Abstract
Aim
A systematic literature review, covering publications from 1994 to 2009, was carried out to determine the effects of teleconsultation regarding clinical, behavioral, and care coordination outcomes of diabetes care compared to usual care. Two types of teleconsultation were distinguished: (1) asynchronous teleconsultation for monitoring and delivering feedback via email and cell phone, automated messaging systems, or other equipment without face-to-face contact; and (2) synchronous teleconsultation that involves real-time, face-to-face contact (image and voice) via videoconferencing equipment (television, digital camera, webcam, videophone, etc.) to connect caregivers and one or more patients simultaneously, e.g., for the purpose of education.
Methods
Electronic databases were searched for relevant publications about asynchronous and synchronous tele-consultation [Medline, Picarta, Psychinfo, ScienceDirect, Telemedicine Information Exchange, Institute for Scientific Information Web of Science, Google Scholar]. Reference lists of identified publications were hand searched. The contribution to diabetes care was examined for clinical outcomes [e.g., hemoglobin A1c (HbA1c), dietary values, blood pressure, quality of life], for behavioral outcomes (patient-caregiver interaction, self-care), and for care coordination outcomes (usability of technology, cost-effectiveness, transparency of guidelines, equity of access to care). Randomized controlled trials with HbA1c as an outcome were pooled using standard meta-analytical methods.
Results
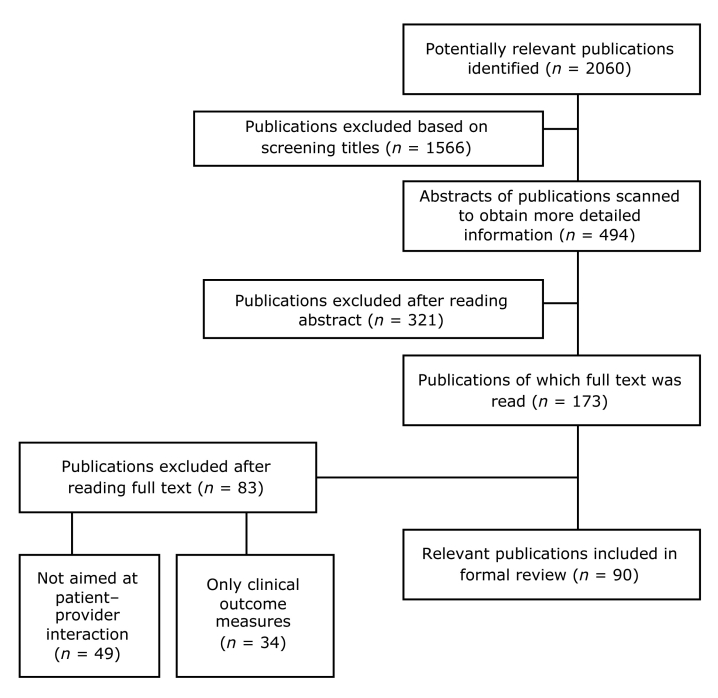
Of 2060 publications identified, 90 met inclusion criteria for electronic communication between (groups of) caregivers and patients with type 1 and 2 or gestational diabetes. Studies that evaluated teleconsultation not particularly aimed at diabetes were excluded, as were those that described interventions aimed solely at clinical improvements (e.g., HbA1c or lipid profiles).
In 63 of 90 interventions, the interaction had an asynchronous teleconsultation character, in 18 cases interaction was synchronously (videoconferencing), and 9 involved a combination of synchronous with asynchronous interaction. Most of the reported improvements concerned clinical values (n = 49), self-care (n = 46), and satisfaction with technology (n = 43). A minority of studies demonstrated improvements in patient-caregiver interactions (n = 28) and cost reductions (n = 27). Only a few studies reported enhanced quality of life (n = 12), transparency of health care (n = 7), and improved equity in care delivery (n = 4). Asynchronous and synchronous applications appeared to differ in the type of contribution they made to diabetes care compared to usual care: asynchronous applications were more successful in improving clinical values and self-care, whereas synchronous applications led to relatively high usability of technology and cost reduction in terms of lower travel costs for both patients and care providers and reduced unscheduled visits compared to usual care. The combined applications (n = 9) scored best according to quality of life (22.2%). No differences between synchronous and asynchronous teleconsultation could be observed regarding the positive effect of technology on the quality of patient-provider interaction. Both types of applications resulted in intensified contact and increased frequency of transmission of clinical values with respect to usual care. Fifteen of the studies contained HbA1c data that permitted pooling. There was significant statistical heterogeneity among the pooled randomized controlled trials (χ2 = 96.46, P < 0.001). The pooled reduction in HbA1c was not statically significant (weighted mean difference -0.10; 95% confidence interval -0.39 to 0.18).
Conclusion
The included studies suggest that both synchronous and asynchronous teleconsultations for diabetes care are feasible, cost-effective, and reliable. However, it should be noted that many of the included studies showed no significant differences between control (usual care) and intervention groups. This might be due to the diversity and lack of quality in study designs (e.g., inaccurate or incompletely reported sample size calculations). Future research needs quasi-experimental study designs and a holistic approach that focuses on multilevel determinants (clinical, behavioral, and care coordination) to promote self-care and proactive collaborations between health care professionals and patients to manage diabetes care. Also, a participatory design approach is needed in which target users are involved in the development of cost-effective and personalized interventions. Currently, too often technology is developed within the scope of the existing structures of the health care system. Including patients as part of the design team stimulates and enables designers to think differently, unconventionally, or from a new perspective, leading to applications that are better tailored to patients' needs.
Keywords: chronic diseases, diabetes mellitus, telemedicine, remote consultation, teleconsultation, videoconferencing, telemonitoring
Introduction
Diabetes requires more effective management for it is a disease that is “skyrocketing, partly because of obesity, partly because it's not treated as effectively as it could be.”1 Worldwide, diabetes is an overwhelming problem due to increasing overweight and the foreseen shortage of highly qualified medical professionals to deliver cost-effective care.2 People at high risk for diabetes should be monitored more closely and encouraged to modify their lifestyle.3 In here, information and communication technology (ICT) might serve as a solution. A previous literature review demonstrated that use of technology that supports electronic information and communication exchange has a significant positive effect on both clinical and behavioral outcomes, such as knowledge, perceived social support, and health behavior.4 However, it was not possible to determine the effects on outcomes on the care coordination level (e.g., cost reduction, equity of health care access), possibly due to a lack of robust methods for evaluation of the cost–benefits or a lack of adequate business models for chronic care management by technology.
Current health care systems are often not supportive enough to stimulate the use of technology in chronic care.5 In principle, ICT exceeds the boundaries of a health care organization and therefore it does not match with fragmented and disorganized health care.6 Therefore, next to the advanced information and communication capacities of technology that allow patients to control their own care and behavior, technology should incorporate disease management. According to the Care Continuum Alliance, disease management is a system of coordinated health care interventions and communications for popu-lations with conditions in which patient self-care efforts are significant, such as diabetes. Disease management supports the physician or practitioner/patient relationship and plan of care; emphasizes prevention of exacerbations and complications utilizing evidence-based practice guidelines and patient empowerment strategies; and evaluates clinical, humanistic, and economic outcomes on an ongoing basis with the goal of improving overall health. Only as such can ICT contribute to a more effective health care system. Thus, technology-based interventions should not only address clinical or disease aspects but also consider behavioral control and the care delivery process in order to realize sustainable changes in diabetes care. This implies for health care applications that they should combine information with at least one additional ICT functionality (e.g., monitoring) for behavior change, education, decision support, or social support with peers or families (online chat rooms) to have optimal results.4,7
The most promising technology in here is teleconsultation, which is defined as a telemonitoring intervention includingpatient–caregiver asynchronous communication [monitoring and delivering feedback via email, Internet, cell phone, automated messaging systems, or other equipment without face-to-face contact], or synchronous communication, which involves real-time, face-to-face contact (image and voice) via videoconferencing equipment (television, digital camera, webcam, videophone, etc.) to connect caregivers and one or more patients simultaneously, for instance, for the purpose of education.8
The aim of this systematic literature review is to assess the effects of teleconsultation for people with diabetes from a holistic perspective by not solely considering clinical outcomes but also holding a behavioral and care coordination viewpoint in order to determine the degree to which existing interactive health care applications contribute to a more effective health system. Clinical outcomes include metabolic control and quality of life. Behavioral outcomes include self-care and patient–care-giver interaction. Care coordination outcomes refer to cost-effectiveness, transparency of the care delivery process, equity of access to care, and usability of equip-ment to facilitate the care delivery process. Our review, which covers publications from 1994 until 2009, identifies the effects of teleconsultation from a multilevel viewpoint in order to inform both scientists and practitioners about the potential of technology to improve diabetes care.
Methods
Search Strategy
We collected publications regarding the empirical evaluation of health care applications facilitating inter-action between caregivers and patients or groups of patients, or among caregivers or patients themselves, using the method for systematic reviews developed by the Centre for Reviews and Dissemination.9 The review was restricted to studies evaluating teleconsultation developed for type 1, 2, and/or gestational diabetes patients and to English language publications. Publications wereidentified in two phases. First, publications that appeared between 1994 and 2007 were collected and analyzed between May 2005 and December 2007.7 Second, given the recent developments in diabetes care and to verify whether more advanced technology and research designs were applied in the meantime, we performed an update of the literature search in June 2009 employing the identical search strategy as in the first case.
No restrictions were imposed on the quality of study designs because assessment studies dealing with inter-active health care applications are not widely available. In particular, behavioral or care coordination aspects have seldom been the focus of reviews on diabetes care. Most reviews on diabetes care focus mainly on clinical values in randomized controlled trials (RCTs).10 In light of a holistic approach, we wanted to provide a broad range of information in order to facilitate decisions about implementing new technology in health care. We excluded studies dealing with broader target groups than diabetes, studies not aimed at patient–caregiver interaction but solely reporting technical aspects of the equipment used, and those that only strived for clinical improvements as well. We included studies that covered both clinical and one or more outcomes (behavioral, care coordination).
The following electronic databases on medicine, psychology, and telemedicine were searched: Medline, Science Direct, Institute for Scientific Information Web of Science, Telemedicine Information Exchange, Psychinfo, Picarta, Google Scholar, and journal indexes (Diabetes Care, Effective Health Care, Journal of Medical Internet Research, International Journal of Medical Informatics, Telemedicine and E-health, Telemedicine and Telecare). Keyword sets combined the word “diabetes” and one of the following words: “telemedicine,” “telecare,” “telehealth,” “e-health,” “teleconsultation,” “telemonitoring,” or “videoconferencing.” We used “telemedicine” because the terms “e-health” and “electronic care” were rarely used in the literature before 2004. In addition to the databases, the reference lists of identified publications were hand searched. Each citation was reviewed and designated as “in,” “out,” or “uncertain” based on the aforementioned restrictions. Sources designated as “in” or “uncertain” were obtained for further review. Two of the authors independently reviewed titles and abstracts of the identified publications to decide whether they should be examined in full detail. We resolved discrepancies by discussion and/or consulting a third person.
One author completed data extraction forms developed by the Centre for Reviews and Dissemination, recording the following details: study design (evidence level and methods for measurement outcomes, patient selection, description intervention and control groups), study population (type of diabetes, age group, number, and recruitment of patients), and intervention details (care setting, technology used to support the care delivery process, and duration of the intervention).9 Using the care levels mentioned previously (clinical, behavioral, and care coordination), we developed a checklist to categorize the outcomes of the interventions (see Table 1).
Table 1.
Checklist Used to Classify Outcome Measures in Identified Studies
| Level of diabetes care | Outcome measures |
|---|---|
| Clinical |
|
| Behavioral |
|
| Care coordination |
|
Five levels (see Table 2) were used to categorize the methodological approaches of the studies.11 Two authors independently rated the study designs. In case of disagreement, consensus was reached by discussion.
Table 2.
