Abstract
Bolus calculators are effective tools in controlling blood glucose levels in patients treated with insulin. Diabetics is a new software devised for patients to facilitate and improve self-managing for prandial insulin dosing and for better controlling food intake. This device contains two integral parts: a nutrition database and a bolus calculator. The algorithm is based on a formula in which carbohydrate (CHO) and either fat and/or protein (FP) products are engulfed in insulin. The insulin dose setting is programmed individually for CHO in a normal bolus (N-W) and for FP in a square-wave bolus (S-W). The device calculates the dose of insulin for N-W or S-W, suggests the optimal kind of bolus, and indicates the timing in hours for an S-W bolus. In addition, this calculator, which contains a nutrition database and insulin dosing software, helps determine the correct type of necessary boluses for selected foods.
Keywords: bolus calculator, insulin pump, type 1 diabetes
Introduction
Continuous subcutaneous insulin infusion (CSII) provides a convenient method for insulin self-dosing for patients with diabetes.1,2 Many clinical studies have shown that CSII can improve metabolic control, decrease the risk of severe hypoglycemia, and improve a patient's quality of life.3–5 Although the use of CSII has the many advantages just listed, failure of that therapy, resulting in poor metabolic control, has also been observed. The most common documented reasons for high levels of glycosylated hemoglobin are as follow: missing prandial boluses and/or faulty programming of the dose or of the type of bolus for a particular meal.6–8 Programming functions depend solely on the educated patient and his/her compliance. Calculation of an insulin dose is a complex process in which numerous factors, such as the preprandial glucose level, grams of carbohydrate (CHO), insulin sensitivity expressed as an insulin-to-CHO ratio,9 and active insulin on board, should be taken into account. Inappropriate calculation of these factors can lead to either under- or overdosing of prandial insulin,10 resulting in unexpected glucose fluctuations. Therefore, bolus calculators have been developed for patients treated with insulin as a valuable tool in facilitating insulin adjusting.
Warsaw Pump Therapy School (WPTS) New Procedures in Programming Mealtime Insulin
In 2003, a new original procedure of using dual-wave (D-W)/square-wave (S-W) boluses was developed by the authors in the Department of Pediatrics of the Medical University of Warsaw, Poland. This procedure is based on three main assumptions:
Meals containing fat and/or proteins, such as carbohydrate products, should be covered in insulin.
Time of meal absorption depends on the type of nutrition product, for example, rich-in-fat meals are absorbed longer.
The insulin dose should be programmed individually for carbohydrate products in a normal-wave (N-W) bolus and in a S-W bolus for fat/protein (FP) food ingredients.11
A new fat–protein unit (FPU)-exchange factor was added to the food-counting system—defined as 100 kcal of fat and/or protein foods. In addition, it was established empirically that the dose of insulin in a N-W bolus should be calculated from the number of carbohydrate units (CU), whereas the dose for the S-W bolus is the number of FPU multiplied by the insulin ratio (IR), a dose of insulin that covers 10 grams of CHO product or 100 kcal of FP products. The total dose of insulin calculated for a meal is the sum of the insulin dose in N-W and S-W boluses. A new procedure, based on empirical observations, was also developed to establish the time length for S-W boluses programmed for 3 hours or longer, providing that the food was rich in fat. The time length was established to be 3 hours for a meal containing 1 FPU, 4 hours for 2 FPU, 5 hours for 3 FPU, and, finally, 8 hours if a meal included more than 3 FPU (300 kcal).12
The goals and aims of the WPTS for dosing mealtime insulin in pump therapy are to establish a form of education for patients using an insulin pump. Patient's training in food counting and in proper dosing of insulin takes place in an outpatient clinic and includes two 1.5-hour-long meetings in groups of one to three families under a doctor's supervision. The supervised meetings include a theoretical explanation of a healthy diet, type of nutrition products, and the absorption process dependency upon the type of food and its impact on the postprandial glycemic profile. Moreover, during these informative sessions, patients are trained to calculate the number of CU and FPU themselves, adjust the type of bolus to a specific meal, and program the time length of the S-W bolus, among others.
