Abstract
Question:
Can an information prescription protocol be successfully integrated into a family medicine practice seeking to enhance patient education and self-management?
Setting:
Milton Family Practice, an outpatient clinic and resident teaching site of the University of Vermont and Fletcher Allen Health Care, is located in a semirural area fifteen miles from main campus.
Objectives:
The objectives were to increase physicians' knowledge and use of information prescriptions, sustain integration of information prescription use, and increase physicians' ability to provide patient education information.
Methods:
Methods used were promotion of the National Library of Medicine's Information Rx, physician instruction, installation of patient and provider workstations, and a collaborative approach to practice integration.
Main Results:
A post-intervention survey showed increased physician knowledge and use of the Information Rx protocol. Support procedures were integrated at the practice.
Conclusions:
Sustainable integration of Information Rx in a primary care clinic requires not only promotion and education, but also attention to clinic organization and procedures.
INTRODUCTION
An information prescription, a physician's direction to a patient to obtain further information on a health topic, has been proposed in various studies to enhance patient-physician communication, patient self-management, and patient education [1–4]. Patient-physician communication and patient self-management are considered important for managing chronic conditions as described in the chronic care model (CCM) [5]. Additionally, improved patient education increases patient safety according to Institute of Medicine reports [6].
Most Americans have access to the Internet at home, work, school, or public libraries, and more than 60% of all American adults use the Internet to seek health information [7]. Many look for health information online before they seek professional guidance. Despite this self-reliance, most people prefer to obtain information about health from their physicians and believe information from them to be more trustworthy than from other sources [7, 8]. These three factors—Internet availability, frequency of Internet use to find health information, and patient preference for information received from physicians—increase the likelihood that patients would follow a physician-directed information prescription with a recommended website, aiding in patient education and communication efforts.
In 2003, the National Library of Medicine (NLM) and the American College of Physicians Foundation (ACPF) developed an information prescription protocol predicated on high use of online health information and availability of a trustworthy consumer-oriented health information website: the National Institutes of Health/NLM website, MedlinePlus [9–11]. The Information Rx protocol described on the ACPF website includes these basic elements: the physician directs a patient to find information about a health-related topic and writes the topic on a prescription-like note preprinted with the name and uniform resource locator (URL) of the MedlinePlus website [10, 11]. The Information Rx toolkit, which can be ordered free from the NLM website, includes Information Rx prescription pads of various sizes, small MedlinePlus posters, information cards, and brochures [9]. The National Network of Libraries of Medicine (NN/LM) developed a related toolkit for medical librarians who use the Information Rx program in collaboration with physicians, medical practices, and public libraries [12].
In 2006, Siegel et al. published the results of two surveys evaluating the Information Rx protocol [4]. In a 2003 survey, a majority of American College of Physicians (ACP) members who had received and used the NLM/ACPF toolkit agreed that the Information Rx and MedlinePlus combination improved patient-physician communication and increased patient knowledge about a condition or treatment. In a second survey, conducted in 2005, patients who had received an Information Rx prescription responded positively when asked about their Internet use for health information and the value of a physician's recommendation of the website. These results suggested that the Information Rx contributed to effective patient education and improved communication between patient and physician. The study also suggested that the protocol would be used and accepted by physicians [4].
SETTING
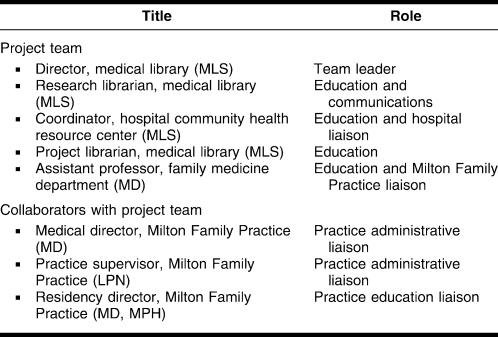
This case study describes a collaboration between the University of Vermont (UVM) Dana Medical Library and College of Medicine (COM) Family Medicine Department (FMD), the Frymoyer Community Health Resource Center (FCHRC) at Fletcher Allen Health Care (FAHC), the UVM affiliated teaching hospital, and Milton Family Practice (MFP). An outpatient clinic and resident teaching site in Vermont, MFP was the primary setting for the project. Located in a semirural area removed from the main campus, MFP is a clinical site of FAHC. The participant population included ten attending physicians, eighteen residents, and fifteen nursing and medical office staff. The medical director (a physician) and the practice supervisor (a nurse) from MFP were the primary collaborators with the project team. The project team included three medical librarians (UVM library faculty), a physician member of FMD and former clinician at MFP, and the coordinator (also a medical librarian) of FCHRC at FAHC (Table 1). The library and COM faculty members of the team provide hospital- and clinic-related services but are not hospital employees. The project was funded by an outreach subcontract from the NN/LM, New England Region, from April 2007 to June 2008.
