Abstract
Objectives:
The Medical Library Association (MLA)/National Library of Medicine (NLM) Joint Electronic Personal Health Record Task Force examined the current state of personal health records (PHRs).
Methods:
A working definition of PHRs was formulated, and a database was built with fields for specified PHR characteristics. PHRs were identified and listed. Each task force member was assigned a portion of the list for data gathering. Findings were recorded in the database.
Results:
Of the 117 PHRs identified, 91 were viable. Almost half were standalone products. A number used national standards for nomenclature and/or record structure. Less than half were mobile device enabled. Some were publicly available, and others were offered only to enrollees of particular health plans or employees at particular institutions. A few were targeted to special health conditions.
Conclusions:
The PHR field is very dynamic. While most PHR products have some common elements, their features can vary. PHRs can link their users with librarians and information resources. MLA and NLM have taken an active role in making this connection and in encouraging librarians to assume this assistance role with PHRs.
Highlights.
A variety of personal health records (PHRs) exist with some tied to medical health records and others offered as standalone products.
Librarians can be connected to PHR users through inclusion of an assistance statement in PHRs.
PHRs offer librarians another means of providing consumers with quality health information.
Implications.
PHR user support is a new role for medical librarians.
Medical librarians need to be proactive in their communities to educate consumers about PHRs.
Given the dynamic nature of this market, medical librarians should make a concerted effort to stay abreast of trends in this area.
INTRODUCTION
The idea of connecting medical librarians and quality health information resources with personal health record (PHR) consumers was the rationale behind the formation of the Medical Library Association (MLA)/National Library of Medicine (NLM) Joint Electronic Personal Health Record Task Force. Among other tasks, the group was charged with identifying key providers of PHRs. Findings reported here ensued from the work of this task force.
The first PHRs, of course, were paper-based, and many people still maintain their personal health information in print. The emergence of consumer-driven health care has led to a greater interest in access to personal health information. As health providers began to shift their records to electronic formats, demand began to emerge for patients to be able to access their health information online. In reviewing literature about the development of electronic PHRs, the task force found that PHRs were still evolving and that a wide range of professions, organizations, and agencies had interest in them (e.g., American Medical Informatics Association, Chilmark Research, Markle Foundation, AARP, the US government, health insurers, health information management organizations, health care providers, health information technology organizations, and others). One of the developments that occurred during the work of the task force was the entry of Google and Microsoft into the list of PHR players.
There is evidence of a growing demand for PHRs. In a 2008 Deloitte survey of health care consumers, 78% of respondents indicated that they were interested in having online access to medical records and test results provided by doctors, while 76% were interested in online access to an integrated medical record, 72% in online scheduling of appointments, and 69% in a website providing information about health conditions or treatments [1]. The Center for Information Technology Leadership (CITL) reported that PHRs could result in an annual net value of $19 billion, based on a 10-year implementation period and an 80% adoption rate by the US population. The CITL document implied that health information exchange would be more efficient with widespread use of PHRs and that the resulting patient engagement would improve quality of care [2].
Several movements are behind the growing popularity of PHRs, including interest in web-based social networking and the Health 2.0 movement [3]. Another concept that promotes the PHR as a tool for patient self-management is the web-based personal medical home model [4]. Many consumers have PHRs through their employers, health insurers, or health providers. Additionally, there are consumers who have PHRs through independent vendors. One estimate indicates that seventy million people in the United States have access to a PHR [5]. While the work of the task force did not focus on consumer acceptance of PHR technology, there is literature that addresses this issue [6].
METHODOLOGY
The task force began its work by defining “personal health record” for the purpose of identifying PHRs and key players in the field. After examining various existing definitions, the following working definition was accepted:
Electronic personal health record (PHR): a private, secure application through which an individual may access, manage, and share his or her health information. The PHR can include information that is entered by the consumer and/or data from other sources such as pharmacies, labs, and health care providers. The PHR may or may not include information from the electronic health record (EHR) that is maintained by the health care provider and is not synonymous with the EHR. PHR sponsors include vendors who may or may not charge a fee, health care organizations such as hospitals, health insurance companies, or employers.
Particular attributes of PHRs were selected to be tagged as fields in a database. The database was structured to collect the information found in Table 1. The task force quickly found that a number of different organizations were interested in PHRs and had accumulated their own lists of PHRs. These included health insurers, foundations, retired individuals, and those in the fields of health information technology, medical records, and medical informatics. PHRs were identified through these lists, a literature review, news releases, and the experience of task force members. A cumulative list of PHR products was compiled, and each member was assigned a portion of the list that included PHR vendors as well as institutions that offered PHRs to their employees. Task force members then began gathering data via websites, telephone calls, and email contacts with representatives who could answer specific questions about their PHR products.
