Abstract
Background
Both N-terminal pro B-type natriuretic peptide (NT-pro BNP) and depressive symptoms independently predict cardiac events in heart failure (HF) patients. However, the relationship among NT-pro BNP, depressive symptoms, and cardiac event is unknown.
Methods and Results
Blood was drawn to measure NT-pro BNP and depressive symptoms were measured by the Patient Health Questionnaire 9 (PHQ-9) among 210 patients with HF. Data about cardiac event-free survival were collected for the average follow-up period of 397 days. Cox proportional hazards regression with survival curves were used to determine the relationship of NT-pro BNP and depressive symptoms to cardiac event-free survival. Higher NT-pro-BNP confers greater risk of cardiac events among those with depressive symptoms than those without depressive symptoms (p for the interaction = .029). Patients with NT-pro BNP > 581 pg/ml and total PHQ-9 score ≥ 10 had a 5.5 times higher risk for cardiac events, compared to patients with NT-pro BNP ≤ 581 pg/ml and total PHQ-9 score < 10 (p = .001).
Conclusions
The prognostic association of NT-pro BNP with cardiac event-free survival in patients with HF differed by the presence of depressive symptoms. Monitoring and treatment of depressive symptoms may be important for improving cardiac event-free survival in patients with HF.
INTRODUCTION
Heart failure (HF) currently afflicts approximately 5.3 million people in the United States.1 Approximately 27% of patients with HF are rehospitalized in the 90 days after discharge for decompensated HF and about one third of these patients have multiple admissions.2, 3 The annual hospitalization rate for a primary or secondary diagnosis of HF increased approximately 1.5 times during the past decade.4, 5 HF is the major cause of death for individuals over 65 years old with one year mortality rates of about 20%.3, 6
Accordingly, prior investigators have focused on identifying predictors of adverse outcomes following HF diagnosis. B-type natriuretic peptide (BNP) and N-terminal pro BNP (NT-pro BNP) have been identified as biological markers that provide prognostic and diagnostic value in individuals with symptoms of decompensated HF.7-9 The presence of depressive symptoms is a significant problem for many patients with HF. Approximately 22% of patients with HF suffer from clinical depression,10 while up to 36% have significant depressive symptoms.11, 12 Individuals can experience significant depressive symptoms without the diagnosis of major depressive disorder.13 A recent meta analysis demonstrated that patients with HF who have depressive symptoms are more than twice as likely to die or experience a cardiac event when compared to those without depressive symptoms.10
To date, researchers have compared the prognostic value of NT-pro BNP relative to other traditional risk factors such as age, gender, ischemic heart disease, body mass index (BMI), New York Heart Association (NYHA) functional class, left ventricular ejection fraction (LVEF), and comorbidities.14-16 However, the prognostic value of NT-pro BNP has not been considered in the context of psychosocial factors. Given the high prevalence of depressive symptoms and their prognostic implications in HF, study of the prognostic value of NT-pro BNP in the context of depressive symptoms may be particularly important and clinically relevant. Thus, the purpose of this study was to determine whether the association of NT-pro BNP with cardiac event-free survival differed by the presence of depressive symptoms among HF patients.
METHOD
Design and procedure
This was a prospective study of patients with HF recruited from outpatient HF clinics between January 1, 2004 and December 31, 2007. Patients were recruited from one regional tertiary medical center and several community hospitals located in Lexington, Kentucky. Approval from the Institutional Review Board at each of the hospitals was obtained prior to the study. Written informed consent was obtained from patients. At baseline, all patients visited the General Clinical Research Center to have blood drawn and complete baseline questionnaires. After baseline assessment, patients were followed by monthly telephone interview for 12-months.
Sample
Patients recruited had a diagnosis of chronic HF with impaired left ventricular systolic function (LVEF ≤ 40%) or preserved systolic function (LVEF > 40%) and any NYHA functional class. Diagnosis of chronic HF and HF etiology were confirmed by a cardiologist using established criteria. Patients were included in this study if they had undergone evaluation for HF, were receiving stable doses of drugs for at least three month and had not been referred for heart transplantation. Patients were excluded if they had valvular heart disease, peripartum heart failure, myocarditis or other known inflammatory process, history of cerebrovascular accident or recent myocardial infarction within past 3 months, or any co-existing terminal illness.
A total of 222 patients were eligible for this study. Six patients withdrew and one patient refused to participate. Five patients were lost to follow-up. Thus, data from 210 patients were included in the analysis.
Measurements of variables
N-terminal pro B-type natriuretic peptide (NT-pro BNP)
We used NT-pro BNP as it may be considered the best marker of prognosis in patients with HF.9, 17 BNP is a 32 amino acid polypeptide secreted by ventricular walls of the heart.9 In response to excessive stretching and tension of the myocardium, BNP’s precursor pro BNP splits into BNP and the physiologically inactive remnant, NT-pro BNP.18 The half-life of NT-pro BNP is 120 minutes; whereas, the half-life of BNP is around 20 minutes.19, 20 Higher levels of NT-pro BNP than BNP were detected in patients with left ventricular dysfunction,7, 21 whereas, the serum level of BNP and NT-pro BNP are similar in people without HF.
