Abstract
Objectives. We examined the extent of unmet needs and barriers to accessing health care among homeless people within a universal health insurance system.
Methods. We randomly selected a representative sample of 1169 homeless individuals at shelters and meal programs in Toronto, Ontario. We determined the prevalence of self-reported unmet needs for health care in the past 12 months and used regression analyses to identify factors associated with unmet needs.
Results. Unmet health care needs were reported by 17% of participants. Compared with Toronto's general population, unmet needs were significantly more common among homeless individuals, particularly among homeless women with dependent children. Factors independently associated with a greater likelihood of unmet needs were younger age, having been a victim of physical assault in the past 12 months, and lower mental and physical health scores on the 12-Item Short Form Health Survey.
Conclusions. Within a system of universal health insurance, homeless people still encounter barriers to obtaining health care. Strategies to reduce nonfinancial barriers faced by homeless women with children, younger adults, and recent victims of physical assault should be explored.
Homeless people are among the most marginalized groups in society, and large numbers of homeless individuals are found in the United States, Canada, and throughout the world.1,2 Although the majority of homeless people are men, women and parents with children represent substantial segments of the homeless population.3 Homeless people suffer from many serious threats to their health, including an increased risk of all-cause mortality.4 Common medical conditions in this population include epilepsy, chronic obstructive pulmonary disease, hypertension, diabetes, and musculoskeletal disorders.5 Substance abuse, mental illness, and related comorbidities are also highly prevalent.5
Despite high levels of morbidity and mortality, homeless people face numerous financial and nonfinancial barriers to obtaining needed health services.6,7 A 1996 nationwide survey of homeless people across the United States found that 57% were uninsured, and lack of health insurance was associated with significantly lower odds of using ambulatory health care.7 Nonfinancial barriers have also been described. Competing priorities such as securing adequate food and shelter may lead to delays in seeking health care.8 Lack of transportation to health visits, long waiting times in clinics, and feelings of being stigmatized by health care professionals are also obstacles frequently reported by homeless people.6,9 Lack of appropriate health care for homeless people may contribute to deterioration in health status, prolonged homelessness, and even death.10,11
Most studies of unmet needs for care among homeless individuals have been conducted in the United States.6,7,12 Unmet needs for medical care in the past year were reported by 25% of respondents in a nationwide survey of homeless people in the United States and were somewhat more common among homeless families than among single homeless persons (27% vs 24%, respectively).7,13 Studies conducted in various US urban centers have found even higher rates of unmet needs for care. Among homeless people living in urban encampments in Los Angeles, California, 41% felt there was a time in the past 6 months when they had needed to go to a doctor but did not.12 A study of homeless women in Los Angeles County in 1997 found that 37% of participants had unmet needs for health care in the past 60 days.6 In a survey of low-income adults in Baltimore, Maryland, 57% of whom were homeless, 51% reported having difficulty accessing health care services.14 A recent study conducted in Birmingham, Alabama, found that the prevalence of unmet needs for care among homeless people rose from 32% in 1995 to 54% in 2005.15 This overall pattern suggests inadequacy of the US health care safety net for low-income and uninsured individuals.15
Canada has a publicly funded system of universal health insurance that consists of single-payer plans administered by each province. All medically necessary physician services and hospital-based care are fully covered with no copayments. However, the extent to which such a system meets the needs of severely disadvantaged individuals has not been well defined.16,17 Our objectives were to determine the prevalence of unmet needs for health care among homeless single men, single women, and women with dependent children within Canada's universal health insurance system and to identify individual characteristics associated with having unmet needs.
METHODS
Toronto is Canada's largest city, with a population of approximately 5 million. About 5000 individuals are homeless in Toronto each night, and about 29 000 different individuals use shelters each year.2,18 We recruited a representative sample of homeless persons, where homelessness was defined as living within the past 7 days at a shelter or hostel for the homeless, public place, vehicle, abandoned building, or someone else's place, and not having a place of one's own.13 Previous studies by Koegel et al. have demonstrated that samples of homeless persons selected from shelters and meal programs via these methods provide good approximations of the total homeless population.19 Based on a pilot study, we determined that approximately 90% of homeless individuals who used shelter or meal program services in Toronto had slept at a shelter in the past month, whereas 10% had not slept at a shelter but had eaten at a meal program.20 We therefore recruited 90% of our study participants at shelters and 10% at meal programs.
We contacted every homeless shelter in Toronto and obtained permission to enroll participants at 58 (91%) of the 64 shelters. Of these 58 shelters, 20 were for single men (i.e., men not accompanied by dependent children), 12 were for single women (i.e., women not accompanied by dependent children), 6 were for single men and women, 12 were for youths aged 16 to 25 years, and 8 were for families (i.e., adults with dependent children). The number of beds at each shelter ranged from 20 to 406. Recruitment at meal programs took place at 18 sites selected at random from 62 meal programs in Toronto that served homeless people. Because the goal of recruiting at meal programs was to enroll homeless people who did not use shelters, we excluded individuals at meal programs who had used a shelter within the past 7 days.
