Abstract
Objective:
To determine the effect of the prokinetic agent cisapride in the prevention of aspiration of gastric contents.
Design:
A prospective randomized two-period crossover study.
Setting:
Fourteen-bed polyvalent intensive care unit in a University Hospital.
Patients:
Eighteen intubated, mechanically ventilated patients who were seated in a semirecumbent position were studied.
Method:
Tc-99 m sulfur colloid (80 megabecquerels) was administered via nasogastric tube on 2 consecutive days. Patients randomly received cisapride (10 mg, via nasogastric tube) one day and a placebo the other. Bronchial secretions were obtained before and for 5 consecutive h after Tc-99 m administration. The radioactivity was measured in a standard amount (1ml) of bronchial fluid using a gamma counter and expressed as counts per min (cpm) after correction for decay.
Results:
Sixteen out of 18 (88%) patients had increased radioactivity in bronchial secretions. The radioactivity increased over time both with and without cisapride, although it was lower in patients receiving cisapride than in those receiving a placebo. The cumulative bronchial secretion radioactivity obtained when patients received cisapride was significantly lower than when patients received a placebo: 7540 ± 5330 and 21965 ± 16080 cpm, respectively (P <0.05).
Conclusion:
Our results suggest that aspiration of gastric contents exists even in patients who are kept in a semirecumbent position. Moreover, cisapride decreases the amount of gastric contents aspiration in intubated and mechanically ventilated patients and may play a role in the prevention of ventilator associated pneumonia. Cisapride, even with the patient in the semirecumbent position, did not completely prevent gastric content aspiration.
Keywords: cisapride, mechanical ventilation, aspiration, pneumonia, VAP
Introduction
The aspiration of gastric contents induces or exacerbates bronchoconstriction and it is the most commonly recognized pathogenic factor for the development of pneumonia, especially in ventilator-associated pneumonia (VAP) [1,2].
The incidence of aspiration of gastric contents is high in intensive care unit (ICU) patients and even higher in intubated and mechanically ventilated patients. Gastrointestinal tract dysmotility is a relatively common condition in critically ill patients and is associated with gastric contents aspiration [3,4]. Additional risk factors for gastric content aspiration included enteral feeding, naso or oral-gastric tubes and position of the patients. Enteral feeding via a nasogastric tube may also result in increased gastric volume, reflux and Gram-negative bacterial overgrowth in the stomach [5]. Wide bore nasogastric tubes themselves probably impair the function of the lower esophageal sphincter, thereby facilitating aspiration and bacterial contamination of the tracheobronchial tree [6]. Moreover, an important risk factor in causing the aspiration of gastric contents seems to be the supine position. A semirecumbent position of mechanically ventilated patients could help in part to prevent the aspiration of gastric contents into airways, but aspiration still remains a problem [7]. Orozco-Levi and colleagues [8] showed a significant increase in radioactivity count in oropharyn-geal contents after Tc99m isotope instillation through nasogastric tube. This gastroesophageal reflux was irrespective of body position. In contrast, the radioactivity count values in bronchial secretions were higher in the supine position than in semirecumbency, which suggests that the semirecumbent position helps prevent in part gastric content aspiration. Apart from position, agents, such as erythromycin and cisapride, increase the gastric motility and they could accelerate gastric emptying and prevent gastric aspiration [9,10].
Cisapride is a very effective prokinetic agent that acts by increasing the physiological release of acetylcholine from the postganglionic nerve endings of the myenteric plexus without any associated dopamine antagonism [10].
In this study, we assessed the effect of cisapride in the prevention of pulmonary aspiration of gastric contents in mechanically ventilated patients maintaining the benefit of a semirecumbent position.
Materials and methods
Patients
Eighteen mechanically ventilated patients (15 men and three women, mean age 52.33 ± 17.90 years) were included in this study. The protocol was approved by the Medical Ethics Committee of The University Hospital of Ioannina and consent was obtained from the patients' relatives. Patients with gastrectomy, ileus, respiratory infections, sepsis and hemodynamic instability (low blood pressure needing high doses of inotropes, or wide fluctuation of blood pressure over time) were excluded from the study. The demographic data and the underlying clinical conditions of these patients are summarized in Table 1.