Except for taking their regularly prescribed medication, patients fasted overnight and blood samples were drawn into chilled tubes containing EDTA. Although fasting is not required for the measurement of NT-pro BNP, patients were fasting for other aspects of the protocol. The electrochemiluminescence immunoassay (Roche Diagnostics)9 was used to assess NT-pro BNP concentration. The detectable range of NT-pro BNP with this technique is 5 to 35,000 pg/mL. The technician who performed these assays was blinded to patient status. NT-pro BNP has been approved for use in diagnosing HF by the FDA.22 Because there is no standard value to determine prognosis,9, 23, 24 a receiver operating characteristic (ROC) curve was used to assess the prognostic value of NT-pro BNP. The area under the curve for the ROC curve was .695, significantly different from the null value of .5 (p = .005); NT-pro BNP discerned cases from non-cases approximately 70% of the time. It was determined from the ROC curve using the median split of NT-pro BNP (581 pg/ml) to predict cardiac events resulted in the optimal combination of sensitivity (65%) and specificity (55%). With 581 pg/ml as the cut-off point, time to first cardiac event was significantly different between the two groups (p = .005).
Depressive symptoms
Depressive symptoms were measured by the Patient Health Questionnaire 9 (PHQ-9).25, 26 The PHQ-9 is based directly on the diagnostic criteria for major depressive disorder in the DSM-IV.25, 26 It consists of 9 items; little interest or pleasure, feeling down or depressed, trouble falling or staying asleep, or sleeping too much, feeling tired, poor appetite or overeating, feeling bad about themselves, trouble concentrating, moving or speaking so slowly or fidgety, and thought of suicide or hurting themselves.25, 26 These 9 items are self-rated by the patient on a 4-point scale ranging from 0 (not at all) to 3 (nearly every day). The scores can range from 0 to 27 and higher scores indicate more severe depressive symptoms. Patients were categorized into 2 groups based on their PHQ-9 total score: those with depressive symptoms (total PHQ-9 score ≥10) and those without depressive symptoms (total PHQ-9 score <10). Ten is the published cut-point.25 This cut-point has a sensitivity of 83% and a specificity of 90% for diagnosing major depressive disorder.25 The PHQ-9 has been used in scores of studies to assess for depressive symptoms and has evidence of reliability and validity. In this study, the Cronbach’s alpha coefficient of the PHQ-9 was 0.76.
Other risk factors
The following variables have been identified as traditional risk factors which are associated with prognosis of patients with HF in prior resesearches5, 24, 27-32; older age, female gender, ischemic heart disease as underlying HF etiology, low BMI, worse NYHA functional class, lower LVEF, and comorbidities such as diabetes and renal dysfunction are associated with poor prognosis in patients with HF. Data on age, gender, etiology of HF, BMI, NYHA functional class, LVEF, and total comorbidity score using the Charlson comorbidity index were collected through patient interview and medical record review.
Cardiac event-free survival
The primary outcome of this study was a composite end-point of time to first event of emergency department (ED) visit, hospitalization, or death due to HF exacerbation and other cardiac-related problems for 12-months follow-up periods. During monthly telephone follow-up interviews, patients were asked about all hospitalization or ED visits. The date and cause of any reported events determined by monthly telephone interview were confirmed by hospital record review by a nurse with expertise in HF. Data about death were obtained from family members, physicians, medical record, and death certificates.
Statistical Analysis
Statistical analyses were conducted using SPSS for Windows 16.0. The ANOVA or chi-square test was used to compare difference in sample characteristics of patients categorized into 4 groups by the median value of NT-pro BNP and by total PHQ-9 score of 10. Cox proportional hazards regressions were used to determine whether NT-pro BNP and depressive symptoms were independent predictors of cardiac event-free survival in patients with HF after controlling for age, gender, etiology of HF, BMI, NYHA functional class, LVEF, and total comorbidity score. Cox proportional hazards regression with standard survival curves was used to determine whether the association between NT-pro BNP and cardiac event-free survival differed by presence of depressive symptoms among patients with HF after adjusting for the same risk factors, and the interaction of depression and NT-pro BNP. The statistical significance of the interaction of NT-pro BNP by depressive symptoms was assessed using likelihood ratio test, comparing the models with main effects only with the models that included the interaction term. Proportional hazard assumption indicated that covariates are independent with respect to time and their hazards are constant over time.33 Proportional hazard assumptions were confirmed through visual inspection of the log (−log) survival curves. A hazard ratio (HR) for cardiac events was obtained for all independent variables along with 95% confidence intervals (CIs).
RESULTS
Sample characteristics
Sample characteristics are displayed in Table 1. The majority of the patients were over 60 years old with an age range of 24 to 87 years. As a group, patients were primarily in NYHA functional class II/III. Nearly two thirds had ischemic heart disease as the underlying etiology of HF. Almost one third of the patients had preserved systolic function with LVEF > 40%. The common comorbidities were hypertension and diabetes mellitus. The mean value of NT-pro BNP was 733 pg/ml while the median value was 581 pg/ml with a range from 143 to 3301pg/ml. Twenty seven percent of patients had depressive symptoms as indicated by a PHQ-9 score greater than or equal to 10. Approximately 25% of patients taking antidepressant agents had higher total PHQ-9 scores indicating greater depressive symptoms than patients who were not prescribed antidepressants (8.4 ± 5.6 vs 5.5 ± 5.3, p < .001).
Table 1.