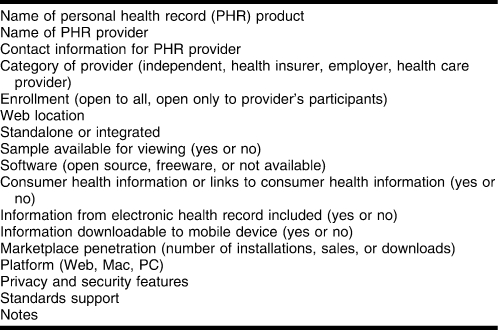
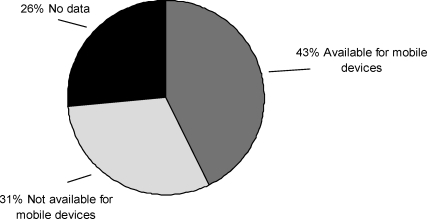
Table 1.
Data elements for personal health record entries
The PHR inventory database evolved during the process of identifying PHRs. Task force members discovered that, in some cases, different health systems were using the same PHRs and some entries had to be merged. Also, after further investigation some of the assigned PHRs did not actually meet the task force's working definition or were no longer viable. To maintain a record of these nonviable PHRs, a note was created in the database. Any PHR that was tagged as not meeting the definition went into a separate area of the database. In general, websites did not provide all the information required to complete each field in the database. When a representative for a PHR could not be reached, some fields were left blank. Fields were also left blank if the person contacted could not provide particular pieces of information, such as marketing data or technical information about software and security. Marketplace penetration, for example, was considered proprietary information by many vendors.
After collecting data for a number of PHRs, the group asked for assistance in identifying additional or missed PHRs; informal calls for information were placed on appropriate email discussion lists and in a special edition of MLA-FOCUS, MLA's online member newsletter [7]. Email discussion list members were asked to submit additional PHR products not named on a provided list of identified viable PHRs. New PHR products continued to enter the market, but the task force set a date to stop gathering data so that analysis of the collected data could commence.
RESULTS
The task force initially identified 85 PHR products, but the working list increased to 121 after all data gathering was completed. Ultimately, 117 PHR products were entered into the database after eliminating duplicates. Of those, 91 both met the task force's definition and were currently available. The remaining 26 did not meet the working definition, had not yet been implemented, or were defunct. Contact with an actual representative, either by telephone or in person, was attempted for all the PHR products on the working list and was successful for 55 of the PHR listings. Information for the remainder was gathered from whatever data were available at their websites.
Findings provided a snapshot of the state of PHRs at a given time. As shown in Figure 1, many of the PHRs were standalone products (non-tethered) with all information self-entered by the consumer. Others were integrated with official EHRs (tethered) offered by a health care provider or insurer. Some PHR vendors provided both standalone and integrated versions of their products, depending on whether the vendor was working directly with a patient or with a health care provider who, in turn, made the product available to patients. Features varied, such as whether or not prescription refills were available through the PHR and whether or not secure messaging between providers and patients was available. Some PHR products actually allowed patients to see portions of their official EHRs. The purpose also varied from one product to another. While a number of PHRs offered an overall health history to simplify health information exchange, others focused on a particular aspect of health, such as chronic pain or end of life issues, or on a specific population, such as children or migrant workers.
Figure 1.
Personal health records (PHRs) integrated with electronic health records (n = 91)
The task force found that some PHRs were available for anyone who wishes to use them. Others required enrollment in a particular health plan and/or under a particular employer or with a particular provider. In these cases, vendors might have reported that they were “open to all,” meaning “open to all in their system,” rather than open to the public. Many PHRs were free to consumers, such as those that were on the web where information was self-entered. The PHRs that charge consumers were mainly those that offered special formats, such as CDs, flash drives, bracelets, or wallet cards. Health providers, insurers, and employers who offered PHRs to users often paid the PHR providers but did not pass along a charge to their users. Some health systems developed their own PHRs.
