Abstract
Background
Childhood obesity is a growing problem, particularly in rural, Louisiana school children. Traditionally, school-based obesity prevention programs have used a primary prevention approach. Finding methods to deliver secondary prevention programs to large numbers of students without singling out overweight students has been a challenge. An innovative approach to achieving this goal is through use of an Internet intervention targeted toward a student's weight status. This article describes the Louisiana (LA) Health Internet intervention, including the student Web site, the Internet counselor Web site, and the Internet counseling process.
Method
The LA Health Internet intervention had separate interfaces for students and Internet counselors. The main features of the student site were behavioral weight loss lessons, lesson activities, chat with an Internet counselor, and email. The Internet counselor site contained these same features, plus a student directory and various means of obtaining student information to guide counseling. Based on their baseline weight status, students received lessons and counseling that promoted either weight loss or weight maintenance. Intervention was delivered during class time, and teachers scheduled Internet counseling sessions with intervention personnel.
Results
The LA Health Internet intervention was initially implemented within 14 schools; 773 students were granted access to the site. From Fall 2007 to Spring 2009, 1174 hours of Internet counselor coverage was needed to implement the Internet counseling component of this intervention
Conclusion
The LA Health Internet intervention is an innovative and feasible method of delivering a secondary prevention program within a school setting to large numbers of students.
Keywords: children, counseling, Internet, obesity, school, weight management
Introduction
Over the last 20 years, the prevalence of childhood obesity has been increasing rapidly. Children in rural Louisiana are particularly susceptible to this epidemic.1 To combat this growing problem, primary and secondary obesity prevention approaches are being used. Primary prevention programs seek to prevent the onset of obesity. These programs typically employ environmental approaches and are implemented on the family, school, organizational, or policy level. Secondary prevention programs aim to detect and treat obesity or risk for obesity. These programs are implemented most commonly at the individual level and target only those at risk (i.e., individuals who are overweight or obese).
Childhood obesity prevention programs are commonly implemented within school settings. These school-based programs typically use a primary prevention approach that targets all students in the school environment.2 A common challenge to implementing secondary prevention programs within schools is finding a way to provide individualized support to large numbers of students in a manner that overweight children will not be singled out. Consequently, secondary prevention programs for children have been commonly reserved for clinical settings, e.g., pediatric medical offices or clinical research centers.
A novel way to deliver secondary intervention programs within a school-based obesity prevention program is via Internet intervention, as described by Williamson et al.3 Internet interventions can be an effective tool for both children and adults to alter dietary behavior, increase physical activity, and lose weight.4 Furthermore, addition of an Internet counselor to an educational Web site improves weight loss outcomes.5,6 In addition, the anonymity of the Internet may be attractive to students who are embarrassed about issues such as weight or appearance.7
A barrier to the effectiveness of Internet interventions is a decrease in utilization over time. More frequent log-ins are associated with better outcomes; however, over time, log-in rates decrease.8,9 Williamson and colleagues10 observed that delivering an Internet intervention within a school setting may help overcome the phenomenon of decreased utilization over time. This method allows all children within a school to have an equal opportunity to access the site, eliminating disparities that may be associated with a lack of Internet access at home. In addition, delivery within a school setting may be helpful for sustaining utilization because students are brought to the site, do not have to remember to access the site at home, and do not have to make decisions between accessing the site and participating in competing after-school activities.
The Louisiana (LA) Health study is a randomized control trial that compared the effectiveness of two school-based obesity prevention programs—a primary prevention program and a primary plus secondary prevention program—on inappropriate weight gain in rural, Louisiana school children. The design and methods of this 28-month study have been reported elsewhere.3 The secondary prevention program used an Internet intervention that placed emphasis on behavior modification approaches. This Internet intervention contained lessons on healthy eating and regular physical activity. In addition, students were allowed to communicate with an Internet counselor synchronously using chat and asynchronously using email.
