Abstract
Investigator-initiated research in both asthma and chronic obstructive pulmonary disease conducted at the Baylor Martha Foster Lung Care Center has sought to improve management throughout the continuum of respiratory care using a multidisciplinary approach. Respiratory care therapists employed in the primary care setting were shown to improve the quality of asthma care: rescue inhaler use decreased by 75% and respiratory symptom score decreased by 49% in patients who were seen by this midlevel specialty provider. In addition to similar results in a geriatric population, patients' diagnosis was changed in 48% of cases and treatment was changed in 76% of cases after the intervention. For pulmonary rehabilitation, an activity of daily living assessment form was created, and rehabilitation—whether traditional or water-based—was shown to improve patients' ability to perform activities of daily living and improve quality of life scores. The Rules of Two®, developed by Baylor University Medical Center at Dallas to simplify understanding of good asthma control, continues to be taught, and patient education has also been offered through asthma summer camps for children. Finally, a multidisciplinary team worked to develop a protocol for treatment of asthma patients in the emergency department and, through this effort, was able to reduce length of stay from an average of 278 minutes to an average of 168 minutes. These efforts aim to overcome the gap between recommended care and actual practice, so that patients benefit from evidence-based medicine and continuing refinements to diagnosis and treatment.
It has long been recognized that in America's fragmented health care system, chronic diseases could be much better managed. These issues are being discussed by health care professionals and policymakers alike in the context of the health care reform debate. As one example, the Partnership to Fight Chronic Diseases has described some “unhealthy truths” about chronic disease:
Chronic diseases are the number one cause of death and disability in the US.
Treating patients with chronic diseases accounts for 75% of the nation's health care spending.
Two thirds of the increase in health care spending is due to the increased prevalence of treated chronic disease.
The vast majority of cases of chronic disease could be better prevented or managed.
Many Americans are unaware of the extent to which chronic diseases could be better prevented or managed (1).
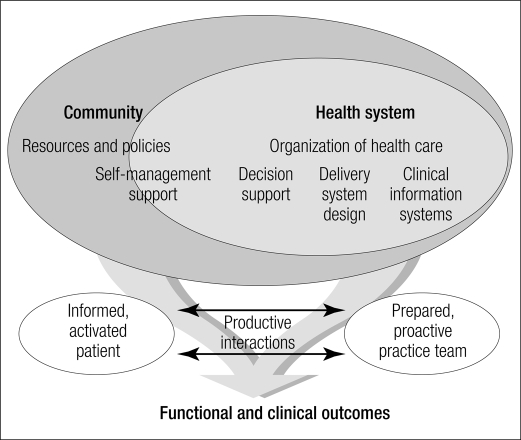
The chronic disease management movement has been in place since the 1990s. This patient-centered approach fosters a multidisciplinary coordination and integration of care emphasizing patient self-management and continuous quality improvement. Wagner presented a chronic care model (Figure 1) and explained:
Patients and families struggling with chronic illness … require planned, regular interactions with their caregivers, with a focus on function and prevention of exacerbations and complications. This interaction includes systematic assessments, attention to treatment guidelines, and behaviorally sophisticated support for the patient's role as self-manager. These interactions must be linked through time by clinically relevant information systems and continuing follow-up initiated by the medical practice (2).
Figure 1.
Model for improvement of chronic illness care. Reprinted from Wagner, 1998 (2), with permission from the American College of Physicians.
At Baylor University Medical Center at Dallas (BUMC), the roots of chronic disease management for patients with pulmonary disease can be traced back to 1981 with the creation of the campus's pulmonary rehabilitation program for patients with chronic obstructive pulmonary disease (COPD) or chronic asthma, and while the outpatient asthma center was created separately from pulmonary rehabilitation, in 1990 both programs intercalated into a single entity with staff sharing responsibilities for the varying aspects of the center.