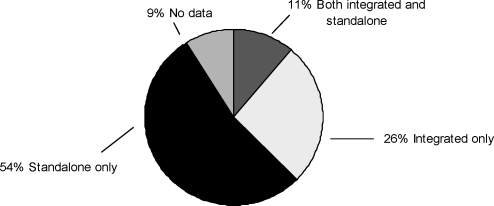
Approximately half of the examined PHRs contained consumer health information (CHI), as shown in Figure 2. The most commonly linked CHI resource was MedlinePlus, followed by Healthwise, information from medical societies or organizations, and vendor-developed content. Aside from societal information and vendor-developed content, the CHI resources included:
Figure 2.
PHRs with consumer health information (CHI) (n = 91)
Centers for Disease Control and Prevention (CDC) <http://www.cdc.gov>
Cerner Multum: Medisource Desktop Reference <http://www.multum.com/mdoc/MediSource-DeskRef.pdf>
Healthwise <http://www.healthwise.org>
Mayo Clinic <http://www.mayoclinic.com>
MedlinePlus <http://www.medlineplus.gov>
MyOptumHealth.com <http://www.myoptumhealth.com>
WebMD <http://www.webmd.com>
Only 10% (n = 9) of the PHRs reported operating on open source software or freeware, although the type of software used was undetermined for more than a third of them. Of the few products using open source software, only one open source license was revealed: Tolven's ePHR uses Lesser GPL.
A number of the existing PHRs used particular standards and might employ more than one standard. Others indicated that they were monitoring the development of standards and would adopt them in the future. Standards might be related to structure of the records or to the nomenclature used by the records. Structural standards (some of which were subsets of one another) that were specifically mentioned by the PHR vendors were:
Continuity of Care Document (CCD)
ASTM Continuity of Care Record (CCR)
Clinical Document Architecture (CDA)
Digital Imaging and Communications in Medicine (DICOM)
Good Electronic Health Record (GEHR)
Health Level Seven (HL-7)
Nomenclature standards mentioned by the PHR vendors were:
International Classification of Diseases (ICD-9-CM/ICD-10)
Systemized Nomenclature of Medicine (SNOMED)
Vocabularies contained in the Unified Medical Language System (UMLS)
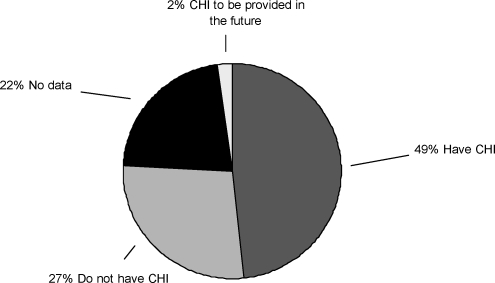
Of the currently available PHRs examined, the majority operated on a web-based platform. As shown in Figure 3, fewer than half were available for use with mobile devices. A portion of those were initially sold as mobile devices, such as flash drives that were incorporated into bracelets or wallet cards. These were mainly for use in emergency situations. As smart phones become more prevalent, there may be more demand for access to PHRs on these devices, but none of the vendors mentioned specifically targeting their products toward mobile devices.
Figure 3.
PHRs on mobile devices (n = 91)
Security is an important issue for protecting the privacy of personal information in PHRs. Many of the web-based products used secure socket layer (SSL) to enable encryption. A number of them specified the VeriSign certificate authority, often seen when making online purchases with a credit card. While the vendor representatives sometimes could not name any security features beyond requiring password access, others mentioned protected servers, firewalls, and compliance with the Health Insurance Portability and Accountability Act (HIPAA).
DISCUSSION
During the course of its work, the task force has found that PHRs can be quite different from one product to another. As noted by the National Committee on Vital and Health Statistics, PHR attributes can vary by:
the scope or nature of the information and contents
the source of the information
the features and functions offered
the custodian of the record
the storage location of the contents
the technical approach
the party who authorizes access to the information [8]
Even the simplest ones can be invaluable to consumers who need a central place to keep their medical histories, easing the pain of filling out forms when visiting a new provider. One of the products actually calls itself “NoMoreClipboard!”
Project Health Design, sponsored by the Robert Wood Johnson Foundation, has made interoperability a major focus in its development of a common platform for personal health applications. The Common Platform Components software is now available under an open source license [9]. Interoperability will be an important factor in any widespread adoption of PHRs.
FUTURE TRENDS
Certification of PHRs is a possibility for the future. The Certification Commission for Health Information Technology (CCHIT) has both a Personal Health Record Work Group and a PHR Advisory Task Force, the latter of which has recommended certification of these PHR attributes: privacy, security, interoperability, and functionality [10]. The CCHIT PHR Advisory Task Force has a notable roster representing the government, individual patients, consumers, hospitals, health information management organizations, health foundations, health insurers, health information technology organizations, organizations such as the American Heart Association, and large employers such as Wal-Mart.