The LA Health Internet intervention evolved from findings of two previous studies: HIPTeens9,11 and Wise Mind.12 HIPTeens evaluated the efficacy of an Internet-based, secondary prevention intervention for weight loss in overweight, African-American girls. In comparison to a control condition, girls with access to the Internet-based behavioral weight loss intervention lost more weight and body fat at 6 months but these differences were not maintained at 18 months.9 Wise Mind tested an environmental program for weight gain prevention in which an Internet intervention was delivered to elementary school students.12 This 2-year weight gain prevention program was associated with a reduction in caloric intake, dietary fat intake, and increased physical activity but had no effect on body weight, relative to a control arm.
This article describes the LA Health Internet intervention, including the student Web site, the Internet counselor Web site, and the Internet counseling process. In addition, information on the time and personnel required for the implementation of Internet counseling for this intervention is discussed.
Methods
The methods of the larger LA Health study have been described previously.3 Briefly, the LA Health intervention started in February 2007 and ended in May 2009. Thirty-three schools were assigned randomly to one of three conditions: primary prevention, primary prevention plus secondary prevention, or no-intervention control. Participants included school children initially enrolled in grades four to six who consented to participation in the study. No students were excluded based on their baseline weight or body mass index (BMI) percentile. Participation was voluntary, and not all students in a class participated in the study. Only the primary plus secondary prevention condition contained the LA Health intervention discussed in this article.
Development of the LA Health Internet Intervention
The aim of the LA Health Internet intervention was to treat and prevent inappropriate weight gain in rural, Louisiana school children using a targeted, secondary prevention approach. The Web site utilized educational lessons and brief behavioral counseling to teach behavioral weight management skills. The LA Health Internet intervention Web site had different user interfaces: one for students and one for Internet counselors. The Web site was developed by a multidisciplinary team of researchers with educational backgrounds in psychology, public health, nutrition, exercise and sport science, and computer science.
The LA Health Web site was based on Web sites used in the two previously reported pilot studies: HIPTeens and Wise Mind. Lessons were designed to be appropriate for the age level targeted in this study. Post-hoc analyses of lesson content indicated a Flesch–Kincaid grade level of 5.6. Because lessons covered a two and a half school year period with students in the fourth to sixth grades during the first year and in the sixth to eighth grades in the last year, lessons were written at a level appropriate for the given sample.
Using data obtained through in-person baseline assessments, students were categorized as either normal weight (less than 85th BMI percentile) or overweight/obese (at or above 85th BMI percentile). This cut point was based on previously established guidelines for screening populations for obesity.13 According to these guidelines, children above the 85th percentile are classified as overweight and children above the 95th percentile are classified as obese. Because the Internet intervention was part of a population-based secondary prevention program aimed to detect and treat obesity or risk for obesity, we used the 85th percentile cut point as a means of identifying those at greater risk for obesity who may benefit from brief behavioral weight loss counseling.
Information provided within lessons differed based on the student's baseline weight category (i.e., normal weight or overweight/obese). Normal weight children received information on nutrition and exercise designed to promote weight maintenance. Overweight children received information designed to promote weight loss. Students in both weight categories had access to the same Web site containing a similar format, appearance, and lesson topics. The Web site appeared identical and students were not told whether they were receiving a weight loss or weight maintenance intervention. This was designed to help avoid singling out overweight students.
LA Health Student Web Site Components
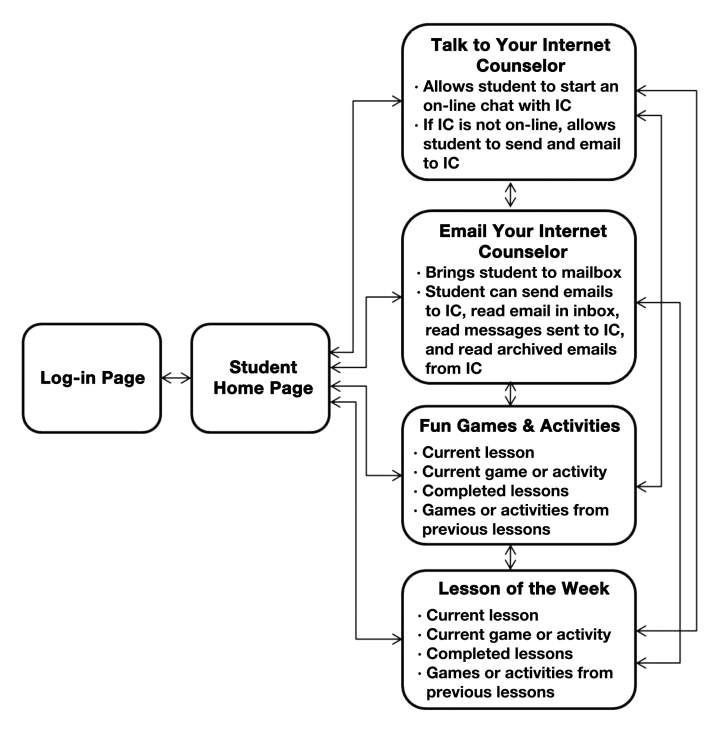
Figure 1 displays the components of the student Web site. A description of each component is described here.