Since then, the (now) Baylor Martha Foster Lung Care Center (BMFLCC) has applied a multidisciplinary approach to patient care, clinical research, and community outreach and has achieved national recognition for its successes in these endeavors, addressing issues of chronic disease management within a broad spectrum of ages and pulmonary-related diagnoses. Publications as abstract presentations at national and international meetings and peer-reviewed original investigations have regularly flowed from BMFLCC's staff addressing issues in asthma and COPD that impact both the process and content of clinical care. Community interventions such as the provision of peak flow meters for public schools to monitor children with asthma, which was pioneered in Dallas through a cooperative relationship between BUMC and the Dallas Independent School District (DISD), have become models for national programs to improve school-based asthma management, most notably, the American Association of Respiratory Care's Peak Performance USA. Rules of Two™, an innovative asthma assessment and management tool, has been nationally syndicated for use by local asthma coalitions around the country to assist in chronic disease management strategies.
PRIMARY CARE STRATEGIES
The central caregiver at BMFLCC is a respiratory care specialist (RCS), a registered respiratory therapist or registered nurse who has been specially trained in diagnosing and managing pulmonary diseases. This trained individual not only demonstrates value in BMFLCC, but has also been shown to bring a unique value and perspective to different primary care practices. In two separate published studies, one with internal medicine practices and one with geriatric practices, RCS involvement improved both diagnostic and guideline-driven management.
In one study (3), 121 adult patients with asthma, COPD, or both were enrolled, and the RCS provided evaluation services, discussed treatment recommendations with the primary care provider, and provided patient education. A previous study, reported by a BUMC internal medicine resident (4), had revealed deficiencies in both diagnostic and therapeutic compliance with current respiratory guidelines in the primary care setting, and the subsequent RCS–primary care physician partnership reflected the awareness of the need to improve care. The published results exceeded expectations of success. Compared with historical controls:
The rate of rescue inhaler use decreased by 75%.
The respiratory symptom score decreased by 49%.
Use of formal spirometry for diagnosis and assessment of severity increased from 26% to 100%.
The rate of documentation of patient training in proper inhaler device technique increased from 13% to 90%.
The rate of documentation of quick-relief inhaled bronchodilator use increased from 13% to 90% (all P < 0.05).
The skill effectiveness of the RCS was rated by both physicians and patients, with scores (on a 1 to 4 scale) of 3.6 and 3.8, respectively.
Additional revenue from procedures offset the RCS salary cost, so the intervention was cost neutral. Based on that, and the fact that the RCS intervention was both clinically effective and well accepted by patients and primary care physicians, the model was disseminated to other sites within the HealthTexas Provider Network, until staffing and budgetary concerns (notwithstanding cost neutrality) led to the program's end.
RCS involvement on the ground floor of care in geriatric practices of Baylor Health Care System's senior care center network produced similar improvements in patient outcomes. In these senior care centers, one additional objective was to identify seniors with symptomatic but as yet undiagnosed lung disease. The presence of comorbid conditions in el-derly patients, the limited use of functional testing in the primary care setting, common misconceptions about asthma and COPD, and the idea that shortness of breath is part of the aging process lead to underdiagnosis and misdiagnosis of lung diseases.
In the geriatric study (5), 148 senior patients diagnosed with asthma, COPD, unexplained dyspnea, or nicotine dependency were referred for RCS-augmented care. The supplementary service included a preformatted symptom evaluation, diagnostic testing with spirometry, a 6-minute walk to measure exercise tolerance and oxygen desaturation, treatment recommendations to the primary care provider based on GOLD (6) and National Asthma Education and Prevention Program (7) guidelines, and disease-specific patient education including smoking cessation counseling. Again, results were positive:
The patient's diagnosis was changed in 48% of cases.
The treatment was changed in 76% of cases.
Use of spirometry for diagnosis and severity increased from 4% to 100%.
14% of the patients were found to be hypoxic, and 86% of them were started on oxygen therapy.
All patients received disease-specific patient education.
