Abstract
Objectives. We assessed whether local health departments (LHDs) were conducting obesity prevention programs and diabetes screening programs, and we examined associations between LHD characteristics and whether they conducted these programs.
Methods. We used the 2005 National Profile of Local Health Departments to conduct a cross-sectional analysis of 2300 LHDs nationwide. We used multivariate logistic regressions to calculate odds ratios (ORs) and 95% confidence intervals (CIs).
Results. Approximately 56% of LHDs had obesity prevention programs, 51% had diabetes screening programs, and 34% had both. After controlling for other factors, we found that employing health educators was significantly associated with LHDs conducting obesity prevention programs (OR = 2.08; 95% CI = 1.54, 2.81) and diabetes screening programs (OR = 1.63; 95% CI = 1.23, 2.17). We also found that conducting chronic disease surveillance was significantly associated with LHDs conducting obesity prevention programs (OR = 1.66; 95% CI = 1.26, 2.20) and diabetes screening programs (OR = 2.44; 95% CI = 1.90, 3.15). LHDs with a higher burden of diabetes prevalence were more likely to conduct diabetes screening programs (OR = 1.20; 95% CI = 1.11, 1.31) but not obesity prevention programs.
Conclusions. The presence of obesity prevention and diabetes screening programs was significantly associated with LHD structural capacity and general performance. However, the effectiveness and cost-effectiveness of both types of programs remain unknown.
The prevalence of obesity among US adults doubled between 1980 and 2004, and the 2005–2006 National Health and Nutrition Examination Survey found that more than 72 million US adults were obese.1–3 Obesity contributes to many chronic conditions, including type 2 diabetes, hypertension, stroke, heart disease, certain cancers, and arthritis.1 Of these conditions, type 2 diabetes, the sixth-leading cause of death in the United States,4 may be most closely linked to obesity.5 The prevalence of diagnosed diabetes among Americans increased from 2.5% in 1980 to 5.5% in 2005.6 In 2007, approximately 17.9 million Americans had diagnosed diabetes, and approximately 5.7 million had undiagnosed diabetes.7
The public health system has traditionally focused on the prevention and control of infectious diseases. However, improved sanitation and hygiene and the wide adoption of antibiotic use and vaccination have made infectious diseases less common. Conversely, chronic diseases, such as heart disease, cancer, and diabetes, have become more prevalent.8,9 Chronic diseases now account for 7 of 10 US deaths.10 Thus, public health agencies, including local health departments (LHDs), may be expected to play an expanded role in chronic disease prevention and control, in addition to their traditional role in infectious disease prevention and their recently enhanced role in disaster and emergency response.11 For example, New York City has started a mandatory registry of glycosylated hemoglobin values.12
There is a need to better understand the public health system's responses to chronic diseases (e.g., obesity and diabetes). Although many studies have examined characteristics of LHDs and their public health practices,13–21 little is known about these departments' obesity and diabetes prevention activities.22 To fill this gap, we assessed whether LHDs in the United States were conducting obesity prevention programs and diabetes screening programs. We used a conceptual framework developed by an expert panel and the Public Health Practice Program Office of the Centers for Disease Control and Prevention23 to examine the characteristics of LHDs that conducted these programs and to discover associations between those characteristics and whether LHDs conducted the programs.