Recruitment took place over 12 consecutive months in 2005. Enrollment was stratified to recruit a sample that was approximately 50% single men, 25% single women, and 25% adults with dependent children. These groups represented 68%, 24%, and 8% of all shelter users in Toronto in 2005, respectively. Adults with dependent children were oversampled to permit separate analyses for this subgroup. The number of participants recruited at each site was proportionate to the number of homeless individuals served monthly. Individuals were selected from bed lists or meal lines by using a random number generator and then they were screened for eligibility. All participants gave written informed consent to participate in the study and received $15 for completing the survey. This study was approved by the St Michael's Hospital Research Ethics Board.
Participants
Of 2516 individuals screened, 882 (35%) were ineligible: 229 (9%) did not meet our definition of homelessness, 104 (4%) were unable to communicate in English, 54 (2%) were homeless individuals at meal programs who had used a shelter within the past 7 days, and 53 (2%) were unable to give informed consent. Because this study was part of a larger study of homeless people's health care utilization, an additional 442 individuals (18%) were excluded because they had never had an Ontario health insurance number, which is necessary for tracking of health care use with electronic databases. Most of these 442 individuals were refugees, refugee claimants, or recent migrants to Ontario. Our study did, however, include 315 participants who had an Ontario health insurance number but who were not in possession of their health insurance card, which serves as proof of insurance and which almost all health care providers require to be presented at each visit. The most common reasons for not possessing a health card were that it had been lost or stolen.
Of 1634 eligible individuals, 443 declined to participate and 1191 (73% of those eligible) were enrolled in the study. For this report, 19 homeless families without adult female members and 3 participants who did not provide information on unmet needs for care were excluded. Thus, data were analyzed for a total of 1169 single men, single women, and women with dependent children.
Survey
Information was obtained on demographic characteristics and health conditions by self report. Race was self-identified, with participants selecting from categories adapted from the Statistics Canada Ethnic Diversity Survey.21 The most commonly selected categories were White, Black, and Aboriginal; all other categories were grouped together as “other.” Unmet needs for health care were considered present among participants who answered affirmatively to: “Have you needed to see a doctor/nurse in the past 12 months but were not able?” We calculated a weighted estimate of the prevalence of unmet needs among all shelter users in Toronto in 2005. All participants were also asked if there was any time in the past 12 months when they or their doctor thought they needed to see a specialist, but they were not able to.
We used the Behavioral Model for Vulnerable Populations, which has been frequently applied to homeless individuals, to guide the selection of candidate predictors of unmet health care needs.22 This model of access to health care explains health behavior in terms of predisposing factors (e.g., demographic characteristics, health beliefs), enabling factors (e.g., personal, family, and community resources), and need factors (e.g., perceived health status, evaluated health status).
The predisposing factors considered were demographic group (single men, single women, women with dependent children); age; lifetime years of homelessness; race; place of birth; education; being a victim of physical assault in the past 12 months; being a victim of sexual assault in the past 12 months; drug, alcohol, and mental health problems in the past 30 days; and propensity to underseek care. The symptom threshold at which individuals seek medical attention may affect their likelihood of reporting unmet health care needs. The Propensity to Underseek Care scale is an instrument developed to measure health care–seeking behavior among individuals in low-income communities in the United States.23 Participants are asked if it would be extremely important, somewhat important, a little important, or not at all important for them to seek care if they had each of 5 specific symptoms: weight loss of more than 10 pounds in a month when not dieting; shortness of breath with light exercise or light work; chest pain when exercising; loss of consciousness, fainting, or passing out; and bleeding other than nosebleeds and not caused by accident or injury. Scores range from 0 to 5, with 1 point assigned for each symptom that the respondent rates as “a little important” or “not at all important.” A higher score represents more underseeking of care.
We assessed mental health problems, alcohol problems, and drug problems in the past 30 days with the Addiction Severity Index (ASI), an instrument that has been validated and used extensively in studies of homeless individuals.24 We dichotomized problems as being present or absent with cut-off scores established for homeless populations.13 These criteria included the classification of participants as having a mental health problem if their ASI mental health score was 0.25 or greater, an alcohol problem if their ASI alcohol score was 0.17 or greater, and a drug problem if their ASI drug score was 0.10 or greater.13
We also examined enabling factors, including monthly income, having a primary care provider, being accompanied to health visits, and having competing priorities, or the concept that difficulty meeting basic survival needs may be a barrier to obtaining health care.8 The competing priorities score is a previously validated 5-item measure of frequency of difficulty in meeting the following needs over the past 30 days: shelter, food, clothing, a place to wash, and access to a bathroom.8 Possible responses to each item are never, rarely, sometimes, or usually. Individuals were classified as having competing priorities if they responded “usually” to any of the 5 items.