Patient characteristics
N = 210
| Characteristics | N (%) | Mean ± SD | |
|---|---|---|---|
| Age (years) | 61 ± 11 | ||
| Gender | Male | 147 (70.0) | |
| Female | 63 (30.0) | ||
| Body mass index (kg/m2) | 31.9 ± 7.6 | ||
| Normal weight (18.5 ~ 24.9) | 39 (18.6) | ||
| Overweight (25.0 ~ 29.9) | 54 (25.7) | ||
| Obese(≥ 30.0) | 117 (55.7) | ||
| NYHA functional class | I | 16 ( 7.6) | |
| II | 74 (35.2) | ||
| III | 90 (42.9) | ||
| IV | 30 (14.3) | ||
| Heart failure etiology | Non-ischemic heart disease | 92 (43.8) | |
| Ischemic heart disease | 118 (56.2) | ||
| Medication | ACE inhibitors | 154 (73.3) | |
| Angiotension II receptor blocker | 20 ( 9.5) | ||
| Digoxin | 70 (33.3) | ||
| β blocker | 142 (88.2) | ||
| Diuretics | 154 (73.3) | ||
| Aldosterone antagonist | 43 (20.5) | ||
| Antidepressants | 52 (24.8) | ||
| Left ventricular ejection fraction (%) | 34.6 ± 14.4 | ||
| <40% | 138 (65.7) | ||
| ≥ 40% | 72 (34.3) | ||
| Total comorbidity score | 3.4 ± 2.1 | ||
| Hypertension | 159 (75.7) | ||
| Diabetes mellitus | 95 (45.2) | ||
| Atrial fibrillation | 91 (43.3) | ||
| Cerebrovascular attack | 45 (21.4) | ||
| N-terminal pro B type natriuretic peptide (pg/ml) | 733 ± 504 | ||
| Depressive symptoms (The Patient Health Questionnaire 9 score ) | 6.3 ± 5.5 | ||
| No depressive symptoms (0 to 9) | 153 (72.9) | ||
| Depressive symptoms (10 to 27) | 57 (27.1) | ||
ACE, angiotensin converting enzyme, NYHA; New York Heart Association
Different sample characteristics in 4 groups classified by levels of NT-pro BNP and presence of depressive symptoms
Sample characteristics of patients categorized by level of NT-pro BNP and by the presence of depressive symptoms are shown in Table 2. Women more commonly had depressive symptoms than men. Patients with depressive symptoms had worse NYHA functional class and higher total comorbidity scores than those without depressive symptoms. Patients with high concentrations of NT-pro BNP had lower BMI and more ischemic heart disease than patients with low concentrations of NT-pro BNP. Patients who had depressive symptoms were prescribed antidepressants more than those without depressive symptoms.
Table 2.
Sample characteristics among 4 groups classified by NT-pro BNP and depressive symptoms
N = 210
| No depressive symptoms (n = 153) |
Depressive symptoms (n = 57) |
||||
|---|---|---|---|---|---|
| Characteristics | Low NT-pro BNP (n = 70) |
High NT-pro BNP (n = 83) |
Low NT-pro BNP (n = 35) |
High NT-pro BNP (n = 22) |
p |
| Age, years | 58 ± 11 | 66 ± 11 | 56 ± 8 | 56 ± 9 | < .001 |
| Female gender (%) | 21 (30) | 19 (23) | 16 (46) | 7 (32) | .105 |
| BMI, kg/m2 | 34.5 ± 8.0 | 29.3 ± 6.5 | 34.1 ± 7.7 | 30.4 ± 7.4 | < .001 |
| NYHA functional class III/IV (%) |
28 (42) | 43 (53) | 25 (78) | 19 (86) | < .001 |
| IHD (%) | 32 (46) | 60 (72) | 15 (43) | 11 (50) | .002 |
| LVEF, % | 34 ± 13 | 34 ± 16 | 37 ± 13 | 32 ± 16 | .606 |
| Total comorbidity score |
2.7 ± 1.5 | 3.7 ± 2.2 | 3.7 ± 2.5 | 4.1 ± 2.1 | .003 |
| Antidepressants | 10 (15) | 14 (40) | 19 (23) | 9 (45) | .006 |
BMI; Body mass index, IHD; ischemic heart disease, LVEF; left ventricular ejection fraction, NYHA; New York Heart Association, NT-pro BNP; N-terminal pro B-type natriuretic peptide
Cardiac event-free survival
During the average follow-up period of 397 days, 13 patients (6.2%) died, 36 (17.1%) were hospitalized, and 9 (4.3%) had ED visits due to decompensated HF and cardiac-related cause. The average time to the first event of ED visits, hospitalization, or mortality was 235 days.
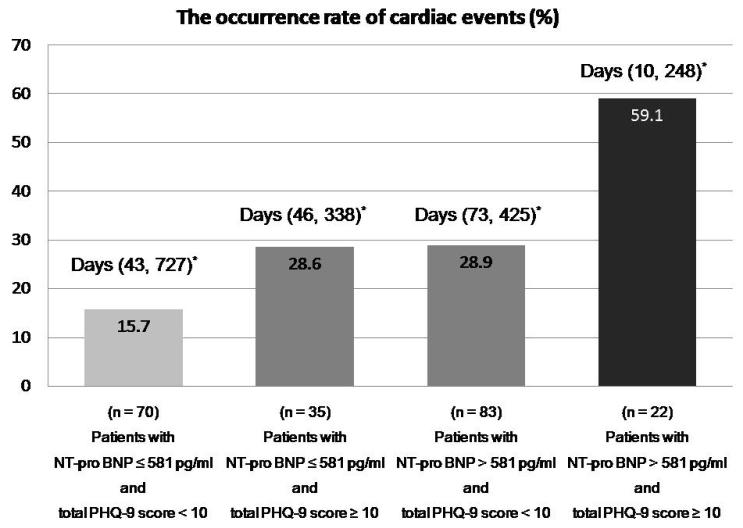
The incidence of cardiac events, and 25th % and 75th % of time to first cardiac event among 4 groups categorized by NT-pro BNP and depressive symptoms is shown in Figure 1.