Figure 1.
The LA Health student Web site architecture. IC, Internet counselor.
Log-in Page
When students went to the site Uniform Resource Locator (URL), they were brought to a log-in page. Each student was provided with a unique id and password that allowed access to the site.
Home Page
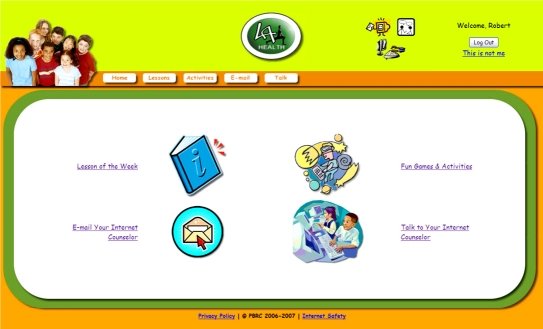
Once students logged onto the LA Health Web site, they were brought to a colorful, age-appropriate home page (Figure 2) containing images and links for each of the four sections of the site: “Lesson of the Week,” “Fun Games and Activities,” “Talk to Your Internet Counselor,” and “Email Your Internet Counselor.” All pages on the LA Health Web site included a tool bar with links to the home page and each of these four sections so students could navigate across site components easily. In addition, a footer on the home page contained three additional links to provide students with information on Internet safety, the privacy policy of the LA Health Web site, and teacher announcements.
Figure 2.
Student home page.
Lesson of the Week and Fun Games and Activities
The Lesson of the Week link and the Fun Games and Activities link brought students to the same Web page (Figure 3). This page allowed students to view current and any previous lessons. Each lesson ended with a five-question quiz. Students received immediate feedback on each response and a quiz score (Figure 4).
Figure 3.
Student lessons and activities page.
Figure 4.
Student quiz question with feedback.
Games or activities were provided for some lessons. Examples included choosing healthy items to put in a grocery cart, choosing healthy snacks to take on vacation, and choosing accurate statements regarding goal setting and energy balance. Students were not allowed to access activities until after they completed the lesson associated with the activity. If students did not complete a lesson, they were prompted to complete the lesson before they could access the activity.
Talk to Your Internet Counselor
Students could communicate with an Internet counselor synchronously via an on-line chat using the Talk to Your Internet Counselor link. When selecting this link, students were notified if an Internet counselor was on-line. If the Internet counselor was on-line, students could initiate a chat session with the counselor. If the Internet counselor was not on-line, students were prompted to send an email to their Internet counselor so any questions or needs they had could be addressed. All chats were one on one and the student could only see his or her information.
Email Your Internet Counselor
Students were able to communicate with an Internet counselor asynchronously using the Email Your Internet Counselor link. This link brought students to a LA Health inbox. Students could post a new message to their Internet counselor, read any new or old messages received from their Internet counselor, and view messages sent previously to their Internet counselor. When a student sent a new message to their Internet counselor, an automated reply was sent immediately to the student to notify the student that the counselor would respond within the next one to two school days.