Theoretical Concept of Prandial Insulin Dosing Developed for Diabetics Software
According to the Dose Adjusting for Normal Eating program and many others in centers for children and adolescents with type 1 diabetes, the correct prandial insulin dose is the individual's IR multiplied by the amount of CHO intake, expressed by exchange/portions of 10 CHO or CU.9,13 In this method, only the amount of CHO forms the basis of insulin dosing. Unfortunately, there are no strict guidelines regarding the FP food content as determining factors of insulin adjustment. However, it is well established that a high FP meal leads to prolonged hyperglycemia. One example of such a high FP in a meal is pizza. Both Jones and colleagues14 and Lee and associates15 found that for a such high fat meal, the D-W achieves postprandial glycemic control most effectively. Directives of the Diabetics program are based on the assumptions developed by the WPTS.12,16 The Diabetics system calculates proper insulin doses, not only for CU, but also for fat/protein products as FPU. In order to standardize terms associated with this food-counting system, CU was defined as 10 grams of CHO product, and a new term—FPU—was defined as the equivalent of 100 kcal of fat and/or protein foods.11 The individual insulin sensitivity, expressed by IR, is used for CU as well as for FPU. Comparing two methods (a standard method to the WPTS method) of calculation of the prandial dose and the type of insulin bolus for a mixed meal will lead to two different conclusions (Table 1). In the WPTS method presented in this article, as compared to a traditional carbohydrate-counting method, the D-W should be programmed in such a way to deliver 5 additional units of insulin. The difference of 5 additional units of insulin of the WPTS method, which we consider an advantage over the traditional method, includes additional factors in the amount of proteins and fats in a dose in the form of the S-W. The Diabetics software counts CHO or CU, FPU, and calorie contents of every meal. When the IR is introduced into the WPTS formula, the dose of insulin is programmed and adjusted automatically. Moreover, Diabetics is the first software that includes the original WSPT algorithm for a time length for an extended bolus, as well as providing user-friendly suggestions for the type of bolus needed (i.e., N-W, D-W, or S-W).
Table 1.
(A) Nutrition Meal Data and (B) Prandial Insulin Calculation
| A. | ||||||
|---|---|---|---|---|---|---|
| Product | kcal | CHO | Fat | Protein | CU | FPU |
| 100 g boiled rice | ||||||
| 130 g fried salmon | 633.3 | 34.9 | 42.4 | 30.4 | 3.5 | 5 |
| 40 g lettuce | ||||||
| B. | ||||
|---|---|---|---|---|
| CU | FPU | Insulin ratio | Total insulin dose and type of bolus, according to standard method | Total insulin dose and type ofbolus, according to the WPTS |
| 3.5 | 5 | 1 IU/10 g CHO | 3.5 IU in BNa | 8.5 IU of D-W: 3.5 IU in BN 5 IU in S-W for 8 h |
Bolus normal.
A Description of the Diabetics Program
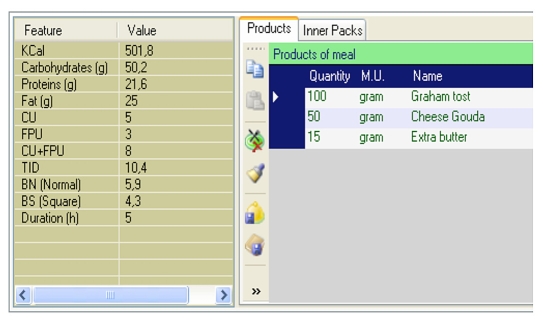
The Diabetics system consists of two integrated parts: the nutrition database software and the bolus calculator. A list of specific food products can be extended by each individual user to satisfy their therapeutic needs. Currently, this database includes products with posted nutritional information, such as caloric value (kilocalories) and the amount of CHO, as well as the FP content per 100 grams of a given food product (Figure 1).
Figure 1.
An example of calculating a created meal using the Diabetics software. BN, bolus normal; BS, bolus square; TID, total insulin dose.
The Diabetics devise facilitates mixing food ingredients and composition of any complex meal with parameters of quantity and content and permits saving and later retrieval of this information. When the user chooses a specific product, the user can choose a specific type of unit and conversion factor (e.g., one glass = 200 ml).
An insulin dose calculated for a meal depends primarily on the quantity and the kind of food but also on the preprandial glucose level and his/her personal IR. The disadvantage of the Diabetics software is that it does not consider either the target glucose level or the insulin sensitivity in its measurements. Its calculations depend solely on CU and FPU information. The Diabetics software recalculates meal parameters if the user changes his/her meal content. Subsequently, the final Diabetics calculation is performed using the person's own IR.
Algorithm of Prandial Insulin Calculation
The algorithm is composed of four parts (Table 2):
Table 2.
