Diabetes: it's the seventh leading cause of death, a major cause of heart disease and stroke, and the leading cause of adult blindness, kidney failure, and nontraumatic lower-extremity amputations, responsible for $116 billion in direct medical costs in the United States and $58 billion more in indirect costs, such as disability. Diabetes is an epidemic, with 23.6 million people affected—5.7 million of whom are undiagnosed—and rates that continue to grow. Moreover, diabetes is not a disease that affects all equally: African Americans, Hispanics, American Indians, and Alaska Natives are twice as likely as white adults to have diabetes. Further, diabetes is more common among those with less education, with disease rates of 15.8% among those without a high school diploma compared with 6.9% among those who attended college. A quarter of all adults aged 60 and older have the disease, and a third of all US children born in 2000 could develop it during their lifetime (1).
Statistics for the state of Texas are even worse than the national average:
The prevalence of diabetes in Texans aged 18 and older rose to 10.3% in 2007.
More than 1.8 million adults in Texas are diabetic, and 460,000 are believed to be undiagnosed.
Diabetes rates were 12.9% among African Americans, 12.2% among Hispanics, 11.8% among other minorities, and 8.5% among whites (1).
These latest statistics from the Centers for Disease Control and Prevention (CDC) (1) reinforce the need to prevent diabetes and manage it to avoid the worst outcomes for patients. This article provides a brief overview of the patient empowerment model promoted by Baylor Health Care System (BHCS). It then describes BHCS's coordinated efforts for disease management, as well as its new community outreach program and Diabetes Health and Wellness Institute—both projects of the BHCS Office of Health Equity.
PATIENT EDUCATION AND EMPOWERMENT
In regular office visits for diabetes care, health care professionals tend to focus on several treatment targets and ensure that examinations are completed to assess for potential complications. Despite the array of medications available, however, most patients do not reach the goals for the targets (Table 1) (2).
Table 1.
Goals for patients with diabetes
Anderson and Funnell pointed out that patients provide 98% of their own diabetes care (4); the main self-care efforts are outlined in Table 2. Thus, patients' daily decisions have the greatest impact on their health, and they are responsible for the actions and the consequences. While health care professionals have an important role in helping patients make informed self-management decisions, according to the patient empowerment model, they cannot control patients' self-care decisions. Instead, they focus on asking questions, beginning the office visit with the patient's agenda, and developing an individualized treatment plan or contract with the patient. A step-by-step approach is helpful, focusing on behaviors and problem-solving skills rather than outcomes. It is also important to involve family members and other supports, maintain contact between visits, and nourish patients' coping skills. Finally, health care professionals need to obtain assistance from colleagues and refer patients to specialists as needed (4). Table 3 reiterates these steps and translates them into questions that can be asked during office visits using the empowerment model.
Table 2.
Self-care behaviors for patients with diabetes∗
| Behavior | Comments |
| Healthy eating | Making healthy food choices, understanding portion sizes, and learning the best times to eat are central to managing diabetes. By making appropriate food selections, children and teenagers grow and develop as they would if they didn't have diabetes. And, by controlling their weight, many adults may be able to manage their condition for a time without medications. |
| Being active | Regular activity is important for overall fitness, weight management, and blood glucose control. With appropriate levels of exercise, those at risk for type 2 diabetes can reduce that risk, and those with diabetes can improve glycemic control. Being active can also help improve body mass index, enhance weight loss, help control lipids and blood pressure, and reduce stress. |
| Monitoring | Daily self-monitoring of blood glucose provides people with diabetes the information they need to assess how food, physical activity, and medications affect their blood glucose levels. People with diabetes also need to regularly check their blood pressure, urine ketones, and weight. |
| Taking medication | The health care team will be able to determine which medications those with diabetes should be taking and help them understand how these medications work. Effective drug therapy, in combination with healthy lifestyle choices, can lower blood glucose levels, reduce the risk of diabetes complications, and produce other clinical benefits. |
| Problem solving | Those with diabetes must keep their problem-solving skills sharp because on any given day, a high or low blood glucose episode or a sick day will require them to make rapid, informed decisions about food, activity, and medications. This skill is continuously put to use because even after decades of living with the disease, stability is never fully attained: the disease is progressive, chronic complications emerge, life situations change, and patients age. |
| Reducing risks | Effective risk reduction behaviors such as smoking cessation and regular eye, foot, and dental examinations reduce diabetes complications and maximize health and quality of life. An important part of self-care is learning to understand, seek, and regularly obtain an array of preventive services. |
| Healthy coping | Health status and quality of life are affected by psychological and social factors. Psychological distress directly affects health and indirectly influences motivation to keep diabetes in control. When motivation is dampened, the commitments required for effective self-care are difficult to maintain. |
∗Adapted from American Association of Diabetes Educators (http://www.diabeteseducator.org/ProfessionalResources/AADE7/).
