Abstract
With the increasing prevalence of hypertension, there has been a growing interest in understanding the health-related quality of life (HRQOL) of patients with hypertension. Although hypertension is often perceived as asymptomatic, it is associated with impaired HRQOL due to complications or co-morbidities, awareness of the diagnosis and adverse effects from anti-hypertensive medications. This article focuses on the literature published since 2000, on HRQOL in elderly hypertensive individuals as well as hypertensives with co-existent diseases, including chronic kidney disease (CKD), cardiovascular disease and diabetes mellitus. Most of the studies found that hypertensive individuals with co-existent co-morbidities tend to have lower HRQOL than those with hypertension alone, and identified the number of co-morbid illnesses as an independent determinant of HRQOL. The most pronounced effect was noted in the physical function domains of HRQOL. Studies have also examined the effects on HRQOL of specific classes of antihypertensive drugs without specific demonstration of superiority of 1 drug class over another in terms of HRQOL measures. While there is evidence in favor of ACE-inhibition for improving renal and cardiovascular outcomes in hypertensive patients, its role in ameliorating HRQOL outcomes remains to be established.
Keywords: Hypertension, quality of life, chronic kidney disease, aging, cardiovascular diseases, diabetes mellitus
Introduction
Hypertension is estimated to affect 29% of the population in the United States (U.S.)(1) Health-related quality of life (HRQOL) among those with hypertension has been shown to be diminished compared to that of community-based controls and has also been shown to decrease over time. The impact of disease on HRQOL is especially relevant for a disease such as hypertension, as treatments to control hypertension may also worsen HRQOL. Studies of HRQOL among hypertensive individuals have been conflicting, with some studies finding worse HRQOL among hypertensives compared to the general population,(2-4) and some finding no impact of hypertension on HRQOL in some or all domains.(5) These disparate findings may be related to the different populations examined in different studies. In studies that have found poorer HRQOL associated with a diagnosis of hypertension, the mechanism for the lower HRQOL is unknown. Some studies have suggested that a patient's awareness of the diagnosis of hypertension itself is responsible for the lower HRQOL, with those unaware of the diagnosis of hypertension having better HRQOL than those aware of the diagnosis.(6) However, the question of HRQOL in hypertension is a complicated one, as hypertension frequently co-exists with other illnesses or states in which HRQOL can be negatively impacted. The question of hypertension and its treatment influencing HRQOL is an important one since HRQOL may influence long-term independence and adherence to therapy. Since HRQOL in hypertension has been previously reviewed through 2000,(7, 8) this review emphasizes on work published since 2000 and focuses primarily on physical, mental and social well-being among older adults with hypertension in the setting of chronic kidney disease (CKD) and chronic health conditions. The aim of this review is to examine HRQOL in subsets of hypertension with an additional co-morbidity, i.e CKD, cardiovascular disease, diabetes mellitus (DM) and the elderly.
Models of Health-Related Quality of Life
The most widely accepted model of HRQOL is based on the World Health Organization's definition of quality of life as a complete state of physical, mental, and social well-being and not merely an absence of disease in infirmity.(9) This model stresses the importance of psychological, social and physical functioning to perceived HRQOL.(10) Some researchers have argued for more comprehensive measurement of quality of life in hypertension, suggesting assessment of physical capabilities, mood, social interaction, intellectual functioning, economic status, and self-perceived health status.(11, 12) The conceptual approach includes HRQOL measurements that are based on a patient's “subjective” sense of well-being and are commonly used as indicators of successful medical treatment. While the questionnaires are subjective and represent the patients' own perspectives, they are highly reproducible and the reliability of HRQOL domains compares favorably with the reliability of blood pressure measurements. Some well-validated instruments used in hypertension studies are Short Form-36 (SF-36), Sickness Impact Profile (SIP), Nottingham Health Profile (NHP) and Profile of Mood States (POMS).
Health-related quality of life in hypertension with CKD
Hypertension is both a cause and a complication of CKD, accounting for 26.8% of incident end-stage renal disease (ESRD) cases in 2006(13) and affecting 50% to 75% of the CKD population.(14) It is also well recognized as a risk factor for CKD progression.(14) In addition, trials have established hypertension and CKD as independent risk factors for cardiovascular disease.(14-19) Notably, a prospective study conducted in the urban Japanese population suggested that hypertensive individuals with even mild CKD with and estimated glomerular filtration rate (eGFR) of 50-59 ml/min/1.73 m2 are at greater risk of stroke than hypertensive individuals with normal eGFR (>60 ml/min/1.73 m2), and that hypertensive subjects with more severe renal impairment were at an even greater risk for stroke.(20)
While HRQOL has been studied in hypertension(21-24) and CKD,(25-28) there is paucity of literature on HRQOL in patients with both hypertension and CKD. The dramatically expanding prevalence of CKD(29) and the role of hypertension in progression of CKD prompt the need for a better understanding of HRQOL in this population. One study that has evaluated HRQOL in subjects with both hypertension and CKD was the African American Study of Kidney Disease and Hypertension (AASK) Trial.(30) It was a 7-year, double-blind multicenter randomized controlled clinical trial designed to evaluate the effects of 2 goal levels of blood pressure control and 3 anti-hypertensive drug regimens on decline in renal function in patients with hypertensive nephrosclerosis.(31) A total of 1094 participants were randomized to either a usual mean arterial pressure goal of 102 to 107 mm Hg or a low mean arterial pressure goal of 92 mm Hg or lower, and to initial anti-hypertensive therapy with either a beta-blocker (metoprolol), angiotensin-converting enzyme (ACE) inhibitor (ramipril), or dihydropyridine calcium channel blocker (amlodipine). The investigators also assessed the HRQOL by the Medical Outcomes Short-Form 36 (SF-36) at baseline and at the last follow up visit. The cross-sectional analysis showed that study participants at baseline had lower physical-domain HRQOL scores than the general population in the U.S., but higher scores than hypertensive African Americans on hemodialysis.(32) These patients suffered significant impairment in the physical dimensions of HRQOL as compared to the mental dimensions, with scores in women being worse than in men. Low socioeconomic status, unemployment, obesity and co-existing co-morbidity were identified as independent determinants of HRQOL. Furthermore, the researchers found a significant negative impact of higher mean arterial pressure, longer duration of hypertension, larger number of anti-hypertensive medications and greater degree of renal insufficiency on HRQOL. HRQOL scores and symptom scores at baseline were comparable in the 2 blood pressure goal groups and the 3 anti-hypertensive regimen groups.(32)
On longitudinal annual follow-up of the AASK study participants, Lash and colleagues observed that there were no significant differences in HRQOL scores or self-reported symptoms between the low and usual-mean arterial pressure groups,(33) as shown in Figures 1(a) and 1(b). Comparison by treatment group revealed lower rates of decline in HRQOL in the ramipril group than the metoprolol group, suggesting superiority of ramipril. However, larger prospective trials are required to establish its superiority over other anti-hypertensive agents with respect to HRQOL outcomes.