Of the patients who returned for a follow-up visit, 88% reported a reduction in symptoms (all P < 0.05).
As with the study in the internal medicine practices, patient satisfaction with the intervention was very high, and the services provided were cost neutral. RCS intervention led to significant improvements in compliance with evidence-based guideline management. This study extended the diagnostic role of the RCS in assessing not only patients with known asthma or COPD, but also those with dyspnea of uncertain etiology.
DISEASE-SPECIFIC STRATEGIES
As noted earlier, BMFLCC staff have published abstracts for specialty society meetings as well as in the peer-reviewed literature describing the results of investigations in both asthma and COPD. These projects are the result of cooperative efforts of staff RCS and have also included physical and occupational therapists who participate in pulmonary rehabilitation, with administrative and medical oversight and support. The overarching goal of clinical research is to improve chronic disease management.
Within BMFLCC, staff have worked to accurately determine the effectiveness of medication delivery with differing aerosol generators. One recent pilot study, for example, compared the effectiveness of different devices in delivering aerosolized medications in 14 patients (8). Albuterol treatment given with a pressur-ized metered dose inhaler together with a valved-holding chamber facemask and mouthpiece (Aerochamber MAX, Monaghan Medical Corp., Plattsburgh, NY) was shown to be as effective as albuterol treatment given with a small-volume nebulizer in terms of forced expiratory volume in 1 second (FEV1), heart rate, oxygen saturation, perceived work of breathing, and hand tremor 15 and 30 minutes after treatment. A transition to the metered dose inhaler would be more convenient, portable, and efficient than the current “standard” of small-volume nebulization with an air compressor for power.
In an effort to breach the walls barring access to effective medical care for children with asthma, BUMC and DISD have partnered for almost 2 decades in an effort to improve the care of asthmatic students. Not only was Dallas one of the first major urban school districts with peak flow meters used by nurses to assess children with asthma—the result of an educational grant obtained by BMFLCC—but in a unique and innovative strategy that incorporated school-based medication delivery to a select group of asthmatic children who were not receiving optimal asthma care, BMFLCC and DISD school nurses were able to improve school attendance rates to the same level as those of nonasthmatic children. In an article published in Chest (9), BUMC investigators reported attendance rates of asthmatic versus nonasthmatic students and highlighted the critical role that school nurses played in identifying children with out-of-control asthma and referring them for appropriate medical therapy. This paper was cited by the American School Health Association and the American Academy of Pediatrics as one of the “must read” articles about school health in 2009. Although untreated asthma can have devastating effects on academic and athletic performance, with proper supervision and management, the impact of asthma can be minimized.
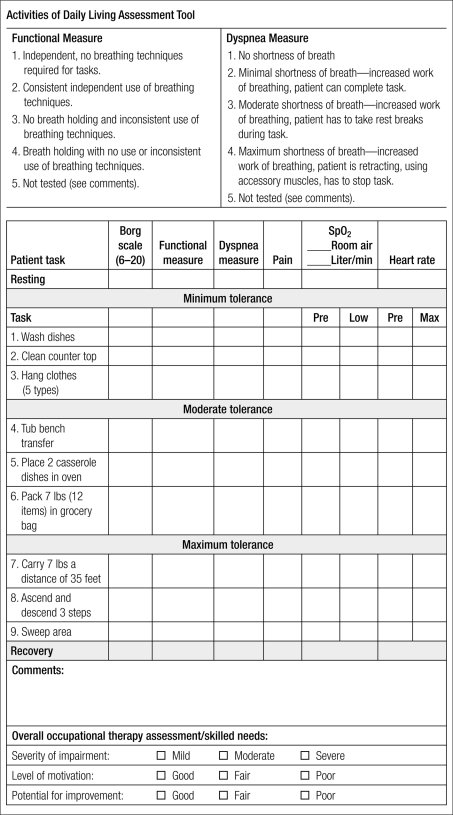
