Abstract
Direct spending on diabetes, already exceeding $118 billion, is forecast to reach $336 billion in 2034, driven by newly diagnosed cases secondary to an aging, increasingly sedentary, obese population and the advent of comorbidities, particularly cardiovascular complications affecting more than one-third of persons with diabetes. Traditional, directive, and fragmented approaches to patient management based on acute intervention and specialty care has been unable to stem the impending tsunami of diabetes-related complications and costs. Health care reform and the growing shortage of primary care physicians will only exacerbate the situation.
Consumer-centric health care, enabled by digital media and technology, is integral to engagement, self-management, behavior change, and outcomes. It is time for the health care establishment to consider the “other” 360 days per year when a patient is not being seen by a physician.
Keywords: behavior change, consumer-centric collaborative care, consumer engagement, diabetes, disease-centric care, self-management
Situation Analysis: Disease-Centric Care
“The good physician treats the disease; the great physician treats the patient who has the disease.”
Sir William Osler
Despite these words spoken over 100 years ago, the U.S. health care delivery system and its primary stakeholders (i.e., providers, insurers, suppliers, and the government) remain focused on treating the specific complications associated with diabetes rather than preventing its onset or ameliorating its longer-term progression. Internists, cardiologists, nephrologists, and ophthalmologists as well as diabetes educators, dieticians, home care nurses, and others may all interface with patients on a transactional basis without adequate care coordination and transitional management. Insurers focus on the “bottom line” and an annual return on investment for a condition that yields limited near-term economic benefits for preventive practices. Suppliers offer innovative drugs and devices that still require therapeutic optimization, medication adherence, and adequate user literacy to derive full benefits. The government has instituted perverse incentives rewarding specialization rather than primary care and procedures rather than prevention.
The prevalence of diabetes in the United States is 23.6 million people, or 7.8% of the population; nearly 76% of cases are diagnosed.1 The mean and median age of diagnosis continue to decline and approximate 51 years.2 Due to the large number of newly diagnosed patients, 43% have had the condition for less than five years.3 This comparatively short duration, combined with a relatively young age, creates an opportunity for early engagement and behavioral intervention. Conversely, 23% have lived with diabetes for more than 15 years.3 More than 60% of people diagnosed with diabetes are less than 65 years of age, 21% are between 65 and 74, and 18% are greater than 75.4,5 Baby boomers account for a substantial number of the cases. Diabetes-related complications, comorbidities, and thus disease management complexity increase with age and duration.
Not all people with diabetes are alike. They differ not only in terms of medical risk, but also in knowledge and their interest in health engagement, social mindset, self-credibility, beliefs (susceptibility), and motivation. Their psychosocial profile can also vary by their age demographic, timing of medical diagnosis, and/or events and presence/absence of specific comorbidities. Baby boomers in particular have expressed a need for an “active, youthful approach to life.”6
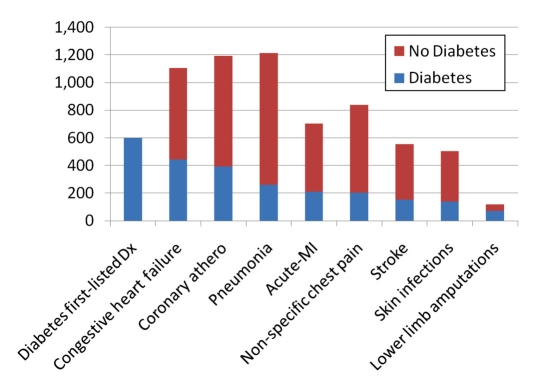
Direct and indirect spending on diabetes totaled $174 billion, with direct spending accounting for two-thirds of the expenditures and being driven by hospitalization.7 In 2004, there were 6.2 million hospital stays among patients with diabetes, listed either as a primary diagnosis or comorbidity (see Figure 1).8 In 2007, there were 10.6 million emergency department visits, of which 46% reportedly led to a hospital admission.9 Many of these admissions and emergency department visits were cardio- vascular and reflect the long-term impact of diabetes and/or hypertension.
Figure 1.
Cause of hospital stays for persons with diabetes.8 Dx, diagnosis; MI, myocardial infarction.