Figure 1.
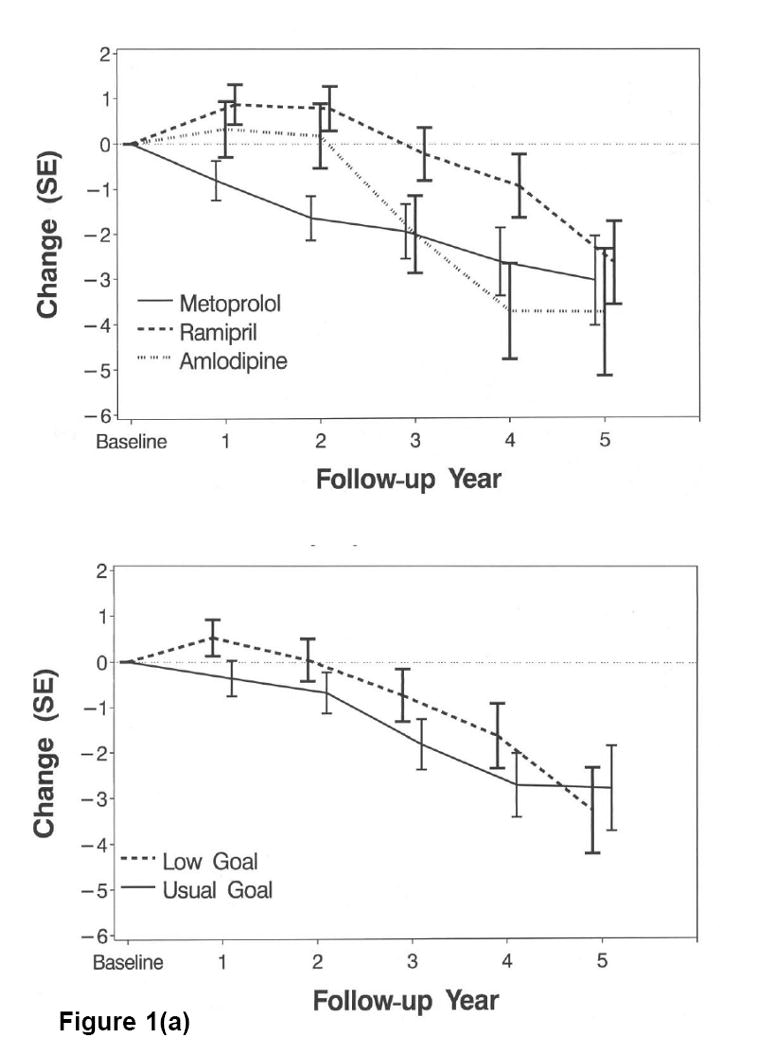
(a). Mean change in SF-36 Physical Health Component Scores by drug group (top) and blood pressure goal (bottom). Low goal: Mean arterial pressure 92 mm Hg or lower. Usual goal: Mean arterial pressure 102-107 mm Hg. Reprinted with permission.(33)
(b). Mean change in SF-36 Mental Health Component Scores by drug group (top) and blood pressure goal (bottom). Low goal: Mean arterial pressure 92 mm Hg or lower. Usual goal: Mean arterial pressure 102-107 mm Hg. Reprinted with permission.(33)
Other investigators have studied the impact of anti-hypertensive treatment on HRQOL.(21, 26, 34) Among these, a small 3-year randomized trial by De Rosa and associates is notable for comparing the effects of losartan to those of enalapril on blood pressure, left ventricular mass, renal function and HRQOL.(35) They concluded that both the drugs had relatively similar hemodynamic profiles as well as similar effects on the glomerular filtration rate and HRQOL, as assessed by the battery-of-scales instrument. There was no significant difference in the self-reported symptoms except for a higher incidence of cough in the enalapril arm.
The effect of antihypertensive therapy on HRQOL is particularly important because control of blood pressure is the mainstay of therapy for patients with CKD. The National Kidney Foundation Kidney Disease Outcomes Quality Initiative (K/DOQI) recommends a blood pressure target of less than 130/80 mm Hg in CKD with aims of therapy being to lower blood pressure, reduce the risk of cardiovascular disease and slow the progression of renal disease, with emphasis on use of ACE-inhibitors or angiotensin-receptor blockers.(14) While there is a substantial body of evidence in favor of ACE-inhibition for improving renal outcomes in patients with CKD,(36-41) its role in ameliorating HRQOL outcomes remains to be established.
Health-related quality of life in hypertension with cardiovascular disease
In general, studies examining the impact of single or multiple co-morbid illnesses on HRQOL have suggested that greater numbers of co-morbid illnesses are associated with lower HRQOL. There has been a comprehensive overview of HRQOL in cardiovascular disease through 1998 by Swenson and Clinch.(42) The literature focusing on this topic is diverse as it includes multiple types of cardiovascular diseases including coronary disease, heart failure, peripheral vascular disease as well as cardiovascular risk factors such as DM. Because cardiovascular risk factors including hypertension tend to cluster in individuals, the subject of HRQOL in patients with hypertension and cardiovascular disease has been examined specifically to determine the impact of individual cardiovascular risk factors and cardiovascular disease itself on HRQOL.
As is the case for literature regarding other co-morbid illnesses, population-based studies have demonstrated that individuals who report greater numbers of cardiovascular risk factors (including DM, hypertension, hyperlipidemia, obesity and smoking) are more likely to rate their overall health as “poor” or “fair” than those with fewer cardiovascular risk factors.(43) The physical domain measurements of HRQOL appear to be most affected by the clustering of cardiovascular risk factors and cardiovascular disease itself. Bayliss and colleagues examined data from the Medical Outcomes Study with respect to longitudinal changes in physical domain measurements in HRQOL of hypertensive patients,(44) some components of the physical domain being the ability to deal with the physical requirements of life such as attending to personal needs, walking, flexibility, physical symptoms and vitality.(45) The authors used a previously defined cutoff of a “clinically significant” change in physical HRQOL scores and found that a diagnosis of congestive heart failure, DM, chronic respiratory illness, or the presence of 4 or more chronic illnesses predicted a clinically significant change in physical HRQOL over 4 years. It is notable that a diagnosis of congestive heart failure was associated with a larger decrement in physical HRQOL scores than the diagnosis of coronary artery disease.