Chronic disease impacts the individual in a myriad of ways, one of the most damaging being deconditioning with activity limitation leading to social withdrawal from the community. In COPD, the goal of pulmonary rehabilitation is to recapture “lost ground,” thereby restoring the patient's endurance and strength and encouraging reintegration into the surrounding community. Unfortunately in pulmonary rehabilitation, outcomes have traditionally been measured by standard tests such as the 6-minute walk and strength testing, without the ability to measure improvements in activities of daily living (ADL) that reflect practical outcomes more specifically. Comprehensive rehabilitation occurs not only when individuals improve exercise abilities, but also when they can return to their roles and occupational tasks. The pulmonary rehabilitation staff subsequently developed and validated a new tool to assess ADL skills (Figure 2) and assess the impact of pulmonary rehabilitation on patients with COPD. In a study involving 36 patients (10), this “tool” was able to show that following pulmonary rehabilitation, the patients were able to demonstrate a significant improvement (all P < 0.05) in five areas:
Effective use of coping skills and relaxation techniques to decrease anxiety, stress, and fear associated with shortness of breath
The application of proper breathing techniques and body mechanics during the performance of the functional tasks related to life roles
Consistent use of energy conservation/work simplification, pacing, and modifications to increase levels of functional independence
An increase in endurance during task completion and a decrease in rest periods between tasks
A return to life roles associated with home, work, school, leisure, community, and social activities
Figure 2.
Form developed by the Baylor Martha Foster Lung Care Center to assess patients' performance of activities of daily living in the pulmonary rehabilitation setting.
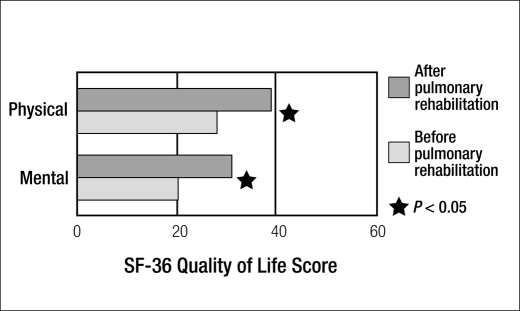
Another study involving 119 patients showed that completion of pulmonary rehabilitation significantly improved patients' quality of life scores (Figure 3) (11).
Figure 3.
SF-36 Quality of Life scores following pulmonary rehabilitation in 119 patients.
Traditional pulmonary rehabilitation employs land-based exercise in training muscles for both strength and endurance. However, a number of patients who would benefit from rehabilitation find themselves unable to participate because of comorbidities such as arthritis, osteoporosis, heart disease, and obesity. Related to the proximity of lap pools at both the Baylor Tom Landry Center and the Baylor Institute for Rehabilitation, the application of water-based exercise to training patients with COPD appeared to offer an innovative approach to circumvent the limitations to rehabilitation from these comorbidities. However, very little information existed in the literature on the effect of partial immersion on lung function and exercise tolerance in COPD when this idea was first considered. Subsequently, members of the rehabilitation team at BMFLCC answered these unaddressed questions and proceeded to develop one of the first water-based pulmonary rehabilitation programs that published outcomes comparing water- and land-based programs. A study comparing results of 20 participants in the aquatics program with 20 matched participants in the land-based program showed equivalent results, with all showing significant improvements in physical performance and quality of life measurements (12). Currently, patients can access an aquatic rehabilitation program offered at the Baylor Institute for Rehabilitation Aquatics Center as part of the BMFLCC pulmonary rehabilitation program during summer months. Aquatic exercise can add variety to established exercise programs and may be the preferred mode for specific patients.