METHODS
We used data from the 2005 National Profile of Local Health Departments (NPLHD), which was collected by the National Association of County and City Health Officials and funded by the Centers for Disease Control and Prevention. In 2005, a core questionnaire was sent to all 2864 LHDs in the United States, including every state except Rhode Island (no LHD operates in Rhode Island). A total of 2300 LHDs responded (overall response rate 80%; individual states' response rates ranged from 40% to 100%). As a proxy for disease burden, we used estimates of county-level prevalence of diabetes among individuals aged 20 years or older.24
Conceptual Framework
Our conceptual framework for measuring performance of public health systems in the form of LHDs mirrors a framework that has been used previously.23,25 The framework, based on Donabedian's traditional model for quality,26 includes 5 key elements: mission, structural capacity, processes, outcomes, and macro context.23 Although an LHD's mission can be conceptualized in terms of its core functions of assessment, policy development, and assurance, these functions are difficult to quantify. The structural capacities and processes of LHDs are relatively easy to measure, however, and the relationships among the 5 key elements have been studied and previously discussed.25,27
Structural capacity includes such components as organizational, informational, physical, human, and fiscal resources. The processes of LHDs usually refer to the 10 essential public health services: monitor, diagnose and investigate, inform, mobilize, make policy, enforce, link to health care, assure, evaluate, and conduct research.23 The outcomes of LHDs refer to changes in health status in the community. Macro context refers to factors that are not part of LHDs' characteristics but that directly or indirectly affect the existence and functioning of LHDs. For example, increases in a population's demand and need for public health services that result from increasing disease burden and public concerns about obesity and diabetes may affect whether an LHD conducts obesity prevention and diabetes screening programs.
For our study, we tested the association between LHDs' structural capacity (jurisdiction, governance, financing, and workforce) and processes (surveillance activities and community health assessment and planning), on the one hand, and whether LHDs were conducting obesity prevention and diabetes screening programs on the other. We hypothesized that LHDs with greater structural capacity (e.g., more staff full-time equivalents, better skill mix of staff) and higher performance in general (e.g., conducting surveillance activities, having recently conducted community health assessment and planning) were more likely to respond to community needs and have specific public health intervention programs (model 1). We had no information on county-level obesity burden and thus could not explore the direct impact of obesity burden on the presence of relevant programs. Instead, we used diabetes prevalence as a proxy for obesity burden and added diabetes burden to model 1 (model 2).
Measurements
In the 2005 NPLHD, LHDs were asked if they had population-based primary prevention services for obesity and if they operated screening programs for diabetes. The questionnaire contained no standard of obesity prevention or diabetes screening programs, nor did it define the components required for prevention services to be considered population-based; hence, the questionnaire determined whether the respondents considered their LHD to have such a program. We classified an LHD as conducting obesity prevention or diabetes screening programs if the respondent indicated that the LHD directly performed or contracted for obesity prevention or diabetes screening activities (dependent variables). However, we were not able to assess other aspects of LHDs' public health interventions related to prevention and control of obesity and diabetes.
We assessed 6 types of LHD characteristics (within the categories of structural capacity and processes) as independent variables: jurisdiction, governance, financing, workforce, surveillance, and community health assessment and planning. Jurisdiction variables included: (1) degree of urbanization (i.e., urban, suburban, or rural), (2) population size (i.e., < 25 000, 25 000–49 999, 50 000–99 999, 100 000–499 999, ≥ 500 000), and (3) population race/ethnicity (i.e., proportions of population that were African American or Hispanic/Latino). NPLHD used the rural–urban commuting-areas method to categorize LHD jurisdictions by degree of urbanization.28 Governance was measured by the presence of a local board of health (yes or no). Financing variables included annual LHD per capita expenditure (2005 US dollars) and proportions of federal and state funding (there are many sources of funding besides federal and state governments). NPLHD included the total public health expenditure of each LHD for the most recent available year (2003, 2004, or 2005) and for the previous fiscal year if possible. Because both variables had a certain number of missing values, we used the Consumer Price Index to convert the expenditure into 2005 dollars, and we calculated the average expenditure for both years where possible.
Workforce variables included: (1) the characteristics of LHDs' top agency executives (i.e., being full-time [yes or no], tenure of office, having a medical or public health degree [e.g., MD, DDS, DVM, MPH, DrPH; yes or no]); (2) staff full-time equivalents per 1000 population; (3) employment of physicians or nurses (yes or no); (4) employment of health educators (yes or no); and (5) employment of nutritionists (yes or no). Surveillance activity variables included whether the LHD performed chronic disease surveillance (yes or no) or risk behavior surveillance (yes or no). Community health assessment and planning variables included: (1) whether the LHD had completed a community health assessment within the prior 3 years (yes or no); (2) whether the LHD had developed or participated in developing a health improvement plan for the community within the prior 3 years (yes or no); and (3) whether the LHD's participation in collaborations with other community agencies and organizations had changed over the prior 3 years (increased or not increased).