Algorithm of Prandial Insulin Calculation
| Part of algorithm | Calculation of CU and FPU total number for a meal | CU and FPU rounding for calculation | Calculation of insulin dose and type of boluses. IR factor for specific meal time | Calculation of time length (T) of bolus square delivery |
|---|---|---|---|---|
| Description | CU = carbohydrates/10FPU = (protein * 4.0 + fat * 9.0)/100, where carbohydrates – total amount of CHO in the meal protein – total amount of protein in the mealfat – total amount of fat in the meal | Half-piece method (default) – calculated value is rounded to whole or half unit with relation to:
|
CDI – total insulin dose CDI = (CU + FPU) * IRFactor CU _perc (percentage chare in CU + FPU)—technical information used in calculation of bolus type and extended time
CU _perc = CU/(CU + FPU)
BN (bolus normal)
|
|
Part 1: Calculation of the CU and FPU total for a particular meal
Part 2: CU and FPU rounding to facilitate further calculations
Part 3: Calculation of the needed insulin dose and type of boluses. The IR factor for a specific meal is used in this equation
Part 4: Calculation of the time length of bolus square-wave delivery
Working with Diabetics Program
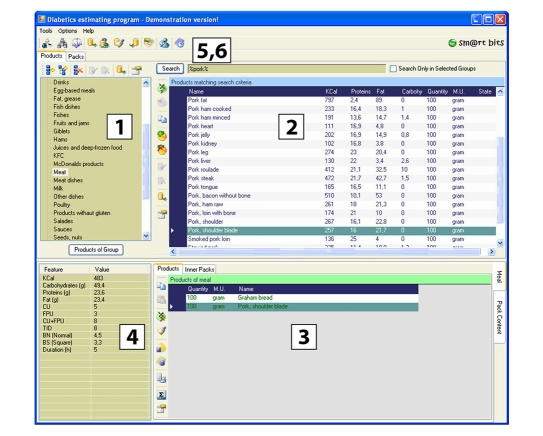
The Diabetics software is available online at www.diabetics.pl in two language versions: Polish and English. Before downloading the software, potential users must check their own computer and hardware requirements (Table 3). This software is designed for a Windows operating system. After downloading and installing the program, it is necessary to choose a software icon and install it onto the desktop. The main window of application is divided into subareas (Figure 2).
Table 3.
Computer Parameters Required for Downloading of Diabetics Software
| Hardware requirements | ||
|---|---|---|
| Version | Desktop | |
| Computer type | PC | Pocket PC, SmartPhonea |
| Hard disk operating system | Windows: 98, XP, Vista | Windows Mobile 2003 or newer (5.0;6.x) |
| Processor | Minimum 400 MHz | ARM |
| Internal memory | Minimum 64 MB | Minimum 64 MB |
For a tool such as the SmartPhone the operating system has to be Professional.
Figure 2.
Main window of the Diabetics software. (1) Product or pack group hierarchy—listed data depend on the active tab (products or packs). (2) Search results—list of elements (product or packs) matching given search criteria. Element type depends on the active tab (products or packs). (3) Meal or selected pack content (products and inner packs)—detailed information about a meal or selected pack content (from search results). (4) Meal or selected pack calculations—detailed calculations for meal or selected pack. (5) Main menu and toolbar—group functions for managing units of measurement, data exporting and importing, managing archive data, managing user-sensitive data, application help, and program information. (6) Search bar—allows the user to define product or select search criteria. BN, bolus normal; BS, bolus square; TID, total insulin dose.
Advantages and Disadvantage of the Diabetics System
This system was created to optimize prandial insulin dosing by calculating nutrition product data accurately and adjusting insulin dosages for all meal components accurately, including FP. With this user-friendly program, patients receive quick information about the amounts of CU and FPU, these types of boluses, and the proportion of insulin dose. This software thereby serves two purposes: normalizes (1) patient's daily blood glycemic profile and (2) patient's proper weight watch. The software facilitates calculation of insulin doses to satisfy different types of food and extends into an individually selected diet, without any danger of unexpected deterioration of the postprandial glycemia profile.
The Diabetics program can be adapted to prandial insulin programming options, available in new types of insulin pumps. In addition, this software, when used with insulin delivery devices, such as pens or pumps, permits minute adjustments of the insulin delivery rate to match the rate of food absorption, which depends on many factors, including the food fat content. To our knowledge, the Diabetics system is the first insulin bolus dose calculator that suggests the optimal type of bolus for a created meal, as well as the necessary period of time that an extended bolus is needed to cover a particular type of food. A helpful feature of this software is its availability and flexibility, as it can be downloaded from the Web site and installed into a variety of personal computers or pocket personal computers. In comparison to other bolus calculators, the consideration of total calorie intake, as well as protein-type calories, fat-type calories, and carbohydrate-type calories, is very useful for persons with other metabolic challenges in which diet and measurement of caloric intake are necessary measurements, e.g., during both low-calorie and high-calorie diets. Integration of a food database and a bolus calculator makes it a valuable diet education tool. It facilitates proper calculation of an insulin dose necessary for all three different types of food. Patients who are informed using this software tool have an opportunity to choose a self-selected and individually adopted diet without deterioration of their postprandial glycemia profiles.