PATIENT EDUCATION STRATEGIES
BUMC created the Rules of Two® for asthma as a way of incorporating national guidelines for managing patients with persistent asthma into a simple paradigm that could frame the discussion between clinicians and lay people related to asthma activity and direct medical therapy with the simple goal of achieving good asthma “control” (Table 1). That this message works has been demonstrated in a number of venues. At the State Fair of Texas in 1999, Rules of Two questionnaires were distributed to attendees with asthma, followed by brief on-site counseling with BMFLCC staff. In follow-up contacts, over half of these contacts reported changing behavior to improve adherence or even discussing with their primary care physician the need for further treatment (13). Rules of Two posters were distributed to all primary care physician offices in Dallas as part of World Asthma Day in 2007 and likewise were placed in the clinics of every school in DISD.
Table.
The Rules of Two®
| • Do you have asthma symptoms or use a quick-relief inhaler more than two times a week? |
| • Do you wake up at night with asthma more than two times a month? |
| • Do you refill the inhaler more than two times a year? |
| • Do you measure your peak flow at less than two times 10 (20%) from baseline with asthma symptoms? |
| If you answered “yes” to any of these questions, ask your health provider whether adding a long-term “controller” medication might provide better control of your asthma. |
A further effort to reinforce this message is the free one-day Camp Airways, held five times a year during school holidays as well as in the summer for asthmatic children aged 8 to 12. During one of these camps, staff assessed asthma severity with history and lung function measurements. Baseline abnormal lung function was identified in nearly a third of the 43 children, including 10 of 25 of those receiving inhaled cortico-steroid therapy and 3 of the 18 not receiving such therapy. In the children with abnormal FEV1, 9 of 10 parents perceived good compliance, whereas only 6 of 10 children reported compliance (14), highlighting the need to focus on symptom management, control, and medication adherence. The Rules of Two was able to be remembered by 79% of the children attending one camp when assessed 6 months afterwards. Telephone assessment of asthma control also indicated improved symptoms following camp attendance. Asthma camp appears to be a good venue to reinforce the need for daily therapy in the setting of persistent asthma.
EMERGENCY CARE STRATEGIES
On average, 80 adult asthma patients are treated in the emergency department (ED) at BUMC each month. From September 2007 to September 2008, the average length of stay (LOS) was 278 minutes for those discharged and 516 minutes for those admitted. Based on Expert Panel Report 3 published by the National Institutes of Health in late 2007 (7), ED management of asthma should take no longer than 180 minutes before a decision can be made for admission or discharge. Having recognized the need for intervention, a quality improvement multidisciplinary asthma ED team, led by BMFLCC, employed quality improvement tools, such as a fishbone cause-and-effect diagram, run charts, and affinity charts, to help identify and prioritize problems responsible for excess LOS (15). The team leader coordinated and facilitated meetings with physicians, respiratory therapists, and nurses.