Statistical Analysis
We used Stata version 9 (StataCorp LP, College Station, TX) and SAS version 9.1 (SAS Institute Inc, Cary, NC) to perform data analyses. We used descriptive statistics, calculated nationwide and by state, to assess whether LHDs conducted obesity prevention programs and diabetes screening programs. We compared characteristics of LHDs with and without obesity prevention and diabetes screening programs, and we tested these differences using the χ2 or t test, as appropriate. Bivariate relations between the 2 dependent variables and independent variables were also evaluated. To perform multivariate comparisons, we derived separate logistic models for obesity prevention and diabetes screening programs. We report odds ratios (ORs) and 95% confidence intervals (CIs), marking ORs that were significantly different from 1.00 at P less than .05, .01, and .001, where applicable.
RESULTS
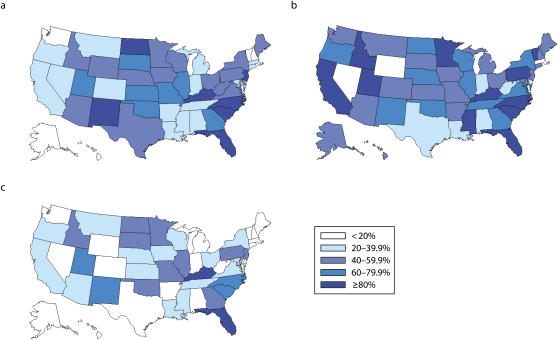
Figure 1 presents the proportion of local health departments with obesity prevention programs and diabetes screening programs, by state. Approximately 56% (n = 1287) of the responding LHDs had obesity prevention programs, approximately 51% (n = 1166) had diabetes screening programs, and 34% (n = 788) had both kinds of programs. Ninety percent of states had both programs in the state. Only Washington, DC, had neither program at all, and 4 states (Delaware, Hawaii, New Hampshire, and Vermont) had only 1 of the 2 types of programs. In some states, almost all the responding LHDs had either an obesity prevention, a diabetes screening program, or both. In a few states, most LHDs conducted neither program. In 6 states (Florida, Kentucky, North Carolina, New Mexico, South Carolina, and Utah), at least 60% of LHDs conducted both programs, and in 2 states (Florida and Kentucky), at least 80% of LHDs conducted both programs.
FIGURE 1.
Proportion of local health departments, by state, with (a) obesity prevention programs, (b) diabetes screening programs, and (c) both obesity prevention and diabetes screening programs: United States, National Profile of Local Health Departments, 2005.
LHDs with obesity prevention or diabetes screening programs were more likely than were LHDs without these programs to have certain characteristics (Table 1). Table 2 (model 1) reports associations between LHD characteristics and obesity prevention and diabetes screening programs, after other factors were controlled. We found that a 1% increase in the proportion of state funding for LHDs was associated with a 1% increase in the odds of LHDs having obesity prevention programs (OR = 1.01; 95% CI = 1.00, 1.02). LHDs with a full-time top agency executive (OR = 2.76; 95% CI = 1.71, 4.46) and an executive with a medical or public health degree (OR = 1.44; 95% CI = 1.06, 1.96) were more likely to have obesity prevention programs than were those without. A higher number of staff full-time equivalents per 1000 population (OR = 1.50; 95% CI = 1.14, 1.96) and employing health educators (OR = 2.08; 95% CI = 1.54, 2.81) were significantly associated with LHDs carrying out obesity prevention programs. LHDs conducting chronic disease surveillance (OR = 1.66; 95% CI = 1.26, 2.19), conducting risk behavior surveillance (OR = 2.91; 95% CI = 2.18, 3.87), recently having conducted community assessments (OR = 1.43; 95% CI = 1.07, 1.90), having recently conducted health improvement planning (OR = 1.70; 95% CI = 1.28, 2.26), and having recently increased external collaborations (OR = 1.78; 95% CI = 1.18, 2.67) were significantly associated with LHDs carrying out obesity prevention programs.