Further studies have examined the impact of specific cardiovascular diseases on HRQOL in hypertensive individuals. A Turkish study used the SF-36 to describe the effects of co-morbid conditions on HRQOL in hypertensive individuals.(46) The hypertensive patients had lower SF-36 scores than population norms, and a variety of clinical and demographic factors were found to affect HRQOL scores. Age and female gender were associated with low SF-36 subscale scores, while diagnosis of congestive heart failure, cerebrovascular disease, obesity and angina lowered the scores in the physical domain subscales. History of transient ischemic attack or of myocardial infarction was associated with impaired mental health scores in this study whereas peripheral vascular disease was associated with decrements in perceptions of overall health. Obesity, which is also a cardiovascular risk factor and is often linked with hypertension, was found to be independently associated with impaired physical function in a study by Johansen and colleagues.(47) Other studies have more intensively examined coronary disease, particularly in patients who have required coronary artery bypass grafting (CABG), with regard to effects on HRQOL in hypertensive individuals. Most of the studies have found that hypertensive patients with coronary disease have a lower HRQOL than non-hypertensive individuals or that they respond less favorably to coronary interventions than do patients without hypertension in terms of improvements in HRQOL. Another study followed non-ST-elevation MI patients longitudinally after MI and found that patients with hypertension had smaller improvements in HRQOL after MI than did patients without hypertension.(48) Two studies have addressed HRQOL in hypertensive patients with coronary disease within the context of CABG. A study that compared on-pump and off-pump CABG demonstrated that patients with hypertension in both surgical groups had worse physical domain HRQOL scores after CABG than those without hypertension.(49) A second study followed patients from the time of CABG for 5 years afterward and compared HRQOL and mortality in patients with hypertension versus those without hypertension.(50) Patients with hypertension had higher 5-year mortality and smaller improvement in the physical domain of HRQOL measurement after CABG than those without hypertension. The authors postulated that accelerated atherosclerosis in hypertensive patients with cardiac disease could have led to the different findings in the 2 groups.
In summary, hypertensive individuals with cardiovascular disease or increased numbers of cardiovascular risk factors tend to have lower HRQOL than those with hypertension alone. This effect appears to be most pronounced in the physical function domains of HRQOL. Though the cardiovascular disease can contribute to poorer physical function and HRQOL through several mechanisms, 1 study(51) suggests that poor HRQOL may lead to increased progression of atherosclerosis, which could in turn lead to loss of physical function.
Health-related quality of life in hypertension with DM
The global health burden of DM is of epidemic proportions with the worldwide prevalence projected to reach 366 million in 2030.(52) Studies have established that diabetic patients demonstrate impaired HRQOL(53-55) which is associated with disease severity, duration, diabetic complications and concomitant morbidities.(56) Hypertension frequently coexists with DM and published studies that have sought to evaluate the impact of these co-morbidities on HRQOL have yielded variable results.
Lloyd and colleagues assessed the influence of complications associated with type 2 DM on HRQOL.(57) Although hypertension was found to be the most prevalent complication, it was not found to affect HRQOL independently. Comparable results were observed in 2 subsequently published studies.(46, 58) Interestingly, a study by Miksch and associates reported better HRQOL in patients with both hypertension and DM than in those with DM alone, but the results were not significant.(55) The interpretation for these findings was that hypertension is often asymptomatic until later stages of the disease and hence it does not lower HRQOL in patients with DM. In contrast, several other studies have reported notable negative effects of hypertension on HRQOL in type 1(59) and type 2(56, 60) diabetics, with the most detrimental influence on the physical(54, 59) and general health domains.(56) Wee and associates further described this influence as being an additive phenomenon.(54) It is interesting to note that in addition to the physical domains, patients with DM and hypertension identified medication-related issues and diet as aspects that were relevant to HRQOL. While patients were concerned about factors affecting their physical and social functioning, health-care providers focused on improving clinical outcomes and the process of care.(61)
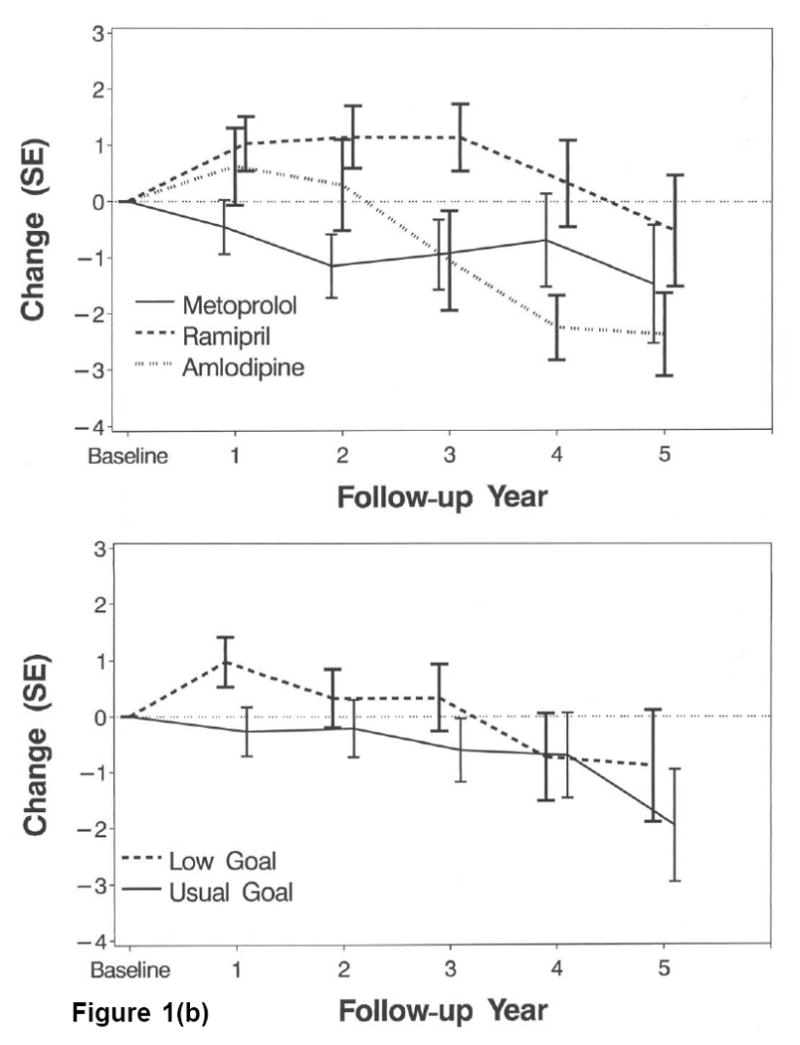
The discrepancies in these results can be explained by the use of varying HRQOL instruments, variation in study populations, disease severity, duration and presence of additional co-morbidities. It is also notable that most of these studies were performed on subjects with DM type 2 and the co-morbidities were self-reported. Despite the inconsistency in results from these studies, identification and treatment of hypertension is nonetheless very crucial in diabetics, in order to reduce their cardiovascular mortality and morbidity. With only a handful of studies on effects of antihypertensive treatment on HRQOL in the diabetic population, our understanding of the treatment choice is limited. While Ostman and colleagues found no significant differences in the overall well-being and symptom scores with either metoprolol or quinapril,(62) McGill and colleagues demonstrated that carvedilol was superior to metoprolol in terms of the perceived burden of DM-related symptoms.(63) This was attributed to the differences in the pharmacological profiles of the 2 drugs. As shown in Figure 2, the addition of carvedilol to renin-angiotensin-aldosterone-system blockade seemed better tolerated than adding metoprolol. In particular, there were fewer neuropathic, hypoglycemic or hyperglycemic symptoms with carvedilol than with metoprolol. Also notable are results from the United Kingdom Prospective Diabetes Study (UKPDS) which reported no association of target blood pressure levels on HRQOL.(64) However, the high cardiovascular risk exhibited by this patient population underscores the need for focusing on treatment of hypertension, which is a putatively asymptomatic but important risk factor.