One study suggests that direct spending on diabetes will reach $336 billion in 2034, a near tripling from current levels.10 The increase in Medicare spending is far greater, rising from $45 billion in 2009 to $171 billion in 2034, reflective of the rapidly aging population.10
The Opportunity: Consumer-Centric Collaborative Care
The behavior of patients with diabetes could substantially impact their own clinical, economic, and quality-of-life outcomes. More than 85% of people with type 2 diabetes are overweight; 59% of all adults do no vigorous physical activity in their leisure time.11 The Diabetes Prevention Program found that, after three years, a modest weight loss based on lifestyle intervention (e.g., dietary changes and increased activity) reduced the probability of developing diabetes in high-risk patients by 58%; the 10-year Diabetes Prevention Program Outcomes Study suggests a longer-term reduction of 34%.12 The benefits were especially impactful in those over 60.12
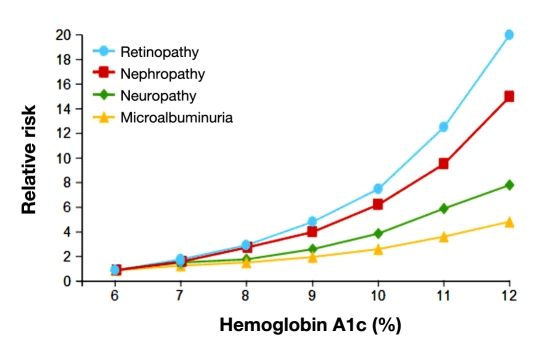
Studies have shown that (a) each 1% absolute reduction in mean hemoglobin A1c levels can reduce the risk of microvascular complications by 40%,1 (b) blood pressure control can reduce the risk cardiovascular complications among persons with diabetes by 33–50% and the risk of microvascular complications by approximately 33%,1 and (c) low-density lipoprotein cholesterol control can reduce cardiovascular complications by 20–50%1 (see Figure 2). Screening for foot care, vision, and vaccination also reduces the complication rate. Diabetes complications can be prevented, delayed, and/or reduced in severity.
Figure 2.
Relative risk of complications in type 1 diabetes.
Given the opportunity, patients and, if possible, their caregivers and families must be engaged to generate favorable longer-term outcomes. Self-management is essential for goal attainment in a highly fragmented, uncoordinated, intervention-oriented health care delivery system.
According to the Agency for Healthcare Research and Quality, patients with diabetes may be asked to make major lifestyle changes; closely monitor symptoms; respond with appropriate actions when symptom levels indicate a problem (e.g., adjust medications; initiate call to health care coach; schedule visits to a primary care physician, certified diabetes educator, registered dietitian, and/or endocrinologist); adhere to medication regimens; and make office visits for lab tests, physical exams, and clinical consultations. Enabling technology potentially has a role for each of these requirements.
The ability of self-management for a patient depends on many factors, including their knowledge; psychosocial mediators such as self-efficacy, attitudes, health beliefs, mood, motivation, and coping skills; lifestyle behaviors; and degree of social support.
Knowledge alone is insufficient to result in significant behavior change; however, it is integral to the process of change. Knowledge attainment requires health literacy; inadequate literacy is independently associated with worse glycemic control13 and higher rates of hospitalization and emergency services utilization.14 Nearly half of the adult U.S. population has difficulty understanding and using health information, i.e., the ability to understand instructions on prescription drug bottles, appointment slips, medical education brochures, doctor's directions and consent forms, and the ability to negotiate complex health care systems.15
Attitudes toward diabetes, its complications, and the possibility to alter its natural progression via alternative interventions such as diet, exercise, and medications are important determinants of engagement. According to the Prochaska and DiClemente Stages-of-Change Model,16 the practice of new behaviors (3–6 months) requires a commitment to maintenance (6–60 months) to avoid a relapse.
Self-management also depends on the patient's mental status. According to the National Center of Health Statistics, 42% of adults with diabetes report at least 1 day of poor mental health in the past 30 days.17 Diabetes increases the annual risk of a major depression to 15–20%, nearly double the risk for most Americans.18 People with diabetes and depression have higher health care costs due to worsening self-care behaviors.19
Self-management alone is insufficient to reach goal; patient–physician collaboration remains essential. However, in the current health care delivery system, primary care physicians have a limited amount of time to address the chronic care needs of diabetes patients, i.e., lifestyle issues, risk factors, comorbidities, and medications. The average face-to-face patient care time measured by direct observation was 10.7 minutes, excluding visit-specific work outside the examination room (2.6 minutes), figures far lower than the self-reported results of the National Ambulatory Medical Care Survey in 2003.20 Virtually no time is spent addressing nutrition, exercise, smoking cessation, or mental health concerns.21,22
Technology as an Enabler of Change
Consumer engagement requires an extension beyond a direct clinical focus. The interplay among disease management, health and wellness, cognitive and psychological well-being, social connectedness, personalization, and safety and security requires consideration of the individual patient. Technology is emerging that enables consumers and, importantly, their caregivers to enhance their health care experience.
The role of technology as an enabler depends on a variety of factors, including the complexity of the treated condition and comorbidities, technology savvy of the patient and/ or caregiver, and financial resources, including insurance coverage.