Table 1.
Project team and collaborator roles
OBJECTIVES
The project's objectives were to:
increase physicians' knowledge and use of the NLM/ACPF Information Rx protocol,
integrate the Information Rx protocol and MedlinePlus consumer health information into the medical practice in sustainable ways within the capabilities and policies of the practice, and
increase physicians' ability to provide relevant patient education information during an office visit.
The project team hypothesized that with education and collaboration, physicians would accept and use the Information Rx protocol and increase recommendations of MedlinePlus.
METHODS
Planning
Initial meetings between the project team and the MFP medical director, practice supervisor, and director of resident education established mutual interest in the project, outlined possible activities, and clarified goals. The FMD was incorporating aspects of CCM into its resident training and outpatient clinics at the time the project was beginning. CCM emphasizes improved patient education in managing chronic conditions, such as hypertension and diabetes, and the importance of patient-physician communication centered on patient needs. According to the model, when patient knowledge and two-way communication improves, the patient and physician are activated to manage the condition effectively together [13, 14]. The project team and practice leaders identified the Information Rx protocol as a step toward reaching the practice's education, communication, and patient-empowerment goals in keeping with CCM. Specific activities were planned to reach project goals:
education of physicians and medical office staff through classes, meetings, and consultations conducted by team members;
distribution and display of informational materials about MedlinePlus and Information Rx at the practice; and
distribution of preprinted Information Rx tear-off pads to all physicians and access to pads in each exam room.
In the planning meetings, the project team learned that physicians had little time to provide patient education even though it was required by hospital policy. Keeping the practice's patient education handout collection current was a recognized problem. Earlier investigation by a resident had indicated that physicians seeking current online information lacked timely access to a computer and printer because of competing clinical demands on the computers. An improved method of finding and delivering online patient education information was desired. Practice leaders also raised concerns that some patients did not have adequate Internet access or the health literacy to use the Internet for health information. In response to these concerns, intervention activities were added that included:
installation of a dedicated search-only, Internet-accessible computer and printer for physicians to identify and print patient education information; and
installation of a second workstation for patients to use to fill information prescriptions.
Intervention
Following planning and a pre-intervention survey, the intervention activities were conducted over eight months, from December 2007 through July 2008. The project team developed and presented a class intended for both attending and resident physicians. Invitations to attend group or individual educational sessions were extended to all physicians. Using hands-on computing exercises, the class highlighted features of MedlinePlus that are especially relevant to primary care, such as chronic disease management, alternative and conventional drug therapies, and audiovisual tools. The availability of both low-literacy and research-level information in MedlinePlus was emphasized in response to concerns raised by some physicians. The comprehensiveness of MedlinePlus, its use of evidence-based information, and its commercial-free nature were also emphasized. All physicians received emails explaining the project and giving directions on the components of the Information Rx protocol and the location of Information Rx tear-off pads. Staff education was presented both at a staff meeting early in the project and at a lunchtime table discussion at MFP midway through the project.
The bulletin board displays, including Information Rx posters and MedlinePlus brochures, were posted in eighteen exam rooms in large formats for six months and later in smaller displays that remain in place as of this writing (December 2009). Displays were intended to prompt both physicians and patients to consider MedlinePlus a credible health information source and to encourage physicians to use Information Rx pads during office visits.
A computer workstation and printer were installed for physicians to use solely for the purpose of finding online evidenced-based resources. A patient-use computer and a telephone with a dedicated line to FCHRC were installed in a clinic area to meet patient information needs. Signs advertising the computer for patient use were posted in exam rooms and the waiting room. Both computer installations required extensive technical collaboration and negotiation with the affiliated hospital information technology (IT) department regarding connectivity, access level, and security. The IT department, project team, and MFP collaborators agreed that both computers would have search-only Internet access outside the hospital firewall. The safety and privacy of patients, including Americans with Disabilities Act requirements, were considered in the choice of furniture and room ambience. Signs directed patients needing assistance to use the dedicated telephone line to contact FCHRC. Office staff agreed to keep the printer paper stocked and help with basic technical questions, but not with information access or retrieval questions. Regular meetings and negotiation with the medical director and practice supervisor were needed to resolve these intervention details. The project team developed an information binder for the practice supervisor to ensure continuity after the project ended. It contained samples and directions for ordering toolkit items, the URL for downloading MedlinePlus brochures, troubleshooting information for the computers, and background on the project.