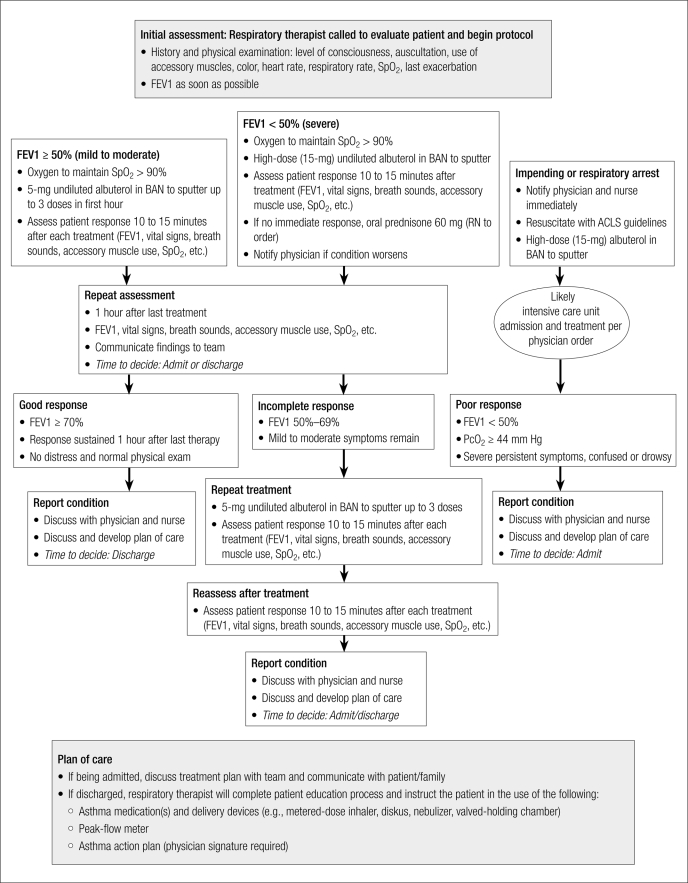
During the first brainstorming session the team discovered that no standardized asthma protocol existed for ED staff. A protocol was developed (Figure 4), and FEV1 meters were given to respiratory therapists to use to determine severity and treatment effectiveness. A breath-actuated nebulizer (AeroEclipse II BAN) was introduced to deliver all bronchodilator therapy more effectively and safely. Staff was educated on the asthma guidelines, choice of medications, use of the protocol, and effective patient handoff. The team leader spent time working with staff in the ED to help improve their performance as they gained more confidence. Physician champions met one on one with physicians to discuss specific cases. Ongoing chart reviews helped identify areas that needed further improvement.
Figure 4.
Asthma treatment protocol for patients aged 12 and over developed for the emergency department at Baylor University Medical Center at Dallas. ACLS indicates advanced cardiac life support; BAN, breath-actuated nebulizer; FEV1, forced expiratory volume in 1 second; PcO2, partial pressure of carbon dioxide; SpO2, saturation of peripheral oxygen.
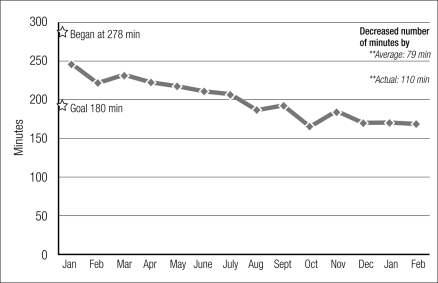
Four months after implementing the asthma protocol, the average LOS decreased significantly (Figure 5) and FEV1 measurements were performed 99% of the time. Medication delivery using the breath-actuated nebulizer was effective, allowing some patients to be discharged who would normally be admitted (15). Further work that links ED discharge with outpatient follow-up and education is under way through a partnership with Baylor's Worth Street Clinic and BMFLCC.
Figure 5.
Reduction in length of stay for patients with the diagnosis of asthma discharged from the emergency department at Baylor University Medical Center at Dallas from January 2009 to February 2010.
CONCLUSION
Although continuing progress is being made in treatment approaches for chronic pulmonary diseases, evidence-based guidelines have been published and widely distributed. The main task is implementation, which is tailored locally. BMFLCC has attempted to address some of the challenges behind the gap between recommended care and current practice—identified in a recent Cochrane review as “poor provider adherence to treatment guidelines, suboptimal patient education and self-care, poor patient adherence to treatment and lifestyle modification, neglect of preventive care and lack of coordination between healthcare providers, among others” (16). But more than just providing local encouragement and implementation strategies to BHCS, the BMFLCC has published its outcomes for all to see the impact that innovative chronic care strategies can achieve.
Acknowledgments
The authors thank Cynthia Orticio, MA, ELS, for editorial contributions.
References
- 1.Partnership to Fight Chronic Disease. An unhealthy truth: rising rates of chronic disease and the future of health care in America [PowerPoint pres-entation]. Available at http://www.fightchronicdisease.org/issues/about.cfm; accessed January 25, 2010.
- 2.Wagner EH. Chronic disease management: what will it take to improve care for chronic illness? Eff Clin Pract. 1998;1(1):2–4. [PubMed] [Google Scholar]
- 3.Boehm R, Petersen P, Hart M, Millard M, Kennerly D. Use of a respiratory care specialist in a primary care practice improves outcomes Poster presented at the meeting of the American College of Chest Physicians, 2003.