Consumer engagement, self-management, and behavior change is being facilitated earlier in the diabetes life cycle by the growth of condition-specific and social media Web sites, wireless technology, and mobile phones. Condition-specific and lifestyle-oriented sites are increasingly using checklists, tools, animations, and/or video, whereas social media sites have facilitated the sharing of clinical experience within peer communities. Interactive video games are also being applied to specific conditions. Wireless connectivity has eliminated the communication tether. Mobile technologies have also emerged as a 24/7, always-available source of information, reminders, and data collection.
Medication adherence also represents a major opportunity for increased consumer engagement. The World Health Organization has identified the major factors affecting adherence, including those related to the patient, condition, therapy, socio-economic status, and health system.23 According to the National Community Pharmacists Association Survey, patients often forget to take a prescribed medication (49%), forget to fill a prescription (31%), stop taking a medicine before the supply runs out (29%), or take less than the recommended dosage (24%).24 Patients with diabetes may utilize a wide variety of drugs for glycemic control, hypertension, cholesterol management, and other comorbidities. Physicians often lack the time and skills and are not reimbursed for patient education. New algorithm-based and digital technologies, as well as adjunctive behavioral coaching approaches, are emerging to optimize therapeutic management; engage, educate, and remind the consumer; and monitor actual utilization (beyond prescription refills).
The Internet, mobile phones, and medication adherence technology have potential applications to all patients with diabetes. Glucose testing, continuous glucose monitor, and insulin pump manufacturers are beginning to increase the functionality of their devices via interfacing trackers and analytic tools, as well as more engaging educational materials and community forums.
Other enabling technologies apply to the more severely ill or complex management cases, usually associated with cardiovascular, renal, or other comorbidities. Remote monitoring technology incorporating data from a variety of medical devices and sensors are being increasingly utilized to facilitate early intervention in patients and to provide the consumer and their caregiver a sense of safety and security. The unmet need is highlighted by published data reporting rehospitalization rates of 20–30% between 30 and 90 days postdischarge.25 Restrictive third-party reimbursement policies have limited market penetration. Sensors are also being used to monitor activity levels. Opportunities exist for baby boomers and others to pay out of pocket for themselves or their parents for these valuable services.
Telehealth networks are being established to provide increased access to patients in rural areas, as well as convenience to consumers. The Scottish National Health Service is attempting to recreate the patient experience in a remote kiosk via the use of high-definition video-conferencing technology, integrated with a range of medical devices.26
Conclusion
Unlike many other chronic conditions, complications associated with diabetes are preventable. Consumer engagement is absolutely necessary to change negative behaviors and to facilitate the self-confidence necessary for effective self-management. The shortage of primary care physicians, combined with a highly fragmented, poorly coordinated, and wrongly incentivized health care delivery system makes it unlikely that the “fix” will be driven by the clinical community. Emerging technology could potentially enable consumers to enhance their own outcomes while improving quality of life. A fresh mindset with a holistic perspective on the person with diabetes, rather than the patient with a specific medical condition, is required.
References
- 1.Department of Health and Human Services, Centers for Disease Control and Prevention. National Diabetes Fact Sheet. 2007. www. cdc.gov/diabetes/pubs/pdf/ndfs_2007.pdf.
- 2.Department of Health and Human Services. Diabetes data and trends. United States; 1980–2008. Centers for Disease Control and Prevention. Distribution of age at diagnosis among adult incident cases aged 18–79 years http://www.cdc.gov/diabetes/statistics/age/fig2.htm. [Google Scholar]
- 3.Department of Health and Human Services. Diabetes data and trends. United States; 2007. Centers for Disease Control and Prevention. Distribution of duration of diabetes among adults aged 18–79 years http://www.cdc.gov/diabetes/statistics/duration/fig1.htm. [Google Scholar]
- 4.Department of Health and Human Services. Data and trends. United States; 1980–2007. Centers for Disease Control and Prevention. Percentage of civilian, non-institutionalized population with diagnosed diabetes, by age http://www.cdc.gov/diabetes/statistics/prev/ national/figbyage.htm. [Google Scholar]
- 5.U.S. Census Bureau. 2007 population estimates. Table T6-2007. http://factfinder.census.gov/servlet/DTTable?_bm=y&-geo_id=01000US&-ds_name=PEP_2007_EST&-_lang=en&-mt_name=PEP_2007_EST_ G20 07_T0 01&-mt_name=PEP_ 20 07_ EST_G20 07_T0 06_ 20 07&-format=&-CONTEXT=dt.
- 6. Market Research.com. Baby boomers in the U.S. Available from http://www.marketresearch.com/product/display.asp?productid=1190036&xs=r.