Need factors evaluated were physical and mental health status scores on the 12-Item Short Form Health Survey (SF-12) and number of chronic health problems. The SF-12 is a widely used general health status instrument that has been validated in homeless populations.25 The SF-12 generates an overall measure of physical health status (physical component subscale) and mental health status (mental component subscale) with higher scores indicating better health. These scores range from 13 to 69 for physical health and 10 to 70 for mental health, standardized to a mean of 50 and standard deviation of 10 in the US general population.
Data on unmet needs for health care and lack of a primary care provider in the general population of Toronto were obtained from the Canadian Community Health Survey, cycle 3.1.26 This nationwide survey was conducted in 2005 by Statistics Canada by using in-person and telephone interviews. Data were available for 1883 adults living in Toronto. Unmet needs for health care were determined with the question, “During the past 12 months, was there ever a time when you felt that you needed health care but you didn't receive it?” Prevalence of unmet needs was calculated by age group and household type (men living alone, women living alone, and women living with dependent children).
Statistical Analyses
We used age-adjusted standardized morbidity ratios (SMRs) to compare the observed rate of unmet needs for health care among homeless individuals to the expected rate based on general population data. An SMR greater than 100 indicated that the observed rate was higher than expected, after adjustment for age. Confidence intervals (CIs) that excluded 100 were statistically significant at P < .05. Separate analyses were performed for single men, single women, and women with dependent children. We used Open Source Epidemiologic Statistics for Public Health, version 2.2.1, available at http://www.OpenEpi.com (Emory University Rollins School of Public Health, Atlanta, GA) to calculate SMRs and 95% CIs.
We performed univariate and multivariate regression analyses to identify factors associated with increased odds of unmet health care needs. All factors considered to be plausibly associated with risk of unmet needs were included in the multivariate model. Our a priori hypothesis was that demographic group would be significantly associated with unmet needs; analyses of other variables were exploratory in nature.
Tests of multicollinearity showed that no tolerance values were less than 0.40, and, therefore, multicollinearity was not a concern. We performed data analyses by using SPSS 16.0 for Windows software (SPSS Inc, Chicago, IL) and SAS version 9.2 software (SAS Institute, Cary, NC).
RESULTS
Characteristics of the 1169 study participants are shown in Table 1. On average, participants reported a lifetime duration of homelessness of 3.7 years (SD = 5.5 years). Substance use and mental health problems were common among our sample, with 41% of participants reporting drug problems, 30% reporting alcohol problems, and 38% reporting mental health problems in the past 30 days. Assaults were also common among our sample, especially among participants with unmet needs; 29% of participants reported that they were the victim of a physical assault and 5% reported they were the victim of a sexual assault in the past 12 months. Participants reported low scores for the SF-12 mental (mean = 40.6; SD = 13.3) and physical (mean = 46.0; SD = 11.1) component subscales relative to the standardized mean of 50 (SD = 10) for the US general population. Only 5% of participants experienced competing priorities, defined as difficulty obtaining shelter, food, clothing, a place to wash, and access to a bathroom in the past 30 days, and more than one third of participants had a primary care provider.
TABLE 1.