TABLE 1.
Characteristics of Local Health Departments, by Whether Departments Conduct Obesity Prevention and Diabetes Screening Programs: United States, National Profile of Local Health Departments, 2005
| Obesity Program |
Diabetes Program |
|||
| Characteristics | Yes | No | Yes | No |
| Degree of urbanization in jurisdiction, % | ||||
| Urban | 39.8 | 41.1 | 37.5* | 43.2 |
| Suburban | 19.4 | 20.3 | 18.8 | 21.1 |
| Rural | 40.8 | 38.7 | 43.7 | 35.8 |
| Population in jurisdiction, % | ||||
| < 25 000 | 33.6* | 49.4 | 40.6 | 40.8 |
| 25 000–49 999 | 21.7 | 21.1 | 21.8 | 21.0 |
| 50 000–99 999 | 16.3 | 13.3 | 14.9 | 15.2 |
| 100 000–499 999 | 20.6 | 13.6 | 16.1 | 18.6 |
| ≥ 500 000 | 7.8 | 2.7 | 6.6 | 4.5 |
| Race/ethnicity in jurisdiction, % | ||||
| African American | 9.2* | 6.8 | 9.4* | 6.8 |
| Hispanic or Latino | 6.4 | 6.1 | 6.2 | 6.3 |
| Having a local board of health, % | 74.8 | 73.9 | 78.3* | 70.2 |
| Financing | ||||
| Annual expenditure per capita, mean $ | 62.7* | 44.6 | 68.5* | 40.8 |
| Proportion of federal funding, % | 20.2* | 17.6 | 18.3* | 20.0 |
| Proportion of state funding, % | 24.1* | 16.4 | 21.6 | 20.2 |
| Workforce | ||||
| Full-time top agency executive, % | 93.3* | 76.8 | 89.5* | 82.9 |
| Tenure of top agency executive, mean y | 8.0 | 8.5 | 8.7* | 7.7 |
| Top agency executive with a medical or public health degree, % | 31.5* | 26.4 | 29.7 | 28.5 |
| Staff FTEs per 1000 population, mean | 0.8* | 0.5 | 0.8* | 0.5 |
| Employing physicians or nurses, % | 98.0* | 90.7 | 97.6* | 92.0 |
| Employing health educators, % | 67.0* | 37.5 | 60.7* | 48.9 |
| Employing nutritionists, % | 65.6* | 43.7 | 61.6* | 51.3 |
| Surveillance activities, % | ||||
| Chronic diseases | 55.1* | 24.6 | 54.4* | 28.5 |
| Risk behavior | 51.4* | 16.1 | 43.5* | 28.3 |
| Community health assessment and planning, % | ||||
| Health assessment | 63.4* | 36.0 | 55.8* | 46.9 |
| Health improvement plan | 65.1* | 38.3 | 58.0* | 48.8 |
| Collaboration increased | 91.6* | 82.5 | 90.0* | 85.1 |
Note. FTEs = full-time equivalents.
*P < .05, for difference between local health departments that have obesity prevention or diabetes screening programs and those that lack such programs (by to the χ2 or t test, as appropriate).
TABLE 2.