Figure 2.
Changes in score in the individual items from the Diabetes Symptom Checklist. Patients with hypertension and type 2 diabetes treated with carvedilol reported a lower perceived burden of diabetes-related symptoms than those treated with metoprolol. Reprinted with permission.(63)
Health-related quality of life in elderly hypertensives
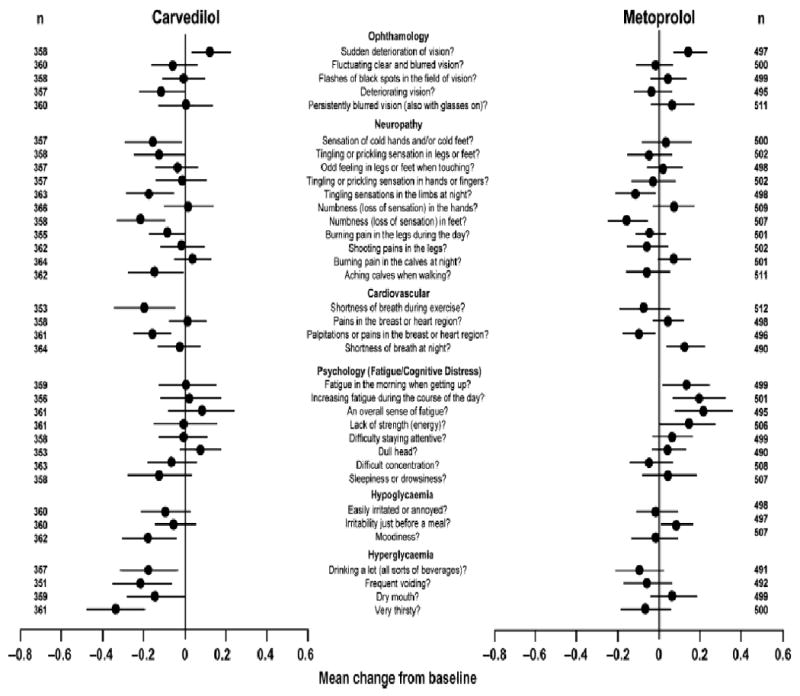
Population-based studies have indicated worse HRQOL in the general population of older than younger adults, particularly in the physical domains of HRQOL measurements.(65) Possible reasons for this finding include the increasing burden of disease, including hypertension among older individuals. HRQOL among hypertensive elderly individuals is of particular interest for several reasons. First, the prevalence of hypertension is higher among elderly individuals than among individuals in younger age groups.(66) This has also been underscored by recent work in the National Health and Nutrition Examination Survery (NHANES)(1) as shown in Figure 3. There is a marked increase in prevalence with increasing age and there are also significantly higher rates of hypertension among non-Hispanic blacks. Second, while hypertension contributes to significant morbidity and mortality in this age group due to cardiovascular disease,(67, 68) it is frequently thought to be asymptomatic, which underscores the importance of examining any decrement to HRQOL caused by treatment of hypertension. To this end, multiple studies have examined the impact of both pharmacologic and non-pharmacologic treatments of hypertension on HRQOL among the elderly population.(69) The effects of anti-hypertensives on HRQOL in the elderly have been reviewed by Fogari and Zoppi(69) (Table 1) and this comprehensive review addressed both pharmacologic and non-pharmacologic studies published through 2003. The authors concluded that although no class of anti-hypertensive agents offered a definite advantage over the others in terms of HRQOL effects, ACE-inhibitors and angiotensin II receptor antagonists were noted to demonstrate an improvement in cognitive ability and sexual function in the elderly.(69)
Figure 3.
Hypertension prevalence in 2003–2004 by age and race/ethnicity in men and women. Data are weighted to the US population. *P_0.05, †P_0.01, ‡P_0.001 for the difference within the same age group (non-Hispanic whites as the referent for race/ethnicity). Error bars indicate 95% confidence intervals. Reprinted with permission. (1)
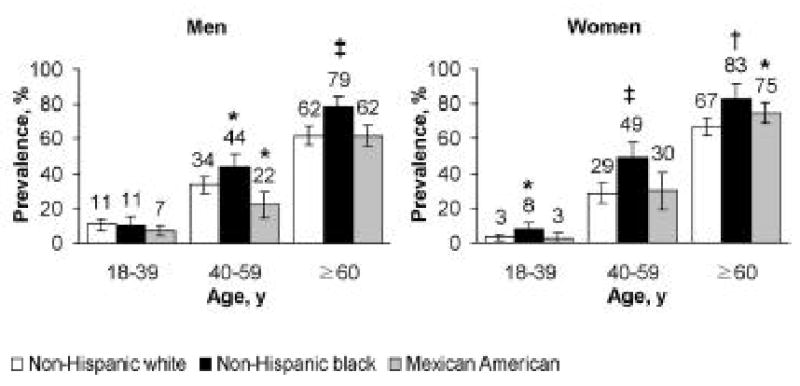
Table 1.