Figure 1.
Differences in the incidence of cardiac events and time to first cardiac event among 4 groups classified by NT-pro BNP and depressive symptoms (N = 210)
*; (25th % of time to first cardiac event, 75th % of time to first cardiac event)
NT-pro BNP and depressive symptoms as independent predictors of cardiac event-free survival
In Cox regression, high concentration of NT-pro BNP and depressive symptoms independently predicted cardiac event-free survival after controlling for age, gender, etiology of HF, BMI, NYHA class, LVEF, and total comorbidity score. Patients with NT-pro BNP above 581 pg/ml were approximately twice likely to experience cardiac events as compared to those with NT-pro BNP below 581 pg/ml (p = .027). Patients with depressive symptoms had a 2.7-fold higher risk for cardiac events than those without depressive symptoms (p = .005) (Table 3).
Table 3.
Independent predictors of cardiac event-free survival in patients with heart failure
N = 210
| Characteristics | Adjusted HR |
95% CI | p | |
|---|---|---|---|---|
| Risk factors | ||||
| Age (year) | 0.98 | 0.95 - 1.01 | .163 | |
| Gender | Male | 1.00 | ||
| Female | 0.79 | 0.39 - 1.59 | .504 | |
| Body mass index (kg/m2) | 0.97 | 0.93 - 1.02 | .277 | |
| NYHA functional class | I | 1.00 | ||
| II | 0.96 | 0.32 - 2.86 | .946 | |
| III | 0.66 | 0.22 - 2.02 | .468 | |
| IV | 0.62 | 0.16 - 2.36 | .481 | |
| Heart failure etiology | Non-IHD | 1.00 | ||
| IHD | 2.02 | 0.98 - 4.16 | .058 | |
| Left ventricular ejection fraction (%) | 0.99 | 0.97 - 1.02 | .505 | |
| Total comorbidity | 1.03 | 0.87 - 1.22 | .766 | |
|
| ||||
| Independent predictors | ||||
| NT-pro BNP | ≤ 581 pg/ml | 1.00 | ||
| > 581 pg/ml | 2.02 | 1.08 - 3.78 | .027 | |
| Depressive symptoms (total PHQ-9 score) |
No depressive symptoms (0 - 9) | 1.00 | ||
| Depressive symptoms (10 - 27) | 2.70 | 1.35 - 5.39 | .005 | |
CI; confidence interval, IHD; ischemic heart disease, HR; hazard ratio, NYHA; New York Heart Association, NT-pro BNP; N-terminal pro B-type natriuretic peptide, PHQ-9; the Patient Health Questionnaire 9
The relationship of NT-pro BNP, depressive symptoms, and cardiac event-free survival
The greater risk for cardiac events of patients with NT-pro BNP > 581 pg/ml were higher in the presence of depressive symptoms than in the absence of depressive symptoms (p for interaction = .001). After controlling for the same risk factors, a stronger association between NT-pro BNP and cardiac event-free survival was shown among patients with depressive symptoms but not among those without depressive symptoms (p for interaction = .029) (Table 4).
Table 4.
Interaction effects of NT-pro BNP by depressive symptoms on cardiac event-free survival in patients with heart failure
N = 210
| Characteristics | Unadjusted HR (95% CI) |
P* | Adjusted HR (95% CI) |
P** | |
|---|---|---|---|---|---|
| NT-pro BNP ≤ 581 pg/ml | 1.00 | 1.00 | |||
| NT-pro BNP > 581 pg | 2.13 (1.04-4.36) |
.038 | 1.80 (0.81-3.97) |
.151 | |
|
| |||||
| Depressive symptoms (total PHQ-9 score≥10) |
NT-pro BNP ≤ 581 pg/ml | 1.00 | |||
| NT-pro BNP > 581 pg/ml | 3.26 (1.42-7.48) |
.005 | 3.48 (1.04 - 11.69) |
.043 | |
; P value for the interaction effect of NT-pro BNP by depressive symptoms = .001
; P value for the interaction effect of NT-pro BNP by depressive symptoms = .029
CI; confidence interval, NT-pro BNP; N-terminal pro B-type natriuretic peptide, PHQ-9; the Patient Health Questionnaire 9
Adjusted hazard ratio (HR) was obtained from controlling for age, gender, etiology of HF, BMI, NYHA class, LVEF, and total comorbidity score.