- 7.American Diabetes Association. Diabetes Care. 2008;31(3):596–615. doi: 10.2337/dc08-9017. Economic costs of diabetes in the U.S. in 2007. [DOI] [PubMed] [Google Scholar]
- 8.Russo CA, Jiang HJ. Agency for Healthcare Research and Quality, Healthcare Cost and Utilization Project. 2006. Nov, Statistical brief #17: hospital stays among patients with diabetes, 2004 www.hcup-us.ahrq.gov/reports/statbriefs/sb17.pdf. [PubMed]
- 9.Agency for Healthcare Research and Quality. Healthcare Cost and Utilization Project (HCUPnet). http://hcupnet.ahrq.gov/HCUPnet.jsp.
- 10.Huang ES, Basu A, O'Grady M, Capretta JC. Projecting the future diabetes population size and related costs for the U.S. Diabetes Care. 2009;32(12):2225–2229. doi: 10.2337/dc09-0459. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Lethbridge-Çejku M, Vickerie J U.S. Department of Health and Human Services. Centers for Disease Control and Prevention, National Center for Health Statistics. Vital Health Stat. 2005;10(225) Summary health statistics for U.S. adults: National Health Interview Survey, 2003 http://www.cdc.gov/nchs/data/series/sr_10/sr10_225.pdf. [Google Scholar]
- 12.Lifestyle changes may stave off diabetes for a decade. Einstein News. November 2, 2009. http://www.einstein.yu.edu/home/news.asp?id=430.
- 13.Schillinger D, Grumbach K, Piette J, Wang F, Osmond D, Daher C, Palacios J, Sullivan GD, Bindman AB. Association of health literacy with diabetes outcomes. JAMA. 2002;288(4):475–482. doi: 10.1001/jama.288.4.475. [DOI] [PubMed] [Google Scholar]
- 14.Berkman ND, DeWalt DA, Pignone MP, Sheridan SL, Lohr KN, Lux L, Sutton SF, Swinson T, Bonito AJ. Literacy and health outcomes. Rockville: Agency for Healthcare Research and Quality; 2004. Evidence report/technology assessment No. 87. [PMC free article] [PubMed] [Google Scholar]
- 15.National Network of Libraries of Medicine New England Region. Health literacy. http://nnlm.gov/outreach/consumer/hlthlit.html.
- 16.UCLA Center for Human Nutrition. Prochaska and DiClemente's Stages of Change Model. http/www.cellinteractive.com/ucla/physcian_ed/stages_change.html.
- 17.Department of Health and Human Services. United States; 1994–2004. Centers for Disease Control and Prevention. Age-adjusted percentage of adults with diabetes reporting poor mental health, poor physical health, poor mental or physical health, and inability to do usual activities at least one day in the past 30 days http://www.cdc.gov/diabetes/statistics/mental/FigmentphyUS.htm. [Google Scholar]
- 18.National Institute of Mental Health, PsychCentral. Diabetes and depression. 2008. http://psychcentral.com/lib/2008/diabetes-and-depression/
- 19.Egede LE, Zheng D, Simpson K. Comorbid depression is associated with increased health care use and expenditures in individuals with diabetes. Diabetes Care. 2002;25(3):464–470. doi: 10.2337/diacare.25.3.464. [DOI] [PubMed] [Google Scholar]
- 20.Gottschalk A, Flocke SA. Time spent in face-to-face patient care and work outside the examination room. Ann Fam Med. 2005;3(6):488–493. doi: 10.1370/afm.404. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Yawn B, Goodwin MA, Zyzanski SJ, Stange KC. Time use during acute and chronic illness visits to a family physician. Fam Pract. 2003;20(4):474–477. doi: 10.1093/fampra/cmg425. [DOI] [PubMed] [Google Scholar]
- 22.Tai-Seale M, McGuire T. Time allocation in primary care with competing demands. Presented at the Economics of Population Health: Inaugural Conference of the American Society of Health Economists; June 4, 2006; TBA, Madison, WI. [Google Scholar]
- 23.World Health Organization. Adherence to long-term therapies: evidence for action. Geneva: World Health Organization; 2003. [Google Scholar]
- 24.National Community Pharmacists Association and Pharmacists for the Protection of Patient Care. 2006. Dec 15, Take as directed: a prescription not followed http://www.ncpanet.org/media/releases/2006/take_as_directed.php.
- 25.Jencks SF, Williams MV, Coleman EA. Rehospitalizations among patients in Medicare fee-for-service program. N Engl J Med. 2009;360(14):1418–1428. doi: 10.1056/NEJMsa0803563. [DOI] [PubMed] [Google Scholar]
- 26.Cisco Internet Business Solutions Group. Telemedicine pilot promises step change in healthcare delivery to rural and urban areas. http://www.ciscosecure.net/web/about/ac79/docs/wp/Scottish_Centre_for_ Telehealth_UK_SS.pdf.