Main potential quality-of-life effects of antihypertensive drugs(69)
| Drug Class | Quality-of-Life Symptoms |
| Diuretics | Impotence, decreased libido, dizziness, lethargy, constipation, nausea, dry eye |
| Beta-adrenoceptor antagonists | Cold extremities, dizziness, fatigue, insomnia, nausea, anorexia, vivid dreams, depression, reduced verbal memory |
| Central alpha-2-adrenoreceptor agonists (Methyl-dopa, clonidine) | Impotence, tiredness, diarrhea, dry mouth, depression, vivid dreams, sleep disturbance, postural hypotension, sedation, reduced verbal memory |
| Alpha-1 adrenoreceptor Antagonists | Postural hypotension, headache |
| Calcium channel antagonists | |
| Dihydropyridines | Ankle edema, flushing, headache, dizziness |
| Non-dihydropyridines | Constipation, headache, nausea, dizziness |
| ACE inhibitors | Cough, rash, taste disturbance, angioedema |
| Angiotensin II receptor antagonists | Dizziness, rash, loss of taste |
In general, studies of pharmacologic treatment of hypertension among the elderly have found either no decrement(22, 70, 71) or improvement in HRQOL associated with anti-hypertensive therapy.(4, 72) Notable is a study that reported a negative impact of antihypertensive treatment in the domain of social interaction, but not in domains of physical function of HRQOL.(73) Possible reasons for these disparate findings include the different instruments used to measure HRQOL, different drugs used for treatment and differences in the ages of the populations studied. The effects on HRQOL of specific classes of antihypertensive drugs including diuretics, beta blockers, calcium channel blockers and ACE inhibitors have been examined in the elderly in several studies, without specific demonstration of superiority of 1 drug class over another in terms of HRQOL measures among elderly individuals.(74-76)
While multiple studies have examined pharmacologic treatments of hypertension and HRQOL in the elderly, few studies have focused on non-pharmacologic treatments and HRQOL. One study examined exercise and HRQOL in a group of post-menopausal hypertensive women. This study found that increasing doses of exercise were associated with improved HRQOL measurements, a finding which was independent of weight loss, but change in blood pressure was not reported.(77)
In summary, elderly individuals are at risk for worse HRQOL and hypertension may contribute to the decrements in HRQOL. As hypertension is a chronic condition, it is important to examine the effect of antihypertensive therapy on HRQOL in this population already at risk for worsened HRQOL. More studies are needed to address the optimum anti-hypertensive therapy for preserving HRQOL in this group.
Conclusion
Hypertension may be associated with lower HRQOL, particularly in domains of physical function. The mechanisms are unclear, but this decrement in HRQOL has broad implications in terms of treatment goals and decisions and prevention of further decreases in HRQOL. One way in which this might occur is by prevention of complications of hypertension including cerebrovascular disease and chronic kidney disease, which both are associated with even greater decreases in HRQOL among individuals with hypertension. Additionally, diabetics and elderly patients with hypertension are also special populations in which consideration of HRQOL preservation is of particular interest.
Acknowledgments
Support and Financial Disclosure Declaration: This work was supported by NIH DK66006 and DK77785 (Unruh). Dr. Unruh also receives grant support from the Paul Teschan Research Fund, Norman Coplon Research Award, and the Baxter Extramural Grant Program. Dr. Unruh serves on the Medical Advisory Board for Baxter Healthcare.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Ong KL, Cheung BM, Man YB, Lau CP, Lam KS. Prevalence, awareness, treatment, and control of hypertension among United States adults 1999-2004. Hypertension. 2007 Jan;49(1):69–75. doi: 10.1161/01.HYP.0000252676.46043.18. [DOI] [PubMed] [Google Scholar]
- 2.Stewart AL, Greenfield S, Hays RD, et al. Functional status and well-being of patients with chronic conditions. Results from the Medical Outcomes Study. JAMA. 1989 Aug 18;262(7):907–913. [PubMed] [Google Scholar]
- 3.Bardage C, Isacson DG. Hypertension and health-related quality of life. an epidemiological study in Sweden. J Clin Epidemiol. 2001 Feb;54(2):172–181. doi: 10.1016/s0895-4356(00)00293-6. [DOI] [PubMed] [Google Scholar]
- 4.Arslantas D, Ayranci U, Unsal A, Tozun M. Prevalence of hypertension among individuals aged 50 years and over and its impact on health related quality of life in a semi-rural area of western Turkey. Chin Med J (Engl) 2008 Aug 20;121(16):1524–1531. [PubMed] [Google Scholar]
- 5.Moum T, Naess S, Sorensen T, Tambs K, Holmen J. Hypertension labelling, life events and psychological well-being. Psychol Med. 1990 Aug;20(3):635–646. doi: 10.1017/s0033291700017153. [DOI] [PubMed] [Google Scholar]
- 6.Mena-Martin FJ, Martin-Escudero JC, Simal-Blanco F, Carretero-Ares JL, Arzua-Mouronte D, Herreros-Fernandez V. Health-related quality of life of subjects with known and unknown hypertension: results from the population-based Hortega study. J Hypertens. 2003 Jul;21(7):1283–1289. doi: 10.1097/00004872-200307000-00015. [DOI] [PubMed] [Google Scholar]
- 7.Cote I, Gregoire JP, Moisan J. Health-related quality-of-life measurement in hypertension. A review of randomised controlled drug trials. Pharmacoeconomics. 2000 Nov;18(5):435–450. doi: 10.2165/00019053-200018050-00003. [DOI] [PubMed] [Google Scholar]
- 8.Coyne KS, Davis D, Frech F, Hill MN. Health-related quality of life in patients treated for hypertension: a review of the literature from 1990 to 2000. Clin Ther. 2002 Jan;24(1):142–169. doi: 10.1016/s0149-2918(02)85012-3. [DOI] [PubMed] [Google Scholar]
- 9.Leppo NE. The first ten years of the World Health Organization. Minn Med. 1958 Aug;41(8):577–583. [PubMed] [Google Scholar]
- 10.Dew MA, Switzer GE, DiMartini AF, Matukaitis J, Fitzgerald MG, Kormos RL. Psychosocial assessments and outcomes in organ transplantation. Prog Transplant. 2000 Dec;10(4):239–259. 260–231. doi: 10.1177/152692480001000408. quiz. [DOI] [PubMed] [Google Scholar]