Adoption of national standards will be a necessity because it will be crucial for interoperability, transportability, and security, features that will likely be mandated by legislation. As both EHRs and PHRs become standardized, patients will be able to move from one place to another and have their medical records accessible and transferable wherever they go. MyChart, developed by Epic, is one of the most widely used PHRs by health systems such as Kaiser Permanente. With the entry of Microsoft's HealthVault in October 2007 and Google Health in February 2008 into the PHR market, PHRs have become more competitive. Both Google and Microsoft were represented at the “Personal Health Records: From Biomedical Research to People's Health” conference, sponsored by the Friends of the National Library of Medicine in May 2009 [11]. James Mault of Microsoft spoke about some of their PHR partnerships, including those with Mayo Clinic, Aetna, and AT&T, to name a few [12]. Alfred Spector of Google noted a number of GoogleHealth partners, including Beth Israel Deaconess Medical Center, Cleveland Clinic, CVS, and Longs Drug Stores [13]. Government agencies, foundations, and corporations are all working on systems to make people's health records available to them.
During the tenure of the task force (April 2007 to December 2008), privacy protection was voluntary on the part of PHR providers as HIPAA regulations do not cover PHRs offered by commercial vendors [14]. However, the US government has since begun to make PHR consumers aware of privacy issues and to protect them. In May 2009, the Office of the National Coordinator for Health Information Technology began a project to develop an online model for PHR providers to present data regarding their privacy, security, and information management policies [15]. In August 2009, the Federal Trade Commission issued a final rule, as part of the American Recovery and Reinvestment Act, requiring web-based businesses to notify consumers when the security of their electronic health information is breached [16].
Librarians' roles in personal health records
In addition to assaying the current state of PHRs, the task force tried to identify ways in which librarians could provide assistance to consumers in finding reliable health information in the context of the PHR. PHR users who are online may be consulting questionable sources such as wikis, blogs, and social networking sites [17]. The task force began drafting a statement that could be inserted in PHRs to alert users that they can obtain information from authoritative resources such as NLM's MedlinePlus [18] and those listed at MLA's Consumer and Patient Health Information Section website [19], as well as through direct contact with medical librarians. Email and telephone conferences with task force members were used to refine the statement. A plain language expert at NLM was also consulted, and, as a result, the statement's length was abbreviated. The assistance statement reads:
For quality health information, connect to National Library of Medicine's MedlinePlus for patients, families, and the public <http://www.medlineplus.gov/>, Resources for Health Consumers <http://www.mlanet.org/resources/consumr_index.html> or a Top 100 List ranked by medical librarians <http://www.caphis.mlanet.org/consumer/>.Medical librarians can help you find other health information. To find a medical librarian near you, call 1-800-338-7657 or view http://www.nlm.nih.gov/medlineplus/libraries.html. Librarians will not provide personal medical advice, but they will find trusted information about drugs, conditions, procedures, lab tests and other health topics.
PHR providers have been contacted and asked to embed the assistance statement in PHRs so that users could connect to quality resources endorsed by medical librarians or obtain help directly from medical librarians in finding answers to their health-related questions. Working with vendors to incorporate the assistance statement into their PHR products is ongoing. During the term of the task force, a small test was conducted with seven vendors. A letter signed by the president of MLA and the director of NLM was sent to these vendors in summer 2008. Three responded positively on behalf of four products:
Medem: iHealth Record
Tolven: ePHR
Access Strategies: Follow Me and MiVIA
Demonstrating again how dynamic the PHR field is, Medem's iHealth Record has already been sold to another vendor, Medfusion.