LA Health Internet Counselor Web Site Components
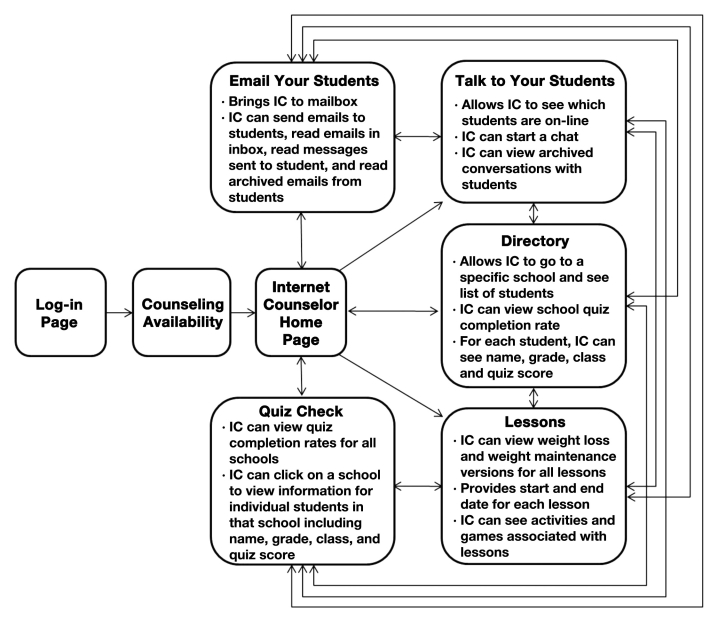
Internet counselors had access to a Web site that differed from the student site. Figure 5 displays the different elements of the counselor Web site.
Figure 5.
The LA Health Internet counselor Web site architecture. IC, Internet counselor.
Log-in Page
After signing on to the site URL, counselors were brought to a log-in page. Here they entered a unique id and password to gain site access.
Counseling Availability
After logging onto the site, counselors were brought to a Web page that required them to select the school(s) to which they would provide Internet counseling. This notified students in particular schools that their Internet counselor was on-line and available to chat. Counselors could also select an option to provide no Internet counseling. If a counselor chose not to be available to students, students were unaware a counselor was on-line and no chat sessions were initiated.
Home Page
Once counselors selected an option for their availability, they were brought to the home page. From the home page, counselors had five options: “Directory,” “Talk to Your Students,” “Email Your Students,” “Lessons,” and “Quiz Check.”
Directory
The student directory allowed counselors to view student information, including quizzes completed, grades, treatment arm, and age.
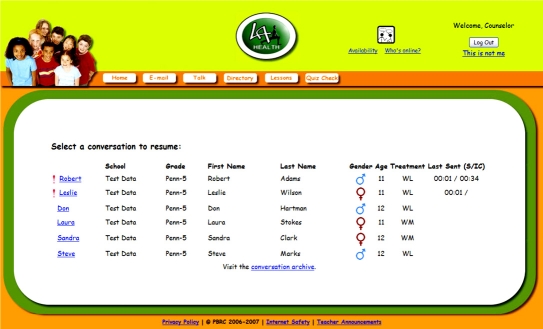
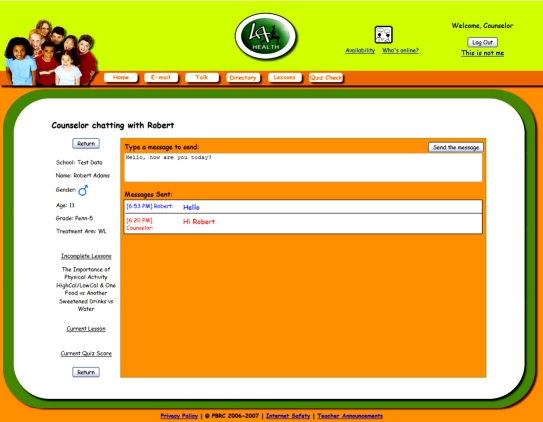
Talk to Your Students
This option allowed counselors to view which students were on-line and start a one-on-one chat with a student (Figure 6). Counselors could communicate with more than one student at a time using separate chats. When chatting with students, counselors could review the following student information: name, school, gender, age, grade in school, treatment arm (weight loss or weight maintenance), incomplete lessons, current lesson, and current quiz score (Figure 7). Using this information, counselors were able to provide individualized counseling that was targeted toward the student's needs and was age appropriate. If a student had not completed lessons, counselors encouraged students to complete a lesson before chatting.
Figure 6.
Internet counselor Web page displaying information for students available for chat. Note that this shows a snapshot of a test page. No information from actual students is shown. WL, weight loss condition; WM, weight maintenance condition.