- 11.Bulpitt CJ, Fletcher AE. The measurement of quality of life in hypertensive patients: a practical approach. Br J Clin Pharmacol. 1990 Sep;30(3):353–364. doi: 10.1111/j.1365-2125.1990.tb03784.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Leonetti G, Comerio G, Cuspidi C. Evaluating quality of life in hypertensive patients. J Cardiovasc Pharmacol. 1994;23(Suppl 5):S54–58. doi: 10.1097/00005344-199423005-00011. [DOI] [PubMed] [Google Scholar]
- 13.Collins AJ, Foley RN, Herzog C, et al. United States Renal Data System 2008 Annual Data Report Abstract. Am J Kidney Dis. 2009 Jan;53(1 Suppl):vi–vii. S8–374. doi: 10.1053/j.ajkd.2008.10.005. [DOI] [PubMed] [Google Scholar]
- 14.K/DOQI clinical practice guidelines on hypertension and antihypertensive agents in chronic kidney disease. Am J Kidney Dis. 2004 May;43(5 Suppl 1):S1–290. [PubMed] [Google Scholar]
- 15.Vasan RS, Larson MG, Leip EP, et al. Impact of high-normal blood pressure on the risk of cardiovascular disease. N Engl J Med. 2001 Nov 1;345(18):1291–1297. doi: 10.1056/NEJMoa003417. [DOI] [PubMed] [Google Scholar]
- 16.Hallan S, Astor B, Romundstad S, Aasarod K, Kvenild K, Coresh J. Association of kidney function and albuminuria with cardiovascular mortality in older vs younger individuals: The HUNT II Study. Arch Intern Med. 2007 Dec 10;167(22):2490–2496. doi: 10.1001/archinte.167.22.2490. [DOI] [PubMed] [Google Scholar]
- 17.Hillege HL, Fidler V, Diercks GF, et al. Urinary albumin excretion predicts cardiovascular and noncardiovascular mortality in general population. Circulation. 2002 Oct 1;106(14):1777–1782. doi: 10.1161/01.cir.0000031732.78052.81. [DOI] [PubMed] [Google Scholar]
- 18.McCullough PA, Soman SS, Shah SS, et al. Risks associated with renal dysfunction in patients in the coronary care unit. J Am Coll Cardiol. 2000 Sep;36(3):679–684. doi: 10.1016/s0735-1097(00)00774-9. [DOI] [PubMed] [Google Scholar]
- 19.Sarnak MJ, Levey AS, Schoolwerth AC, et al. Kidney disease as a risk factor for development of cardiovascular disease: a statement from the American Heart Association Councils on Kidney in Cardiovascular Disease, High Blood Pressure Research, Clinical Cardiology, and Epidemiology and Prevention. Circulation. 2003 Oct 28;108(17):2154–2169. doi: 10.1161/01.CIR.0000095676.90936.80. [DOI] [PubMed] [Google Scholar]
- 20.Kokubo Y, Nakamura S, Okamura T, et al. Relationship between blood pressure category and incidence of stroke and myocardial infarction in an urban Japanese population with and without chronic kidney disease: the Suita Study. Stroke. 2009 Aug;40(8):2674–2679. doi: 10.1161/STROKEAHA.109.550707. [DOI] [PubMed] [Google Scholar]
- 21.Wiklund I, Halling K, Ryden-Bergsten T, Fletcher A. Does lowering the blood pressure improve the mood? Quality-of-life results from the Hypertension Optimal Treatment (HOT) study. Blood Press. 1997 Nov;6(6):357–364. doi: 10.3109/08037059709062095. [DOI] [PubMed] [Google Scholar]
- 22.Degl'Innocenti A, Elmfeldt D, Hofman A, et al. Health-related quality of life during treatment of elderly patients with hypertension: results from the Study on COgnition and Prognosis in the Elderly (SCOPE) J Hum Hypertens. 2004 Apr;18(4):239–245. doi: 10.1038/sj.jhh.1001657. [DOI] [PubMed] [Google Scholar]
- 23.Hansson L. The Hypertension Optimal Treatment study and the importance of lowering blood pressure. J Hypertens Suppl. 1999 Feb;17(1):S9–13. [PubMed] [Google Scholar]
- 24.Hayes DK, Denny CH, Keenan NL, Croft JB, Greenlund KJ. Health-related quality of life and hypertension status, awareness, treatment, and control: National Health and Nutrition Examination Survey, 2001--2004. J Hypertens. 2008 Apr;26(4):641–647. doi: 10.1097/HJH.0b013e3282f3eb50. [DOI] [PubMed] [Google Scholar]
- 25.Rocco MV, Gassman JJ, Wang SR, Kaplan RM. Cross-sectional study of quality of life and symptoms in chronic renal disease patients: the Modification of Diet in Renal Disease Study. Am J Kidney Dis. 1997 Jun;29(6):888–896. doi: 10.1016/s0272-6386(97)90463-7. [DOI] [PubMed] [Google Scholar]
- 26.Perlman RL, Finkelstein FO, Liu L, et al. Quality of life in chronic kidney disease (CKD): a cross-sectional analysis in the Renal Research Institute-CKD study. Am J Kidney Dis. 2005 Apr;45(4):658–666. doi: 10.1053/j.ajkd.2004.12.021. [DOI] [PubMed] [Google Scholar]
- 27.Mujais SK, Story K, Brouillette J, et al. Health-related quality of life in CKD Patients: correlates and evolution over time. Clin J Am Soc Nephrol. 2009 Aug;4(8):1293–1301. doi: 10.2215/CJN.05541008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Finkelstein FO, Wuerth D, Finkelstein SH. Health related quality of life and the CKD patient: challenges for the nephrology community. Kidney Int. 2009 Aug 12; doi: 10.1038/ki.2009.307. [DOI] [PubMed] [Google Scholar]
- 29.Weiner DE. Public health consequences of chronic kidney disease. Clin Pharmacol Ther. 2009 Nov;86(5):566–569. doi: 10.1038/clpt.2009.137. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Kusek JW, Lee JY, Smith DE, et al. Effect of blood pressure control and antihypertensive drug regimen on quality of life: the African American Study of Kidney Disease and Hypertension (AASK) Pilot Study. Control Clin Trials. 1996 Aug;17(4 Suppl):40S–46S. doi: 10.1016/s0197-2456(97)82681-5. [DOI] [PubMed] [Google Scholar]
- 31.Wright JT, Jr, Kusek JW, Toto RD, et al. Design and baseline characteristics of participants in the African American Study of Kidney Disease and Hypertension (AASK) Pilot Study. Control Clin Trials. 1996 Aug;17(4 Suppl):3S–16S. doi: 10.1016/s0197-2456(96)00081-5. [DOI] [PubMed] [Google Scholar]
- 32.Kusek JW, Greene P, Wang SR, et al. Cross-sectional study of health-related quality of life in African Americans with chronic renal insufficiency: the African American Study of Kidney Disease and Hypertension Trial. Am J Kidney Dis. 2002 Mar;39(3):513–524. doi: 10.1053/ajkd.2002.31401. [DOI] [PubMed] [Google Scholar]