Table 1.
Patient characteristics
| No | Sex | Age | Diagnosis | APACHE II | Medications | MV | Outcome |
| 1 | F | 58 | SBH | 22 | Midazolam | 5 | S |
| 2 | M | 54 | ICH | 20 | — | 5 | D |
| 3 | M | 54 | COPD | 28 | Midazolam | 5 | D |
| 4 | F | 70 | COPD | 30 | Propofol | 8 | S |
| 5 | M | 48 | Head injury | 24 | Fentanyl, Midazolam | 10 | S |
| 6 | M | 19 | GBS | 14 | Fentanyl | 5 | S |
| 7 | M | 40 | Head injury | 29 | Fentanyl, Midazolam | 6 | D |
| 8 | M | 67 | Head injury | 28 | Fentanyl, Midazolam | 7 | S |
| 9 | M | 76 | ICH | 28 | Midazolam | 6 | D |
| 10 | M | 41 | Drug overdose | 12 | — | 4 | S |
| 11 | M | 74 | ICH | 25 | Midazolam, Fentanyl | 4 | D |
| 12 | M | 74 | Cardiac failure | 27 | Lorazepam | 4 | D |
| 13 | F | 64 | ICH | 25 | Midazolam | 6 | S |
| 14 | M | 25 | Head injury | 17 | Lorazepam, Fentanyl | 5 | S |
| 15 | M | 26 | Trauma | 22 | Fentanyl | 5 | S |
| 16 | M | 55 | Head injury | 24 | Propofol | 8 | S |
| 17 | M | 62 | ICH | 27 | — | 6 | S |
| 19 | M | 35 | Head injury | 19 | Propofol, Fentanyl | 8 | S |
| Mean | 52 | 23 | 6 | ||||
| SD | 17 | 5 | 1.7 |
M, male; F, female; S, survival; D, death; ICH, intracerebral hemorrhage; GBS, Guillain Barr syndrome; SBH, subarachnoid brain hemorrhage; COPD, chronic obstructive pulmonary disease; MV, days of mechanical ventilation.
Protocol
All patients had a 5 mm diameter nasogastric tube in place for enteral nutritional support and received sucralfate 2 g twice daily for stress ulcer prophylaxis. The position of the nasogas-tric tube was radiographically checked before the study. Sedation and all the other medications were kept unchanged throughout the study (Table 1). Nobody was given paralytic agents, antibiotics or inotropes. The enteral nutrition and other medications via nasogastric tube were withheld 8 h before the onset and during the study. The body position of the patients was semirecumbent at a 45 degree angle, and they were put in this position at least 8h before the study.
All patients were intubated and mechanically ventilated with an assist-control mode. A low level of positive end-expiratory pressure (PEEP) was used (PEEP: 5 ± 1.7 cmH2O). The volume, pressure and the leaking of the cuff of the endotracheal tube was checked, before and at the end of every day of the study. The minimal volume and pressure necessary to prevent air leaking around the cuff were used. The study lasted 2 consecutive days for each patient. Eighteen hours before the study, the patients received, at 6 h intervals, a cisapride suspension (Alimix, Janssen Pharmaceutica, Beerse, Belgium; 1 mg/ml) in a dose of 10 mg, or a placebo given as a bolus randomly via nasogastric tube. The next morning, 60 megabecquerels of Tc99m sulfur colloid were carefully administered via the tube as described by Chernow and colleagues [11]. Bronchial secretions were taken at zero time (baseline radioactivity) and then once an hour for 5 consecutive h. The secretions were taken in a sterile container by bronchial suction. The suction catheter was placed at the level of the carina. The distance of the carina from the tip of the endotracheal tube was measured on a chest X-ray. Just after the end of this procedure, patients who had previously received cisapride were given placebo and vice versa. On the second day, the procedure was repeated in the same way. Blood samples were taken from the first five patients in the study, before and 5 h after isotope instillation and checked for radioactivity. Just before starting the procedure, bronchial secretion, oropharyngeal and gastric samples were taken for microbiological cultures. A gentle suction of gastric content was performed just before the administration of the isotope.