Evaluation
Dana Medical Library's standard education evaluation form was used to assess the quality of the teaching and the content and usefulness of the class. No formal assessment was conducted of the limited staff education programming. Project team members used the NN/LM subcontract outreach activity data collection form to record all interactions with physicians, medical office staff, practice leaders, and FAHC officials. Collaboration activities such as planning meetings, presentations at scheduled provider and staff meetings, individual consultations, and IT-related interactions were entered and described on the form.
The project team modified a questionnaire developed by Schifferdecker et al., Dartmouth College, that assessed physicians' knowledge and use of professional and consumer online resources [15]. The modified questionnaire asked for the physicians' level of knowledge of consumer health websites including MedlinePlus, knowledge of the Information Rx protocol, and ability to provide patient education information during an office visit (Appendix, online only). The responses to questions were made on a 5-point Likert scale. Institutional review board approval to conduct the surveys and collect data was sought and granted. The pre-intervention questionnaire was distributed to clinic mailboxes and at resident group meetings. The same questionnaire was administered at the end of the project period with the addition of questions on the frequency of use of the Information Rx pad and frequency of a MedlinePlus recommendation. Physicians identified themselves as either attending or resident physicians. An attempt was also made to survey nurses and medical office staff, but few questionnaires were returned from this group and were not analyzed in this study.
Because the survey data were not linked to individual respondents, the survey results provide a snapshot of physicians' knowledge and behavior at the practice at two points in time rather than results for a specific sample of physicians. Some physicians who had been present for the intervention completed their residency training and left the practice prior to the post-intervention survey. Other attending physicians and residents might have responded to the second survey only.
RESULTS
Education results
Twelve of eighteen family medicine residents attended the fifty-minute class taught by project team librarians. The residents' evaluations gave high ratings and positive comments about the features and utility of MedlinePlus. No attending physicians from the study population attended a scheduled group class. However, three attending physicians did receive individual sessions at their offices, and the project team gave brief presentations at two monthly provider meetings.
Collaboration results
Over the project's planning and active intervention periods, 148 direct contacts with physicians, medical office staff, or practice leadership were documented on the NN/LM reporting form. The Information Rx and NN/LM librarians' toolkits were heavily used in the collaboration. The project team ordered and reordered prescription pads, posters, and information cards, and they distributed hundreds of pads to meet the demand from project participants and other providers who had heard about the project. The team also printed and distributed more than 1,000 copies of a MedlinePlus tri-fold brochure used in the exam room displays. Medical office staff monitored and replenished the bulletin board displays and prescription pads. Each of the promotion steps was discussed with and approved by the clinic leadership.
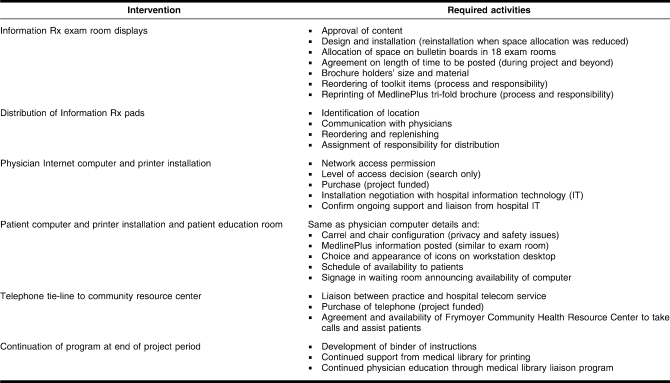
The level of detail required to collaborate successfully and the implementation steps required to meet project objectives were not anticipated at the planning stage. A chart describing many of the detailed activities of the intervention is shown in Table 2. NN/LM reporting form notes indicated that the FCHRC coordinator (a hospital employee) played a key role in accomplishing the networked computer technology interventions by facilitating communication between the practice office staff and hospital IT manager. The former practice physician on the team overcame communication hurdles and found solutions to policy and protocol issues at the practice.
Table 2.