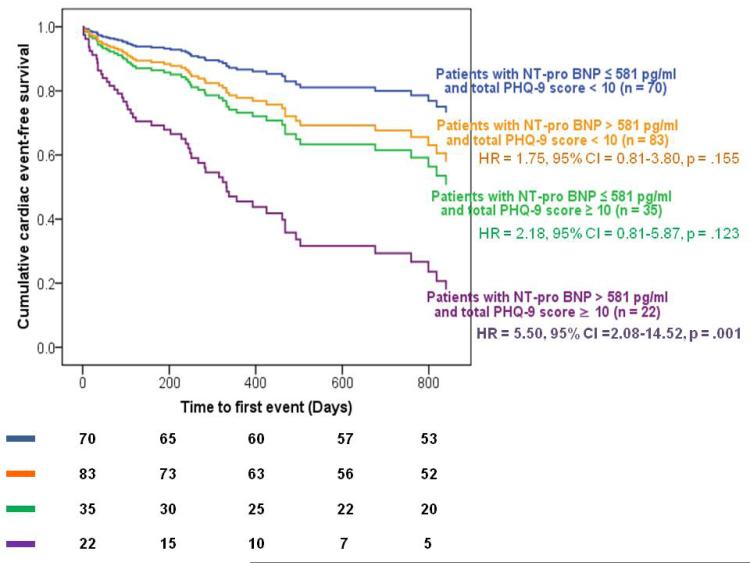
The group who had NT-pro BNP greater than 581 pg/ml and depressive symptoms showed shorter cardiac event-free survival than those with NT-pro BNP ≤ 581 pg/ml and no depressive symptoms (p = .001), after adjusting for the same risk factors and the interaction of NT-pro BNP by presence of depressive symptoms. Patients with NT-pro BNP > 581 pg/ml and depressive symptoms exhibited a 5.5 times higher risk for cardiac events, when compared to patients with NT-pro BNP ≥ 581 pg/ml and no depressive symptoms (Figure 2).
Figure 2.
Adjusted cardiac event-free survival among groups stratified by NT-pro BNP and depressive symptoms (N = 210)
Survival curves were adjusted for age, gender, HF etiology, BMI, NYHA class, LVEF, total comorbidity score, and the interaction of NT-pro BNP by depressive symptoms.
DISCUSSION
This is the first study to demonstrate that the prognostic relationship of NT-pro BNP to cardiac event-free survival of patients with HF differed by the presence of depressive symptoms after controlling for age, gender, etiology of HF, BMI, NYHA functional class, LVEF, total comorbidity score, and the interaction between level of NT-pro BNP and the presence of depressive symptoms. The most compelling finding of this study was the relationship of NT-pro BNP and cardiac event-free survival among patients stratified by depressive symptoms. The coexistence of elevated NT-pro BNP and depressive symptoms predicted the shortest cardiac event-free survival in patients with HF. Of particular note, survival rates of patients with high levels of NT-pro BNP in the absence of depressive symptoms were not significantly different from those with low levels of NT-pro BNP. Thus, higher NT-pro-BNP confers greater risk of cardiac events among those with depressive symptoms than those without depressive symptoms.
Only one prior study demonstrated a similar relationship between BNP, depressive symptoms and cardiac events among hospitalized patients with HF.34 Parissis and colleagues34 reported the presence of a relationship between BNP and depressive symptoms to cardiac events within 6-month of hospital discharge without adjustments for other risk factors. Our study extended this finding to demonstrate that NT-pro BNP was the more significant predictor for cardiac event-free survival when coupled with the presence of depressive symptoms. Our finding suggests possible biobehavioral mechanisms through which depressive symptoms hasten the progression of HF via elevated sympathetic hyperactivity, increased inflammatory cytokines, and non-adherence to self-management. Our finding also strongly suggests that consideration be given to the prognostic value of NT-pro BNP in patients with depressive symptoms, as coupling of depressive symptoms and elevated concentrations of NT-pro BNP appears to provide powerful prognostic value.
Consistent with the previous studies,8, 16, 17, 35 NT-pro BNP was found to be an independent predictor of cardiac event-free survival after adjusting for traditional risk factors in patients with HF. Previous investigators8, 16, 17 have demonstrated that high levels of NT-pro BNP are positively associated with increased risk for cardiac events, only in patients with impaired left ventricular systolic function who have ischemic heart disease as an underlying etiology of HF. We recruited patients with both impaired and preserved left ventricular systolic function. Additionally, left ventricular ejection fraction was controlled in Cox hazard regression. Thus, our study extends these findings to demonstrate that NT-pro BNP has prognostic value among patients with preserved left ventricular function,8, 16, 35 but that the prognostic value is modified by presence of depressive symptoms.
Twenty seven percent of patients in this study had depressive symptoms. This finding is similar to previous studies,11, 12 in which depressive symptoms were measured with the PHQ-9 among patients with HF. It has been demonstrated that the presence of depressive symptoms based on self-rated questionnaires may over-estimate the prevalence of depression when compared to clinical depression. Depressive symptoms differ from a diagnosis of clinical depression which is defined as a major depressive disorder in the Diagnostic and Statistical Manual of Mental Disorders, Forth Edition (DSM-IV-TR).36 Major depressive disorders referred to as clinical depression is diagnosed if 5 or more of 9 depressive symptom criteria such as depressed mood, loss of interest, fatigue, and decreased ability to concentration have been present at least most of day in the past 2 weeks, and 1 of symptoms should be depressed mood or loss of pleasure.36 However, the presence of depressive symptoms measured by the PHQ-9 had comparative validity with the Structured Clinical Interview for International Classification of Diseases 10 (ICD-10) or DSM-IV as reference standards.37, 38 Furthermore, the PHQ-9 has been recommended as a screening tool for depressive symptoms especially in patients with heart disease.39 Therefore, the PHQ-9 could be helpful to assess depressive symptoms easily in clinical area.