Characteristics of Homeless Individuals Who Used Shelter or Meal Programs: Toronto, Ontario, 2005
| All Participants (n = 1169) | Participants With Unmet Needs (n = 196), No. (%) | Participants Without Unmet Needs (n = 973), No. (%) | P | |
| Predisposing variables | ||||
| Demographic group, no. (%) | .004 | |||
| Single men | 602 (51) | 83 (42) | 519 (53) | |
| Single women | 303 (26) | 68 (35) | 235 (24) | |
| Women with dependent children | 264 (23) | 45 (23) | 219 (23) | |
| Age, y, mean (SD) | 36.1 (12.4) | 35.3 (11.7) | 36.3 (12.6) | .34 |
| Lifetime years of homelessness, mean (SD) | 3.7 (5.5) | 4.5 (6.9) | 3.5 (5.1) | .03 |
| Race, no. (%) | .71 | |||
| White | 646 (55) | 103 (53) | 543 (56) | |
| Black | 261 (22) | 43 (22) | 218 (22) | |
| Aboriginal | 102 (9) | 20 (10) | 82 (8) | |
| Other race | 160 (14) | 30 (15) | 130 (13) | |
| Place of birth, no. (%) | .85 | |||
| Canada | 800 (68) | 63 (32) | 667 (69) | |
| Outside Canada | 369 (32) | 133 (68) | 306 (31) | |
| Education, no. (%) | .27 | |||
| Some high school or less | 585 (50) | 99 (51) | 486 (50) | |
| High school diploma or equivalent | 252 (22) | 34 (18) | 218 (22) | |
| College/vocational training or more | 330 (28) | 61 (31) | 269 (28) | |
| Victim of physical assault (in past 12 mo), no. (%) | 340 (29) | 85 (44) | 255 (26) | <.001 |
| Victim of sexual assault (in past 12 mo), no. (%) | 63 (5) | 23 (12) | 40 (4) | <.001 |
| Drug problems (in past 30 d), no. (%) | 474 (41) | 85 (43) | 389 (40) | .38 |
| Alcohol problems (in past 30 d), no. (%) | 345 (30) | 63 (32) | 282 (29) | .38 |
| Mental health problems (in past 30 d), no. (%) | 444 (38) | 105 (54) | 339 (35) | <.001 |
| Propensity to underseek care score,a mean (SD) | 0.8 (1.2) | 1.0 (1.3) | 0.8 (1.2) | .059 |
| Enabling variables | ||||
| Health card in possession during the interview, no. (%) | .27 | |||
| Yes | 808 (69) | 129 (66) | 679 (70) | |
| No | 361 (31) | 67 (34) | 294 (30) | |
| Monthly income,b no. (%) | .75 | |||
| < $500 | 563 (48) | 89 (47) | 474 (50) | |
| $500 to $999 | 315 (27) | 55 (29) | 260 (27) | |
| ≥ $1000 | 264 (23) | 46 (24) | 217 (23) | |
| Has a primary care provider, no. (%) | 798 (68) | 128 (65) | 670 (69) | .33 |
| Accompanied to health visits,c no. (%) | 164 (14) | 40 (20) | 124 (13) | .005 |
| Competing priorities, no. (%) | 60 (5) | 17 (9) | 43 (4) | .013 |
| Need variables | ||||
| SF-12 mental component subscale score,d mean (SD) | 40.6 (13.3) | 35.8 (12.7) | 41.6 (13.2) | <.001 |
| SF-12 physical component subscale score,d mean (SD) | 46.0 (11.1) | 41.0 (11.0) | 47.0 (10.9) | <.001 |
| Number of chronic health conditions,e no. (%) | <.001 | |||
| 0 | 464 (40) | 49 (25) | 415 (43) | |
| 1 | 335 (29) | 60 (31) | 275 (28) | |
| 2 | 199 (17) | 39 (20) | 160 (16) | |
| ≥ 3 | 171 (15) | 48 (25) | 123 (13) | |
Note. SF-12 = 12-Item Short-Form Health Survey.
On a scale of 0 (least underseeking) to 5 (most underseeking).
Incomes are given in Canadian dollars.
Defined as usually being accompanied to health care visits by a service provider, friend, or family member (other than dependent child).
On a scale where 50 is the mean and 10 is the standard deviation in the US general population.
Chronic health conditions include diabetes; anemia; hypertension; heart disease and stroke; liver problems (including chronic viral hepatitis); arthritis, rheumatism, or joint problems; cancer; physical handicaps; or HIV/AIDS.
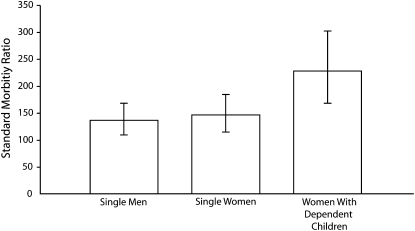
A total of 196 participants (17%) reported unmet needs for health care in the past 12 months. The weighted estimate of the prevalence of unmet needs among all shelter users in Toronto was 16%. Single women reported the highest rate of unmet needs (22%), followed by women with dependent children (17%), and single men (14%). Unmet needs for health care were significantly more common among homeless individuals in all 3 demographic groups, with age-adjusted SMRs of 146 (95% CI = 114, 184) for homeless single women, 227 (95% CI = 168, 301) for homeless women with dependent children, and 136 (95% CI = 109, 168) for homeless single men; (Figure 1). Only 53 (27%) of 196 individuals who reported unmet needs for care stated that they or their doctor thought they needed to see a specialist in the past 12 months but that they were not able to see one.
FIGURE 1.
Standardized morbidity ratios (SMRs) for unmet needs for health care among homeless individuals compared with the general population of Toronto by demographic group: Toronto, Ontario, 2005.
Note. Error bars represent the 95% confidence interval (CI) for the SMR. All 95% CIs exclude 100, indicating that unmet needs are significantly higher among homeless individuals compared with their counterparts in the general population.