Required activities for Information Rx clinic intervention
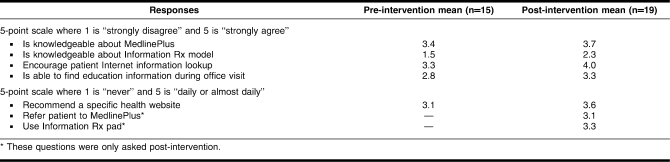
Survey results
Fifteen of twenty-eight (54%) physicians responded to the pre-intervention survey, and nineteen (68%) responded to the post-intervention survey. Table 3 shows a summary, reported as means, of physicians' changes in knowledge and attitude toward online consumer health information, as well as their use of MedlinePlus and the Information Rx protocol. The results show changes in overall knowledge and behavior. Key findings related to the objectives include:
Table 3.
Results of physician survey on knowledge, attitude, and use of Information Rx and MedlinePlus
Pre-intervention, 47% (7/15) of physicians reported themselves as knowledgeable or having detailed knowledge about MedlinePlus, compared to 58% (11/19), post-intervention.
Pre-intervention, 27% (4/15) recommended a specific health information website to patients weekly or daily/almost daily, compared to 63% (12/19), post-intervention.
Pre-intervention, 53% (8/15) agreed or strongly agreed with encouraging patients to look up health information on the Internet, versus 84% (16/19), post-intervention.
Pre-intervention, 13% (2/15) reported knowledge or detailed knowledge of the Information Rx protocol, compared to 42% (8/19), post-intervention.
Pre-intervention, 33% (5/15) reported they could find education materials during a patient office visit well or extremely well, compared to 42% (8/19), post-intervention.
In the post-intervention survey, 2 questions were added regarding frequency of physician use of the Information Rx protocol. Regarding MedlinePlus, 42% (8/19) reported referring patients to the website weekly or daily/almost daily, 16% (3/19) reported monthly use, and 42% (8/19) reported rarely or never referring patients to it. On use of the Information Rx prescription pad, 47% (9/19) reported weekly or almost daily use, 26% (5/19) reported using it once or twice a month, and 26% (5/19) said they rarely or never used it. In a comment, one cited the low literacy level of patients as a reason for not using the protocol.
Many physicians reported lack of time as a barrier to using Internet health information with patients, pre- and post-intervention. Pre-intervention, 93% (14/15) agreed or strongly agreed that lack of time interfered with their use of consumer health information, and 95% (18/19) agreed or strongly agreed with it, post-intervention. A minority of physicians felt that lack of an easily accessible computer or printer was a barrier to using consumer health information with patients. Pre-intervention, 20% (3/15) of physicians agreed or strongly agreed that lack of easy access to an Internet accessible computer was a barrier, and 40% (6/15) agreed that lack of a printer was a barrier. Post-intervention, 32% (6/19) agreed or strongly agreed that lack of a computer was a barrier and 37% (7/19) agreed that lack of a printer was a barrier.
DISCUSSION
While the project team had thought that teaching classes to the study population would constitute the majority of project time and effort, this did not prove to be the case. Fewer classes than anticipated were held because attending physicians reported they did not have the time to attend them. Instead, extensive time and effort went into developing and managing the medical office system processes. Implementing the Information Rx protocol was a complex process and required more organization than the seeming simplicity of the protocol or the NLM and ACPF process toolkits had suggested. In a follow-up to another Information Rx implementation, Leisey and Shipman found that physicians intended to use the protocol but left out steps such as giving the written information prescription or directing patients to use it [16].
In this case study, reinforcement through prescription pad distribution, exam room postings, and class attendance might have contributed to acceptance and regular use of the Information Rx protocol by clinic physicians. Reaching agreement with the clinic supervisor on these process details was essential to successful implementation. Despite the uneven education participation and collaboration hurdles, the survey showed that more MFP physicians regularly recommended a consumer health website to patients and reported confidence in their ability to find patient information during an office visit after the intervention. Nearly half of the physicians reported using the Information Rx pad weekly or daily. The added physician computer and printer access had little impact pre- or post-intervention on use of consumer health information with patients according to the survey. However, several physicians reported in conversation that this computer was heavily used and appreciated.
The collaborators in the project planning stage considered participation in the project by clinic staff important, but it proved difficult to accomplish. A proposal for MFP staff to direct patients receiving an information prescription to the patient computer was considered but then rejected by the practice supervisor owing to time, training, and job classification concerns. Another approach considered was to have a librarian project team member present at the practice two afternoons a week to help patients fill information prescriptions. This approach was deemed too time intensive to be sustainable. The dedicated telephone line to the FCHRC was installed as the alternative. This telephone and the patient computer were installed in a room adjacent to the clinical area, instead of in the patient waiting area itself. The room turned out to be less accessible to patients than anticipated, and few patients utilized it during the intervention period.