Consistent with other studies,10 patients with depressive symptoms experienced shorter earlier cardiac event-free survival, even after controlling for other traditional risk factors. Moreover, depressive symptoms were an independent predictor of shorter cardiac event-free survival among patients with HF in this study. This finding suggests that depressive symptoms should be considered a predictor of HF prognosis as well as NT-pro BNP concentration. It is recommended that close monitoring for depressive symptoms should be emphasized in primary care. One in four patients was taking antidepressants but their depressive symptoms in the PHQ-9 score were still higher than patients with depressive symptoms who were not prescribed antidepressants in our study. This result indicates that depressive symptoms of some patients were not adequately treated. Therefore, non-pharmacological interventions identified to be effective to decrease depressive symptoms such as cognitive behavioral therapies and exercise programs could prevent early cardiac events in patients with HF.
Several limitations in this study should be noted. High NT-pro BNP levels have been associated with renal dysfunction while lower levels are found in overweight or obese patients with HF. BMI and renal dysfunction were controlled in Cox proportional hazard regression. However, no objective measurement of renal function was included in this study. Another potential limitation of this study was measurement of depressive symptoms and NT-pro BNP one time only. This precluded the possibility of following changes or patterns in these variables over time. Longitudinal monitoring of depressive symptoms and NT-pro BNP may have produced different findings. Future research should consider repeated measurement to further clarify their respective roles in long-term outcomes. Stratifying the sample into four groups by NT-pro BNP and depressive symptoms limited the sample size in each group. Future studies using a larger sample may identify differences between groups with one of the risk factors (i.e. either depressive symptoms or NT-pro BNP) and a group with neither risk factor. In the interim, conclusions regarding no differences among these groups should be drawn with caution.
CONCLUSIONS
Coexistence of elevated NT-pro BNT and severe depressive symptoms predicted shorter cardiac event-free survival in patients with HF. NT-pro BNP was a non-significant predictor of cardiac event-free survival in the absence of depressive symptoms. Depressive symptoms were a strong predictor of cardiac event-free survival as well as more widely used biological marker such as NT-pro BNP. Monitoring and treatment of depressive symptoms are important for improving cardiac event-free survival in patients with HF. Further research is needed to address the standard prognostic value of NT-pro BNP in HF patients with and without depressive symptoms.
Acknowledgments
Funding: The project described was supported by grant number R01 NR008567, R01 NR 009280 from the National Institute of Nursing Research (NINR), by a Center grant, P20NR010679 from National Institutes of Health (NIH), NINR, by a grant from American Acute Critical Nurses Phillips Medical Research Award, and by grant number M01RP02602 from University of Kentucky General Clinical Research Center. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institute of Nursing Research or the National Institutes of Health
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Contributor Information
Eun Kyeung Song, Department of Nursing, University of Ulsan.
Debra K. Moser, University of Kentucky, College of Nursing.
Susan K. Frazier, University of Kentucky, College of Nursing.
Seongkum Heo, Indiana University School of Nursing.
Misook L Chung, University of Kentucky, College of Nursing.
Terry A. Lennie, University of Kentucky, College of Nursing.
References
- 1.Heart and stroke statistics-2008 update. 2008. [DOI] [PubMed]
- 2.Masoudi FA, Havranek EP, Krumholz HM. The burden of chronic congestive heart failure in older persons: magnitude and implications for policy and research. Heart Fail Rev. 2002 Jan;7(1):9–16. doi: 10.1023/a:1013793621248. [DOI] [PubMed] [Google Scholar]
- 3.Miller LW, Missov ED. Epidemiology of heart failure. Cardiology Clin. 2001 Nov;19(4):547–555. doi: 10.1016/s0733-8651(05)70242-3. [DOI] [PubMed] [Google Scholar]
- 4.Haldeman GA, Croft JB, Giles WH, Rashidee A. Hospitalization of patients with heart failure: National Hospital Discharge Survey, 1985 to 1995. Am Heart J. 1999 Feb;137(2):352–360. doi: 10.1053/hj.1999.v137.95495. [DOI] [PubMed] [Google Scholar]
- 5.Koelling TM, Chen RS, Lubwama RN, L’Italien GJ, Eagle KA. The expanding national burden of heart failure in the United States: the influence of heart failure in women. Am Heart J. 2004 Jan;147(1):74–78. doi: 10.1016/j.ahj.2003.07.021. [DOI] [PubMed] [Google Scholar]