Figure 7.
Internet counselor Web page showing chat session for a student along with student information.
Email Your Students
This option allowed counselors to communicate with students asynchronously. Counselors could access a student directory, send a new message to a student, read any messages received from students, and view previous email exchanges. When emailing students, counselors could obtain the same student information as described previously with chat. When a counselor received a message in their LA Health inbox, an email notification was sent to the counselor's main email to notify the counselor to check their LA Health mailbox. This reminder helped ensure that messages sent by students were responded to promptly.
Lessons
This link allowed counselors to review lessons the students received. This facilitated discussion and allowed the counselor to quickly review information about the session before and during communication with students.
Quiz Check
The quiz link allowed counselors to see the percentage of students within each school that completed a particular lesson. In addition, counselors could access students' quiz scores.
Implementation of the LA Health Internet Intervention
The LA Health Internet intervention was delivered during class time. LA Health staff trained classroom teachers on how to access, navigate, and use the Web site. Teachers were provided with calendars on when to deliver lessons and information on how they could use the Web site within their curriculum to meet curriculum requirements. LA Health staff served as a consultant to teachers and trained any new teachers when there was staff turnover. Teachers were then responsible for teaching their students how to access the site, use the site, and communicate with Internet counselors.
A new lesson was placed on the site approximately every 2 weeks, with accommodations made for school holidays and testing periods. During the first week of the lesson, teachers introduced the lesson topic to all students and covered printed material on the topic in class. Classroom lessons focused on behaviors associated with weight gain prevention. During the second week, teachers provided students with class time to access the LA Health Web site, complete lessons and quizzes, and communicate with an Internet counselor. Thirty-two unique lessons were placed on the site (see Table 1). Five of these lessons were repeated in the final semester to review key weight management concepts.
Table 1.
LA Health Lesson Topics along with Date on the Site
| Lesson topic | Date on site |
|---|---|
| Overview of Health Outcomes | 11/29/2006 |
| Reducing Sedentary Activity | 04/01/2007 |
| The Importance of Physical Activity | 04/17/2007 |
| High Calorie/Low Calorie and One Food vs Another | 05/01/2007 |
| Sweetened Drinks vs Water | 08/25/2007 |
| Energy Balance | 09/17/2007 |
| How to Set Goals | 10/01/2007 |
| Portion Sizes/Portion Distortion | 10/15/2007 |
| Tips on Increasing Physical Activity | 11/05/2007 |
| Eat Five-a-Day the Color Way | 11/12/2007 |
| Family Fun Indoor Activities | 12/03/2007 |
| Healthy Holiday Snacks and Activities | 12/10/2007 |
| Aerobic Exercise | 01/07/2008 |
| Be a Fast-Food Survivor | 01/21/2008 |
| Fat in Foods | 02/04/2008 |
| Warm-up/Cool Down and Injuries | 02/18/2008 |
| Stretching | 03/03/2008 |
| Let's Talk about Fried Foods | 04/07/2008 |
| Purpose of Various Activities | 04/21/2008 |
| Fun Facts about Fruits and Veggies | 05/05/2008 |
| How Much TV Do You Watch? | 09/08/2008 |
| High Fiber Foods | 09/22/2008 |
| Eating Healthy with Your Friends | 10/06/2008 |
| Planning Ahead for Get-Togethers | 10/20/2008 |
| Intro to Food Labels | 11/03/2008 |
| Getting the Family on Board | 11/17/2008 |
| Aerobic Activities for the Whole Family | 12/01/2008 |
| Planning Ahead for Physical Activity/Snacks on the Go | 01/19/2009 |
| Keys to Maintaining an Active Lifestyle | 01/05/2009 |
| Planning Ahead for a Healthy Breakfast | 01/19/2009 |
| Portion Sizes/Portion Distortion | 02/01/2009 |
| Healthy Cues | 02/16/2009 |
| Ways to Motivate Yourself to Engage in Physical Activity | 03/02/2009 |
| Energy Balance | 03/16/2009 |
| High Cal/Low Cal and One Food vs Another | 04/20/2009 |
| Let's Talk about Fried Foods | 04/27/2009 |
| Overview of Health Outcomes | 05/04/2009 |
Internet counselors served two main purposes in the LA Health Internet intervention. First, they provided personalized nutrition and physical activity guidance to students. Counseling focused on behavioral principles for weight management that were presented in lessons. Healthy eating and increasing physical activity were encouraged. Second, Internet counselors prompted students to read lessons and complete quizzes. All communication between Internet counselors and students occurred within the LA Health Web site through either chat sessions or email.