The disadvantages of the Diabetics system, when compared to other bolus calculators, are that this system does not take into account the patient's current blood glucose level, the target blood glucose level, and the duration of insulin action and it does not calculate the correction dose. Its main function, however, is to adjust insulin dosing to prevent postprandial hyperglycemia. Comparing Diabetics to the standard method in calculating the prandial insulin bolus dose, Błazik and colleagues17 noticed significantly lower postprandial glycemia values after every main meal in the Diabetics group. For a reason of not having two different readouts, the WPTS recommends that this software not be incorporated into other prandial insulin dose calculators during insulin pump therapy. The authors are in their final research stage of safety of the Diabetics program.
Summary
The increasingly frequent use of CSII therapy faces the potential problem associated with programming mealtime bolus doses by pump users. The Diabetics system addresses that problem by assisting patients in making educated decisions regarding necessary bolus doses. This novelty software system indicates the types of boluses—as well as the amount of time length—needed to deliver an extended bolus for meals designed even by the most creative users. When meal calories are known a priori for a given meal, this calculator is helpful in controlling a patient's body weight. The Diabetics program is to be used by health professionals and educators, as well as by the diabetic patients themselves, who are often challenged by classifying foods according to their caloric or ingredients compositions and who have problems with adjusting proper insulin dosages. This product will satisfy patients' therapeutic needs, as well as provide valuable readings for the diabetes team dealing with insulin pumps. The authors made a special effort in designing the program so that it will make the younger generation comfortable using this life-saving device in their daily routine and who will embrace this new type of product with enthusiasm. The authors understand and wholly support further evaluation and improvements of the Diabetics software, including more clinical trials, more objective evidence of the algorithm safety, and more input from its users.
Acknowledgment
We thankfully acknowledge computer analyst Mariusz Florek for his outstanding technical support.
Abbreviations
- CHO
carbohydrate
- CSII
continuous subcutaneous insulin infusion
- CU
carbohydrate unit
- D-W
dual wave
- FP
fat/protein
- FPU
fat–protein unit
- IR
insulin ratio
- N-W
normal wave
- S-W
square wave
- WPTS
Warsaw Pump Therapy School
References
- 1.Pickup J, Keen H. Continuous subcutaneous insulin infusion at 25 years: evidence base for the expanding use of insulin pump therapy in type 1 diabetes. Diabetes Care. 2002;25(3):593–598. doi: 10.2337/diacare.25.3.593. [DOI] [PubMed] [Google Scholar]
- 2.Danne T, Battelino T, Jarosz-Chobot P, Kordonouri O, Pánkowska E, Ludvigsson J, Schober E, Kaprio E, Saukkonen T, Nicolino M, Tubiana-Rufi N, Klinkert C, Haberland H, Vazeou A, Madacsy L, Zangen D, Cherubini V, Rabbone I, Toni S, de Beaufort C, Bakker-van Waarde W, van den Berg N, Volkov I, Barrio R, Hanas R, Zumsteg U, Kuhlmann B, Aebi C, Schumacher U, Gschwend S, Hindmarsh P, Torres M, Shehadeh N, Phillip M PedPump Study Group. Establishing glycaemic control with continuous subcutaneous insulin infusion in children and adolescents with type 1 diabetes: experience of the PedPump Study in 17 countries. Diabetologia. 2008;51(9):1594–1601. doi: 10.1007/s00125-008-1072-2. [DOI] [PubMed] [Google Scholar]
- 3.Ahern JA, Boland EA, Doane R, Ahern JJ, Rose P, Vincent M, Tamborlane WV. Insulin pump therapy in pediatrics: a therapeutic alternative to safely lower HbA1c levels across all age groups. Pediatr Diabetes. 2002;3(1):10–15. doi: 10.1034/j.1399-5448.2002.30103.x. [DOI] [PubMed] [Google Scholar]