Checklist to Categorize Level of Evidence of Study Design
| Level of evidence | Study design (description of methodological approaches) |
|---|---|
| 1 | Experimental studies (e.g., RCT with concealed allocation) |
| 2 | Quasi-experimental studies (e.g., experimental study with randomization) |
| 3 | Controlled observational studies |
| 3a | Cohort studies |
| 3b | Case control studies |
| 4 | Observational studies without control groups |
| 5 | Expert opinion based on bench research or consensus |
Statistical Methods
A quality assessment was completed for all RCTs using the Jadad scale.11 This scale contains questions regarding randomization, blinding, and withdrawals that are scored by a yes (1) or no (0). In total, five points can be awarded, with higher points indicating higher study quality.
Points are, however, deducted if the method of random-ization and/or the method of blinding is described, but is inappropriate.
Changes in hemoglobin A1c (HbA1c) values were calculated from baseline and follow-up means and standard deviations. Only studies researching effects on adults were included in the meta-analysis. When the deviation of the mean difference was not available in the papers, the authors were contacted. In case of no response or no availability of the requested information, we estimated the variance by using (1) reported confidence intervals, (2) reported P values, or (3) an imputation technique.12 A random-effects model was used for pooling the included studies because clinical hetero-geneity between studies was expected. Between-study heterogeneity was tested using the χ2 statistic. One study reported data on two intervention groups and one control group.35 In the meta-analysis, both intervention groups were compared with the same control group, resulting in one extra comparison for this study. In one study, three intervention groups and one control group were studied.76 In the meta-analysis, all three intervention groups were compared with the same usual care group, resulting in two extra comparisons.
Results
Study Characteristics
Of the 2060 potentially relevant publications identified, 90 were included in our final review (see Figure 1). The Appendix summarizes the intervention characteristics as described in the included publications. In 63 of 90 interventions the interaction had an asynchronous teleconsultation character,14,15,17–26,28,29,35–46,48,50,52–57,60,62–66,68–71,73–88,90,92,96 in 18 cases interaction was synchronous (video-conferencing),13,16,27,33,34,37,47,51,58,67,72,89,93,98–102 and 9 involved a combination of synchronous with asynchronous interaction.30–32,59,61,91,94,95,97 The most frequently applied methodological approach was an observational study (case series or before–after design), which was used in 48 studies. Twenty-eight studies were RCTs, and 8 involved quasi-experimental studies. If not reported otherwise in the Appendix, control groups accurately reflected current standard practices as they would be administered outside of the trial. In other words, “controls”—within the scope of this article—imply those patients who received usual care as practiced at the participating institution, concurrently enrolled along with the intervention group. Other methodological approaches were used only incidentally (4 cohort studies and 2 studies based on expert interviews). Sample sizes ranged from ≤20 (n = 18), ≤100 (n = 43), to >100 (n = 28), and in one case sample size was not specified. Samples sizes include both intervention and control respondents. Respondents were selected by the research team (n = 36),19,24,27,29,31–33,35,43–45,49,54–57,65,67,68,71,74,77,79–81,83,86–88,90,92,94,95,97,98,102 the general practitioner (GP) (n = 5),13,16,28,76,102 a specialist (n = 8),20,28,46,64,69,52,78,85 or via convenience sampling (n = 3).82,51,93 For the remaining studies, it remained unclear who selected the participants (n = 38). Interestingly, we detected a relationship between the selection procedure and the outcome level. First, it appeared that interventions for which a convenience sampling method was used mainly involved video-conferencing51,93 and particularly attracted patients that “wanted to maintain their level of health but with minimum intrusiveness.”51 In other words, respondents who had put themselves forward to receive the inter-vention were searching for convenience and happened to obtain this by means of videoconferencing. Second, those interventions to which the respondents were allocated by their own medical specialist led relatively more frequently to improved clinical values (6 out of 8 studies; 75%20,46,64,69,78,85) compared to interventions where participants were recruited via the GP (3 out of 5 studies; 60%13,16,76), the research team (20 out of 36; 55.6%19,27,29,32,43,55,57,65,67,68,71,74,77,80,81,83,86,90,95,98), or via convenience sampling (0 out of 3 studies; 0%82,51,93). This might be explained by the intensive treatment relationship among specialist and diabetic patient; the specialist has a very clear impression for which patients the intervention might be suited. Third, in cases which the GP was responsible for patient recruitment, the interventions particularly served educational purposes by means of videoconferencing, leading to higher levels of knowledge among patients.16,18,102
Figure 1.
Selection process.
A variety of research methods were used to gather data: interviews, focus groups, log files, and nonstandardized questionnaires. Also, one usability test15 and a cognitive walk-through61 were used. Validated questionnaires were used in 27 of the 90 studies to measure usability of technology, quality of life, and self-care. The Telemedicine Satisfaction Questionnaire was used for measuring usability of technology.21,60,58,102 Quality of life was measured via various questionnaires: the World Health Organization Quality of Life-Bref,21 World Health Organization–Diabetes Treatment Satisfaction Question-naire,85 SF-12,28,60,76 SF-36,17,27,30,32,37,58,85,99 Diabetes Quality of Life,19,27,58,60,76,99 Depression Scale CES-D,76 Problem Areas in Diabetes Scale,35,58 Visual Analog Scale,62 Zung Self-Rating Depression Scale,98 Depression Short-CARE,94 Diabetes Distress Scale,94 and Health-Related Quality of Life.43 The Diabetes Knowledge Assessment,27 Test of Diabetes Knowledge mTDK,78,98 Diabetes Treatment Satisfaction Questionnaire,58 Appraisal of Diabetes Scale,58 Diabetes Management Self-Efficacy Scale,35 Diabetes Self-Care Activity Scale,43,81 Diabetes Empowerment Scale,55,98 and Diabetes Care Profile98 were used to measure self-care. Sometimes, researchers developed and validated an instrument themselves.44,57,97
The Appendix presents improvements found in the included studies per outcome level (clinical values, quality of life, patient–caregiver interaction, self-care, usability, cost reduction, transparency, and equity). Most of the studies reported clinical improvements (n = 49; 37 asynchronous, 9 synchronous, and 3 combined interventions), followed by usability of technology (n = 43; 27 asynchronous, 12 synchronous, and 4 combined interventions), self-care (n = 42; 34 asynchronous, 6 synchronous, and 2 combined interventions), patient–caregiver interaction (n = 28; 21 asynchronous, 5 synchronous interventions, and 2 combined interventions), and cost reduction (n = 27; 15 asynchronous, 9 synchronous, and 3 combined interventions). A minority of the studies reported improvements in quality of life (n = 12; 7 asynchronous, 3 synchronous, and 2 combined interventions), transparency of care delivery guidelines (n = 7; 4 asynchronous, 2 synchronous, and 1 combined intervention), and in equity in access to health care (n = 4; 3 synchronous and 1 combined intervention).
Settings and Interventions
Interventions took place in different care settings (see Appendix): 40 took place in primary care settings,15,22,25,30–32,36,37,49,52–54,56,58,65,68–70,73,76,77,79–85,87–95,97,10229 in secondary care settings,16–20,26,28,29,33,35,39,40,45–48,51,55,60,63,64,67,72,78,89,96,100,101 and 13 in integrated care settings.14,21,34,38,43,44,50,57,59,61,71,74,98 In seven studies, the setting was not specified13,23,41,42,66,75,86 and one study was carried out in tertiary care.62 Half of the studies took place in the United States (n = 4514,16,17,24,26,28,30–32,36,37,43,47,49,52–59,61,65,72,73,76,79–83,87,88,90–95,97–101). Five were in Spain41,42,45,48,60 or in the United Kingdom.15,35,40,44,74 Four studies were conducted in Australia71,75,78,89 or in Denmark.34,38,39,67 Three studies were performed in Poland25,63,64 and China.27,96,102 The remaining studies took place in Canada,51,69 Taiwan,68 The Netherlands,23,86 Korea,29,62 Norway,33,50 Austria,13,84 France,19,46 Germany,20 Italy,66,85 and Israel.22 In three cases, the study was conducted in multiple countries: Italy, Spain and Norway18,21 and Wales and Germany.70
The interventions were particularly targeted at monitoring clinicalvalues,14,17–20,22,25,26,29,34,35,39,41–43,45,46,48,50,52–57,60,62–71,79–81,83–87,92,96 education,13,15,16,23,30–33,37,44,51,58,72,75,78,88,89,90,93,98,99,100,102 or monitoring combined with education.21,24,27,28,30,32,38,40,47,59,61,73,74,76,77,82,91,94,95,97,99,101 Several interventions were based on Wagner's chronic care model,27,30,51,53,54,66,82,83,90 socioecological model,98 social cognitive theory,88 practice guidelines for diabetes care,16,36,70,92,94,95 a Bayesian model of carbohydrate metabolism,39 various behavioral theories such as Bandura's self-efficacy theory,14,15,35,74,88 theories about patient centeredness,38,40 organization learning13 or information theories,75 and health information management theory.61 It appeared that 37 out of 90 studies involved interventions with team-based care settings consisting of a specialized nurse, a specialist, or a primary care provider supported by a case manager to coordinate the care delivery process,21,29–32,34–36,38,39,44,54,55,57,59–61,67,68,70,73,78,83,88,90–95,97,99 a team with primary care providers, nurses, and a call center,74 or patients, peers, and care providers.15 In three publications, a health care team was mentioned, but it remained unclear of whom this team consisted.16,24,98
Different types of technologies were used for measuring and sending clinical data: palmtops, glucometers, cell phones, and digital cameras. In most cases (60 out of 90 studies), stand-alone applications were used, such as mobile (smart) phones or personal digital assistants (PDAs),14,19,20,35,41,43,44,62–64,66,69,73,78,84,85,87,92 videoconferencing tools,13,16,17,27,33,34,37,51,58,72,89,94,95,98,100–102 or Web-based disease management systems.15,23–25,38,39,45,49,50,53,54,55,57,60,62,65,66,68,71,73,75–77,83,86,90,96 If reported, the choice of the system depended on the patients' priorities or the availability of a telephone or Internet connection. In 30 out of 90 studies, multiaccess systems were used, such as Web-based electronic communication networks combined withmobiletechnology,18,21,22,26,29,35,40,42,46,52,70,74,77,79,81 videoconsultation,30,31,32,47,59,61,91,93,97,99 or specially designed devices (such as Health Buddy or a PDA) for instruction and feedback.28,30–32,56,88 To enhance disease control, feedback in 24 cases was provided automatically via computer-generated reminders via a short message service (SMS) and email whenever values were alarming17,19, 21–26,36,43,45,49,55–57,63,65,68,69,71,82,84,85,96 and/or in 54 cases caregivers provided feedback personally via SMS, (video)phone, PDA, fax, video consultation, and email (within the Web-based system) or face-to-face to instruct patients when necessary.14,16,17,25–29,31,33–35,38–41,44,46–48,50,52,53,58, 59,61–63,65–68,74,76–79,81,83–90,92,93,97–102 In 15 cases, it was not clear how feedback was given.15,18,20,30,32,37,51,56,57,70,72,80,91,94,95
Criteria applied to include patients in the intervention group were (only mentioned here if reported in at least five publications) being diagnosed with type 1 diabetes,18–20,26,38,40,45,46,48,60,73,85 being diagnosed with type 2 diabetes,29,43,52,62,69,70,76,81,82,86,87,88,93 being diagnosed with either type 1 or type 2 diabetes,17,24,25,36,53,57,97,98 being motivated to take part in the intervention,18,21,24,26,43 having or being a caregiver taking part in the inter-vention,28,44,56,96,77,80,86,90,96,97 living in region of care,28,36,41,59,76,82,92,97,98 being younger than 30 years,14,26,40,46,49,78 being an adult,19,22,24,43,53,55,65,81,85,87,88,93,98 being economically disadvantaged,28,46,73,76,82 having poor metabolic control (HbA1c >8%),14,19,35,40,43,46,48,52,60,65,77,78,81,87 being able to handle the technique,20,28,38,42,62,76 having access to the Internet21,29,42,49,62,68 or a cell phone,17,21,28,29,36,41,42,49,62,70,76,79 or being without severe comorbidities.26,59,68,70,94
Clinical Effects
Improved Clinical Values
Hemoglobin A1c levels were measured in 25 RCTs,20–22,25,29,35,40,45,46,49,50,55,60,63,65,66,68,76–78,81,83,84,90,93 but only 15 were suitable for meta-analysis. Two RCTs studied only children46,78 and were therefore not included in the meta-analysis. Three trials solely involved two intervention groups29,49,65 and 2 were excluded because it concerned a crossover design.45,84 Furthermore, we excluded 1 study given the patients had gestational diabetes.55 Two studies were excluded because using an imputation technique was unadvisable, as data provided by the author differed from published data21 or the author did not provide data.90
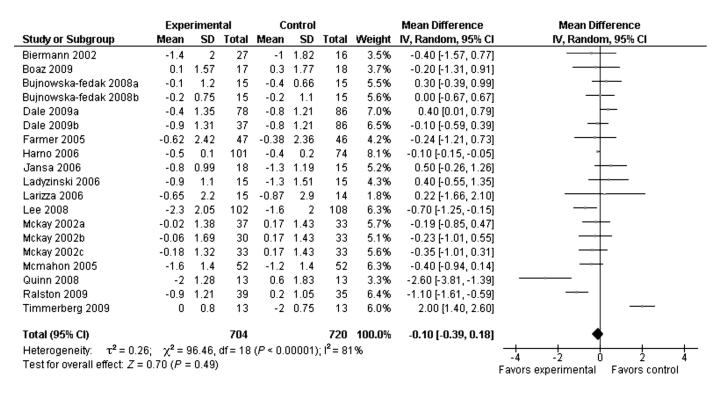
Changes in HbA1c values were calculated from baseline and follow-up means and standard deviations. The Jadad quality scores of pooled trials varied from 0 to 3 (see Table 3). The method used to generate the sequence of randomization was not clear in 8 of 15 RCTs, and a description of withdrawals and dropouts was only given in 7 of 15 studies. Pooled RCTs included patients with type 1 diabetes,18,20,40,60,63 type 2 diabetes,35,68,77,81,83,93 both type 1 and type 2 diabetes,22,50 or diabetes type was not specified.25,66,77 Glucose values were sent via a telephone network/modem,20,21,35,40,50,60,63,66 via the Internet,18,22,25,68,76,77,81,83 or via videoconferencing.93 Care settings were primary care,22,25,68,76,77,81,83,93 secondary care,20,40,60,35,63 or integrated care21,50 or the care setting remained unspecified.66 Trials varied in duration from 3 to 12 months. Only 3 of the pooled RCTs showed a significant difference in HbA1c between intervention and control groups.68,81,83 In one study, the control group even showed a significantly larger fall in HbA1c compared to the intervention group.93 Of the 10 RCTs that were excluded from meta-analysis, 3 studies demonstrated a significant difference between intervention and control groups.21,46,84 Table 3 presents the mean difference between baseline and follow-up HbA1c values for each included RCT in the meta-analysis. These values were either reported in the paper or provided by the authors. A random-effects meta-analysis was performed due to significant statistical heterogeneity among the pooled RCTs (χ2 = 96.46, P < 0.001). The pooled reduction in HbA1c was not statistically significant [weighted mean difference (WMD) –0.10; 95% confidence interval –0.39 to 0.18].Figure 2 shows the mean difference and WMD of mean differences between baseline and follow-up HbA1c values.