Measurements
The activity of Tc99m was measured, using a gamma counter (Gamma Counting system, Crystal TM II, 5400 Series, Packard Instrumental Company), in a standard amount (1 ml) of bronchial secretions. The amount of radioactivity is expressed as counts per min (cpm) after correction for decay according to the equation of radioactive decay law:
N = N0.e-λt
where N0 is the number of parent nuclei present at t = 0,N is the number remaining nuclei at time t, λ is a constant of proportionality, called the decay constant, which is different for different isotopes and e is the base of natural logarithm [12].
During the procedure, monitoring was performed with a two-lead electrocardiogram (ECG) and a 12-lead ECG was performed before and soon after the end of every procedure.
Statistics
The differences between groups were tested for significance by analysis of variance (ANOVA) test for repeated measures. Results are expressed as mean± SD. A P value less than 0.05 was considered significant.
Results
Sixteen out of 18 patients (88%) demonstrated an increased radioactivity in bronchial secretions and it increased over time both in patients receiving cisapride or placebo. When patients received cisapride, the radioactivity increased from 120 ± 18 cpm (baseline radioactivity at zero time) to 1930 ± 1340 cpm at the fifth hour (P < 0.05). When patients received a placebo the radioactivity increased from 115 ± 22 cpm (baseline radioactivity at the zero time) to 6825 ± 5100 cpm 5 h later (P < 0.01). There was no significant difference in baseline radioactivity of bronchial secretions whether the patients were given cisa-pride or placebo. The change in radioactivity of bronchial secretions over time is demonstrated in Fig 1. The difference in radioactivity during cisapride and placebo administration became statistically significant after the third hour (P < 0.05). The cumulative bronchial secretion radioactivity obtained when patients received cisapride was significantly lower than when patients received a placebo (7540 ± 5330 and 21965 ± 16080cpm, respectively; P < 0.05; Fig 2).
Figure 1.
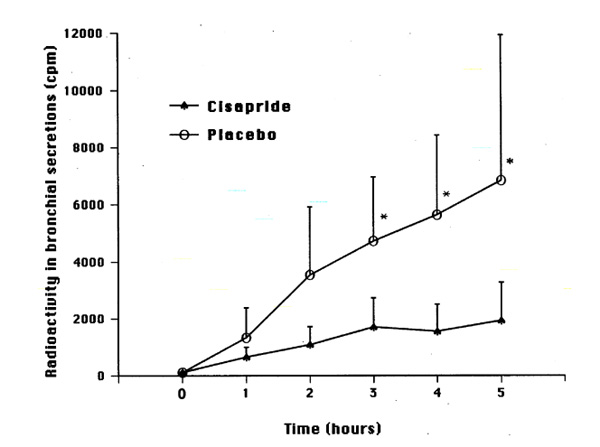
The radioactivity of bronchial secretions over time. The values at zero time represent the baseline radioactivity. Asterisk (*) denotes statistical significance between cisapride and placebo.
Figure 2.
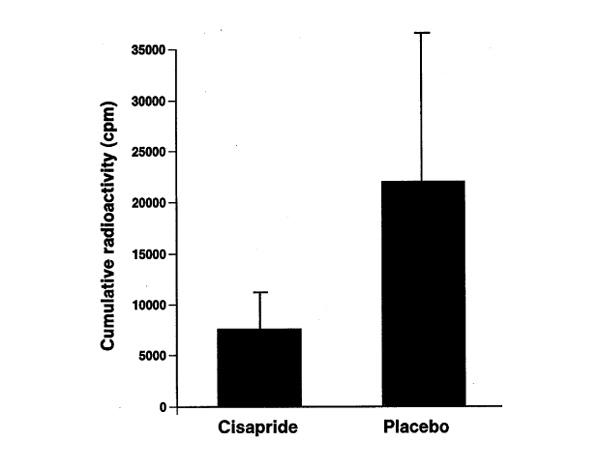
The cumulative radioactivity of bronchial secretions with and without cisapride.