Table 3.
Four-step patient empowerment counseling model∗
| Step | Question to ask patient |
| 1. Help patient identify diabetes-related problems and issues on which they want to work. | What problem are you having with diabetes that you want to work on? |
| 2. Help patient identify thoughts and feelings associated with an issue. | What are you thinking and feeling when you are struggling with the problem? |
| 3. Help patient identify health-related attitudes and beliefs underlying the problem and establish diabetes self-care goals. | What deeper attitudes and beliefs lead you to think and feel as you do when you are struggling with a problem? |
| What is your ultimate goal for dealing with the problem? | |
| 4. Help patient develop and commit to a plan for achieving their goal. | What would be the steps, one by one, that would lead to you reaching your goal? |
∗Reprinted with permission from the American Association of Diabetes Educators (5).
These questions relate to the “LIFE” approach Funnell and Weiss later described. This framework consists of four steps: L, learn about diabetes, the health care team, and personal life circumstances; I, identity the three guiding principles of role, flexibility, and targets; F, formulate a personal self-management plan; and E, experiment with and evaluate the plan (6). Thus, while education is involved, it is personalized, ongoing, and touches on more than the disease process and medications. Equal emphasis is placed on individual patient goal setting. Professionals feel responsible to their patients, not responsible for them (7). This is the model Baylor Health Care System has espoused in its partnership with patients with diabetes.
BHCS'S EFFORTS TO IMPROVE DIABETES CARE
A BHCS Diabetes Council was established in October 2008 to coordinate and provide a systematic approach to diabetes care across BHCS. This council, which reports to the BHCS Best Care Committee, includes physicians (representing primarily endocrinology but also cardiology, primary care, and kidney/pancreas transplantation), administrators (including BHCS's chief medical officer, chief quality officer, and other senior leaders), and diabetes educators. Subgroups on inpatient care and outpatient care have taken numerous steps to improve care.
Inpatient efforts
An inpatient workgroup of the Diabetes Council established three strategies for inpatients with diabetes at all BHCS hospitals: to reduce hypoglycemia and hyperglycemia, to improve the timing of insulin administration, and to improve overall care, including transitions of care. Efforts are currently under way to improve medication reconciliation, to develop a care coordination/social work care plan, and to develop a stan-dardized diabetes education training plan for inpatient diabetes resource teams. Order sets are also being developed and tested for patients admitted with diabetic ketoacidosis. Finally, the group is developing a diabetes scorecard to reflect clinical and process improvements in the care of patients with diabetes at a facility level. The scorecard will have six measures:
Hemoglobin A1C on admission (process/patient outcome)
Length of stay
30-day mortality
30-day readmission rate
Emergency department visits
Severity index and population information (primary and secondary diagnoses)
Also being considered for the scorecard are measures to capture hypoglycemia, hyperglycemia, outpatient referrals for diabetes education, and complication rates/comorbid conditions.