Table 3.
Randomized Controlled Trials with Hemoglobin A1c Data
| Study | Trial duration (months) | Intervention | Control | |||||
|---|---|---|---|---|---|---|---|---|
| N | B-Fa | Mean difference ± standard deviation | N | B-Fa | Mean difference ± standard deviation | Quality score11 | ||
| Biermann20 | 4 | 27 | 8.3 ± 2.3 (B) | −1.4 ± 2.0b | 16 | 8.0 ± 2.1 (B) | −1.0 ± 1.82 | 3 |
| 6.9 ± 1.3 (F) | 7.0 ± 1.0 (F) | |||||||
| Boaz22 | 6 | 17 | 8.4 ± 1.4 (B) | 0.1 ± 1.57b | 17 | 9.3 ± 1.6 (B) | 0.3 ± 1.77 | 0 |
| 8.5 ± 1.7 (F) | 9.6 ± 1.9 (F) | |||||||
| Bujnowska-Fedak25,c (a) | 6 | 15 | 8.9 ± 1.2 (B) | −0.1 ± 1.2b | 15 | 8.1 ± 0.6 (B) | −0.4 ± 0.66 | 0 |
| 8.8 ± 1.2 (F) | 7.7 ± 0.7 (F) | |||||||
| Bujnowska-Fedak25,c (b) | 6 | 15 | 6.8 ± 0.8 (B) | −0.2 ± 0.75b | 15 | 6.4 ± 1.1 (B) | −0.2 ± 1.1 | 0 |
| 6.6 ± 0.7 (F) | 6.2 ± 1.1 (F) | |||||||
| Dale35,d (a) | 6 | 78 | 8.4 ± 1.1 (B) | −0.4 ± 1.35b | 86 | 8.7 ± 1.3 (B) | −0.8 ± 1.21 | 3 |
| 8.0 ± 1.5 (F) | 7.9 ± 1.1 (F) | |||||||
| Dale35,d (a) | 6 | 37 | 8.9 ± 1.5 (B) | −0.9 ± 1.31b | 86 | 8.7 ± 1.3 (B) | −0.8 ± 1.21 | 3 |
| 7.9 ± 0.9 (F) | 7.9 ± 1.1 (F) | |||||||
| Farmer40 | 9 | 47 | 9.2 ± 1.1 (B) | −0.62 ± 2.42e | 46 | 9.3f ± 1.5 (B) | −0.38 ± 2.36 | 2 |
| 8.6 ± 1.4 (F) | 8.9 ± 1.4 (F) | |||||||
| Harno50 | 12 | 101 | 7.8 ± 0.1 (B) | −0.5 ± 0.1b | 74 | 8.2 ± 0.2 (B) | −0.4 ± 0.2 | 2 |
| 7.3 ± 0.1 (F) | 7.8 ± 0.2 (F) | |||||||
| Jansa60 | 12 | 18 | 8.4 ± 1.2 (B) | −0.8 ± 0.74f | 15 | 8.9 ± 1.3 (B) | −1.3 ± 0.64 | 3 |
| 7.6 ± 0.9 (F) | 7.6 ± 0.7 (F) | |||||||
| Ladyzinski64 | 6 | 15 | 8.0 ± 1.1 (B) | −0.9 ± 1.1b | 15 | 8.1 ± 1.7 (B) | 1.3 ± 1.51 | 0 |
| 7.1 ± 1.1 (F) | 6.8 ± 1.2 (F) | |||||||
| Larizza66,g | 12 | 15 | 8.40 ± 2.53 (B) | −0.65 ± 2.20b | 14 | 10.15 ± 3.25 (B) | −0.87 ± 2.90 | 2 |
| 7.75 ± 1.16 (F) | 9.28 ± 2.34 (F) | |||||||
| Lee68 | 9 | 102 | 9.0 ± 2.8 (B) | −2.3 ± 2.05b | 108 | 9.0 ± 2.2 (B) | −1.6 ± 2.0 | 0 |
| 6.7 ± 2.1 (F) | 7.4 ± 1.7 (F) | |||||||
| McKay76,h (a) | 3 | 37 | 7.75 ± 1.33 (B) | −0.02 ± 1.38b | 33 | 7.20 ± 1.36 (B) | 0.17 ± 1.43 | 3 |
| 7.73 ± 1.42 (F) | 7.37 ± 1.49 (F) | |||||||
| McKay76,h (b) | 3 | 30 | 7.64 ± 1.71 (B) | −0.06 ± 1.69b | 33 | 7.20 ± 1.36 (B) | 0.17 ± 1.43 | 3 |
| 7.59 ± 1.66 (F) | 7.37 ± 1.49 (F) | |||||||
| McKay76,h (c) | 3 | 33 | 7.46 ± 1.35 (B) | −0.18 ± 1.32b | 33 | 7.20 ± 1.36 (B) | 0.17 ± 1.43 | 3 |
| 7.28 ± 1.28 (F) | 7.37 ± 1.49 (F) | |||||||
| McMahon77 | 12 | 52 | 10.0 ± 0.8 (B) | −1.6 ± 1.4 | 52 | 9.9 ± 0.8 (B) | −1.2 ± 1.4 | 2 |
| Quinn81 | 3 | 13 | 9.5 ± 1.4 (B) | −2.0 ± 1.28b | 13 | 9.0 ± 2.0 (B) | −0.6 ± 1.83 | 1 |
| 7.5 ± 1.1 (F) | 8.4 ± 1.6 (F) | |||||||
| Ralston83 | 12 | 39 | 8.2 ± 0.7 (B) | −0.9 ± 1.21b | 35 | 7.9 ± 1.1 (B) | 0.2 ± 1.05 | 3 |
| 7.3 ± 1.4 (F) | 8.1 ± 1.0 (F) | |||||||
| Timmerberg93 | 2 | 13 | 7.2 ± 0.8 (B) | 0 ± 0.8b | 13 | 6.7 ± 0.8 (B) | −0.2 ± 0.75 | 0 |
| 7.2 ± 0.8 (F) | 6.5 ± 0.8 (F) | |||||||
B, baseline; F, follow-up.
Imputation technique.
Group (a) includes insulin-dependent patients and group (b) includes noninsulin-dependent patients.
Intervention (a) was peer support and intervention (b) was diabetes specialist nurse.
Calculated using 95% confidence interval.
Calculated using P values provided by author.
Data from location 2 (adults), see Appendix.
Intervention (a) was personal self-management coach, intervention (b) was peer support, and intervention (c) was combined condition.
Figure 2.
Comparison of changes in hemoglobin A1c control versus intervention. SD, standard deviation; IV, intravenous; CI, confidence interval.
Furthermore, 22 observational and quasi-experimental studies also demonstrated a decrease of HbA1c: 14 involving asynchronouscommunication,14,18,19,23,25,36,43,48,52,64,70,74,86,96 7 studies evaluating synchronous communication,13,27,47,58,93,98,99 and 1 concerning a combination of synchronous and asynchronous communication.32 Improvements in inter-vention groups, however, were not always significant compared to a control group (usual care).19,77,86 In 1 study, control group participants even outperformed inter-vention participants.93 Improvements with regard to metabolic control were achieved in several types of interventions: Web-based care management programs for patients who have poor metabolic control, with automatic data transmission, educational modules, and messaging systems for communication and personal feedback. All types of media were employed in these interventions: motivational phone calls, palmtop computers, cell phones, telemedicine units, or videoconferencing.