The LA Health Internet counselors had bachelor (n = 4), master (n = 5), or doctoral (n = 2) degrees in nutrition, health behavior, psychology, or exercise and sport science. A doctoral level clinical psychologist supervised all counselors. Internet counselors were required to attend a training session about nutrition and physical activity recommendations for children, handling frequently asked questions that children were predicted to have, and how to discuss topics that would be presented to children in lessons (e.g., decreasing the consumption of sugar-sweetened beverages, eating a wider variety of fruits and vegetables, and finding ways to be physically active with family and friends). Internet counselors also received training on effective goal setting, stages of change, and motivational interviewing techniques. Materials used in this seminar were compiled and disseminated to each counselor for reference while communicating with students.
Ongoing training and supervision sessions ensured that Internet counselors were delivering counseling as intended, reinforcing positive eating and physical behaviors, and providing counseling in a manner that was sensitive to weight issues. A protocol was developed to handle situations in which possible eating disorder or depressive symptoms were observed during Internet counseling. If concerns were observed, the school counselor or principal would be contacted to ensure that students had access to the appropriate resources. No situations emerged that required the school to be contacted. Changes were made in the way Internet counseling was scheduled during the course of the study. In the spring of 2007, there was a mixed method of scheduling. Internet counselors were assigned specific times to watch the site and provide counseling if a class logged on, and schools also had the opportunity to schedule specific appointment times. In subsequent semesters, a scheduling system was used in which schools set appointments for Internet counseling. This schedule reduced the amount of time Internet counselors had to reserve for counseling and also helped ensure that there was an appropriate student-to-counselor ratio. Each month teachers were given calendars with the dates and times of their assigned Internet counseling sessions and were instructed to notify their school coordinator if any scheduling conflicts arose. Teachers were advised that the Internet counseling sessions were seen as “appointments” in which Internet counseling staff were scheduled to be present.
Results
At the start of LA Health, 14 schools had access to the LA Health Internet intervention. For 12 of the 14 schools, information was obtained on the number of students who were invited to participate in the larger LA Health study. Between 26 and 52% (M = 41%) of students invited to participate provided parental consent and assent to participate in the larger LA Health intervention, be part of the study condition to which their school was randomized (control, primary, or primary plus secondary condition), provide measurements of weight and body fat percentage, and complete surveys. The 14 schools that received the LA Health Internet intervention had between 33 and 103 students [M = 55; standard deviation (SD) = 19.78] participating in the LA Health intervention. Initially, 773 students were granted access to the site. Of these, 763 accessed the site at least once.
Students granted access to the LA Health Internet intervention had a mean age of 10.5 years (SD = 1.2). Fifty-seven percent (n = 443) were female. Regarding ethnicity, 68.7% (n = 531) were African-American, 29.6% were Caucasian (n = 229), 0.9% was Hispanic (n = 7), and 0.8% (n = 6) was of another ethnicity. Students had a mean BMI percentile of 68.2 (SD = 29.5) and a mean body fat percentage of 24.4 (SD = 11.1). Forty-eight percent (n = 449) had a BMI percentile greater than 85% and were considered overweight or obese.
During the 2007–2008 school year, when classes began using a scheduling system for Internet counseling, teachers scheduled 443 LA Health Internet counseling class sessions. These sessions ranged from 30 to 120 minutes (M = 51.55 minutes; SD = 15.39). For 37 of these sessions, two counselors were scheduled due to a large class size. A total of 864.38 hours of Internet counselor time was reserved to provide Internet counseling for these sessions.
During the 2008–2009 school year, 314 Internet counseling class sessions were scheduled. The session duration ranged from 25 to 129 minutes (M = 56.13 minutes; SD = 19.90). For 19 of these sessions, two counselors were present. A total of 309.42 hours of Internet counselor time was reserved to deliver Internet counseling.