Outpatient efforts
In BHCS, outpatient diabetes education services are offered in 8 hospital-based diabetes education centers, 2 senior health centers, as well as physician offices. Since 1998, the outpatient diabetes education centers have provided quality diabetes self-management education, as recognized by the American Diabetes Association. In 2009 over 4000 patients received diabetes self-management education in one of Baylor's ADA–recognized education centers.
The outpatient workgroup of the BHCS Diabetes Council is involved in several initiatives:
Providing current, accurate, and convenient online diabetes resources for ambulatory providers and increasing awareness of these resources
Standardizing diabetes education materials provided to patients across the continuum of care throughout BHCS
Providing a standard staff diabetes education training program for the outpatient care team
Initiating a diabetes wellness program for employees
Equity efforts: grant for outreach and culturally competent care
In 2009, Baylor's Office of Health Equity received a grant supporting a community diabetes education initiative for the underinsured and uninsured throughout Dallas County. The $1.7 million, 5-year Diabetes Equity Project grant, supported by The Merck Company Foundation through its Merck Alliance to Reduce Disparities in Diabetes program, was given so BHCS could expand the existing CoDE™ (Community Diabetes Education) program at Central Dallas Ministries. As one facet of the project, diabetes health promotion “community hubs” have been established at Baylor Family Medicine at Worth Street, Healing Hands Ministries of Lake Highlands, HOPE Clinic of Garland, and Irving Interfaith Clinic.
In CoDE, bilingual community health workers meet one on one with patients for seven 60-minute visits during a 12-month period. They discuss crucial diabetes topics such as blood glucose levels, medications, exercise, and nutrition. Key to this intervention is the amount of time spent in conversation between the patient and community health worker, who mirrors the primary patient demographic. Initially, the community health workers concentrate on teaching self-management skills, but over time, as their relationship with the patient develops, they become a case manager and patient advocate. Results reported at 1 year showed annual direct medical expenditures of $461 per participant and significant reduction in hemoglobin A1C levels in patients who participated in the program for 12 months compared with a control group (8).
Baylor's Office of Health Equity has enhanced this patient intervention by utilizing a newly created job type, the diabetes health promoter. This medical assistant is state certified as a community health worker through a 160-hour program and participates in 50 hours of diabetes/clinical training initially, with several hours of ongoing continuing education each month. Frequent, intentional coordination with the patient's primary care provider is critical to this model. Community partnerships are also important to the intervention, including funding from the Genesis Medical Foundation to provide mobile retinal scans; coordination with Project Access Dallas, Dallas County Medical Society's safety net for the uninsured; and other organizations such as the North Texas Food Bank.
In addition to the patient intervention, the Diabetes Equity Project offers continuing education for providers on cross-cultural care. National experts will lead evidence-based continuing education sessions on strategies that foster patient adherence. Twelve events will be conducted throughout Dallas County over the next 4 years.
Lastly, clinical, quality of life, health status, satisfaction, and process outcome measures will be collected on the 1000 or more patients who enroll in the project. This data will assist BHCS and the broader health care arena in improving outcomes for people with diabetes, particularly those who are disadvantaged because of socioeconomic status, language, or lack of insurance.
Equity efforts: new diabetes center in South Dallas
Finally, when BHCS's Office of Health Equity was organized in 2006 with the vision of improving health care quality through the elimination of variation in health care access, delivery, and outcomes, it identified the Frazier community of South Dallas as having the greatest potential for health equity improvement:
The hospitalization rates for diabetes in South Dallas averaged 412.9 per 100,000 in the years 2000, 2002, and 2003, compared with 175.3 per 100,000 for Dallas County as a whole in the same period.
The diabetes death rate was 57.4 per 100,000 persons in 2003 in ZIP code 75210 in South Dallas, compared with 21.7 per 100,000 persons for Dallas County as a whole.