Other clinical improvements concerned (independent of study design): self-reported health status diminished,98 diabetes regulation,90 lipid profiles,77,86 stable ulcer healing,67 total calorie intake,27 and cardiovascular risk factor control.90 Several interventions were successful in decreasing body mass index27,43,98 and/or weight,95,98 although these changes were not always significant.43,98 Cholesterol concentrations decreased significantly in four interventions,50,58,68,70 but in one case, however, cholesterol levels increased.16 Interventions were particularly beneficial for a decrease in fasting blood glucose levels,22,29,50,57,68,85 mean blood glucose levels,19,63,64 and postprandial glucose levels.29,57,85 Glycemic control improved in four interventions,27,63–65 even as (systolic and/ordiastolic)bloodpressure.43,50,69,70,77,83,86,95,98 Interventions that were beneficial on multiple clinical outcome levels particularly concerned interventions with mobile phones aimed at giving feedback.63,64,70,85
Improved Quality of Life
Quality of life improved in a slightly lower amount of studies compared to HbA1c.19,22,25,27,28,30,58,60,64,76,93,95 Of these, seven interventions were asynchronous, three were synchronous, and two interventions were combined. In five studies, improvement in quality of life was not significant compared to usual care.25,58,60,76,93 Quality of life was not measured in a uniform way, as reported earlier. A broad range of validated instruments was used, such as the Diabetes Quality of Life (DQOL) measure. Quality of life measured with the DQOL improved in two studies.19,60 A mean improvement in general mental and physical status was realized.25,27,28,30,64,76 Interventions also helped patients feel less stressed58 or depressed.22,95 In one study, surprisingly, the rate of depression increased while using an intervention.98 This might be explained by the significant increase in knowledge that the intervention (educational sessions through videoconferencing) realized. Knowledge or information overload might evoke awareness of one's situation, leading to depression. Another study reported an increase in level of worry and the degree in which diabetes affected the patients' life.93 A relatively high amount of interventions with a positive impact on quality of life involved synchronous communication with video.27,30,58,93 Three of these interventions27,58,93 concerned educational interventions. In two cases of these, videoconferencing took place in a community setting,27,93 whereas the other intervention30 consisted of a home message system that allowed monitoring and communication by videophone. In four interventions, patients and care providers interacted via a home telemedicine unit.22,25,28,95 Patients in the telemonitoring group needed to have a personal computer (PC) with Internet access at home. A home telemedicine unit is composed of two modules: a patient unit and a medical unit connected by a computer network. Patients using the telemedicine system were asked to download their data from the blood glucose monitoring device into the PC via an infrared connection and send all results via the Internet to the care provider. Generally, both units offer tools to doctors and patients for data collection, data analysis, and decision support and are enabled to send messages and/or therapeutic advice to the patients. In the remaining interventions, a Web-based disease management program was used,76 a glucometer with a modem,60 a mobile phone,19,64 and/or a PDA.19
Behavioral Effects
Improved Interaction
Twenty-eight studies reported improvements in patient– caregiver interactions (see Appendix).18,23,25,27,28,34,35,38,39,45,46,48,53,54,57,66,73,76,78,81,82,84,85,93,95,97,100,102 This number can be considered high, as the total number of studies that evaluated interaction was 29. The majority of interventions had an asynchronous character (n = 21), five had a synchronous character, and two involved combined interventions. The only intervention of which interaction was not rated positively among users involved the HealthPia GlucoPackTM.26 This is a diabetes monitoring system that has a small blood glucose monitoring device integrated into the battery pack of a cell phone. Adolescents were not enthusiastic about the impact of the phone on the relationship with their parents.
Both asynchronous and synchronous interventions generated identical interactional benefits: increased intensity of contact between provider and patient,23,28,39,45,48,57,76 providers perceived as more supportive according to patients,95,97 more effective communication,34,39,45,57,78,85 increased metabolic data transmission,23,28,48,76 availability and completeness of data among caregivers,23,76 and improved communication between caregivers57,100 or with peers.35,53,100 In general, patients believed that the lack of physical contact was acceptable.
No trend could be observed in the type of medium and/or intervention that was contributing most positively to the quality of interaction. A blood glucose meter was used six times that automatically sends data to a system that generates computer-generated feedback for monitoring purposes and, if necessary, from a care provider.18,46,48,66,73,82 Another six times, a home telemedicine was employed, which, in the most advanced case, was a system that integrates communication with three different medical devices (glucometer, insulin pump, and continuous glucose sensor) with a personal logbook, visualization, therapy viewing, and so on.25,28,45,57,95,97 A Web-based disease management system was also a successful medium to enhance interaction: an Internet-based self-management program providing online blood glucose tracking, patient–physician (primary care provider) contact, and sometimes message postings on a (peer) forum.38,39,53,54,76 Other media concerned a mobile phone81,84,85 and motivational telephone calls.35,78
Improved Self-Care
Improved self-care was observed in 42 studies (see Appendix).14–16,19,22,26–28,38,39,42–45,47–49,53–56,58,60,62–65,68,69,73,77,81,82,85,86,88,92,94,95,97,98,102 Six interventions had a synchronous character, 2 were a combination of asynchronous and synchronous interactions, and the remaining 34 were asynchronous. In six studies, the improvement was significant compared to usual care.22,49,63,65,77,94 In five publications, interventions had no29,35,78 or a negative61,93 impact on self-care. The fact that these interventions focused primarily on general education and not specifically on how to cope with diabetes possibly accounts for this. In these cases, standardized education programs were provided, not tailored specifically to the patients' individual characteristics. Twenty-three of the 42 studies showed that the technology better enabled patients to manage their disease.15,16,22,26,28,38,39,42,44,45,48,53,54,56,57,60,64,73,80–82,86,97 Various instruments were used to measure disease management, varying from interviews to focus groups and nonstandardized questionnaires. However, none of the instruments had been validated before. Interventions that helped patients manage their diabetes better particularly included asynchronous interventions: home telemedicine units22,28,45,56,57,97 and Web-based disease management programs.15,38,39,53,54,82 Synchronous communication appeared less suitable for enhancing self-management, as of these 23 interventions, only 1 had a synchronous character (videoconferencing).97 Furthermore, it appeared from 13 studies that technology increased the frequency with which patients monitored their levels of blood glucose or blood pressure or monitored their meals.19,29,38,43,45,49,63,69,77,81,88,92 Seven studies reported an improvement in knowledge, each measuring knowledge with a different (whether or not validated) instrument.16,27,60,81,85,97,98 Relatively many of these knowledge-improving interventions concerned synchronous communication.16,27,98 Given the facts that only 1 out of 23 interventions that explicitly enhanced self-manage-ment concerned synchronous interaction and that the majority of the knowledge-improving interventions involved synchronous interventions on the contrary, one might conclude that synchronous communication is more appropriate to improve knowledge, whereas asynchronous interaction is suitable to enhance disease management. Other indicators for increased levels of self-care among patients were better management of blood sugar transfer/adherence with medication14,16,29,47,68,92 and a better understanding of the patient's own medical condition.28,45,54,62,81
Care Coordination Effects
Usability
Fifty-six studies included usability of technology as an outcome measure. In the majority of these interventions (n = 45), usability of technology was assessed positively among its users. Generally, usability was assessed via general items such as “technology is useful”15,18,22,24,25,35,45,48,53,69,70,71,73,75,80,81,83,84,85,87,88,93,95,98 and/or the technology appeared “easy touse.”13,15,19,20,22,26,27,28,30,33,41,43,45,47,51,58,66,71,72,81,84,88,91,96,101,102 Asynchronous interaction interventions were particularly reviewed as helpful, whereas synchronous interaction (videoconferencing) was mainly perceived as user-friendly. No systematic comparisons could be made with regular care as the control group participants did not use technology. Usability was particularly measured via interviews or questionnaires. The majority of studies focused on patients. Only four evaluations solely incorporated caregivers.18,73,86,90
Nine publications reported an outstandingly high rate of respondents who assessed usability positively, implying that at least 90% of respondents expressed high satisfaction with the technology.26,30,35,58,72,81,85,93,96 Half of these interventions concerned synchronous communication through videoconferencing 30,58,72,93 and four interventions involved (mobile) phones.26,35,81,85 Also, one intervention that led to extremely high satisfaction included a hand-held computer that automatically sent dietary and clinical data to a diabetes team and with the possibility of system-generated feedback. The four highly appreciated synchronous interventions were all characterized by an educational purpose, mainly on nutrition.58,93 The useful and easy-to-use interventions with a mobile phone each targeted another aspect of diabetes: nutrition,85 treatment regimen,81 lifestyle,35 and blood glucose.26 Mobile phone interventions consisted of a cell phone-based diabetes management software system used with Web-based data analytics and optimization tools. The software provided real-time feedback on patients' nutrition or blood glucose levels, displayed patients' medication regimens, incorporated hypo- and hyperglycemia treatment algorithms, and requested additional data needed to evaluate diabetes management. Patient data captured and transferred to secure servers were usually analyzed by proprietary statistical algorithms. The system sent computer-generated feedback to the patient but also to patients' care providers, so the latter could contact the patient if necessary.
Satisfaction with technology heavily depended on education and training. Training to learn how to handle the equipment was claimed to be given in half of the cases (47 out of 90).19,20,22,26,28,29,31–33,35–40,42–46,48–50,53,55,56,58,60,62–65,68–74,76,81,84,85,88,91,97,98,102 In 11 studies, technology was valued negatively by its users.38,39,46,49,54,56,57,61,67,82,91 Five times, it concerned a Web-based disease management system with values entered by the patient and feedback provided by the system or by care providers.38,39,49,54,82 Web-based disease management programs provide automatic transmission of clinical values, educational modules, and a messaging system for communication and personal feedback (warning messages and instruction). Web-based systems sometimes appeared unreliable,39,54 as laboratory results were sometimes missed or the provided information was inaccurate. Also, Web-based systems led to frustration among patients39,82 or among providers.38 In 5 cases, dissatisfaction concerned the functioning of a home telemedicine unit, which is a specially modified computer that connects to the Internet and is designed to support self-monitoring and electronic upload of finger-stick glucose and blood pressure, logging, and messaging with a care provider. The main problem was that these telemedicine units generated installation problems56,91 or patients' inability to master the unit due to a lack of fine eye–hand coordination. Only in 1 case was dissatisfaction expressed regarding videoconferencing.91 The latter concerned connectivity problems, the impossibility for the visiting nurse to upload images to the record prior to video consultation, unstable audio signal, and an exaggerated red color of the skin on the image.
Other publications also mentioned ICT-related problems. The most frequently mentioned problem was that patients perceived the technology as too complex to handle (n = 17)19,25,26,31,41,48,50,55,61,69,70,71,76,88,91,95,102 and/or too time-consuming to implement in daily routine (n = 15).20,29,38,39,43,45,48,55,63,69,70,76,85,86,97 In 10 cases, there was a lack of an adequate infrastructure21,23,31,66,67,75,81,84,91,102 or there were organizational difficulties, such as the inability to agree on a suitable time for the consultation.31,49 Sometimes (n = 9) patients experienced that using the technology led to information overload,23,28,38,39,54,75,86,91,97 and sometimes patients were reluctant to cooperate, resulting in unreliable clinical data transmissions (n = 7).13,20,38,62,68,91,102 In four interventions, ICT-based care was thought to reduce the trusting and confidential relationship between patients and caregivers.20,38,82,91 These negative side effects are considerable and should be a subject of future research.
Reduction of Costs
In sum, 33 studies mentioned costs. In 27 of them, costs decreased as a consequence of teleconsultation. In the other 6 studies, costs increased or remained the same. Nine of the studies that demonstrated cost reduction involved synchronous communication13,33,37,72,89,97,100, 101,102 and 3 concerned combined interventions.30–32 The interaction in the remaining interventions occurred asynchronously (n = 15).17,20,26,28,36,39,41,50,52,57,60,64,74,87,90 Cost-effectiveness was not measured uniformly among the various studies: by means of interviews, by non-standardized questionnaires, and by retrieving data from visit logs. Also, cost-effectiveness and cost savings were expressed in various ways: in terms of quality-adjusted life years,74 incremental cost-effectiveness ratios,17 savings per year per patient, reduction of overall utilization and charges after 1 year, or treatment time of caregivers. Because cost-effectiveness was not measured uniformly and the intervention characteristics (duration, type of techno-logy, number of professionals and patients involved, and so on) varied strongly among the studies, it was impossible to determine a cutoff point for significant cost savings. Therefore, we were not able to draw more specific conclusions about significant levels of cost savings.