- 4.Gipson JS, Millard MW, Kennerly DA, Bokovoy J. Impact of the national asthma guidelines on internal medicine primary care and specialty practice. Proc (Bayl Univ Med Cent) 2000;13(4):407–412. doi: 10.1080/08998280.2000.11927715. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Brown R, Allen J, Boehm R, Hart M, Millard M, Kennerly D. Impact of the respiratory care specialist in diagnosis and management of multiple respiratory conditions in a senior center population Poster presented at the International Respiratory Congress of the American Association for Respiratory Care, 2004.
- 6.Global Initiative for Chronic Obstructive Lung Disease (GOLD). Global strategy for the diagnosis, management, and prevention of chronic obstructive lung disease Medical Communications Resources, Inc., 2009. Available at http://www.goldcopd.com/; accessed January 25, 2010.
- 7.National Heart, Lung, and Blood Institute; National Asthma Education and Prevention Program. Expert Panel Report 3: Guidelines for the Diagnosis and Management of Asthma Bethesda, MD: US Department of Health and Human Services, 2007. Available at http://www.nhlbi.nih.gov/guidelines/asthma/asthgdln.htm; accessed January 25, 2010.
- 8.Hart M, Abmas E, Boehm R, Hernandez G, Gilder R, Millard M. Comparison of valved-holding chamber (VHC)-facemask/mouthpiece with small volume nebulizer-facemask (SVN-F) for bronchodilator delivery Poster presented at the Annual Congress of the European Respiratory Society, Vienna, Austria, 2009.
- 9.Millard MW, Johnson PT, Hilton A, Hart M. Children with asthma miss more school: fact or fiction? Chest. 2009;135(2):303–306. doi: 10.1378/chest.08-1642. [DOI] [PubMed] [Google Scholar]
- 10.Hart M, Duncan C, Aguirre-Kelley L, Lotshaw A, Millard M. Improvement in physical performance coincides with improvement in activities of daily living performance following pulmonary rehabilitation. Chest. 2005;128(4):253S. [Google Scholar]
- 11.Hart M, Aguirre-Kelley L, Abmas E, Lotshaw A, Millard M. Does improvement in activity of daily living performance relate to improvement in quality of life in pulmonary rehabilitation? Poster presented at the meeting of the American Thoracic Society, 2004.
- 12.Lotshaw AM, Thompson M, Sadowsky HS, Hart MK, Millard MW. Quality of life and physical performance in land- and water-based pulmonary rehabilitation. J Cardiopulm Rehabil Prev. 2007;27(4):247–251. doi: 10.1097/01.HCR.0000281772.28394.30. [DOI] [PubMed] [Google Scholar]
- 13.Millard M, et al. The Dallas Asthma Consortium. Am J Respir Crit Care Med. 1999;159(3):A126. [Google Scholar]
- 14.Abmas E, Duncan C, Hart M, Millard M. The impact of inhaled corticosteroid therapy and compliance on FEV1 in asthmatic children Poster presented at the International Respiratory Congress of the American Association for Respiratory Care, 2003.
- 15.Hart MK, Alexander V, Daniel E, D'Etienne J, Millard M. Decreasing the length of stay in the emergency department for patients discharged with asthma Poster presented at the International Respiratory Congress of the American Association for Respiratory Care, 2009.
- 16.Peytremann-Bridevaux I, Gex G, Bridevaux PO, Burnand B. Chronic disease management programs for adults with asthma (protocol). Coch-rane Database of Systematic Reviews 2009;Issue 3, Art. No. CD007988. Available at http://mrw.interscience.wiley.com/cochrane/clsysrev/articles/CD007988/frame.html; accessed January 25, 2010. [DOI] [PMC free article] [PubMed]