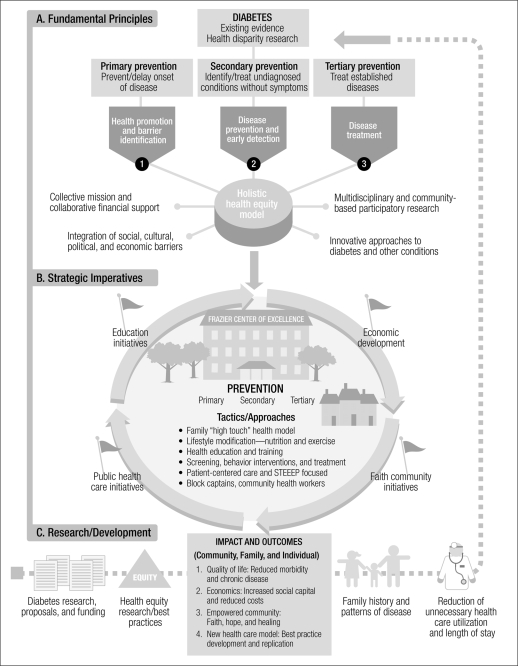
The office planned a center of excellence in diabetes care for this area. The first part of the model for this center (Figure 1) focuses on the chronic disease of diabetes while utilizing three core competencies—primary, secondary, and tertiary—to prevent and delay the onset of disease as well as identify and treat established disease. The model integrates four key factors to ensure that its strategic foundation is collaborative, holistic, innovative, and community based.
Figure 1.
BHCS's diabetes health model in South Dallas. STEEEP™ indicates safe, timely, effective, efficient, equitable, and patient-centered care.
The second part of the model provides a snapshot of the center of excellence working in concert with community partners to promote and implement education, public health, economic development, and faith-based initiatives, as well as clinical interventions. Services extend the walls of the building and are delivered to residents in the community to increase public awareness and promote individual empowerment. A variety of services are offered to encourage individual and family lifestyle changes through screening, health education/training, behavior intervention, and treatment.
The third part of the model identifies development and research opportunities generated by outcomes that impact the community, families, and individuals. Not only can this model improve health promotion and disease prevention, but it can also improve the economy, community empowerment, and quality of life. It is expected that the cost associated with disease and illness will be reduced by increasing the utilization of screening tests for early detection and treatment, which in turn will reduce unnecessary health care utilization and the length of hospital stays. Further, quality of life will be enhanced by offering Frazier residents the opportunity to improve their health status and overcome other barriers, which will result in the reduction of morbidity and chronic disease. The aforementioned outcomes subsequently produce the body of knowledge needed to conduct additional diabetes research, submit proposals for external funding, substantiate best practices for equity research, and assist in detecting patterns of disease. This information will contribute to health disparity research and enable innovative approaches in primary, secondary, and tertiary prevention to be developed and utilized in the future to detect and treat diabetes and other disabling conditions.
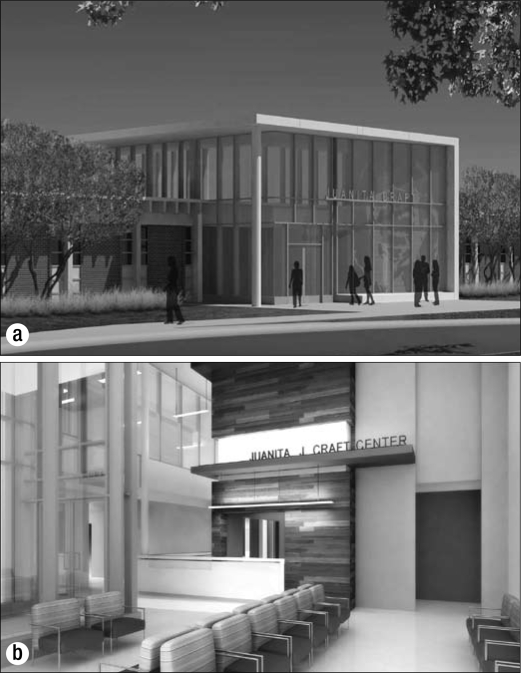
Applying this model, BHCS transformed a local recreation center into the area's first and only diabetes health and wellness institute, with the goal of weaving diabetes prevention into the fabric of the community so that it is a natural and convenient part of life in this neighborhood. The Diabetes Health and Wellness Institute at the Juanita J. Craft Recreation Center opened in June 2010 (Figure 2). It provides a variety of services, all delivered with the patient empowerment approach:
A full-time, on-site physician and nurse practitioner
Visiting medical specialists
Referral coordinator for specialty and ancillary care
Certified diabetes educators
Exercise physiologist
Community health educators
Community diabetes ambassadors
-
Other services:
○ Affordable diabetes medications
○ Health and wellness programs
○ Nutrition and healthy cooking classes
○ Exercise programs including running and walking clinics and weight training
○ Social services
○ Parks and Recreation programs
○ Van service/transportation assistance
Figure 2.