As shown in Table 2, 10 characteristics were significantly associated with unmet need for health care in univariate analyses. Four factors were significantly associated with an increased likelihood of unmet needs for health care in the multivariate model: younger age (adjusted odds ratio [AOR] = 0.82; 95% CI = 0.68, 0.98), having been a victim of physical assault in the past 12 months (AOR = 1.57; 95% CI = 1.08, 2.28), having a poorer SF-12 mental health score (AOR = 0.78; 95% CI = 0.66, 0.91), and having a poorer SF-12 physical health score (AOR = 0.67; 95% CI = 0.56, 0.80; Table 2). The following characteristics were associated with a trend toward unmet needs for care, but did not reach statistical significance at the P < .05 level: single women demographic group compared with single men reference group (AOR = 1.52; 95% CI = 0.98, 2.35), longer lifetime duration of homelessness (AOR = 1.35; 95% CI = 0.98, 1.86), not having a primary care provider (AOR = 0.70; 95% CI = 0.48, 1.02), and higher propensity to underseek health care (AOR = 1.14; 95% CI = 0.99, 1.31).
TABLE 2.
Factors Associated With Unmet Needs for Health Care Among Homeless Individuals Who Used Shelter and Meal Programs in Toronto, Ontario, 2005
| Univariate Models |
Multivariate Model |
|||
| OR (95% CI) | P | AOR (95% CI) | P | |
| Predisposing variables | ||||
| Demographic group | ||||
| Single men (Ref) | 1.00 | 1.00 | ||
| Single women | 1.81 (1.27, 2.58) | .001 | 1.52 (0.98, 2.35) | .06 |
| Women with dependent children | 1.29 (0.87, 1.91) | .21 | 1.10 (0.65, 1.87) | .73 |
| Age (per 10 y increase) | 0.94 (0.84, 1.06) | .34 | 0.82 (0.68, 0.98) | .03 |
| Lifetime years of homelessness (per 10 y increase) | 1.32 (1.02, 1.72) | .027 | 1.35 (0.98, 1.86) | .07 |
| Race | ||||
| White (Ref) | 1.00 | 1.00 | ||
| Black | 1.04 (0.71, 1.53) | .84 | 0.95 (0.53, 1.70) | .86 |
| Aboriginal | 1.29 (0.76, 2.19) | .36 | 0.88 (0.47, 1.64) | .69 |
| Other race | 1.22 (0.78, 1.91) | .39 | 0.91 (0.50, 1.65) | .75 |
| Place of birth | ||||
| Canada (Ref) | 1.00 | 1.00 | ||
| Outside Canada | 1.03 (0.74, 1.44) | .85 | 1.43 (0.86, 2.40) | .17 |
| Education | ||||
| Some high school or less (Ref) | 1.00 | 1.00 | ||
| High school diploma or equivalent | 0.77 (0.50, 1.17) | .21 | 0.79 (0.49, 1.28) | .34 |
| College/vocational training or more | 1.11 (0.78, 1.58) | .55 | 1.07 (0.70, 1.63) | .75 |
| Victim of physical assault (in past 12 mo) | ||||
| No (Ref) | 1.00 | 1.00 | ||
| Yes | 2.22 (1.61, 3.05) | <.001 | 1.57 (1.08, 2.28) | .02 |
| Victim of sexual assault (in past 12 mo) | ||||
| No (Ref) | 1.00 | 1.00 | ||
| Yes | 3.15 (1.84, 5.39) | <.001 | 1.31 (0.69, 2.51) | .41 |
| Drug problems (in past 30 d) | ||||
| Absent (Ref) | 1.00 | 1.00 | ||
| Present | 1.15 (0.84, 1.57) | .38 | 0.81 (0.54, 1.22) | .32 |
| Alcohol problems (in past 30 d) | ||||
| Absent (Ref) | 1.00 | 1.00 | ||
| Present | 1.16 (0.83, 1.62) | .38 | 1.03 (0.68, 1.56) | .89 |
| Mental health problems (in past 30 d) | ||||
| Absent (Ref) | 1.00 | 1.00 | ||
| Present | 2.15 (1.58, 2.93) | <.001 | 1.33 (0.92, 1.94) | .13 |
| Propensity to underseek care scorea (per 1-point increase) | 1.12 (1.00, 1.26) | .06 | 1.14 (0.99, 1.31) | .07 |
| Enabling variables | ||||
| Health card in possession during the interview | ||||
| Yes | 1.00 | 1.00 | ||
| No | 1.20 (0.87, 1.66) | .27 | 1.09 (0.74, 1.59) | .67 |
| Monthly incomeb | ||||
| < $500 (Ref) | 1.00 | 1.00 | ||
| $500 to $999 | 1.13 (0.78, 1.63) | .53 | 1.00 (0.66, 1.52) | .99 |
| ≥ $1000 | 1.13 (0.76, 1.67) | .54 | 1.23 (0.79, 1.91) | .36 |
| Primary care provider | ||||
| No (Ref) | 1.00 | 1.00 | ||
| Yes | 0.85 (0.62, 1.18) | .33 | 0.70 (0.48, 1.02) | .06 |
| Accompanied to health visitsc | ||||
| No (Ref) | 1.00 | 1.00 | ||
| Yes | 1.85 (1.28, 2.68) | <.001 | 1.30 (0.82, 2.07) | .26 |
| Competing priorities | ||||
| Absent (Ref) | 1.00 | 1.00 | ||
| Present | 2.07 (1.15, 3.70) | .015 | 1.04 (0.51, 2.10) | .92 |
| Need variables | ||||
| SF-12 physical component subscale scored (per 10-point increase) | 0.63 (0.54, 0.72) | <.001 | 0.67 (0.56, 0.80) | <.001 |
| SF-12 mental component subscale score (per 10-point increase)d | 0.71 (0.63, 0.80) | <.001 | 0.78 (0.66, 0.91) | .002 |
| Number of chronic health conditionse | ||||
| 0 (Ref) | 1.00 | 1.0 | ||
| 1 | 1.85 (1.23, 2.78) | .003 | 1.43 (0.90, 2.27) | .13 |