In a paper on the governance for PHRs, Reti et al. found, that among the organizations with more than 10,000 registered PHR users, only the Department of Veterans Affairs included librarians in the PHR governance structure. However, Medem did include an informatician, and several others reported including chief information officers, who might or might not have been informaticians [20]. Curious as to additional roles, the task force conducted informal surveys via selected email discussion lists and MLA-FOCUS [7]. Librarians were asked if they currently played a role with PHRs and, if so, what that role was. Responses included the following:
assisting patients with registering for PHRs
training employees in the use of PHRs
educating staff on how use of PHRs might reduce costs, inform consumers, and benefit the institution
incorporating information about PHRs into academic courses
helping implement patient portals that include PHRs
selecting and evaluating consumer health content to be included in personal health records
The task force's own suggestions for possible roles included:
coordinating with health information management professionals responsible for PHRs
assisting health care providers in adopting the use of PHRs
providing PHR vendors with information regarding the UMLS and how it can be integrated into PHRs
promoting the use of PHRs through consumer outreach efforts to build trust and acceptance
Training of librarians
The task force felt that any training or education provided to librarians needed to focus on building an awareness of PHRs and alerting librarians that they might be contacted for information as a result of the inclusion of the assistance statement in PHRs. For more formal education specifically related to awareness of the assistance statement, two presentation slides were developed and delivered for use in MLA-sponsored and NLM-sponsored courses that have a consumer health information focus.
CONCLUSIONS
The PHR field is very dynamic and rapidly evolving. Moore states, “The PHR market remains an elusive, challenging market to understand and predict its future outcome” [21]. Involving and empowering the patient are trends that will continue, not fads that will fade, as health care strives to be more patient centric. Whatever happens with the PHR market, the adoption of PHRs does create the possibility of new roles for health sciences librarians. PHRs will continue to evolve and will become more standardized as regulations and legislation governing them go into effect. These products will be required to meet standards for interoperability, transferability, and security. As the field further develops, there may be fewer vendors of PHRs; the smaller vendors may not be able to maintain a place in the market. Regardless of the number of vendors, as PHRs become more widely adopted, patients will be empowered by being better informed.
While non-tethered PHRs can be useful, PHRs are more powerful and beneficial when integrated with the EHR [22]. According to Halamka and colleagues, “The increasing prevalence of personal health records over the next five years will create many policy and technical challenges for healthcare institutions, payers, and employers. However, it may also provide a great opportunity” [23]. As patients seek assistance in enrolling in PHRs or in finding health information while using their PHRs, health sciences librarians will find that they have another venue for providing quality information for improved health.
Acknowledgments
For data collection and data entry, as well as development of the assistance statement, the authors thank their fellow task force members: Michael Ackerman, National Library of Medicine; Joan S. Ash, Oregon Health & Sciences University School of Medicine; Taneya Koonce, Vanderbilt University Medical Center Eskind Biomedical Library; David Sweet, American Health Information Management Association Library; Carla J. Funk, CAE, headquarters staff liaison, Medical Library Association; T. Scott Plutchak, AHIP, MLA Board of Directors liaison, 2008, and Lister Hill Library of the Health Sciences, University of Alabama at Birmingham.
Footnotes

This article has been approved for the Medical Library Association's Independent Reading Program <http://www.mlanet.org/education/irp/>.
REFERENCES
- 1.Deloitte Consulting, Deloitte Center for Health Solutions. 2008 survey of health care consumers: executive summary [Internet] Washington, DC: Deloitte; 2008 [cited 27 Aug 2009]. < http://www.deloitte.com/assets/Dcom-UnitedStates/Local%20Assets/Documents/us_chs_ConsumerSurveyExecutiveSummary_200208.pdf>. [Google Scholar]
- 2.Kaelber D.C, Shah S, Vincent A, Pan E, Hook J.M, Johnston D, Bates D.W, Middleton B. The value of personal health records [Internet] Charlestown, MA: Center for Information Technology Leadership; 2008 [cited 27 Aug 2009]. < http://www.citl.org/_pdf/CITL_PHR_Report.pdf>. [Google Scholar]
- 3.Coffield R.L, DeLoss G.E, Mooty G.P. The rise of the personal health record: panacea or pitfall for health information. Health Lawyers News. 2008 Oct;12(10):8–13. [Google Scholar]
- 4.Scherger J.E. Future vision: is family medicine ready for patient-directed care. Fam Med. 2009 Apr;41(4):285–8. [PubMed] [Google Scholar]
- 5.Kaelber D.C, Jha A.K, Johnston D, Middleton B, Bates D.W. A research agenda for personal health records (PHRs) J Am Med Inform Assoc. 2008 Nov–Dec;15(6):729–36. doi: 10.1197/jamia.M2547. DOI 10.1197/jamia.M2547. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Weitzman E.R, Kaci L, Mandl K.D. Acceptability of a personally controlled health record in a community-based setting: implications for policy and design. J Med Internet Res. 2009 Apr 29;11(2):e14. doi: 10.2196/jmir.1187. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.MLA/NLM Joint Electronic Personal Health Record Task Force update and survey—please participate! MLA-FOCUS [Internet] 2008 Feb 14 (special edition) [cited 27 Aug 2009]. < http://www.mlanet.org/members/mla-focus/2008/mla-focus-20080214sf.html>.