The microbiological cultures showed that 10 patients had identical microorganisms colonizing the stomach, oropharyngeal area and bronchus. Five patients had the same microorganisms only in the oropharyngeal content and bronchial secretion, and different ones in the gastric content. Three patients had different microorganisms in stomach, oropharynx and bronchus. Two of the studied patients developed VAP during their stay in ICU; both patients had the stomach, oropharynx and bronchus colonized with the causative bacteria of VAP, which were detected by quantitative cultures of protected brush specimens.
There was no significant difference in cuff pressure between measurements before and at the end of the study.
There was no difference in the blood radioactivity before and 5 h after isotope administration, as it was the same as the background radioactivity.
No side effects of cisapride were observed during this study. No cardiac arrhythmia or QT interval prolongation was noted.
Discussion
This study demonstrates that cisapride significantly reduced the pulmonary aspiration of gastric contents in mechanically ventilated patients although the conventional protective methods, such as semirecumbent position and regular checking of cuff leaking, even with cisapride administration are not sufficient to prevent gastric content aspiration completely.
In critically ill patients receiving mechanical ventilation gastrointestinal motility is often impaired [3,4]. The precise mechanism leading to this gastroparesis is still unknown. Medications such as opiates and dopamine [13,14], hyperglycemia [15] or increased intracranial pressure [16] have all been shown to depress the antral motor activity in experimental or clinical conditions. This situation favors not only gastroesophageal reflux but also duo-denogastric reflux, thereby promoting the colonization of the stomach with gastric Gram negative pathogens [17,18]. Enteral nutrition in patients with inadequate gastric emptying can increase the risk of aspiration, and expand the size of the gastric bacterial reservoir by increasing the gastric volume and the pH. Today most investigators agree that gastric colonization with potentially pathogenic microorganisms is important in the pathogenesis of VAP [17,19,20]. Moreover, nasogastric tubes themselves probably impair the function of the lower esophageal sphincter thereby promoting aspiration. In addition, the supine position of patients promotes aspiration and the semirecum-bent position helps minimize the aspiration of gastric contents to lower airways [7,8].
Our results showed that aspiration in mechanically ventilated patients occurs even when they are kept in a semire-cumbent position. The administration of cisapride significantly decreases aspiration in these patients. A properly inflated cuff was insufficient to prevent aspiration to lower airways. The incidence of gastric content aspiration in our group of patients was very high. One explanation could be the high percentage of neurological diseases, which are included in our patient population, because severe head injury has been associated with impaired gastric emptying [16]. Another cause of the high incidence of aspiration could be the sedation received by the majority of the patients. There is no clear explanation for the absence of gastric content aspiration in two patients. It is noteworthy, though, that one of them did not receive sedation and the other was given low-dose (5mg/h) mida-zolam. Both survived, and their age, APACHE II score and the days of mechanical ventilation at the day of the study were equivalent to those of the other patients.
These findings are in agreement with other investigators who found that cisapride prevents the morphine-induced delay in gastric emptying [21]. It also significantly accelerates gastric emptying both in patients with gastroesophageal reflux disease and in patients with delayed gastric emptying caused by idiopathic or postsurgical reasons [22]. It has also been suggested that cisapride can minimize the risk of aspiration pneumonia in patients with long-term enteral feeding [23]. In critically ill patients with gastric dilatation and functional gastric paralysis the administration of cisapride showed a clinical benefit [24,25]. Moreover, cisapride increases the lower esophageal sphincter pressure in normal volunteers and in patients with reflux disease [26]. The velocity of transit in the esophagus remains unchanged with cisapride, but an increase in distal peristalsis is noted [27].
Oral cisapride usually has few side effects. Nevertheless, cardiac arrhythmias, especially torsade de pointes, and prolonged QT intervals with a potentially fatal outcome have been described in patients with concomitant use of medication that is metabolized by the cytochrome P-450 3a4 isoenzyme, eg imidazole antibiotics or macrolides [28]. Cisapride should be administered with caution in patients who are on any medication known to prolong QT interval and in those with renal insufficiency, a history of arrhythmia or cardiac disease. None of our patients received any of the above medications and, possibly for this reason, no side effects were noted during the period of cisapride administration.