Physicians continued to believe that there was not enough time for patient education after the intervention. Although disappointing, this perception was not surprising. Studies by Abbo et al. [17] and Tarn et al. [18] showed that many physicians believed patient education took up time during visits that are already compressed by the number of tasks to be completed. Based on this experience, most physicians will not consider the Information Rx protocol a time saver. The lack of nonphysician medical staff participation in the Information Rx protocol might have affected physicians' perception of having insufficient time. More involvement by staff in patient communication about availability of Internet health information might have lessened the physicians' time concerns.
IMPLICATIONS
Some primary care practices are incorporating the patient-centered medical home (PCMH) model (an outgrowth of CCM) for improving outcomes of chronic conditions in primary care practices. This model relies on a care team, not just the physician, to manage conditions, enhance patient education, and coordinate care [19, 20]. The care team involves nurses, medical assistants, mental health practitioners, and others actively communicating educational information and receiving feedback from patients. Information Rx could be an appropriate addition to this kind of team-based approach, wherein physicians and medical staff share responsibility for patient education. In a clinic with frequent personnel changes, education and promotion of the protocol would need to be continuous.
A medical librarian could be involved in implementing information prescriptions in a PCMH model through planning, education of care-team members, and participation in the care team. A PCMH pilot underway at another UVM-affiliated clinic (not a resident training site) has incorporated several of the processes developed in this project, including education of physicians, nurses, and other medical staff on the Information Rx protocol and MedlinePlus and installation of a patient Internet computer in the waiting room. In this pilot, medical librarians were involved in the development and education stages but not in the direct provision of information services to patients. A medical librarian as a mediator of information prescriptions with patients may be possible in some settings, but further study is needed to test the feasibility and sustainability of this role.
CONCLUSION
The Information Rx protocol provides a methodology to increase use of information prescriptions and online consumer health information. The NLM and ACPF toolkits and support are helpful but not sufficient to assure acceptance and use by physicians and organizations. Education, process development, and practice organization frameworks are needed to assure continuing use of the protocol. Institutional practices and policies must be considered for an information prescription implementation to gain acceptance in a medical group. Where information prescriptions are integrated in PCMH or CCM practice settings with a care team approach, they could be a valuable tool for improved patient education and communication.
Electronic Content
Acknowledgments
The authors thank the physicians and staff at Milton Family Practice and give special thanks to Office Supervisor Holly Van Winkle, Medical Director John Ferguson, Residency Director John King, and Amy Danielson. We also thank Pam Farnham, manager, Adult Outreach Services, Community Health Improvement, Fletcher Allen Health Care, and Susan Bishop, administrative assistant, Dana Medical Library, for assistance with the project and manuscript.
Footnotes
This project has been funded in part with federal funds from the National Library of Medicine, National Institutes of Health, Department of Health and Human Services, under contract no. N01-LM-6-3508 with the University of Massachusetts Medical School.
Preliminary results of this project were presented as a poster at MLA '08, the 108th Annual Meeting of the Medical Library Association; Chicago, IL; May 19, 2008.
Additional findings were presented at the Society of Teachers of Family Medicine (STFM) “Conference on Practice Improvement”; Savannah, GA; December 5, 2008.
A supplemental appendix is available with the online version of this journal.
