psychopharmacology. 2005;185:19–28. doi: 10.1007/s00213-005-0262-6. [DOI] [PubMed] [Google Scholar]
- Winslow JT, Parr LA, Davis M. Acoustic startle, prepulse inhibition, and fear-potentiated startle measured in rhesus monkeys. Biol Psychiatry. 2002;51:859–866. doi: 10.1016/s0006-3223(02)01345-8. [DOI] [PubMed] [Google Scholar]
- Yeomans JS, Li L, Scott BW, Frankland PW. Tactile, acoustic and vestibular systems sum to elicit the startle reflex. Neurosci Biobehav Rev. 2002;26:1–11. doi: 10.1016/s0149-7634(01)00057-4. [DOI] [PubMed] [Google Scholar]
- Zhao Y, Valdez GR, Fekete EM, Rivier JE, Vale WW, Rice KC, et al. Subtype-selective corticotropin-releasing factor receptor agonists exert contrasting, but not opposite, effects on anxiety-related behavior in rats. J Pharmacol Exp Ther. 2007;323:846–854. doi: 10.1124/jpet.107.123208. [DOI] [PubMed] [Google Scholar]
- Zorrilla EP, Koob GF. The therapeutic potential of CRF1 antagonists for anxiety. Expert Opin Investig Drugs. 2004;13:799–828. doi: 10.1517/13543784.13.7.799. [DOI] [PubMed] [Google Scholar]