| 2 | 2.06 (1.31, 3.27) | .002 | 1.39 (0.81, 2.39) | .24 |
| ≥ 3 | 3.31 (2.12, 5.16) | <.001 | 1.56 (0.86, 2.84) | .15 |
Notes. AOR = adjusted odds ratio; CI = confidence interval; OR = odds ratio; SF-12 = 12-Item Short-Form Health Survey.
On a scale of 0 (least underseeking) to 5 (most underseeking).
Incomes are given in Canadian dollars.
Defined as usually being accompanied to health care visits by a family member (other than dependent child), friend, or service provider.
On a scale where 10 points equals 1 standard deviation in the US general population.
Chronic health conditions include diabetes; anemia; hypertension; heart disease and stroke; liver problems (including chronic viral hepatitis); arthritis, rheumatism, or joint problems; cancer; physical handicaps; or HIV/AIDS.
DISCUSSION
We found that 1 in 6 homeless individuals living in Toronto reported unmet needs for health care within the past year. The disparity in access to care between homeless individuals and the general population of Toronto (based on SMRs) was greatest among homeless women with dependent children, who reported inability to obtain needed health care at a rate more than double that expected. Contrary to our hypothesis, however, demographic group was not a significant predictor of unmet health care needs among homeless people in our multivariate model.
Two need factors (worse physical health status and worse mental health status) were associated with increased odds of unmet health care needs. This finding is not surprising, in part because individuals with poorer physical and mental health status have a greater need for care and therefore are at higher risk for having unmet needs. In addition, chronic mental and physical illnesses may contribute to the onset of homelessness, and at the same time increase the risk of having unmet medical needs. Mental illness, for example, can certainly adversely affect an individual's ability to retain stable housing and to seek health care.
Younger age was also associated with an increased likelihood of unmet needs for health care. This finding may be related to unmet needs reported by homeless adolescents in our study sample. In previous studies, homeless adolescents have often reported poor access to needed health care services.27 These adolescents frequently cite specific nonfinancial barriers to obtaining care such as fears of being negatively judged by health care professionals.27
Multivariate Analysis
In our multivariate analysis, being a victim of physical assault in the past year was strongly associated with increased odds of unmet health care needs. The higher rate of physical assault observed among single women and women with children suggests an important gender effect. Previous research with homeless individuals has demonstrated that victimization is related to increased health care needs, as well as poorer self-rated health.28,29 A study of homeless women in Los Angeles County reported increased likelihood of unmet needs for health care among those with a history of rape or physical assault in the past year in unadjusted but not in adjusted analyses.6 In our study, the association between physical assault and unmet health care needs persisted despite adjustment for both mental and physical health status, suggesting that this association is not simply a reflection of increased need for care. It is possible that the increased risk of unmet needs is related to persistent fear among individuals who are victims of a past or ongoing abusive relationship.
Certain characteristics were associated with a trend toward higher odds of unmet needs for care, although they did not meet standard criteria for statistical significance in the multivariate model. One such characteristic was lack of a primary care provider. The multivariate analysis suggested that participants with a primary care provider were less likely to have unmet health care needs (AOR = 0.70; 95% CI = 0.48, 1.02). Further, our study revealed that 32% of homeless individuals in Toronto did not have a primary care provider. In contrast, only 9% of Toronto residents aged 12 years or older did not have a regular medical doctor in 2007.26,30 The magnitude of this disparity indicates that universal health insurance does not obviate the need for programs to ensure that individuals who are homeless have access to a primary care provider.