- 33.Lash JP, Wang X, Greene T, et al. Quality of life in the African American Study of Kidney Disease and Hypertension: effects of blood pressure management. Am J Kidney Dis. 2006 Jun;47(6):956–964. doi: 10.1053/j.ajkd.2006.02.175. [DOI] [PubMed] [Google Scholar]
- 34.The treatment of mild hypertension study. A randomized, placebo-controlled trial of a nutritional-hygienic regimen along with various drug monotherapies. The Treatment of Mild Hypertension Research Group. Arch Intern Med. 1991 Jul;151(7):1413–1423. doi: 10.1001/archinte.151.7.1413. [DOI] [PubMed] [Google Scholar]
- 35.De Rosa ML, Cardace P, Rossi M, Baiano A, de Cristofaro A. Comparative effects of chronic ACE inhibition and AT1 receptor blocked losartan on cardiac hypertrophy and renal function in hypertensive patients. J Hum Hypertens. 2002 Feb;16(2):133–140. doi: 10.1038/sj.jhh.1001305. [DOI] [PubMed] [Google Scholar]
- 36.Ruggenenti P, Perna A, Gherardi G, et al. Renoprotective properties of ACE-inhibition in non-diabetic nephropathies with non-nephrotic proteinuria. Lancet. 1999 Jul 31;354(9176):359–364. doi: 10.1016/S0140-6736(98)10363-X. [DOI] [PubMed] [Google Scholar]
- 37.Agodoa LY, Appel L, Bakris GL, et al. Effect of ramipril vs amlodipine on renal outcomes in hypertensive nephrosclerosis: a randomized controlled trial. JAMA. 2001 Jun 6;285(21):2719–2728. doi: 10.1001/jama.285.21.2719. [DOI] [PubMed] [Google Scholar]
- 38.Randomised placebo-controlled trial of effect of ramipril on decline in glomerular filtration rate and risk of terminal renal failure in proteinuric, non-diabetic nephropathy. The GISEN Group (Gruppo Italiano di Studi Epidemiologici in Nefrologia) Lancet. 1997 Jun 28;349(9069):1857–1863. [PubMed] [Google Scholar]
- 39.Ruggenenti P, Perna A, Remuzzi G. ACE inhibitors to prevent end-stage renal disease: when to start and why possibly never to stop: a post hoc analysis of the REIN trial results. Ramipril Efficacy in Nephropathy. J Am Soc Nephrol. 2001 Dec;12(12):2832–2837. doi: 10.1681/ASN.V12122832. [DOI] [PubMed] [Google Scholar]
- 40.Maschio G, Alberti D, Janin G, et al. Effect of the angiotensin-converting-enzyme inhibitor benazepril on the progression of chronic renal insufficiency. The Angiotensin-Converting-Enzyme Inhibition in Progressive Renal Insufficiency Study Group. N Engl J Med. 1996 Apr 11;334(15):939–945. doi: 10.1056/NEJM199604113341502. [DOI] [PubMed] [Google Scholar]
- 41.Chiurchiu C, Remuzzi G, Ruggenenti P. Angiotensin-converting enzyme inhibition and renal protection in nondiabetic patients: the data of the meta-analyses. J Am Soc Nephrol. 2005 Mar;16(Suppl 1):S58–63. doi: 10.1681/asn.2004110968. [DOI] [PubMed] [Google Scholar]
- 42.Swenson JR, Clinch JJ. Assessment of quality of life in patients with cardiac disease: the role of psychosomatic medicine. J Psychosom Res. 2000 Apr-May;48(4-5):405–415. doi: 10.1016/s0022-3999(99)00092-6. [DOI] [PubMed] [Google Scholar]
- 43.Li C, Ford ES, Mokdad AH, Balluz LS, Brown DW, Giles WH. Clustering of cardiovascular disease risk factors and health-related quality of life among US adults. Value Health. 2008 Jul-Aug;11(4):689–699. doi: 10.1111/j.1524-4733.2007.00307.x. [DOI] [PubMed] [Google Scholar]
- 44.Bayliss EA, Bayliss MS, Ware JE, Jr, Steiner JF. Predicting declines in physical function in persons with multiple chronic medical conditions: what we can learn from the medical problem list. Health Qual Life Outcomes. 2004;2:47. doi: 10.1186/1477-7525-2-47. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Kalantar-Zadeh K, Unruh M. Health related quality of life in patients with chronic kidney disease. Int Urol Nephrol. 2005;37(2):367–378. doi: 10.1007/s11255-004-0012-4. [DOI] [PubMed] [Google Scholar]
- 46.Aydemir O, Ozdemir C, Koroglu E. The impact of co-morbid conditions on the SF-36: a primary-care-based study among hypertensives. Arch Med Res. 2005 Mar-Apr;36(2):136–141. doi: 10.1016/j.arcmed.2004.12.009. [DOI] [PubMed] [Google Scholar]
- 47.Johansen KL, Kutner NG, Young B, Chertow GM. Association of body size with health status in patients beginning dialysis. Am J Clin Nutr. 2006 Mar;83(3):543–549. doi: 10.1093/ajcn.83.3.543. [DOI] [PubMed] [Google Scholar]
- 48.Souza EN, Quadros AS, Maestri R, Albarran C, Sarmento-Leite R. Predictors of quality of life change after an acute coronary event. Arq Bras Cardiol. 2008 Oct;91(4):229–235. 252–229. doi: 10.1590/s0066-782x2008001600008. [DOI] [PubMed] [Google Scholar]
- 49.Kapetanakis EI, Stamou SC, Petro KR, et al. Comparison of the quality of life after conventional versus off-pump coronary artery bypass surgery. J Card Surg. 2008 Mar-Apr;23(2):120–125. doi: 10.1111/j.1540-8191.2008.00590.x. [DOI] [PubMed] [Google Scholar]
- 50.Herlitz J, Caidahl K, Wiklund I, et al. Impact of a history of hypertension on symptoms and quality of life prior to and at five years after coronary artery bypass grafting. Blood Press. 2000;9(1):52–63. [PubMed] [Google Scholar]
- 51.Agewall S, Wikstrand J, Dahlof C, Fagerberg B. Negative feelings (discontent) predict progress of intima-media thickness of the common carotid artery in treated hypertensive men at high cardiovascular risk. Am J Hypertens. 1996 Jun;9(6):545–550. doi: 10.1016/0895-7061(95)00355-x. [DOI] [PubMed] [Google Scholar]
- 52.Wild S, Roglic G, Green A, Sicree R, King H. Global prevalence of diabetes: estimates for the year 2000 and projections for 2030. Diabetes Care. 2004 May;27(5):1047–1053. doi: 10.2337/diacare.27.5.1047. [DOI] [PubMed] [Google Scholar]
- 53.Rubin RR, Peyrot M. Quality of life and diabetes. Diabetes Metab Res Rev. 1999 May-Jun;15(3):205–218. doi: 10.1002/(sici)1520-7560(199905/06)15:3<205::aid-dmrr29>3.0.co;2-o. [DOI] [PubMed] [Google Scholar]