Conclusion
In summary, our results suggest that cisapride decreases the risk of aspiration of gastric contents in intubated and mechanically ventilated patients who are kept in a semirecumbent position. Conventional protective methods though, such as the semirecumbent position and regular checking of cuff leaking, even with cisapride administration are not sufficient to prevent gastric content aspiration completely. Further studies are needed to establish if this drug helps in the prevention of ventilator associated pneumonia, bronchitis or bronchoconstriction.
References
- Graven DE, Steger KA, Barber TW. Preventing nosocomial pneumonia: state of the art and perspectives for the 1990s. Am J Med. 1991;91 (suppl 3B):44S–53S. doi: 10.1016/0002-9343(91)90343-v. [DOI] [PubMed] [Google Scholar]
- Graven DE, Steger KA, Duncan RA. Prevention and control of nosocomial pneumonia. Wenzel RP (editor). Baltimore: Williams and Wilkins; Prevention and control of nosocomial infections. 1993. pp. 580–599.
- Dive A, Moulart M, Jonard PH, et al. Gastroduodenal motility in mechanically ventilated critically ill patients: a manometric study. Crit Care Med. 1994;24:441–447. doi: 10.1097/00003246-199403000-00014. [DOI] [PubMed] [Google Scholar]
- Heyland DK, Toudas G, King D, Cook CJ. Impaired gastric emptying in mechanically ventilated critically ill patients. Int Care Med . 1996;22:1339–1344. doi: 10.1007/BF01709548. [DOI] [PubMed] [Google Scholar]
- Jacobs S, Chang RW, Lee B, Bartelett FW. Continuous enteral feeding: a major cause of pneumonia among ventilated intensive care unit patients. Parenteral Nutrition. 1990;14:353–356. doi: 10.1177/0148607190014004353. [DOI] [PubMed] [Google Scholar]
- Hospital acquired pneumonia in adults : diagnosis, assessment of severity, initial antimicrobial therapy and preventative strategies. A Consensus Statement of ATS. Am J Respir Crit Care Med. 1995;153:1711–1725. doi: 10.1164/ajrccm.153.5.8630626. [DOI] [PubMed] [Google Scholar]
- Torres AJ, Serra Batlles Ros E, Piera C, Puing de la Belacasa Cobos A, Lomena F, Rodriguez Roisin R. Pulmonary aspiration of gastric contents in patients receiving mechanical ventilation: the effect of body position. Ann Intern Med. 1992;116:540–543. doi: 10.7326/0003-4819-116-7-540. [DOI] [PubMed] [Google Scholar]
- Orozco Levi M, Torres A, Ferrer M, et al. Semirecumbent position protects from pulmonary aspiration but not from gastroesophageal reflux in mechanically ventilated patients. Am J Respir Crit Care Med. 1995;152:1387–1390. doi: 10.1164/ajrccm.152.4.7551400. [DOI] [PubMed] [Google Scholar]
- Dive A, Miesse C, Galanti L, et al. Effect of erythromycin on gastric motility in mechanically ventilated critically ill patients: a double-blind, randomized, placebo-controlled study. . Crit Care Med. 1995;23:1356–1362. doi: 10.1097/00003246-199508000-00008. [DOI] [PubMed] [Google Scholar]
- McGallum RW, Prakash C, Campoli Richards DM, et al. Cisapride. A preliminary review of its pharmacodynamic and pharmacokinetic properties, and therapeutic use as a prokinetik agent in gastrointestinal motility disorders. Drugs. 1988;36:652–681. doi: 10.2165/00003495-198836060-00002. [DOI] [PubMed] [Google Scholar]
- Chernow B, Johnson LF, Janowitz WR, Castell DO. Pulmonary aspiration as a consequence of gastroesophageal reflux: a diagnostic approach. Digest Dis Sci. 1979;24:839–844. doi: 10.1007/BF01324899. [DOI] [PubMed] [Google Scholar]
- Giacoli D. Physics for Scientist and Engineers. Prentice Hall,Second edition.International Edition. 1989. p. 980.