Cost savings were particularly achieved in a reduction of health care utilization costs: a decrease in consultation time,20,60,64,97 decreased number of hospital admissions,13,32,36 emergency department visits,30,31,72 hospitalizations,30,37,72 number of bed days of care,30,32,36 and discharges to home care.37 Lower treatment costs refer to the potential of teleconsultation to provide the same number of patient encounters at lower costs,90 the decrease of recertification of patients,37 and the replacement of conventional visits by videoconferencing.72
Seven studies showed that teleconsultation led to more just-in-time care instead of just-in-case (more preventive care). Three interventions reduced unscheduled primary care visits,30–32 decreased the number of doctor visits,26,39,50 and led to more timely follow-up.57 In four cases, teleconsultation generated lower travel costs for patients30,33,101 and caregivers.89 Cost reductions were, for the most part, found in observational studies without a control group,13,20,26,30,33,36,39,41,57,64,72,74,87,89,97,100,102 in which costs were calculated during the intervention period and compared to costs before intervention took place. In 11 studies, cost reductions of teleconsultation were compared to a control group receiving usual care.17,20,28,31,32,37,50,52,60,90,101
Of the 27 interventions that led to cost reduction, almost half concerned synchronous communication through videoconferencing.13,30–33,37,72,89,97,100,101,102 This is remarkable given the relatively low number of synchronous interventions included in the review [27 (18 synchronous and 9 combined) synchronous versus 63 asynchronous interventions]. Regarding asynchronous interventions that led to cost reduction, no relationship could be detected between cost savings and the type of technological devices used. Devices varied from a glucometer,20,60 a home telemedicine unit,17,28,36,57 a mobile phone,26,41,64 email,52,90 and telephone calls74,87 to a Web-based disease management system.39 Overall, it appeared that videoconferencing and combined interventions were more successful in reducing costs compared to Web-based disease management systems. This might be caused by the fact that Web-based systems require care providers to spend extra time on working with the system, whereas system use duration for video conferencing equals face-to-face consultation duration.
Not all studies considering cost-effectiveness demonstrated reduced costs. Six studies reported an increase in costs due to teleconsultation or a lack of (significant) difference between the intervention and the control group.20,24,34,60,78,80,83,84 Teleconsultation significantly increased physician's time, as patients tended to call more often,20 it took more time to review data and to reply per SMS to patients,84 and it took more time updating care plans and communicating over the Web with patients compared to usual care.83 One videoconferencing intervention implied that a lot of time had to be spent on scheduling and waiting in time of delay.34 In one study, more time was needed to handle technical problems.60
Improved Transparency
Enhanced transparency was reported in seven public-ations: four about an intervention with an asynchronous character,52,56,73,86 two with a synchronous character,33,100 and one with combined character.97 From these studies, it appeared that implementing clinical practice guide-lines led to a significant decrease in HbA1c, 52,86 to more complete patient records,86,97 to enhanced coordination in treatment with diabetic foot ulcers,33 or to simplify the process of deciding which patients to include in the intervention.56 Only in one study was there a significant difference between the intervention group and usual care.52 No relationship could be observed regarding the type of intervention and outcomes on the transparency level.
Improved Equity
Four interventions characterized by synchronous communication (video) were reported to have improved equity, such as better access to specialized health care in underserved areas31,72,100,101 or to patients with complex medical conditions.31 Those interventions also appeared to be cost-effective, as it reduced patients' travel and waiting time.100,101
Reported Shortcomings of Studies
Several publications reported shortcomings of the studies. Most frequently mentioned were the lack of a significant difference between the intervention and the control group,19–22,25,27,29,36,40,49,52,58,60,63,66,76,78,86,90,93,101 the inability to measure long-term effects of the intervention,16,21,26,28,29,36,40,43,55,64,65,71,76,79,90,93,99 the fact that interventions sometimes inherently lead to improved results because of a selection bias,17,19,24,26,29,36,39,44,63,64,65,68,69,70,79,81,85,87,92,94 some patient groups benefit more from the intervention than others,31,44,79,80,83,86,87,97 e.g., patients with poor metabolic control,86 high use of health care,31 motivated patients,46 and inexperienced patients,20,30,86 or other shortcomings.14,16,17,19,22,24,26,29,35,39,43,44,45,49,53,55–57,59,67,70,71,74,78,80, 81,85,87,88,90,93–95,97,98
Conclusion and Discussion
A systematic literature review, covering publications from 1994 to 2009, was carried out to determine the effects of teleconsultation regarding clinical, behavioral, and care coordination outcomes of diabetes care compared to usual care. In the period under review, 90 out of 2060 identified studies had a scope broader than clinical outcomes. The evaluated interventions focused on a combination of different services: information exchange, monitoring, education, and care coordination. Studies were performed mainly in the United States (n = 45). Six were conducted in Asia, four in Australia, and the remainder in Europe. Two-third of all studies (n = 66) dated from 2004 to 2009, and the majority of these studies were even carried out in 2006 or later. Most of the interventions concerned observational studies (n = 48), although an increase in the number of RCTs could be observed since 2006.
Asynchronous communication was the most used technology application (n = 63). In most cases, a mobile phone or PDA was used to control clinical values, sometimes in combination with a Web-based information system for education and feedback. Video consultation (synchronous communication) was used in 18 interventions, and 9 interventions combined synchronous with asynchro-nous communication, such as Web-based systems with an integrated possibility for videoconferencing. Thirty-seven interventions involved team-based care, involving different care providers (e.g., nurses, case manager, psychologist, physician, GP). Mostly, technology was used as a stand-alone application (n = 60) rather than an integration of different technology devices for monitoring and communication and education.
Most of the reported improvements concerned clinical values (n = 49), self-care (n = 46), and satisfaction with technology (n = 43). A minority of studies demonstrated improvements in patient–caregiver interactions (n = 28) or cost reductions (n = 27). Only a few studies reported an enhanced quality of life (n = 12), transparency of health care (n = 7), and improved equity in care delivery (n = 4).
Asynchronous and synchronous applications appeared to differ in the type of contribution that was made to diabetes care compared to usual care.
Interventions characterized by asynchronous interaction (n = 63) reported relatively more improvements in clinical values (58%) and self-care (54%). Asynchronous applications appeared to have more impact on self-control and disease management in providing more reliable monitoring results (provided automatically and personally by phone) and intensified contact between patients and caregivers.
Synchronous applications (n = 18) reported relatively more improvements in usability of technology (67%) and cost reduction (50%). Synchronous applications are more user-friendly and cost-effective in terms of lower travel costs for both patients and care providers and reduced unscheduled visits.
Combined applications (n = 9) scored best according to quality of life (22.2%) compared to asynchronous and synchronous applications.
Both synchronous (n = 18) and combined applications (n = 9) had a relatively more positive influence on transparency of health care (both 11%, compared to 6% of asynchronous applications) and equity (16 and 11% for synchronous and combined applications compared to 0% of asynchronous applications).
No differences between synchronous and asynchronous teleconsultation could be observed regarding the positive effect of technology on the quality of patient–provider interaction (33% of asynchronous applications, 28% of synchronous applications, and 22% of combined applications). Asynchronous, synchronous, and combined interaction resulted in intensified contact and increased frequency of transmission of clinical values with respect to usual care. In general, patients did not perceive the lack of face-to-face contact with a caregiver as a barrier for communication. It should be noted, however, that in these studies, almost none of the improvements in quality of interaction were significant compared to usual care. In this sense, it can be argued that technology did not compromise the care delivery process. In fact, on all outcome levels, the use of technology appeared to evoke negative side effects in a minority of cases: clinical values deteriorated;93 the rate of depression increased due to technology;98 there was a negative impact on the relationship between diabetic adolescents and their parents;26 it caused doubts about the ability to manage diabetes;61,93 it led to frustration,38,39,82 organizational difficulties,31,49 and information overload;23,28,38,39,54,75,86,91,97 reduced trust and confidence in the patient–caregiver relationship;20,38,82,91 and led to a cost increase20,24,34,60,78,80, 83,84 due to increased consultation time and time required for caregivers to review data. It should be questioned to what degree these negative side effects are acceptable and are outweighed by the benefits. Negative side effects could have been overcome when patients would have been involved in the early stages of the design process. Too often, technology is developed within the scope of the existing structures of the health care system. However, when including patients as part of the design team, out-of-the-box thinking is stimulated, implying that designers or care providers who develop technology are inspired to think differently, unconventionally, or from a new perspective, leading to applications that are better tailored to patients' needs.
Our findings indicate that ICT, especially asynchronous applications such as mobile phones, is being used increasingly for improving diabetes care, resulting in an increased and even more reliable transmission of clinical values and intensified patient–caregiver information exchange. Given the claim that managing diabetes care should be based on a holistic approach that focuses on different levels of care (clinical feasibility as well as behavioral change and care coordination), we observed that most interventions addressed one or more levels of disease control. However, these interventions were mostly not based on a disease management approach such as the chronic care model: a proactive collaboration between patient and caregivers. Only in a minority of interventions was such a model applied (n = 10). Technology-based diabetes care interventions are rarely used to support collaboration between caregivers and patients aimed at a better balance between self-care and professional care.
As prior reviews also reported, technology-based inter-ventions do not often lead to significant improvements compared to usual care due to practical difficulties to manipulate inclusion criteria for intervention and control groups (randomization problems, dropouts).7,103 However, a comparison with usual care is sensitive for bias. Therefore, to determine the impact of technology on diabetes care it is more relevant to determine which aspect of a particular technology improves which aspect of diabetes care. For example, when considering the impact of automated versus personal feedback on the intensity and reliability of monitoring clinical values, it is interesting to investigate the effects of synchronous versus asynchronous applications on the quality of communication and emotional outcomes. In light of economical outcomes it is worthwhile to find out the optimal intensity of online or phone contacts to realize cost savings and to enhance the quality of care.
To evaluate the impact of technology on diabetes care we need more advanced methods than RCTs.107 From 2006, we detected an increase in the number of RCTs. The fact that most studies have their roots in medical research that favor traditional RCTs in clinical control settings may account for this. However, several disadvantages are inherent to RCTs that impede adequate investigation of the impact of implementing technology in health care organizations: selection bias (patients might be recruited whose prognosis is better than average), study procedures (e.g., in an RCT patients may receive intensive diagnostic procedures and follow-up care difficult to achieve in the “real world”), incomplete reporting of adverse effects of interventions, and, most importantly within the view of this review, outcome measures (e.g., RCTs use composite measures used infrequently in clinical practice). Recently, a debate started that cast doubt on the ideas that “observational studies should not be used for defining evidence-based medical care” and that RCT results are “evidence of the highest grade,” as observational and quasi-experimental studies provide results of the same strength as RCTs. Moreover, observational and quasi-experimental designs enable researchers to study effects of particular intervention characteristics, such as tailored patient–caregiver interaction, which are impossible in a double-blinded, randomized trial.
Future Research
Despite an increase in the number of RCTs since 2006, the number of studies that showed significant improvements in outcomes (on a clinical, behavioral, and/or care coordination level) due to technology did not rise. During the past 16 years, hardly any changes in clinical outcomes and quality of life due to technology could be demonstrated compared to usual care.This may be due to inadequate study designs (e.g., inaccurate or incompletely reported sample size calculations, too small sample sizes to detect significant differences), the lack of robust measurements, and a one-sided focus on comparing interventions to usual care. Given the claim that technology is a challenge for future care, we have to investigate the role of technology in optimizing diabetes care in more detail. This requires quasi-experimental study designs and a holistic approach focusing on multilevel determinants (clinical, behavioral, and care coordination) to promote self-care and proactive collaborations between health care professionals and patients to manage diabetes care. Also, we need a more participatory design approach (involvement of target users in the development of health care interventions) in developing cost-effective and personalized interventions, implying that we have to study what type of intervention designs have the largest impact on disease management. For instance, personalized medicine, such as involvement of patients in the development of health care interventions, can enhance persistence in usage and adherence to treatment plans.104 Involvement of care professionals, payers (e.g., insurance companies), and patients in the development of disease management interventions can overcome the myopic approach of diabetes care interventions that are disease and complications driven, neglecting patient self-management supporting needs and emotional and economical outcomes.6 The involvement of stakeholders in the design, implementation, and evaluation process of technological applications might optimize the contribution of technology to the quality of health care.
One of the most relevant functionalities in technology-based care for persistence in compliance with treatments appeared to be the method for providing feedback on outcomes and behavior. In most of the included studies, feedback was given personally or in combination with automated computer-generated feedback in case of alarming values. To enhance disease control, computer-generated feedback can be more reliable than personal feedback.105 However, we have no insight in the pros and cons of automated-generated electronic feedback. Future research could assess the differences in feedback modalities on the frequency and reliability of disease control (e.g., glucose) and on adherence to treatment goals.