- 6.Stewart S, MacIntyre K, Hole DJ, Capewell S, McMurray JJ. More ‘malignant’ than cancer? Five-year survival following a first admission for heart failure. Eur J Heart Fail. 2001 Jun;3(3):315–322. doi: 10.1016/s1388-9842(00)00141-0. [DOI] [PubMed] [Google Scholar]
- 7.Lainchbury JG, Campbell E, Frampton CM, Yandle TG, Nicholls MG, Richards AM. Brain natriuretic peptide and n-terminal brain natriuretic peptide in the diagnosis of heart failure in patients with acute shortness of breath. J Am Coll Cardiol. 2003 Aug 20;42(4):728–735. doi: 10.1016/s0735-1097(03)00787-3. [DOI] [PubMed] [Google Scholar]
- 8.Stanek B, Frey B, Hulsmann M, et al. Prognostic evaluation of neurohumoral plasma levels before and during beta-blocker therapy in advanced left ventricular dysfunction. J Am Coll Cardiol. 2001 Aug;38(2):436–442. doi: 10.1016/s0735-1097(01)01383-3. [DOI] [PubMed] [Google Scholar]
- 9.Weber T, Auer J, Eber B. The diagnostic and prognostic value of brain natriuretic peptide and aminoterminal (nt)-pro brain natriuretic peptide. Curr Pharm Des. 2005;11(4):511–525. doi: 10.2174/1381612053382034. [DOI] [PubMed] [Google Scholar]
- 10.Rutledge T, Reis VA, Linke SE, Greenberg BH, Mills PJ. Depression in heart failure a meta-analytic review of prevalence, intervention effects, and associations with clinical outcomes. J Am Coll of Cardiol. 2006 Oct 17;48(8):1527–1537. doi: 10.1016/j.jacc.2006.06.055. [DOI] [PubMed] [Google Scholar]
- 11.Faller H, Stork S, Schowalter M, et al. Depression and survival in chronic heart failure: does gender play a role? Eur J Heart Fail. 2007 Oct;9(10):1018–1023. doi: 10.1016/j.ejheart.2007.06.011. [DOI] [PubMed] [Google Scholar]
- 12.Muller-Tasch T, Peters-Klimm F, Schellberg D, et al. Depression is a major determinant of quality of life in patients with chronic systolic heart failure in general practice. J Card Fail. 2007 Dec;13(10):818–824. doi: 10.1016/j.cardfail.2007.07.008. [DOI] [PubMed] [Google Scholar]
- 13.Judd LL, Akiskal HS, Zeller PJ, et al. Psychosocial disability during the long-term course of unipolar major depressive disorder. Arch Gen Psychiatry. 2000 Apr;57(4):375–380. doi: 10.1001/archpsyc.57.4.375. [DOI] [PubMed] [Google Scholar]
- 14.Blankenberg S, McQueen MJ, Smieja M, et al. Comparative impact of multiple biomarkers and N-Terminal pro-brain natriuretic peptide in the context of conventional risk factors for the prediction of recurrent cardiovascular events in the Heart Outcomes Prevention Evaluation (HOPE) Study. Circulation. 2006 Jul 18;114(3):201–208. doi: 10.1161/CIRCULATIONAHA.105.590927. [DOI] [PubMed] [Google Scholar]
- 15.Bibbins-Domingo K, Gupta R, Na B, Wu AH, Schiller NB, Whooley MA. N-terminal fragment of the prohormone brain-type natriuretic peptide (NT-proBNP), cardiovascular events, and mortality in patients with stable coronary heart disease. JAMA. 2007 Jan 10;297(2):169–176. doi: 10.1001/jama.297.2.169. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Fisher C, Berry C, Blue L, Morton JJ, McMurray J. N-terminal pro B type natriuretic peptide, but not the new putative cardiac hormone relaxin, predicts prognosis in patients with chronic heart failure. Heart (British Cardiac Society) 2003 Aug;89(8):879–881. doi: 10.1136/heart.89.8.879. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Richards AM, Doughty R, Nicholls MG, et al. Plasma N-terminal pro-brain natriuretic peptide and adrenomedullin: prognostic utility and prediction of benefit from carvedilol in chronic ischemic left ventricular dysfunction. Australia-New Zealand Heart Failure Group. J Am Coll Cardiol. 2001 Jun 1;37(7):1781–1787. doi: 10.1016/s0735-1097(01)01269-4. [DOI] [PubMed] [Google Scholar]
- 18.Pfister R, Schneider CA. Natriuretic peptides BNP and NT-pro-BNP: established laboratory markers in clinical practice or just perspectives? Clinica Chimica Acta; International Journal of Clinical Chemistry. 2004 Nov;349(1-2):25–38. doi: 10.1016/j.cccn.2004.06.018. [DOI] [PubMed] [Google Scholar]
- 19.Kazanegra R, Cheng V, Garcia A, et al. A rapid test for B-type natriuretic peptide correlates with falling wedge pressures in patients treated for decompensated heart failure: a pilot study. J Card Fail. 2001 Mar;7(1):21–29. doi: 10.1054/jcaf.2001.23355. [DOI] [PubMed] [Google Scholar]
- 20.ProBrian natriuretic peptide package insert. Roche diagnostics; Indianapolis: 2002. [Google Scholar]
- 21.Hunt PJ, Espiner EA, Nicholls MG, Richards AM, Yandle TG. The role of the circulation in processing pro-brain natriuretic peptide (proBNP) to amino-terminal BNP and BNP-32. Peptides. 1997;18(10):1475–1481. doi: 10.1016/s0196-9781(97)00245-3. [DOI] [PubMed] [Google Scholar]