- 8.National Committee on Vital and Health Statistics, US Department of Health and Human Services, National Cancer Institute, National Institutes of Health, National Center for Health Statistics, Centers for Disease Control and Prevention. Personal health records and personal health record systems: a report and recommendations from the National Committee on Vital and Health Statistics [Internet] Washington, DC: The Committee; 2006 [cited 27 Aug 2009]. < http://www.ncvhs.hhs.gov/0602nhiirpt.pdf>. [Google Scholar]
- 9.Robert Wood Johnson Foundation. Project HealthDesign: rethinking the power and potential of personal health records: common platform [Internet] The Foundation [cited 28 Aug 2009] <http://www.projecthealthdesign.org/overview-phr/common_platform>.
- 10.Certification Commission for Healthcare Information Technology. Recommendations of the PHR Advisory Task Force: certification of PHRs [Internet] The Commission; 2008 [cited 27 Aug 2009]. < http://www.hitanalyst.files.wordpress.com/2008/07/cchitphratf.pdf>. [Google Scholar]
- 11.Friends of the National Library of Medicine. 2009 conference: video, speakers, presentations, and program: personal electronic health records: from biomedical research to people's health [Internet] The Friends; 2009 [cited 28 Dec 2009]. < http://www.fnlm.org/Events-2009-Conf.html>. [Google Scholar]
- 12.Mault J.R. Experiences with connected care [Internet] 20 May 2009 [cited 28 Aug 2009]. Presented at Friends of the National Library of Medicine 2009 Conference “Personal Electronic Health Records: From Biomedical Research to People's Health.” Microsoft Health Solutions Group; < http://www.fnlm.org/pdfs/May20/05_James_Mault.pdf>.
- 13.Spector A. Our search for great value in personal healthcare records [Internet] 20 May 2009 [cited 28 Aug 2009]. Presented at Friends of the National Library of Medicine 2009 Conference “Personal Electronic Health Records: From Biomedical Research to People's Health.” Google; < http://www.fnlm.org/pdfs/May20/06_Alfred_Spector.pdf>.
- 14.Department of Health and Human Services. For covered entities [Internet] The Department [cited 11 Dec 2009] < http://www.hhs.gov/ocr/privacy/hipaa/understanding/coveredentities/>.
- 15.Department of Health and Human Services. Agency information collection request; 30-day public comment request. Fed Regist. 2009 May 22;74(98):24012–3. [Google Scholar]
- 16.Federal Trade Commission. FTC issues final breach notification rule for electronic health information [Internet] The Commission; 17 Aug 2009 [cited 27 Aug 2009]. < http://www.ftc.gov/opa/2009/08/hbn.shtm>. [Google Scholar]
- 17.Randeree E. Exploring technology impacts of Healthcare 2.0 initiatives. Telemed J E Health. 2009 Apr;15(3):255–60. doi: 10.1089/tmj.2008.0093. [DOI] [PubMed] [Google Scholar]
- 18.National Library of Medicine. MedlinePlus [Internet] Bethesda, MD: The Library; 11 Dec 2009 [cited 11 Dec 2009]. < http://www.medlineplus.gov>. [Google Scholar]
- 19.Consumer and Patient Health Information Section, Medical Library Association. Top 100 list: health sites you can trust [Internet] The Section; Mar, < http://www.caphis.mlanet.org/consumer/>. [Google Scholar]
- 20.Reti S.R, Feldman H.J, Safran C. Governance for personal health records. J Am Med Inform Assoc. 2009 Jan–Feb;16(1):14–7. doi: 10.1197/jamia.M2854. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Moore J. iPHR Market Report. Cambridge, MA: Chilmark Research; 2008. Preface. [Google Scholar]
- 22.Tang P.C, Ash J.S, Bates D.W, Overhage J.M, Sands D.Z. Personal health records: definition, benefits, and strategies for overcoming barriers to adoption. J Am Med Inform Assoc. 2006 Mar–Apr;13(2):121–6. doi: 10.1197/jamia.M2025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Halamka J.D, Mandl K.D, Tang P.C. Early experiences with personal health records. J Am Med Inform Assoc. 2008 Jan–Feb;15(1):1–7. doi: 10.1197/jamia.M2562. [DOI] [PMC free article] [PubMed] [Google Scholar]