Conclusion
The LA Health Internet intervention was a secondary prevention program aimed at reducing inappropriate weight gain in students in the fourth to sixth grades. The Web site contained separate sites for students and Internet counselors. The main features of the student site were lessons, lesson activities, chat with an Internet counselor, and email. The Internet counselor site contained these same features, plus a student directoryand various means of obtaining student information to guide counseling. Internet counselors provided individualized weight management support to students using both synchronous and asynchronous communication. Counseling and lesson material were targeted toward a student's baseline weight status. Overweight students received information on weight loss, whereas normal weight students received information on weight maintenance.
Using this novel secondary prevention approach, 763 students were reached through the LA Health Internet intervention. From Fall 2007 to Spring 2009, 1174 hours of Internet counselor coverage was needed to implement the Internet counseling component of this intervention.
Information collected from 12 of the 14 schools randomized to the Internet counseling condition indicated that between 26 and 52% (M = 41%) of students invited to participate in LA Health provided parental consent and assent to participate in the larger LA Health intervention. It should be noted that these students were agreeing to be part of the study condition to which their school was randomized (control, primary, or primary plus secondary condition), provide measurements of weight and body fat percentage, and complete surveys prior to having knowledge that they would receive the LA Health Internet intervention. Thus, caution should be used in interpreting these numbers in the context of this article as these numbers do not reflect the percentage of students interested in participating in the LA Health Internet intervention.
The fact that the LA Health Internet intervention was implemented within the context of a larger research study could influence the adoption and implementation of this intervention when delivered outside of a research study. First, LA Health study staff obtained and entered student weights. If implemented within a school setting, school staff would need to obtain and enter these weights. Second, not all students chose to participate in the LA Health study. In most instances, less than half of a class participated. Teachers appeared to approach this in different ways. Some integrated LA Health into their class curriculum, delivered material to all students regardless of whether they were in LA Health or not, and brought all students to the computer laboratory to use the LA Health Internet intervention. When in the computer laboratory, students not in LA Health could read lessons on the Web site and engage in lesson activities but could not participate in Internet counseling. Other teachers seemed to add LA Health to their class' current curriculum and divide their class instruction between those in LA Health and those not in LA Health. Thus, they covered LA Health topics only with LA Health students; this was in addition to topics already covered with their class. Adding an additional teaching component to their curriculum and separating instruction between LA Health and non-LA Health study participants may have increased teacher burden and influenced Web site usage negatively. In the current study, we did not have data to assess this hypothesis. However, if this hypothesis is correct, having a school policy in place that supports implementation of the LA Health Internet intervention as part of a school curriculum presented to all students could potentially improve the reach, adoption, and implementation of this intervention.
The LA Health Internet intervention provides an important contribution to research in the areas of school-based obesity prevention programs and Internet approaches to weight management. LA Health is unique from previous school-based obesity prevention studies in that an Internet intervention was used as a means of delivering a secondary prevention obesity program with individualized counseling to school children. In addition, LA Health is also unique from previous weight management Internet interventions in that Internet intervention was delivered in a school setting in conjunction with classroom instruction and lessons and counseling were targeted toward the student's weight status. Future work will compare the effectiveness of a primary prevention program to the primary plus secondary prevention program, which contains the LA Health Internet Intervention described in this article, on inappropriate weight gain. While the design of our study does not allow us to tease out the effects of Internet intervention alone, we will be able to assess whether there is a dose–response effect among site usage, change in body fat percentage, and change in BMI percentile in students in the primary plus secondary prevention condition, as well as assess predictors of site usage.
Acknowledgments
This project was supported by the National Institute for Child Health and Human Development of the National Institutes of Health (R01 HD048483) and the U.S. Department of Agriculture (58-6435-4-90). This work was partially supported by Nutrition Obesity Research Center Grant P30DK072476 entitled “Nutritional Programming: Environmental and Molecular Interactions” sponsored by the National Institute of Diabetes and Digestive and Kidney Diseases. Corby K. Martin is supported by National Institutes of Health Grant K23-DK068052. The clinical trial number for this project is NCT00289315.