Another issue is the increased use of advanced mobile technologies, such as PDAs and mobile phones in combination with Web-based disease programs, for education and instruction. Future research should focus on how smartphones or other smart technology can be used as integrated systems for monitoring, education, and data exchange.
Implications for Practice
Based on this review, we provide the following practical implications for supporting diabetes care via technology:
Participatory development of interventions to realize personalized medicine instead of template medicine
Key stakeholders (payers, professionals, and patients) should be involved in the development of inter-ventions to create cooperation and collaboration and to assess the critical values for improvement for sustainable care (adequate business models)
Multifaceted architecture of interventions: self-manage-ment of clinical values is most effective when combined with education and information to motivate and persuade patients to do the right thing at the right moment and to support health care professionals to modify the treatment program106
The deployment of mobile technology, which appeared a promising application for monitoring and feedback
Acknowledgments
The authors thank Carina de Blaauw, M.Sc., for performing the literature search and part of the data extraction in phase 2 (June 2009), and Wouter Meijer, M.D., for his careful considerations and valuable comments.
Abbreviations
- DQOL
Diabetes Quality of Life
- GP
general practitioner
- HbA1c
hemoglobin A1c
- ICT
information communication technology
- PC
personal computer
- PDA
personal digital assistant
- RCT
randomized controlled trial
- SMS
short message service
- WMD
weighted mean difference
References
- 1.Obama B. Obama's healthcare townhall transcript–remarks, audience questions. Los Angeles, Los Angeles Times. 2009 Aug 11 [cited 2010 Jan 27]. Available from: http://latimesblogs.latimes.com/washington/2009/08/obama-healthcare-transcript-new-hampshire.html.
- 2.Klonoff DC. The increasing incidence of diabetes in the 21st century. J Diabetes Sci Technol. 2009;2009(1):1–2. doi: 10.1177/193229680900300101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Klonoff DC. Personalized medicine for diabetes. J Diabetes Sci Technol. 2008;2008(3):335–341. doi: 10.1177/193229680800200301. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Murray E, Burns J, See TS, Lai R, Nazareth I. Interactive health communication applications for people with chronic disease. Cochrane Database Syst Rev. 2004;4 doi: 10.1002/14651858.CD004274.pub2. CD004274. [DOI] [PubMed] [Google Scholar]
- 5.Palmer AJ, Dinneen S, Gavin JR, Gray A, Herman WH, Karter AJ. Cost-utility analysis in a UK setting of self-monitoring of blood glucose in patients with type 2 diabetes. Curr Med Res Opin. 2006;2006(5):861–872. doi: 10.1185/030079906X104669. [DOI] [PubMed] [Google Scholar]
- 6.Norris SL, Nichols PJ, Caspersen CJ, Glasgow RE, Engelgau MM, Jack L, Isham G, Snyder SR, Carande-Kulis VG, Garfield S, Briss P, McCulloch D. The effectiveness of disease and case management for people with diabetes. A systematic review. Am J Prev Med. 2002;22(4 Suppl):15–38. doi: 10.1016/s0749-3797(02)00423-3. [DOI] [PubMed] [Google Scholar]
- 7.Verhoeven F, van Gemert-Pijnen L, Dijkstra K, Nijland N, Seydel E, Steehouder M. The contribution of teleconsultation and video-conferencing to diabetes care: a systematic literature review. J Med Internet Res. 2007;9(5):e37. doi: 10.2196/jmir.9.5.e37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Kern J. Evaluation of teleconsultation systems. Int J Med Inform. 2006;75(3-4):330–334. doi: 10.1016/j.ijmedinf.2005.08.001. [DOI] [PubMed] [Google Scholar]
- 9.Centre for Reviews and Dissemination. Undertaking systematic reviews of research on effectiveness. Centre for Reviews and Dissemination. 2001 [cited 2010 Jan 27]. Available from: http://www.york.ac.uk/inst/crd/report4.htm. [Google Scholar]
- 10.Ouwens M, Wollersheim H, Hermens R, Hulscher M, Grol R. Integrated care programmes for chronically ill patients: a review of systematic reviews. Int J Qual Health Care. 2005;2005(2):141–146. doi: 10.1093/intqhc/mzi016. [DOI] [PubMed] [Google Scholar]
- 11.Jadad AR, Moore RA, Carroll D, Jenkinson C, Reynolds DJ, Gavaghan DJ, McQuay HJ. Assessing the quality of reports of randomized clinical trials: is blinding necessary? Control Clin Trials. 1996;1996(1):1–12. doi: 10.1016/0197-2456(95)00134-4. [DOI] [PubMed] [Google Scholar]
- 12.Follman D, Elliott P, Suh I, Cutler J. Variance imputation for overviews of clinical trials with continuous response. J Clin Epidemiol. 1992;1992(7):769–773. doi: 10.1016/0895-4356(92)90054-q. [DOI] [PubMed] [Google Scholar]
- 13.Abrahamian H, Schueller A, Mauler H, Prager R, Irsigler K. Transfer of knowledge from the specialist to the generalist by videoconferencing: effect on diabetes care. J Telemed Telecare. 2002;2002(6):350–355. doi: 10.1258/135763302320939248. [DOI] [PubMed] [Google Scholar]
- 14.Adkins JW, Storch EA, Lewin AB, Williams L, Silverstein J, Malasanos T, Geffken GR. Home-based behavioral health intervention: use of a telehealth model to address poor adherence to type-1 diabetes medical regimens. Telemed J E Health. 2006;2006(3):370–372. doi: 10.1089/tmj.2006.12.370. [DOI] [PubMed] [Google Scholar]
- 15.Armstrong N, Powell J. Preliminary test of an Internet-based diabetes self-management tool. J Telemed Telecare. 2008;2008(3):114–116. doi: 10.1258/jtt.2008.003002. [DOI] [PubMed] [Google Scholar]
- 16.Balamurugan A, Hall-Barrow J, Blevins MA, Brech D, Phillips M, Holley E, Bittle K. A pilot study of diabetes education via telemedicine in a rural underserved community opportunities and challenges: a continuous quality improvement process. Diabetes Educator. 2009;2009(1):147–154. doi: 10.1177/0145721708326988. [DOI] [PubMed] [Google Scholar]
- 17.Barnett TE, Chumbler NR, Vogel WB, Beyth RJ, Ryan P, Figueroa S. The cost-utility of a care coordination/home telehealth programme for veterans with diabetes. J Telemed Telecare. 2007;2007(6):318–321. doi: 10.1258/135763307781644843. [DOI] [PubMed] [Google Scholar]
- 18.Bellazzi R, Larizza C, Montani S, Riva A, Stefanelli M, d'Annunzio G, Lorini R, Gomez EJ, Hernando E, Brugues E, Cermeno J, Corcoy R, de Leiva A, Cobelli C, Nucci G, Del Prato S, Maran A, Kilkki E, Tuominen J. A telemedicine support for diabetes management: the T-IDDM project. Comput Methods Programs Biomed. 2002;2002(2):147–161. doi: 10.1016/s0169-2607(02)00038-x. [DOI] [PubMed] [Google Scholar]
- 19.Benhamou PY, Melki V, Boizel R, Perreal F, Quesada JL, Bessieres-Lacombe S, Bosson JL, Halimi S, Hanaire H. One-year efficacy and safety of Web-based follow-up using cellular phone in type 1 diabetic patients under insulin pump therapy: the PumpNet study. Diabetes Metab. 2007;2007(3):220–226. doi: 10.1016/j.diabet.2007.01.002. [DOI] [PubMed] [Google Scholar]
- 20.Biermann E, Dietrich W, Rihl J, Standl E. Are there time and cost savings by using telemanagement for patients on intensified insulin therapy? A randomised, controlled trial. Comput Methods Programs Biomed. 2002;2002(2):137–146. doi: 10.1016/s0169-2607(02)00037-8. [DOI] [PubMed] [Google Scholar]
- 21.Bellazzi R, Arcelloni M, Bensa G, Blankenfeld H, Brugués E, Carson E, Cobelli C, Cramp D, D'Annunzio G, De Cata P, De Leiva A, Deutsch T, Fratino P, Gazzaruso C, Garcìa A, Gergely T, Gómez E, Harvey F, Ferrari P, Hernando E, Boulos MK, Larizza C, Ludekke H, Maran A, Nucci G, Pennati C, Ramat S, Roudsari A, Rigla M, Stefanelli M. Design, methods, and evaluation directions of a multi-access service for the management of diabetes mellitus patients. Diabetes Technol Ther. 2003;2003(4):621–629. doi: 10.1089/152091503322250640. [DOI] [PubMed] [Google Scholar]
- 22.Boaz M, Hellman K, Wainstein J. An automated telemedicine system improves patient-reported well-being. Diabetes Technol Ther. 2009;2009(3):181–186. doi: 10.1089/dia.2008.0048. [DOI] [PubMed] [Google Scholar]
- 23.Branger PJ, Van't Hooft A, Van Der Wouden JC, Moorman PW, Van Bemmel JH. Shared care for diabetes: supporting communi-cation between primary and secondary care. Int J Med Inform. 1999;53(2-3):133–142. doi: 10.1016/s1386-5056(98)00154-3. [DOI] [PubMed] [Google Scholar]
- 24.Bryce CL, Zickmund S, Hess R, McTigue KM, Olshansky E, Fitzgerald K, Fischer G. Value versus user fees: perspectives of patients before and after using a web-based portal for management of diabetes. Telemed J E Health. 2008;2008(10):1035–1043. doi: 10.1089/tmj.2008.0005. [DOI] [PubMed] [Google Scholar]
- 25.Bujnowska-Fedak MM, Puchała E, Steciwko A. Telemedicine for diabetes support in family doctors' practices: a pilot project. J Telemed Telecare. 2006;12(Suppl 1):8–10. doi: 10.1258/135763306777978551. [DOI] [PubMed] [Google Scholar]
- 26.Carroll AE, Marrero DG, Downs SM. The HealthPia GlucoPack diabetes phone: a usability study. Diabetes Technol Ther. 2007;2007(2):158–164. doi: 10.1089/dia.2006.0002. [DOI] [PubMed] [Google Scholar]
- 27.Chan WM, Woo J, Hui E, Lau WW, Lai JC, Lee D. A community model for care of elderly people with diabetes via telemedicine. Appl Nurs Res. 2005;2005(2):77–81. doi: 10.1016/j.apnr.2004.11.002. [DOI] [PubMed] [Google Scholar]
- 28.Cherry JC, Moffatt TP, Rodriguez C, Dryden K. Diabetes disease management program for an indigent population empowered by telemedicine technology. Diabetes Technol Ther. 2002;2002(6):783–791. doi: 10.1089/152091502321118801. [DOI] [PubMed] [Google Scholar]
- 29.Cho JH, Lee HC, Lim DJ, Kwon HS, Yoon KH. Mobile communi-cation using a mobile phone with a glucometer for glucose control in Type 2 patients with diabetes: as effective as an Internet-based glucose monitoring system. J Telemed Telecare. 2009;2009(2):77–82. doi: 10.1258/jtt.2008.080412. [DOI] [PubMed] [Google Scholar]
- 30.Chumbler NR, Neugaard B, Kobb R, Ryan P, Qin H, Joo Y. Evaluation of a care coordination/home-telehealth program for veterans with diabetes: health services utilization and health-related quality of life. Eval Health Prof. 2005;2005(4):464–478. doi: 10.1177/0163278705281079. [DOI] [PubMed] [Google Scholar]