The Diabetes Health and Wellness Institute at the Juanita J. Craft Recreation Center: (a) exterior and (b) interior.
Baylor Health Care System has invested $15 million in the project. The city of Dallas invested $2 million plus the use of the Juanita J. Craft Recreation Center. The goal of the institute is not just to provide diabetes care, but to change the health outlook for the entire family and the South Dallas community.
CONCLUSION
BHCS has set the goal of providing a best-in-class center for comprehensive diabetes care, research, education, and prevention, and its efforts to coordinate care throughout the system highlight a team approach—involving not only multidisciplinary health care providers but first and foremost the patient. As Funnell and Anderson commented, the patient has the choices, the control, and the consequences (7). Just as the patient must attend to many details and address diabetes management in the context of daily routines, BHCS is focusing on its “daily routines”: its systems, its processes of care, its staff's education, its own monitoring through outcomes—to continuously improve and provide safe, timely, effective, efficient, equitable, and patient-centered care for this growing group of patients.
Acknowledgments
The authors thank Cynthia Orticio, MA, ELS, for editorial contributions.
References
- 1.Centers for Disease Control and Prevention . National Diabetes Fact Sheet: General Information and National Estimates on Diabetes in the United States, 2007. Atlanta, GA: CDC; 2008. [Google Scholar]
- 2.Ho PM, Rumsfeld JS, Masoudi FA, McClure DL, Plomondon ME, Steiner JF, Magid DJ. Effect of medication nonadherence on hospitalization and mortality among patients with diabetes mellitus. Arch Intern Med. 2006;166(17):1836–1841. doi: 10.1001/archinte.166.17.1836. [DOI] [PubMed] [Google Scholar]
- 3.American Diabetes Association Standards of medical care in diabetes—2010. Diabetes Care. 2010;33(Suppl 1):S11–S61. doi: 10.2337/dc10-S011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Anderson RM, Funnell MM. Patient empowerment: myths and misconceptions. Patient Educ Couns 2009 Aug 12 [Epub ahead of print]. [DOI] [PMC free article] [PubMed]
- 5.Franz MJ, editor. A Core Curriculum for Diabetes Education: Diabetes and Complications. 5th ed. Chicago, IL: American Association of Diabetes Educators; 2003. [Google Scholar]
- 6.Funnell MM, Weiss MA. Patient empowerment: the LIFE approach. European Diabetes Nursing. 2009;5(2):75–78. [Google Scholar]
- 7.Funnell MM, Anderson RM. Empowerment and self-management of diabetes. Clinical Diabetes. 2004;22(3):123–127. [Google Scholar]
- 8.Culica D, Walton JW, Prezio EA. CoDE: Community Diabetes Education for uninsured Mexican Americans. Proc (Bayl Univ Med Cent) 2007;20(2):111–117. doi: 10.1080/08998280.2007.11928263. [DOI] [PMC free article] [PubMed] [Google Scholar]