Our study highlights 2 additional issues regarding the provision of health care for homeless people in a system of universal health insurance. We found that 18% of people approached during recruitment for our study had never had health insurance in Ontario, primarily because they were refugees, refugee claimants, or recent migrants to the province. In addition, 31% of study participants did not have a health insurance card in their possession, often because it had been lost or stolen. Thus, even within a system of universal health insurance, some homeless individuals may still lack insurance or proof of insurance coverage.
Limitations and Strengths
Several limitations of this study should be noted. Individual characteristics and unmet health care needs were determined on the basis of self-report. Although inherently subjective, self-reported unmet health care needs is a valuable indicator that has been used in numerous research studies.31 A second limitation of this study is that homeless individuals who use neither shelters nor meal programs were excluded from our study sample. Finally, our study's cross-sectional design limits our ability to assess the causal relationships between individual characteristics and unmet needs for health care.
This study has a number of strengths. A large sample of homeless individuals was enrolled from homeless shelters and meal programs in Canada's largest city. This study reported separately on unmet needs for health care for single women and women with dependent children, whereas previous studies on access to health care have not distinguished between these 2 groups.6 A high response rate was achieved, with 73% of eligible individuals successfully recruited. Our relatively large sample size permitted the examination of numerous candidate predictors of unmet need for care.
Conclusions
Our study demonstrates that despite a system of universal health insurance, health care access can remain a challenge for homeless people. After financial barriers to care have been stripped away, other barriers that increase the risk of unmet needs for health care become evident. Younger adults and recent victims of violence face important nonfinancial barriers that may include general mistrust of health care providers. Assault victims may fear that an assault will be reported when they are seeking treatment. Lack of access to a primary care provider may be another relevant factor. Possible strategies to reduce these barriers may include primary prevention of physical assault, an emphasis on the importance of nonstigmatizing attitudes toward homeless individuals among health care trainees and workers, and special programs to provide primary care for patients who are homeless. In conclusion, the provision of health insurance is necessary but not sufficient to ensure that homeless people receive needed health care.
Acknowledgments
This project was supported by operating grants from the Agency for Healthcare Research and Quality (1 R01 HS014129-01) and the Canadian Institutes of Health Research (MOP-62736), and by an Interdisciplinary Capacity Enhancement grant on Homelessness, Housing, and Health from the Canadian Institutes of Health Research (HOA-80066). The Centre for Research on Inner City Health and the Institute for Clinical Evaluative Sciences gratefully acknowledge the support of the Ontario Ministry of Health and Long-Term Care. D. A. Redelmeier was supported by the Canada Research Chair in Medical Decision Sciences.
The authors thank Marko Katic, Department of Research Design and Biostatistics, Sunnybrook Health Sciences Centre, for expert programming and analyses. The authors also thank the shelters and meal programs that allowed the recruitment of participants and the interviews to be conducted at their sites.
Note. The funders for this study did not play any role in the study design; in the collection, analysis, and interpretation of data; in the writing of the report; and in the decision to submit the article for publication. The views expressed in this publication are the views of the authors and do not necessarily reflect the views of the Ontario Ministry of Health and Long-Term Care or any of the other previously named organizations.
Human Participant Protection
This study was approved by the St Michael's Hospital Research Ethics Board, and informed consent was obtained from each study participant.
References
- 1.Homelessness Research Institute, National Alliance to End Homelessness. Homelessness Counts, January 2007. Washington, DC: Homelessness Research Institute; 2007. Available at: http://www.endhomelessness.org/content/general/detail/1440. Accessed April 18, 2010 [Google Scholar]
- 2.City of Toronto 2006 Street Needs Assessment: Results and Findings 2006. Available at: http://www.toronto.ca/housing/pdf/streetneedsassessment.pdf. Accessed September 7, 2008
- 3.Hunger and Homelessness Survey: A Status Report on Hunger and Homelessness in America's Cities, A 24-City Survey, December 2005 Washington, DC: US Conference of Mayors; 2005 [Google Scholar]
- 4.Cheung AM, Hwang SW. Risk of death among homeless women: a cohort study and review of the literature. CMAJ 2004;170(8):1243–1247 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Street Health. The Street Health Report 2007. Available at: http://www.streethealth.ca. Accessed August 28, 2008.