- 31.Chumbler NR, Neugaard B, Ryan P, Qin H, Joo Y. An observational study of veterans with diabetes receiving weekly or daily home telehealth monitoring. J Telemed Telecare. 2005;2005(3):150–156. doi: 10.1258/1357633053688723. [DOI] [PubMed] [Google Scholar]
- 32.Chumbler NR, Vogel WB, Garel M, Qin H, Kobb R, Ryan P. Health services utilization of a care coordination/home-telehealth program for veterans with diabetes: a matched-cohort study. J Ambul Care Manage. 2005;2005(3):230–240. doi: 10.1097/00004479-200507000-00006. [DOI] [PubMed] [Google Scholar]
- 33.Clemensen J, Larsen SB, Ejskjaer N. Telemedical treatment at home of diabetic foot ulcers. J Telemed Telecare. 2005;11(Suppl 2):14–16. doi: 10.1258/135763305775124830. [DOI] [PubMed] [Google Scholar]
- 34.Clemensen J, Larsen SB. Cooperation versus coordination: using real-time telemedicine for treatment at home of diabetic foot ulcers. J Telemed Telecare. 2007;13(Suppl 3):32–35. [Google Scholar]
- 35.Dale J, Caramlau I, Sturt J, Friede T, Walker R. Telephone peer-delivered intervention for diabetes motivation and support: the telecare exploratory RCT. Patient Educ Couns. 2009;2009(1):91–98. doi: 10.1016/j.pec.2008.09.014. [DOI] [PubMed] [Google Scholar]
- 36.Dang S, Ma F, Nedd N, Florez H, Aquilar E, Roos BA. Care coordination and telemedicine improves glycaemic control in ethnically diverse veterans with diabetes. J Telemed Telecare. 2007;2007(5):263–267. doi: 10.1258/135763307781458958. [DOI] [PubMed] [Google Scholar]
- 37.Dansky KH, Palmer L, Shea D, Bowles KH. Cost analysis of telehomecare. Telemed J E Health. 2001;2001(3):225–232. doi: 10.1089/153056201316970920. [DOI] [PubMed] [Google Scholar]
- 38.Dinesen B, Andersen PE. Qualitative evaluation of a diabetes advisory system, DiasNet. J Telemed Telecare. 2006;2006(2):71–74. doi: 10.1258/135763306776084329. [DOI] [PubMed] [Google Scholar]
- 39.Dinesen B, Rostgaard Andersen PE. Qualitative evaluation of a diabetes advisory system, DiasNet. J Telemed Telecare. 2006;2006(2):71–74. doi: 10.1258/135763306776084329. [DOI] [PubMed] [Google Scholar]
- 40.Farmer AJ, Gibson OJ, Dudley C, Bryden K, Hayton PM, Tarassenko L, Neil A. A randomized controlled trial of the effect of real-time telemedicine support on glycemic control in young adults with type 1 diabetes (ISRCTN 46889446) Diabetes Care. 2005;2005(11):2697–2702. doi: 10.2337/diacare.28.11.2697. [DOI] [PubMed] [Google Scholar]
- 41.Ferrer-Roca O, Cárdenas A, Diaz-Cardama A, Pulido P. Mobile phone text messaging in the management of diabetes. J Telemed Telecare. 2004;2004(5):282–285. doi: 10.1258/1357633042026341. [DOI] [PubMed] [Google Scholar]
- 42.Ferrer-Roca O, Franco Burbano K, Cárdenas A, Pulido P, Diaz-Cardama A. Web-based diabetes control. J Telemed Telecare. 2004;2004(5):277–281. doi: 10.1258/1357633042026288. [DOI] [PubMed] [Google Scholar]
- 43.Forjuoh SN, Reis MD, Couchman GR, Ory MG. Improving diabetes self-care with a PDA in ambulatory care. Telemed J E Health. 2008;2008(3):273–279. doi: 10.1089/tmj.2007.0053. [DOI] [PubMed] [Google Scholar]
- 44.Gambling T, Long AF. Exploring patient perceptions of movement through the stages of change model within a diabetes tele-care intervention. J Health Psychol. 2006;2006(1):117–128. doi: 10.1177/1359105306058854. [DOI] [PubMed] [Google Scholar]
- 45.García-Sáez G, Hernando ME, Martinez-Sarriegui I, Rigla M, Torralba V, Brugues E, Leiva A de, Gomez EJ. Architecture of a wireless Personal Assistant for telemedical diabetes care. Int J Med Inform. 2009;2009(6):391–403. doi: 10.1016/j.ijmedinf.2008.12.003. [DOI] [PubMed] [Google Scholar]
- 46.Gay CL, Chapuis F, Bendelac N, Tixier F, Treppoz S, Nicolino M. Reinforced follow-up for children and adolescents with type 1 diabetes and inadequate glycaemic control: a randomized controlled trial intervention via the local pharmacist and telecare. Diabetes Metab. 2006;2006(2):159–165. doi: 10.1016/s1262-3636(07)70263-x. [DOI] [PubMed] [Google Scholar]
- 47.Gelfand K, Geffken G, Halsey-Lyda M, Muir A, Malasanos T. Intensive telehealth management of five at-risk adolescents with diabetes. J Telemed Telecare. 2003;2003(2):117–121. doi: 10.1258/135763303321328000. [DOI] [PubMed] [Google Scholar]
- 48.Gómez EJ, Hernando ME, García A, Del Pozo F, Cermeño J, Corcoy R, Brugués E, De Leiva A. Telemedicine as a tool for intensive management of diabetes: the DIABTel experience. Comput Methods Programs Biomed. 2002;2002(2):163–177. doi: 10.1016/s0169-2607(02)00039-1. [DOI] [PubMed] [Google Scholar]
- 49.Hanauer DA, Wentzell K, Laffel N, Laffel LM. Computerized Automated Reminder Diabetes System (CARDS): e-mail and SMS cell phone text messaging reminders to support diabetes management. Diabetes Technol Ther. 2009;2009(2):99–106. doi: 10.1089/dia.2008.0022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Harno K, Kauppinen-Mäkelin R, Syrjäläinen J. Managing diabetes care using an integrated regional e-health approach. J Telemed Telecare. 2006;12(Suppl 1):13–15. doi: 10.1258/135763306777978380. [DOI] [PubMed] [Google Scholar]
- 51.Hebert MA, Paquin MJ, Iversen S. Predicting success: stakeholder readiness for home telecare diabetic support. J Telemed Telecare. 2002;8(Suppl 3):33–36. [PubMed] [Google Scholar]
- 52.Henault RG, Eugenio KR, Kelliher AF, Alexis G, Conlin PR. Transmitting clinical recommendations for diabetes care via e-mail. Am J Health Syst Pharm. 2002;2002(22):2166–2169. doi: 10.1093/ajhp/59.22.2166. [DOI] [PubMed] [Google Scholar]
- 53.Hess R, Bryce CL, McTigue K, Fitzgerald K, Zickmund S, Olshansky E, Fischer G. The diabetes patient portal: patient perspectives on structure and delivery. Diabetes Spectrum. 2006;2006(2):106–110. [Google Scholar]
- 54.Hess R, Bryce CL, Paone S, Fischer G, McTigue KM, Olshansky E, Zickmund S, Fitzgerald K, Siminerio L. Exploring challenges and potentials of personal health records in diabetes self-management: implementation and initial assessment. Telemed J E Health. 2007;2007(5):509–517. doi: 10.1089/tmj.2006.0089. [DOI] [PubMed] [Google Scholar]
- 55.Homko CJ, Santamore WP, Whiteman V, Bower M, Berger P, Geifman-Holtzman O, Bove AA. Use of an Internet-based telemedicine system to manage underserved women with gestational diabetes mellitus. Diabetes Technol Ther. 2007;2007(3):297–306. doi: 10.1089/dia.2006.0034. [DOI] [PubMed] [Google Scholar]
- 56.Hopp FP, Hogan MM, Woodbridge PA, Lowery JC. The use of telehealth for diabetes management: a qualitative study of telehealth provider perceptions. Implement Sci. 2007;2:14. doi: 10.1186/1748-5908-2-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Hopp FP, Hogan M. Community-based tele-health systems for persons with diabetes: development of an outcomes model. Soc Work Health Care. 2009;2009(2):134–153. doi: 10.1080/00981380802533389. [DOI] [PubMed] [Google Scholar]
- 58.Izquierdo RE, Knudson PE, Meyer S, Kearns J, Ploutz-Snyder R, Weinstock RS. A comparison of diabetes education administered through telemedicine versus in person. Diabetes Care. 2003;2003(4):1002–1007. doi: 10.2337/diacare.26.4.1002. [DOI] [PubMed] [Google Scholar]
- 59.Izquierdo R, Meyer S, Starren J, Goland R, Teresi J, Shea S, Weinstock RS. Detection and remediation of medically urgent situations using telemedicine case management for older patients with diabetes mellitus. Ther Clin Risk Manag. 2007;2007(3):485–489. [PMC free article] [PubMed] [Google Scholar]
- 60.Jansà M, Vidal M, Viaplana J, Levy I, Conget I, Gomis R, Esmatjes E. Telecare in a structured therapeutic education programme addressed to patients with type 1 diabetes and poor metabolic control. Diabetes Res Clin Pract. 2006;2006(1):26–32. doi: 10.1016/j.diabres.2006.03.005. [DOI] [PubMed] [Google Scholar]
- 61.Kaufman DR, Pevzner J, Hilliman C, Weinstock RS, Teresi J, Shea S, Starren J. Redesigning a telehealth diabetes management program for a digital divide seniors population. Home Health Care Manag Prac. 2006;2006(3):223–234. [Google Scholar]
- 62.Kim H, Yoo Y, Shim H. Effects of an Internet-based intervention on plasma glucose levels in patients with type 2 diabetes. J Nurs Care Qual. 2005;2005(4):335–340. doi: 10.1097/00001786-200510000-00009. [DOI] [PubMed] [Google Scholar]
- 63.Ladyzynski P, Wojcicki JM. Home telecare during intensive insulin treatment–metabolic control does not improve as much as expected. J Telemed Telecare. 2007;2007(1):44–47. doi: 10.1258/135763307779701167. [DOI] [PubMed] [Google Scholar]
- 64.Ladyzinski P, Wojcicki JM, Krzumien J, Foltybski P, Migalska-Musial K, Tracz M, Karnafel W. Mobile telecare system for intensive insulin treatment and patient education. First application for newly diagnosed type 1 diabetic patients. Int J Artif Organs. 2006;2006(11):1074–1081. doi: 10.1177/039139880602901108. [DOI] [PubMed] [Google Scholar]
- 65.Laffel LM, Hsu WC, McGill JB, Meneghini L, Volkening LK. Continued use of an integrated meter with electronic logbook maintains improvements in glycemic control beyond a randomized, controlled trial. Diabetes Technol Ther. 2007;2007(3):254–264. doi: 10.1089/dia.2006.0021. [DOI] [PubMed] [Google Scholar]
- 66.Larizza C, Bellazzi R, Stefanelli M, Ferrari P, De Cata P, Gazzaruso C, Fratino P, D'Annunzio G, Hernando E, Gomez EJ. The M2DM Project–the experience of two Italian clinical sites with clinical evaluation of a multi-access service for the management of diabetes mellitus patients. Methods Inf Med. 2006;2006(1):79–84. [PubMed] [Google Scholar]
- 67.Larsen SB, Clemensen J, Ejskjaer N. A feasibility study of UMTS mobile phones for supporting nurses doing home visits to patients with diabetic foot ulcers. J Telemed Telecare. 2006;2006(7):358–362. doi: 10.1258/135763306778682323. [DOI] [PubMed] [Google Scholar]
- 68.Lee TI, Yeh YT, Liu CT, Chen PL. Development and evaluation of a patient-oriented education system for diabetes management. Int J Med Inform. 2007;2007(9):655–663. doi: 10.1016/j.ijmedinf.2006.05.030. [DOI] [PubMed] [Google Scholar]
- 69.Logan AG, McIsaac WJ, Tisler A, Irvine MJ, Saunders A, Dunair A, Rizo CA, Feig DS, Hamill M, Trudel M, Cafazzo JA. Mobile phone-based remote patient monitoring system for management of hypertension in diabetic patients. Am J Hypertens. 2007;2007(9):942–948. doi: 10.1016/j.amjhyper.2007.03.020. [DOI] [PubMed] [Google Scholar]