Factors Associated With Local Health Departments Conducting Obesity Prevention and Diabetes Screening Programs: United States, National Profile of Local Health Departments, 2005
| Obesity Program |
Diabetes Program |
|||
| Variables | Model 1, OR (95% CI) | Model 2, OR (95% CI) | Model 1, OR (95% CI) | Model 2, OR (95% CI) |
| Degree of urbanization in jurisdiction (vs urban) | ||||
| Suburban | 0.98 (0.66, 1.45) | 0.99 (0.66, 1.47) | 0.99 (0.70, 1.41) | 0.89 (0.62, 1.28) |
| Rural | 1.29 (0.87, 1.91) | 1.31 (0.87, 1.95) | 1.31 (0.92, 1.86) | 1.15 (0.80, 1.64) |
| Population size in jurisdiction (vs < 25 000) | ||||
| 25 000–49 999 | 1.19 (0.80, 1.75) | 1.18 (0.80, 1.75) | 0.93 (0.65, 1.31) | 0.95 (0.67, 1.35) |
| 50 000–99 999 | 1.14 (0.72, 1.82) | 1.14 (0.72, 1.81) | 0.73 (0.48, 1.10) | 0.75 (0.49, 1.14) |
| 100 000–499 999 | 1.13 (0.67, 1.89) | 1.12 (0.67, 1.88) | 0.52** (0.33, 0.83) | 0.55* (0.34, 0.87) |
| ≥ 500 000 | 1.87 (0.83, 4.20) | 1.85 (0.82, 4.16) | 0.91 (0.47, 1.77) | 1.02 (0.53, 1.99) |
| Race/ethnicity in jurisdiction | ||||
| African American | 1.00 (0.99, 1.01) | 1.00 (0.99, 1.01) | 1.01** (1.00, 1.02) | 1.00 (0.99, 1.01) |
| Hispanic or Latino | 0.99 (0.98, 1.00) | 0.99 (0.98, 1.00) | 1.01 (1.00, 1.02) | 1.01* (1.00, 1.02) |
| Having a local board of health (yes vs no) | 1.05 (0.76, 1.47) | 1.06 (0.76, 1.48) | 1.54** (1.15, 2.06) | 1.49** (1.11, 2.00) |
| Financing | ||||
| Expenditure per capita | 1.00 (1.00, 1.00) | 1.00 (1.00, 1.00) | 1.00 (1.00, 1.00) | 1.00 (1.00, 1.00) |
| Proportion of federal funding | 1.00 (0.99, 1.01) | 1.00 (0.99, 1.01) | 0.99** (0.98, 1.00) | 0.99** (0.98, 1.00) |
| Proportion of state funding | 1.01** (1.00, 1.02) | 1.01** (1.00, 1.02) | 1.00 (0.99, 1.01) | 1.00 (0.99, 1.00) |
| Workforce | ||||
| Full-time top agency executive (yes vs no) | 2.76*** (1.71, 4.46) | 2.74*** (1.69, 4.43) | 1.07 (0.71, 1.62) | 1.17 (0.77, 1.77) |
| Tenure of top agency executive | 1.00 (0.98, 1.01) | 1.00 (0.98, 1.01) | 1.01 (0.99, 1.02) | 1.01 (0.99, 1.02) |
| Top agency executive with a medical or public health degree (yes vs no) | 1.44* (1.06, 1.96) | 1.45* (1.07, 1.96) | 1.20 (0.92, 1.56) | 1.17 (0.90, 1.53) |
| Staff FTEs per 1000 population | 1.50** (1.14, 1.96) | 1.50** (1.14, 1.97) | 1.28* (1.01, 1.61) | 1.25 (0.99, 1.57) |
| Employing physicians or nurses (yes vs no) | 1.42 (0.72, 2.81) | 1.44 (0.72, 2.85) | 1.77 (0.97, 3.25) | 1.58 (0.86, 2.91) |
| Employing health educators (yes vs no) | 2.08*** (1.54, 2.81) | 2.08*** (1.54, 2.81) | 1.59** (1.20, 2.11) | 1.63** (1.23, 2.17) |
| Employing nutritionists (yes vs no) | 1.13 (0.84, 1.52) | 1.14 (0.84, 1.53) | 1.28 (0.98, 1.68) | 1.20 (0.91, 1.58) |
| Surveillance activities | ||||
| Conducting chronic disease surveillance (yes vs no) | 1.66*** (1.26, 2.19) | 1.66*** (1.26, 2.20) | 2.45*** (1.91, 3.15) | 2.44*** (1.90, 3.15) |
| Conducting behavior risk surveillance (yes vs no) | 2.91*** (2.18, 3.87) | 2.92*** (2.19, 3.89) | 0.99 (0.76, 1.27) | 0.96 (0.74, 1.24) |
| Community health assessment and planning | ||||
| Health assessment (yes vs no) | 1.43* (1.07, 1.90) | 1.42* (1.07, 1.90) | 1.05 (0.80, 1.37) | 1.07 (0.82, 1.41) |
| Health improvement plan (yes vs no) | 1.70*** (1.28, 2.26) | 1.70*** (1.28, 2.26) | 0.96 (0.74, 1.25) | 0.97 (0.74, 1.27) |
| Collaboration increased (yes vs no) | 1.78** (1.18, 2.67) | 1.78** (1.18, 2.67) | 1.33 (0.92, 1.91) | 1.34 (0.93, 1.94) |
| Estimated prevalence of diabetes | 0.98 (0.90, 1.08) | 1.20*** (1.11, 1.31) | ||
Note. CI = confidence interval; FTEs = full-time equivalents; OR = odds ratio. Associations established by logistic regression.