- 22.McCullough PA, Sandberg KR. Sorting out the evidence on natriuretic peptides. Rev Cardiovasc Med. 2003;4(Suppl 4):S13–19. [PubMed] [Google Scholar]
- 23.Yan RT, White M, Yan AT, et al. Usefulness of temporal changes in neurohormones as markers of ventricular remodeling and prognosis in patients with left ventricular systolic dysfunction and heart failure receiving either candesartan or enalapril or both. Am J Cardiol. 2005 Sep 1;96(5):698–704. doi: 10.1016/j.amjcard.2005.04.048. [DOI] [PubMed] [Google Scholar]
- 24.Richards M, Nicholls MG, Espiner EA, et al. Comparison of B-type natriuretic peptides for assessment of cardiac function and prognosis in stable ischemic heart disease. J Am Coll Cardiol. 2006 Jan 3;47(1):52–60. doi: 10.1016/j.jacc.2005.06.085. [DOI] [PubMed] [Google Scholar]
- 25.Kroenke K, Spitzer RL, Williams JB. The PHQ-9: validity of a brief depression severity measure. J Gen Intern Med. 2001 Sep;16(9):606–613. doi: 10.1046/j.1525-1497.2001.016009606.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Spitzer RL, Kroenke K, Williams JB. Validation and utility of a self-report version of PRIME-MD: the PHQ primary care study. Primary Care Evaluation of Mental Disorders. Patient Health Questionnaire. JAMA. 1999 Nov 10;282(18):1737–1744. doi: 10.1001/jama.282.18.1737. [DOI] [PubMed] [Google Scholar]
- 27.Aboufakher R, Riba A, Jani SM, et al. Incidence, risk factors, and prognosis of inhospital heart failure after percutaneous coronary intervention: insight from the Blue Cross Blue Shield of Michigan Cardiovascular Consortium (BMC2) Am Heart J. 2005 Sep;150(3):455–458. doi: 10.1016/j.ahj.2004.12.011. [DOI] [PubMed] [Google Scholar]
- 28.Curtis JP, Selter JG, Wang Y, et al. The obesity paradox: body mass index and outcomes in patients with heart failure. Arch Intern Med. 2005 Jan 10;165(1):55–61. doi: 10.1001/archinte.165.1.55. [DOI] [PubMed] [Google Scholar]
- 29.Elhendy A, Sozzi F, van Domburg RT, et al. Effect of myocardial ischemia during dobutamine stress echocardiography on cardiac mortality in patients with heart failure secondary to ischemic cardiomyopathy. Am J Cardiol. 2005;96:469–473. doi: 10.1016/j.amjcard.2005.04.004. [DOI] [PubMed] [Google Scholar]
- 30.Fonarow GC, Srikanthan P, Costanzo MR, Cintron GB, Lopatin M. An obesity paradox in acute heart failure: analysis of body mass index and inhospital mortality for 108,927 patients in the Acute Decompensated Heart Failure National Registry. Am Heart J. 2007 Jan;153(1):74–81. doi: 10.1016/j.ahj.2006.09.007. [DOI] [PubMed] [Google Scholar]
- 31.Hall JA, French TK, Rasmusson KD, et al. The paradox of obesity in patients with heart failure. J Am Acad Nurse Pract. 2005 Dec;17(12):542–546. doi: 10.1111/j.1745-7599.2005.00084.x. [DOI] [PubMed] [Google Scholar]
- 32.Orn S, Cleland JG, Romo M, Kjekshus J, Dickstein K. Recurrent infarction causes the most deaths following myocardial infarction with left ventricular dysfunction. Am J Med. 2005;118:752–758. doi: 10.1016/j.amjmed.2005.02.010. [DOI] [PubMed] [Google Scholar]
- 33.Mitchell H, Katz . Multivariable analysis: a practical guide for clinicians. 2nd ed Cambridge University; Cambridge: 2006. [Google Scholar]
- 34.Parissis JT, Nikolaou M, Farmakis D, et al. Clinical and prognostic implications of self-rating depression scales and plasma B-type natriuretic peptide in hospitalised patients with chronic heart failure. Heart (British Cardiac Society) 2008 May;94(5):585–589. doi: 10.1136/hrt.2007.117390. [DOI] [PubMed] [Google Scholar]
- 35.Gardner RS, Ozalp F, Murday AJ, Robb SD, McDonagh TA. N-terminal pro-brain natriuretic peptide. A new gold standard in predicting mortality in patients with advanced heart failure. Eur Heart J. 2003 Oct;24(19):1735–1743. doi: 10.1016/j.ehj.2003.07.005. [DOI] [PubMed] [Google Scholar]
- 36.Diagnostic and statistical manual of mental disorders (DSM-IV-TR) 4th ed American Psychiatric Association; Washinton, D. C.: 2000. [Google Scholar]
- 37.Lowe B, Grafe K, Zipfel S, Witte S, Loerch B, Herzog W. Diagnosing ICD-10 depressive episodes: superior criterion validity of the Patient Health Questionnaire. Psychother Psychosom. 2004 Nov-Dec;73(6):386–390. doi: 10.1159/000080393. [DOI] [PubMed] [Google Scholar]
- 38.Lowe B, Spitzer RL, Grafe K, et al. Comparative validity of three screening questionnaires for DSM-IV depressive disorders and physicians’ diagnoses. J Affect Disord. 2004 Feb;78(2):131–140. doi: 10.1016/s0165-0327(02)00237-9. [DOI] [PubMed] [Google Scholar]
- 39.McManus D, Pipkin SS, Whooley MA. Screening for depression in patients with coronary heart disease (data from the Heart and Soul Study. Am J Cardiol. 2005 Oct 15;96(8):1076–1081. doi: 10.1016/j.amjcard.2005.06.037. [DOI] [PMC free article] [PubMed] [Google Scholar]