- 70.Luzio S, Piehlmeier W, Tovar C, Eberl S, Lätzsch G, Fallböhmer E, Rumpel E, Owens DR, Landgraf R. Results of the pilot study of DIADEM: a comprehensive disease management programme for type 2 diabetes. Diabetes Res Clin Prac. 2007;2007(3):410–417. doi: 10.1016/j.diabres.2006.09.025. [DOI] [PubMed] [Google Scholar]
- 71.Ma C, Warren J, Phillips P, Stanek J. Empowering patients with essential information and communication support in the context of diabetes. Int J Med Inform. 2006;2006(8):577–596. doi: 10.1016/j.ijmedinf.2005.09.001. [DOI] [PubMed] [Google Scholar]
- 72.Malasanos TH, Burlingame JB, Youngblade L, Patel BD, Muir AB. Improved access to subspecialist diabetes care by telemedicine: cost savings and care measures in the first two years of the FITE diabetes project. J Telemed Telecare. 2005;11(Suppl 1):74–76. doi: 10.1258/1357633054461624. [DOI] [PubMed] [Google Scholar]
- 73.Malasanos TH, Patel BD, Klein J, Burlingame JB. School nurse, family and provider connectivity in the FITE diabetes project. J Telemed Telecare. 2005;11(Suppl 1):76–78. doi: 10.1258/1357633054461741. [DOI] [PubMed] [Google Scholar]
- 74.Mason JM, Young RJ, New JP, Gibson JM, Long AF, Gambling T, Friede T. Economic analysis of a telemedicine intervention to improve glycemic control in patients with diabetes mellitus. Dis Manage Health Outcomes. 2006;2006(6):377–385. [Google Scholar]
- 75.Mazzi CP, Kidd M. A framework for the evaluation of Internet-based diabetes management. J Med Internet Res. 2002;10(41):e1. doi: 10.2196/jmir.4.1.e1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.McKay HG, Glasgow R, Feil EG, Boles SM, Barrera M. Internet-based diabetes self-management and support: initial outcomes from the Diabetes Network Project. Rehabil Psychol. 2002;2002(1):31–48. [Google Scholar]
- 77.McMahon GT, Gomes HE, Hickson Hohne S, Hu TM, Levine BA, Conlin PR. Web-based care management in patients with poorly controlled diabetes. Diabetes Care. 2005;2005(7):1624–1629. doi: 10.2337/diacare.28.7.1624. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Nunn E, King B, Smart C, Anderson D. A randomized controlled trial of telephone calls to young patients with poorly controlled type 1 diabetes. Pediatr Diabetes. 2006;2006(5):254–259. doi: 10.1111/j.1399-5448.2006.00200.x. [DOI] [PubMed] [Google Scholar]
- 79.Orr PM, McGinnis MA, Hudson LR, Coberley SS, Crawford A, Clarke JL, Goldfarb NI. A focused telephonic nursing intervention delivers improved adherence to A1c testing. Dis Manag. 2006;2006(5):277–283. doi: 10.1089/dis.2006.9.277. [DOI] [PubMed] [Google Scholar]
- 80.Palmas W, Teresi J, Weinstock RS, Shea S. Acceptability to primary care providers of telemedicine in diabetes case management. J Telemed Telecare. 2008;2008(6):306–308. doi: 10.1258/jtt.2008.080410. [DOI] [PubMed] [Google Scholar]
- 81.Quinn CC, Clough SS, Minor JM, Lender D, Okafor MC, Gruber-Baldini A. WellDoc mobile diabetes management randomized controlled trial: change in clinical and behavioral outcomes and patient and physician satisfaction. Diabetes Technol Ther. 2008;2008(3):160–168. doi: 10.1089/dia.2008.0283. [DOI] [PubMed] [Google Scholar]
- 82.Ralston JD, Revere D, Robins LS, Goldberg HI. Patients' experience with a diabetes support programme based on an interactive electronic medical record: qualitative study. BMJ. 2004;328(7449):1159. doi: 10.1136/bmj.328.7449.1159. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Ralston JD, Hirsch IB, Hoath J, Mullen M, Cheadle A, Goldberg HI. Web-based collaborative care for type 2 diabetes: a pilot randomized trial. Diabetes Care. 2009;2009(2):234–239. doi: 10.2337/dc08-1220. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Rami B, Popow C, Horn W, Waldhoer T, Schober E. Telemedical support to improve glycemic control in adolescents with type 1 diabetes mellitus. Eur J Pediatr. 2006;2006(10):701–705. doi: 10.1007/s00431-006-0156-6. [DOI] [PubMed] [Google Scholar]
- 85.Rossi MC, Nicolucci A, Pellegrini F, Bruttomesso D, Bartolo PD, Marelli G, Dal Pos M, Galetta M, Horwitz D, Vespasiani G. Interactive diary for diabetes: a useful and easy-to-use new telemedicine system to support the decision-making process in type 1 diabetes. Diabetes Technol Ther. 2009;2009(1):19–24. doi: 10.1089/dia.2008.0020. [DOI] [PubMed] [Google Scholar]
- 86.Rutten GE, Maaijen J, Valkenburg AC, Blankestijn JG, De Valk HW. The Utrecht Diabetes Project: telemedicine support improves GP care in Type 2 diabetes. Diabet Med. 2001;2001(6):459–463. doi: 10.1046/j.1464-5491.2001.00491.x. [DOI] [PubMed] [Google Scholar]
- 87.Sarkar U, Handley MA, Gupta R, Tang A, Murphy E, Seligman HK, Shojania S, Schillinger D. Use of an interactive, telephone-based self-management support program to identify adverse events among ambulatory diabetes patients. J Gen Intern Med. 2007;2007(4):459–465. doi: 10.1007/s11606-007-0398-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Sevick MA, Zickund S, Korytkowski M, Piriano B, Sereika S, Mihalko S, Snetselaar L, Stumbo P, Hausmann L, Ren D, Marsh R, Sakraida T, Gibson J, Safaien M, Starrett TJ, Burke LE. Design, feasibility, and acceptability of an intervention using personal digital assistant-based self-monitoring in managing type 2 diabetes. Contemp Clin Trials. 2008;2008(3):396–409. doi: 10.1016/j.cct.2007.09.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Smith AC, Batch J, Lang E, Wootton R. The use of online health techniques to assist with the delivery of specialist paediatric diabetes services in Queensland. J Telemed Telecare. 2003;9(Suppl 2):54–57. doi: 10.1258/135763303322596273. [DOI] [PubMed] [Google Scholar]
- 90.Smith SA, Shah ND, Bryant SC, Christianson TJ, Bjornsen SS, Giesler PD, Krause K, Erwin PJ, Montori VM Evidens Research Group. Chronic care model and shared care in diabetes: randomized trial of an electronic decision support system. Mayo Clin Proc. 2008;2008(7):747–757. doi: 10.4065/83.7.747. [DOI] [PubMed] [Google Scholar]
- 91.Starren J, Tsai C, Bakken S, Aidala A, Morin PC, Hilliman C, Weinstock RS, Goland R, Teresi J, Shea S IDEATel Consortium. The role of nurses in installing telehealth technology in the home. Comput Inform Nurs. 2005;2005(4):181–189. doi: 10.1097/00024665-200507000-00004. [DOI] [PubMed] [Google Scholar]
- 92.Thiebaud P, Demand M, Wolf SA, Alipuria LL, Yes Q, Gutierrez PR. Impact of disease management on utilization and adherence with drugs and tests: the case of diabetes treatment in Florida: a Healthy State (FAHS) program. Diabetes Care. 2008;2008(9):1717–1722. doi: 10.2337/dc07-2118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Timmerberg BD, Wurst J, Patterson J, Spaulding RJ, Belz NE. Feasibility of using videoconferencing to provide diabetes education: a pilot study. J Telemed Telecare. 2009;2009(2):95–97. doi: 10.1258/jtt.2008.080813. [DOI] [PubMed] [Google Scholar]
- 94.Trief PM, Teresi JA, Izquierdo R, Morin PC, Goland R, Field L, Eimicke JP, Brittain R, Starren J, Shea S, Weinstock RS. Psycho-social outcomes of telemedicine case management for elderly patients with diabetes: the randomized IDEATel trial. Diabetes Care. 2007;2007(5):1266–1268. doi: 10.2337/dc06-2476. [DOI] [PubMed] [Google Scholar]
- 95.Trief PM, Sandberg J, Izquierdo R, Morin PC, Shea S, Brittain R, Feldhousen EB, Weinstock RS. Diabetes management assisted by telemedicine: patient perspectives. Telemedicine J E Health. 2008;2008(7):647–655. doi: 10.1089/tmj.2007.0107. [DOI] [PubMed] [Google Scholar]
- 96.Tsang MW, Mok M, Kam G, Jung M, Tang A, Chan U, Chu CM, Li I, Chan J. Improvement in diabetes control with a monitoring system based on a hand-held, touch-screen electronic diary. J Telemed Telecare. 2001;2001(1):47–50. doi: 10.1258/1357633011936138. [DOI] [PubMed] [Google Scholar]
- 97.Tudiver F, Wolff LT, Morin PC, Teresi J, Palmas W, Starren J, Shea S, Weinstock RS. Primary care providers' perceptions of home diabetes telemedicine care in the IDEATel Project. J Rural Health. 2007;2007(1):55–61. doi: 10.1111/j.1748-0361.2006.00068.x. [DOI] [PubMed] [Google Scholar]
- 98.Wagnild G, MacCart JG, Mitchell S, Tyabah K, Leenknecht C, Meszaros JF. A telecommunications intervention for frontier patients with diabetes. Telemed J E Health. 2008;2008(8):793–800. doi: 10.1089/tmj.2007.0133. [DOI] [PubMed] [Google Scholar]
- 99.Whitlock WL, Brown A, Moore K, Pavliscsak H, Dingbaum A, Lacefield D, Buker K, Xenakis S. Telemedicine improved diabetic management. Mil Med. 2000;165(8):579–584. [PubMed] [Google Scholar]
- 100.Whittaker SL, Adkins S, Phillips R, Jones J, Horsley MA, Kelley G. Success factors in the long-term sustainability of a telediabetes programme. J Telemed Telecare. 2004;10(2):84–88. doi: 10.1258/135763304773391512. [DOI] [PubMed] [Google Scholar]
- 101.Wilbright WA, Birke JA, Patout CA, Varnado M, Horswell R. The use of telemedicine in the management of diabetes-related foot ulceration: a pilot study. Adv Skin Wound Care. 2004;17(5):232–238. doi: 10.1097/00129334-200406000-00012. [DOI] [PubMed] [Google Scholar]
- 102.Yip MP, Mackenzie A, Chan J. Patient satisfaction with telediabetes education in Hong Kong. J Telemed Telecare. 2002;16(1):48–51. doi: 10.1258/1357633021937460. [DOI] [PubMed] [Google Scholar]
- 103.Farmer A, Gibson OJ, Tarassenko L, Neil A. A systematic review of telemedicine interventions to support blood glucose self-monitoring in diabetes. Diabet Med. 2005;22(10):1372–1378. doi: 10.1111/j.1464-5491.2005.01627.x. [DOI] [PubMed] [Google Scholar]
- 104.Klonoff DC. The personalized medicine for diabetes meeting summary report. J Diabetes Sci Technol. 2009;3(4):677–679. doi: 10.1177/193229680900300410. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Nijland N, Cranen K, Boer H, van Gemert-Pijnen JE, Seydel ER. Patient use and compliance with medical advice delivered by a web-based triage system in primary care. J Telemed Telecare. 2009;16(1):8–11. doi: 10.1258/jtt.2009.001004. [DOI] [PubMed] [Google Scholar]
- 106.Klonoff DC. Benefits and limitations of self-monitoring of blood glucose. J Diabetes Sci Technol. 2007;1(1):130–132. doi: 10.1177/193229680700100121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Kaplan B. Evaluating informatics applications–some alternative approaches: theory, social interactionism, and call for methodological pluralism. Int J Med Inform. 2001;64(1):39–56. doi: 10.1016/s1386-5056(01)00184-8. [DOI] [PubMed] [Google Scholar]