*P < .05; **P < .01; ***P < .001.
LHDs in jurisdictions with a population ranging from 100 000 to 499 999 were less likely to carry out diabetes screening programs than were LHDs in smaller jurisdictions (population < 25 000; OR = 0.52; 95% CI = 0.33, 0.83; Table 2). For each percentage point increase in the proportion of African Americans in an LHD's population, the odds of that LHD having a diabetes screening program increased by 1% (OR = 1.01; 95% CI = 1.00, 1.02). However, the significant associations between proportion of African American population and the presence of diabetes screening programs diminished after we adjusted for estimated prevalence of diabetes (Table 2). LHDs with a local board of health (OR = 1.54; 95% CI = 1.15, 2.06) were more likely to carry out diabetes screening programs than were those that did not. A 1% increase in the proportion of federal funding decreased the odds of LHDs conducting diabetes screening programs by 1% (OR = 0.99; 95% CI = 0.98, 1.00). A higher number of staff full-time equivalents per 1000 population (OR = 1.28; 95% CI = 1.01, 1.61) and employing health educators (OR = 1.59; 95% CI = 1.20, 2.11) were significantly associated with LHDs conducting diabetes screening programs. Chronic disease surveillance (OR = 2.45; 95% CI = 1.91, 3.15) was also significantly associated with the presence of diabetes screening programs.
In Table 2, after all other structural capacity and processes factors were controlled, each percentage point increase in the estimated prevalence of diabetes resulted in a 20% increase in the odds of LHDs conducting diabetes screening programs (OR = 1.20; 95% CI = 1.11, 1.31). Because our diabetes prevalences were estimates calculated with the use of statistical modeling, we conducted a sensitivity analysis in which we redid the analyses twice, replacing each estimated prevalence with the point estimate plus 1 standard deviation and minus 1 standard deviation. Although estimates changed, associations between diabetes burden and LHDs having diabetes screening programs remained significant (OR = 1.22; 95%CI = 1.11, 1.34; and OR = 1.18; 95% CI = 1.10, 1.27, respectively). However, an increase in estimated diabetes prevalence did not substantially affect the odds of having an obesity prevention program.
DISCUSSION
We found that approximately half of LHDs had obesity prevention or diabetes screening programs, and about one third had both. A recent survey by the Robert Wood Johnson Foundation found that approximately half of LHDs undertook some type of obesity prevention activity targeted toward adolescents, including healthy eating programs, obesity control programs, and physical activity programs.22 Our findings suggest that LHDs do not consistently have either obesity prevention programs or diabetes screening programs. Moreover, there is some evidence suggesting that LHDs respond to the diabetes epidemic on the basis of community needs. Information on the effectiveness of LHD approaches to obesity and diabetes prevention is limited. The lag between diabetes screening and obesity prevention efforts, as well as the lack of human and financial resources to conduct meaningful process and outcome evaluations, is a serious issue in some LHDs. Because obesity and diabetes are common across all states and are becoming increasingly prevalent among socioeconomically vulnerable populations,29 the role of LHDs as the first line of defense in public health should be evaluated more thoroughly.