- 6.Lewis JH, Andersen RM, Gelberg L. Health care for homeless women: unmet needs and barriers to care. J Gen Intern Med 2003;18(11):921–928 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Kushel MB, Vittinghoff E, Haas JS. Factors associated with the health care utilization of homeless people. JAMA 2001;285(2):200–206 [DOI] [PubMed] [Google Scholar]
- 8.Gelberg L, Gallagher TC, Andersen RM, Koegel P. Competing priorities as a barrier to medical care among homeless adults in Los Angeles. Am J Public Health 1997;87(2):217–220 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Wen CK, Hudak PL, Hwang SW. Homeless people's perceptions of welcomeness and unwelcomeness in healthcare encounters. J Gen Intern Med 2007;22(7):1011–1017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Hwang SW, O'Connell JJ, Lebow JM, et al. Health care utilization among homeless adults prior to death. J Health Care Poor Underserved 2001;12(1):50–58 [DOI] [PubMed] [Google Scholar]
- 11.Hwang SW, Dunn JR. Homeless people. : Galea S, Vlahov D, Handbook of Urban Health: Populations, Methods, and Practice New York, NY: Kluwer/Plenum; 2005 [Google Scholar]
- 12.Cousineau MR. Health status of and access to health services by residents of urban encampments in Los Angeles. J Health Care Poor Underserved 1997;8(1):70–82 [DOI] [PubMed] [Google Scholar]
- 13.Homelessness: Programs and the People They Serve. Findings of the National Survey of Homeless Assistance Providers and Clients Washington, DC: Interagency Council on the Homeless; 1999 [Google Scholar]
- 14.O'Toole TP, Arbelaez J, Haggerty C; Baltimore Community Health Consortium. The urban safety net: can it keep people healthy and out of the hospital? J Urban Health 2004;81(2):179–190 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Kertesz SG, Hwang SW, Irwin J, Ritchey FJ, Lagory ME. Rising inability to obtain needed health care among homeless persons in Birmingham, Alabama (1995-2005). J Gen Intern Med 2009;24(7):841–847 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.James PD, Wilkins R, Detsky AS, Tugwell P, Manuel DG. Avoidable mortality by neighbourhood income in Canada: 25 years after the establishment of universal health insurance. J Epidemiol Community Health 2007;61(4):287–296 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Allin S. Does equity in healthcare use vary across Canadian provinces? Healthc Policy 2008;3(4):83–99 [PMC free article] [PubMed] [Google Scholar]
- 18.City of Toronto. The Toronto Report Card on Housing and Homelessness 2003. Available at: http://www.toronto.ca/homelessness/pdf/reportcard2003.pdf. Accessed September 23, 2008.
- 19.Koegel P, Burnam MA, Morton SC. Enumerating homeless people: alternative strategies and their consequences. Eval Rev 1996;20(4):378–403 [Google Scholar]
- 20.Hwang SW, Chiu S, Kiss A, et al. Use of meal programs and shelters by homeless people in Toronto. J Urban Health 2005;82(suppl 2):ii46 [Google Scholar]
- 21.Statistics Canada. Ethnic Diversity Survey, April 2002. Available at: http://www.statcan.gc.ca/cgi-bin/imdb/p2SV.pl?Function=getSurvey&SDDS=4508&lang=en&db=imdb&adm=8&dis=2. Accessed April 18, 2010.
- 22.Gelberg L, Andersen RM, Leake BD. The behavioral model for vulnerable populations: application to medical care use and outcomes for homeless people. Health Serv Res 2000;34(6):1273–1302 [PMC free article] [PubMed] [Google Scholar]
- 23.Bindman AB, Grumbach K, Osmond D, et al. Preventable hospitalizations and access to health care. JAMA 1995;274(4):305–311 [PubMed] [Google Scholar]
- 24.Joyner LM, Wright JD, Devine JA. Reliability and validity of the Addiction Severity Index among homeless substance misusers. Subst Use Misuse 1996;31(6):729–751 [DOI] [PubMed] [Google Scholar]
- 25.Larson CO. Use of the SF-12 instrument for measuring the health of homeless persons. Health Serv Res 2002;37(3):733–749 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Statistics Canada, Special Surveys Division. Canadian Community Health Survey Cycle 3.1. 2006. Available at: http://www.chass.utoronto.ca/datalib/codebooks/cstdli/cchs.htm. Accessed May 15, 2008
- 27.Barkin SL, Balkrishnan R, Manuel J, Andersen RM, Gelberg L. Health care utilization among homeless adolescents and young adults. J Adolesc Health 2003;32(4):253–256 [DOI] [PubMed] [Google Scholar]
- 28.Bassuk EL, Melnick S, Browne A. Responding to the needs of low-income and homeless women who are survivors of family violence. J Am Med Womens Assoc 1998;53(2):57–64 [PubMed] [Google Scholar]
- 29.Wenzel SL, Leake BD, Gelberg L. Health of homeless women with recent experience of rape. J Gen Intern Med 2000;15(4):265–268 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Statistics Canada Canadian Community Health Survey, 2007 Available at: http://www.statcan.ca/Daily/English/080618/d080618a.htm Accessed September 30, 2008.
- 31.Berk ML, Schur CL, Cantor JC. Ability to obtain health care: recent estimates from the Robert Wood Johnson Foundation National Access to Care Survey. Health Aff (Millwood) 1995;14(3):139–146 [DOI] [PubMed] [Google Scholar]