- 54.Wee HL, Cheung YB, Li SC, Fong KY, Thumboo J. The impact of diabetes mellitus and other chronic medical conditions on health-related Quality of Life: is the whole greater than the sum of its parts. Health Qual Life Outcomes. 2005;3:2. doi: 10.1186/1477-7525-3-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Miksch A, Hermann K, Rolz A, et al. Additional impact of concomitant hypertension and osteoarthritis on quality of life among patients with type 2 diabetes in primary care in Germany - a cross-sectional survey. Health Qual Life Outcomes. 2009;7:19. doi: 10.1186/1477-7525-7-19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Papadopoulos AA, Kontodimopoulos N, Frydas A, Ikonomakis E, Niakas D. Predictors of health-related quality of life in type II diabetic patients in Greece. BMC Public Health. 2007;7:186. doi: 10.1186/1471-2458-7-186. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Lloyd A, Sawyer W, Hopkinson P. Impact of long-term complications on quality of life in patients with type 2 diabetes not using insulin. Value Health. 2001 Sep-Oct;4(5):392–400. doi: 10.1046/j.1524-4733.2001.45029.x. [DOI] [PubMed] [Google Scholar]
- 58.Wexler DJ, Grant RW, Wittenberg E, et al. Correlates of health-related quality of life in type 2 diabetes. Diabetologia. 2006 Jul;49(7):1489–1497. doi: 10.1007/s00125-006-0249-9. [DOI] [PubMed] [Google Scholar]
- 59.Hart HE, Redekop WK, Berg M, Bilo HJ, Meyboom-de Jong B. Factors that predicted change in health-related quality of life were identified in a cohort of diabetes mellitus type 1 patients. J Clin Epidemiol. 2005 Nov;58(11):1158–1164. doi: 10.1016/j.jclinepi.2005.02.021. [DOI] [PubMed] [Google Scholar]
- 60.Mena Martin FJ, Martin Escudero JC, Simal Blanco F, Bellido Casado J, Carretero Ares JL. [Type 2 diabetes mellitus and health-related quality of life: results from the Hortega Study] An Med Interna. 2006 Aug;23(8):357–360. doi: 10.4321/s0212-71992006000800002. [DOI] [PubMed] [Google Scholar]
- 61.Bounthavong M, Law AV. Identifying health-related quality of life (HRQL) domains for multiple chronic conditions (diabetes, hypertension and dyslipidemia): patient and provider perspectives. J Eval Clin Pract. 2008 Dec;14(6):1002–1011. doi: 10.1111/j.1365-2753.2007.00933.x. [DOI] [PubMed] [Google Scholar]
- 62.Ostman J, Asplund K, Bystedt T, et al. Comparison of effects of quinapril and metoprolol on glycaemic control, serum lipids, blood pressure, albuminuria and quality of life in non-insulin-dependent diabetes mellitus patients with hypertension. Swedish Quinapril Group. J Intern Med. 1998 Aug;244(2):95–107. doi: 10.1046/j.1365-2796.1998.00319.x. [DOI] [PubMed] [Google Scholar]
- 63.McGill JB, Bakris GL, Fonseca V, et al. beta-blocker use and diabetes symptom score: results from the GEMINI study. Diabetes Obes Metab. 2007 May;9(3):408–417. doi: 10.1111/j.1463-1326.2006.00693.x. [DOI] [PubMed] [Google Scholar]
- 64.Quality of life in type 2 diabetic patients is affected by complications but not by intensive policies to improve blood glucose or blood pressure control (UKPDS 37). U.K. Prospective Diabetes Study Group. Diabetes Care. 1999 Jul;22(7):1125–1136. doi: 10.2337/diacare.22.7.1125. [DOI] [PubMed] [Google Scholar]
- 65.Zahran HS, Kobau R, Moriarty DG, Zack MM, Holt J, Donehoo R. Health-related quality of life surveillance--United States, 1993-2002. MMWR Surveill Summ. 2005 Oct 28;54(4):1–35. [PubMed] [Google Scholar]
- 66.Cutler JA, Sorlie PD, Wolz M, Thom T, Fields LE, Roccella EJ. Trends in hypertension prevalence, awareness, treatment, and control rates in United States adults between 1988-1994 and 1999-2004. Hypertension. 2008 Nov;52(5):818–827. doi: 10.1161/HYPERTENSIONAHA.108.113357. [DOI] [PubMed] [Google Scholar]
- 67.Prevention of stroke by antihypertensive drug treatment in older persons with isolated systolic hypertension. Final results of the Systolic Hypertension in the Elderly Program (SHEP). SHEP Cooperative Research Group. JAMA. 1991 Jun 26;265(24):3255–3264. [PubMed] [Google Scholar]
- 68.Beckett NS, Peters R, Fletcher AE, et al. Treatment of hypertension in patients 80 years of age or older. N Engl J Med. 2008 May 1;358(18):1887–1898. doi: 10.1056/NEJMoa0801369. [DOI] [PubMed] [Google Scholar]
- 69.Fogari R, Zoppi A. Effect of antihypertensive agents on quality of life in the elderly. Drugs Aging. 2004;21(6):377–393. doi: 10.2165/00002512-200421060-00003. [DOI] [PubMed] [Google Scholar]
- 70.Applegate WB, Pressel S, Wittes J, et al. Impact of the treatment of isolated systolic hypertension on behavioral variables. Results from the systolic hypertension in the elderly program. Arch Intern Med. 1994 Oct 10;154(19):2154–2160. [PubMed] [Google Scholar]
- 71.Degl'Innocenti A, Elmfeldt D, Hansson L, et al. Cognitive function and health-related quality of life in elderly patients with hypertension--baseline data from the study on cognition and prognosis in the elderly (SCOPE) Blood Press. 2002;11(3):157–165. doi: 10.1080/080370502760050395. [DOI] [PubMed] [Google Scholar]
- 72.Robbins MA, Elias MF, Croog SH, Colton T. Unmedicated blood pressure levels and quality of life in elderly hypertensive women. Psychosom Med. 1994 May-Jun;56(3):251–259. doi: 10.1097/00006842-199405000-00012. [DOI] [PubMed] [Google Scholar]
- 73.Fletcher AE, Bulpitt CJ, Thijs L, et al. Quality of life on randomized treatment for isolated systolic hypertension: results from the Syst-Eur Trial. J Hypertens. 2002 Oct;20(10):2069–2079. doi: 10.1097/00004872-200210000-00028. [DOI] [PubMed] [Google Scholar]
- 74.Applegate WB, Phillips HL, Schnaper H, et al. A randomized controlled trial of the effects of three antihypertensive agents on blood pressure control and quality of life in older women. Arch Intern Med. 1991 Sep;151(9):1817–1823. [PubMed] [Google Scholar]
- 75.Benetos A, Consoli S, Safavian A, Dubanchet A, Safar M. Efficacy, safety, and effects on quality of life of bisoprolol/hydrochlorothiazide versus amlodipine in elderly patients with systolic hypertension. Am Heart J. 2000 Oct;140(4):E11. doi: 10.1067/mhj.2000.108834. [DOI] [PubMed] [Google Scholar]
- 76.Bulpitt CJ, Connor M, Schulte M, Fletcher AE. Bisoprolol and nifedipine retard in elderly hypertensive patients: effect on quality of life. J Hum Hypertens. 2000 Mar;14(3):205–212. doi: 10.1038/sj.jhh.1000972. [DOI] [PubMed] [Google Scholar]
- 77.Martin CK, Church TS, Thompson AM, Earnest CP, Blair SN. Exercise dose and quality of life: a randomized controlled trial. Arch Intern Med. 2009 Feb 9;169(3):269–278. doi: 10.1001/archinternmed.2008.545. [DOI] [PMC free article] [PubMed] [Google Scholar]