REFERENCES
- 1.Williams M.D, Gish K.W, Giuse N.B, Sathe N.A, Carrell D.L. The Patient Informatics Consult Service (PICS): an approach for a patient-centered service. Bull Med Libr Assoc. 2001 Apr;89(2):185–93. [PMC free article] [PubMed] [Google Scholar]
- 2.D'Alessandro D.M, Kreiter C.D, Kinzer S.L, Peterson M.W. A randomized controlled trial of an information prescription for pediatric patient education on the Internet. Arch Pediatr Adolesc Med. 2004 Sep;158(9):857–62. doi: 10.1001/archpedi.158.9.857. [DOI] [PubMed] [Google Scholar]
- 3.Ritterband L.M, Borowitz S, Cox D.J, Kovatchev B, Walker L.S, Lucas V, Sutphen J. Using the Internet to provide information prescriptions. Pediatrics. 2005 Nov;116(5):e643–7. doi: 10.1542/peds.2005-0404. [DOI] [PubMed] [Google Scholar]
- 4.Siegel E.R, Logan R.A, Harnsberger R.L, Cravedi K, Krause J.A, Lyon B, Hajarian K, Uhl J, Ruffin A, Lindberg D.A. Information Rx: evaluation of a new informatics tool for physicians, patients, and libraries. Inf Serv Use. 2006;26(1):1–10. doi: 10.3233/isu-2006-26101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Wagner E.H, Austin B.T, Von Korff M. Organizing care for patients with chronic illness. The Milbank Q. 1996;74(4):511–44. [PubMed] [Google Scholar]
- 6.Committee on Quality of Health Care in America, Institute of Medicine (US) Crossing the quality chasm: a new health system for the 21st century. Washington, DC: National Academies Press; 2001. [Google Scholar]
- 7.Fox S, Jones S. The social life of health information: Americans' pursuit of health takes place within a widening network of both online and offline sources [Internet] Washington, DC: Pew Research Center; 2009. [rev. Jun 2009; cited 8 Dec 2009]. < http://www.pewinternet.org/∼/media//Files/Reports/2009/PIP_Health_2009.pdf>. [Google Scholar]
- 8.Hesse B.W, Nelson D.E, Kreps G.L, Croyle R.T, Arora N.K, Rimer B.K, Viswanath K. Trust and sources of health information: the impact of the Internet and its implications for health care providers: findings from the first Health Information National Trends Survey. Arch Int Med. 2005 Dec 12–26;165(22):2618–24. doi: 10.1001/archinte.165.22.2618. [DOI] [PubMed] [Google Scholar]
- 9.National Library of Medicine. Information Rx [Internet] The Library [cited 3 Aug 2009]. < http://www.informationrx.org>.
- 10.American College of Physicians Foundation. Information Rx: a joint project of the ACP Foundation and the National Library of Medicine [Internet] The Foundation [rev. 2009; cited 5 Aug 2009]. < http://www.foundation.acponline.org/hl/inforx.htm>.
- 11.National Library of Medicine, National Institutes of Health. MedlinePlus: trusted health information for you [Internet] The Library [rev. 2009; cited 5 Aug 2009]. < http://www.medlineplus.gov>.
- 12.National Network of Libraries of Medicine. Health sciences libraries Information Rx tool kit [Internet] The Network [rev. 2009; cited 5 Aug 2009]. < http://www.nnlm.gov/hip/infoRx/placeorder.html>.
- 13.Bodenheimer T, Wagner E.H, Grumbach K. Improving primary care for patients with chronic illness: the chronic care model, part 2. JAMA. 2002 Oct 16;288(15):1909–14. doi: 10.1001/jama.288.15.1909. [DOI] [PubMed] [Google Scholar]
- 14.Wagner E.H, Austin B.T, Davis C, Hindmarsh M, Schaefer J, Bonomi A. Improving chronic illness care: translating evidence into action. Health Aff. 2001 Nov/Dec;20(6):64–78. doi: 10.1377/hlthaff.20.6.64. [DOI] [PubMed] [Google Scholar]
- 15.Schifferdecker K, Reed V, Homa K. A training intervention to improve information management in primary care. Fam Med. 2008;40(6):248–57. [PMC free article] [PubMed] [Google Scholar]
- 16.Leisey M.R, Shipman J.P. Information prescriptions: a barrier to fulfillment. J Med Libr Assoc. 2007 Oct;95(4):435–8. doi: 10.3163/1536-5050.95.4.435. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Abbo E.D, Zhang Q, Zelder M, Huang E.S. The increasing number of clinical items addressed during the time of adult primary care visits. J Gen Intern Med. 2008 Dec;23(12):2058–65. doi: 10.1007/s11606-008-0805-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Tarn D.M, Paterniti D.A, Kravitz R.L, Heritage J, Liu H, Kim S, Wenger N.S. How much time does it take to prescribe a new medication. Patient Educ Couns. 2008 Aug;72(2):311–9. doi: 10.1016/j.pec.2008.02.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.American Academy of Family Physicians. Patient-centered medical home [Internet] The Academy [rev. 2009; cited 27 Jul 2009]. < http://www.aafp.org/online/en/home/membership/initiatives/pcmh.html>.
- 20.American Academy of Family Physicians, American Academy of Pediatrics, American College of Physicians, American Osteopathic Association. Joint principals of the patient-centered medical home [Internet] Washington, DC: Patient-Centered Primary Care Collaborative; 2007 [cited 9 Dec 2009]. < http://www.pcpcc.net/content/joint-principles-patient-centered-medical-home>. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.