Abbreviations
- BMI
body mass index
- LA
Louisiana
- SD
standard deviation
- URL
Uniform Resource Locator
References
- 1.Williamson DA, Champagne CM, Han H, Harsha D, Martin CK, Newton RL, Ryan DH, Sothern MS, Stewart TM, Webber LS. Increased obesity in children living in rural communities of Louisiana. Int J Pediatr Obes. 2009;4(3):160–165. doi: 10.1080/17477160802596148. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Summerbell CD, Waters E, Edmunds LD, Kelly S, Brown T, Campbell KJ. Interventions for preventing obesity in children. Cochrane Database Syst Rev. 2005;(3):CD001871. doi: 10.1002/14651858.CD001871.pub2. [DOI] [PubMed] [Google Scholar]
- 3.Williamson DA, Champagne CM, Harsha D, Han H, Martin CK, Newton R, Jr, Stewart TM, Ryan DH. Louisiana (LA) Health: Design and methods for a childhood obesity prevention program in rural schools. Contemp Clin Trials. 2008;29(4):783–795. doi: 10.1016/j.cct.2008.03.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Norman GJ, Zabinski MF, Adams MA, Rosenberg DE, Yaroch AL, Atienza AA. A review of eHealth interventions for physical activity and dietary behavior change. Am J Prev Med. 2007;33(4):336–345. doi: 10.1016/j.amepre.2007.05.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Tate DF, Jackvony EH, Wing RR. Effects of Internet behavioral counseling on weight loss in adults at risk for type 2 diabetes: a randomized trial. JAMA. 2003;289(14):1833–1836. doi: 10.1001/jama.289.14.1833. [DOI] [PubMed] [Google Scholar]
- 6.Tate DF, Wing RR, Winett RA. Using Internet technology to deliver a behavioral weight loss program. JAMA. 2001;285(9):1172–1177. doi: 10.1001/jama.285.9.1172. [DOI] [PubMed] [Google Scholar]
- 7.Zabinski MF, Celio AA, Wilfley DE, Taylor CB. Prevention of eating disorders and obesity via the internet. Cogn Behav Ther. 2003;32(3):137–150. doi: 10.1080/16506070310000939. [DOI] [PubMed] [Google Scholar]
- 8.Wangberg SC, Bergmo TS, Johnsen JK. Adherence in Internet-based interventions. Patient Prefer Adherence. 2008;2:57–65. [PMC free article] [PubMed] [Google Scholar]
- 9.Williamson DA, Walden HM, White MA, York-Crowe E, Newton RL, Jr, Alfonso A, Gordon S, Ryan D. Two-year internet-based randomized controlled trial for weight loss in African-American girls. Obesity (Silver Spring) 2006;14(7):1231–1243. doi: 10.1038/oby.2006.140. [DOI] [PubMed] [Google Scholar]
- 10.Williamson DA, Walden H, York-Crowe E, Stewart TM. Internet-based treatment for pediatric obesity. In: Sothern M, Gordon ST, Von Almen TK, editors. Handbook of pediatric obesity: clinical management. Boca Raton, F: CRC/Taylor & Francis; 2006. p. 402. [Google Scholar]
- 11.Williamson DA, Martin PD, White MA, Newton R, Walden H, York-Crowe E, Alfonso A, Gordon S, Ryan D. Efficacy of an internet-based behavioral weight loss program for overweight adolescent African-American girls. Eat Weight Disord. 2005;10(3):193–203. doi: 10.1007/BF03327547. [DOI] [PubMed] [Google Scholar]
- 12.Williamson DA, Copeland AL, Anton SD, Champagne C, Han H, Lewis L, Martin C, Newton RL, Jr, Sothern M, Stewart T, Ryan D. Wise Mind project: a school-based environmental approach for preventing weight gain in children. Obesity (Silver Spring) 2007;15(4):906–917. doi: 10.1038/oby.2007.597. [DOI] [PubMed] [Google Scholar]
- 13.Himes JH, Dietz WH. Guidelines for overweight in adolescent preventive services: recommendations from an expert committee. The Expert Committee on Clinical Guidelines for Overweight in Adolescent Preventive Services. Am J Clin Nutr. 1994;59(2):307–316. doi: 10.1093/ajcn/59.2.307. [DOI] [PubMed] [Google Scholar]