- 4.Pańkowska E, Błazik M, Dziechciarz P, Szypowska A, Szajewska H. Continuous subcutaneous insulin infusion vs. multiple daily injections in children with type 1 diabetes: a systematic review and meta-analysis of randomized control trials. Pediatr Diabetes. 2009;10(1):52–58. doi: 10.1111/j.1399-5448.2008.00440.x. [DOI] [PubMed] [Google Scholar]
- 5.Churchill JN, Ruppe RL, Smaldone A. Use of continuous insulin infusion pumps in young children with type 1 diabetes: a systematic review. J Pediatr Health Care. 2009;23(3):173–179. doi: 10.1016/j.pedhc.2008.07.002. [DOI] [PubMed] [Google Scholar]
- 6.Olinder AL, Kernell A, Smide B. Missed bolus doses: devastating for metabolic control in CSII-treated adolescents with type 1 diabetes. Pediatr Diabetes. 2009;10(2):142–148. doi: 10.1111/j.1399-5448.2008.00462.x. [DOI] [PubMed] [Google Scholar]
- 7.Pańkowska E, Skorka A, Szypowska A, Lipka M. Memory of insulin pumps and their record as a source of information about insulin therapy in children and adolescents with type 1 diabetes. Diabetes Technol Ther. 2005;7(2):308–314. doi: 10.1089/dia.2005.7.308. [DOI] [PubMed] [Google Scholar]
- 8.Burdick J, Chase HP, Slover RH, Knievel K, Scrimgeour L, Maniatis AK, Klingensmith GJ. Missed insulin meal boluses and elevated hemoglobin A1c levels in children receiving insulin pump therapy. Pediatrics. 2004;113(3 Pt 1):e221–e224. doi: 10.1542/peds.113.3.e221. [DOI] [PubMed] [Google Scholar]
- 9.Bangstad HJ, Danne T, Deeb LC, Jarosz-Chobot P, Urakami T, Hanas R. Insulin treatment. ISPAD clinical practice consensus guidelines 2006-2007. Pediatr Diabetes. 2007;8(2):88–102. doi: 10.1111/j.1399-5448.2007.00233.x. [DOI] [PubMed] [Google Scholar]
- 10.Toussi M, Choleau C, Reach G, Cahane M, Bar-Hen A, Venot A. A novel method for measuring patients' adherence to insulin dosing guidelines: introducing indicators of adherence. BMC Med Inform Decis Mak. 2008;8:55. doi: 10.1186/1472-6947-8-55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Szypowska A, Pańkowska E, Lipka M. [Guidelines concerning insulin dosage in children and adolescents with type 1 diabetes on continuous subcutaneous insulin infusion] Endokrynol Diabetol Chor Przemiany Materii Wieku Rozw. 2006;12(1):45–50. [PubMed] [Google Scholar]
- 12.Pańkowska E, Szypowska A, Lipka M, Szpotańska M, Błazik M, Groele L. Application of novel dual wave meal bolus and its impact on glycated hemoglobin A1c level in children with type 1 diabetes. Pediatr Diabetes. 2009;10(5):298–303. doi: 10.1111/j.1399-5448.2008.00471.x. [DOI] [PubMed] [Google Scholar]
- 13.DAFNE Study Group. Training in flexible, intensive insulin management to enable dietary freedom in people with type 1 diabetes: dose adjustment for normal eating (DAFNE) randomized controlled trial. BMJ. 2002;325(7367):746. doi: 10.1136/bmj.325.7367.746. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Jones SM, Quarry JL, Caldwell-McMillan M, Mauger DT, Gabbay RA. Optimal insulin pump dosing and postprandial glycemia following a pizza meal using the continuous glucose monitoring system. Diabetes Technol Ther. 2005;7(2):233–240. doi: 10.1089/dia.2005.7.233. [DOI] [PubMed] [Google Scholar]
- 15.Lee SW, Cao M, Sajid S, Hayes M, Choi L, Rother C, de León R. The dual-wave bolus feature in continuous subcutaneous insulin infusion pumps controls prolonged post-prandial hyperglycaemia better than standard bolus in Type 1 diabetes. Diabetes Nutr Metab. 2004;17(4):211–216. [PubMed] [Google Scholar]
- 16.Pańkowska E. Zasady postepowania w leczeniu pompami insulinowymi dzieci z cukrzyc? typu 1. Klin Pediatryczna. 2008;16:5080–5085. [Google Scholar]
- 17.Błazik M, Szypowska A, Golicka D, Groele L, Pańkowska E. The “Diabetics” software in adjusting prandial insulin in patients treated with insulin pumps. The results of RCT study. Pediatr Diabetes. 2009;10(Suppl 11):71. [Google Scholar]