- Nimmo WS, Heading RC, Wilson J, Tothill P, Prescott LF. Inhibition of gastric emptying and drug absorption by narcotic analgesics. Br J Clin Pharmacol. 1975;2:509–513. doi: 10.1111/j.1365-2125.1975.tb00568.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Frost P, Edwards N, Bihari D. Gastric emptying in the critically ill - the way forward? Intensive Care Med. 1997;23:243–245. doi: 10.1007/s001340050322. [DOI] [PubMed] [Google Scholar]
- Barnett JL, Owyang CH. Serum glucose concentration as a modulator of interdigestive gastric motility. Gastroenterology . 1988;94:739–744. doi: 10.1016/0016-5085(88)90248-x. [DOI] [PubMed] [Google Scholar]
- Matthews DE, Heimanshon DA, Papaila JG, et al. The effect of increased intracranial pressure on gastric motility. J Surg Res. 1988;45:60–65. doi: 10.1016/0022-4804(88)90022-4. [DOI] [PubMed] [Google Scholar]
- Inglis TJ, Sproat L, Sherratt LJ, Gibson JS, Hawkey PM. Gastroduodenal dysfunction and bacterial colonization of ventilated lung. Lancet. 1993;341:911–913. doi: 10.1016/0140-6736(93)91208-4. [DOI] [PubMed] [Google Scholar]
- Atherton ST, White ST. Stomach as a source of bacteria colonising respiratory tract during artificial ventilation. Lancet . 1978;ii:968–969. doi: 10.1016/s0140-6736(78)92530-8. [DOI] [PubMed] [Google Scholar]
- Heyland D, Mandell LA. Gastric colonization by Gram negative bacilli and nosocomial pneumonia in the intensive care unit patient: evidence of causation. Chest. 1992;101:187–193. doi: 10.1378/chest.101.1.187. [DOI] [PubMed] [Google Scholar]
- Torres A, El-Ebiary M, Gonzalez J, Ferrer M, et al. Gastric and pharyngeal flora in nosocomial pneumonia acquired during mechanical ventilation. Am Rev Respir Dis. 1993;148:352–357. doi: 10.1164/ajrccm/148.2.352. [DOI] [PubMed] [Google Scholar]
- Rowbotham DJ, Nimmo WS. Effects of cisapride on morphine induced delay in gastric emptying. Br J Anaesth. 1987;59:536–539. doi: 10.1093/bja/59.5.536. [DOI] [PubMed] [Google Scholar]
- Richards RD, Valenzuela GA, Davenport KG, et al. Objective and subjective results of randomized double bind, placebo controlled trial using cisapride to treat gastroparesis. Dig Dis Sci. 1993;38:811–816. doi: 10.1007/BF01295905. [DOI] [PubMed] [Google Scholar]
- Sartori S, Trevisani , Tassinari D, et al. Prevention of aspiration pneumonia during long-term feeding by percutaneous endoscopic gastrostomy: may cisapride play a role. An open pilot study. Supp Care Cancer. 1994;2:188–190. doi: 10.1007/BF00417479. [DOI] [PubMed] [Google Scholar]
- Lauwers LF. Cisapride in intensive care. Int Care Med . 1991;17:508–509. doi: 10.1007/BF01690782. [DOI] [PubMed] [Google Scholar]
- Shapen H, Duinslaeger L, Diltoer M, Gillet R, Bossuyt A, Huyghens LP. Gastric emptying in critically ill intensive care patients is accelerated by adding cisapride to a standard enteral feeding protocol. Crit Care Med. 1995;23:481–485. doi: 10.1097/00003246-199503000-00011. [DOI] [PubMed] [Google Scholar]
- Gilbert RJ, Dodds WJ, Kahrilas PJ, et al. Double-blinded assessment of the effect of intravenous and oral cisapride on esophageal motor function. Digestion. 1986;34:139. [Google Scholar]
- Case WG, Williams NS. The effect of cisapride upon lower esophageal sphincter pressure and primary peristalsis. Dig Dis Sci . 1986;31:465S. [Google Scholar]
- Wysowski DK, Bascanyi J. Cisapride and fatal arrhythmia. . N Engl J Med. 1996;25:290–291. doi: 10.1056/NEJM199607253350416. [DOI] [PubMed] [Google Scholar]