We are aware of no randomized trials or sustainable public health interventions in real-world settings that have demonstrated the benefits of obesity prevention programs and early diagnosis of diabetes through screening of asymptomatic individuals at the community level. However, the American Diabetes Association recommends that individuals at high risk (i.e., those aged ≥ 45 years, particularly if they have a body mass index ≥ 25 kg/m2, or those aged < 45 years if they are overweight and have another risk factor for diabetes) should be opportunistically screened in a clinical setting at 3-year intervals.30 The US Preventive Services Task Force recommends that clinicians screen all adult patients for obesity and offer intensive counseling and behavioral interventions to promote sustained weight loss for obese adults.31 The task force also recommends screening for type 2 diabetes in asymptomatic adults with sustained blood pressure (either treated or untreated) greater than 135/80 mm Hg.32
The Medicare Prescription Drug, Improvement, and Modernization Act of 2003 expanded services to cover diabetes screening for Medicare beneficiaries at risk for diabetes or those diagnosed with prediabetes.33 The Department of Veterans Affairs and the Indian Health Service also recommend screening for beneficiaries at risk for diabetes and prediabetes.34,35 Moreover, a regimen consisting of screening for prediabetes, treating those identified as having both impaired glucose tolerance and impaired fasting glucose, and implementing the Diabetes Prevention Program lifestyle intervention has been found cost-effective.36 Nevertheless, there is a clear distinction between evidence-based clinical opportunistic screening and community-based screening. Further evaluation of the effect of public health interventions on obesity and diabetes prevention at LHDs are needed.
Some LHDs provide diabetes education and screening programs within their jurisdictions as part of their public health commitment to “fight” diabetes, even though such programs' effectiveness and cost-effectiveness are unknown. For example, among 94 LHDs in Indiana, 37 had diabetes education and screening programs.37 Among them, 30 LHDs offered screening tests (e.g., random plasma glucose, fasting blood glucose, or hemoglobin A1c test) to persons identified as being at risk for diabetes, and 9 also used a written or verbal questionnaire to identify persons at risk for diabetes. However, screening guidelines are only available in 43% of LHDs in Indiana that offer diabetes screening, and there is no common standard for such screening guidelines. All responding LHDs, regardless of whether they offered a diabetes education or screening program, indicated a need for guidance or instruction about diabetes-specific issues, diabetes screening practices, and referral sources. Appropriate common guidelines, such as the Diabetes Detection Initiative, could prove valuable to LHDs.38,39
Characteristics of Local Health Departments
Increasing our knowledge of the characteristics of LHDs could help us better understand how to build a better local public health infrastructure to cope with obesity and diabetes epidemics. Previous studies have suggested that greater local health agency capacity (e.g., budget and staff) was associated with better implementation of public health services.14,16,17 We did not find a strong association between public health expenditure and LHDs conducting obesity prevention and diabetes screening programs. Despite our failure to find cross-sectional associations, previous expenditures by LHDs might still be important. Moreover, our findings suggest that many other characteristics of LHD structural capacity are associated with the presence of obesity prevention and diabetes screening programs. For example, we found that LHD staffing levels were significantly associated with both obesity prevention and diabetes screening programs. LHDs with a higher proportion of state funding were more likely to carry out obesity prevention programs than were those with a lower proportion of state funding. Although only 55% of LHDs had health educators,28 employing health educators in a LHD was significantly associated with LHDs having obesity prevention and diabetes screening programs.
After having accounted for other factors, having a full-time top agency executive and an executive with a medical or public health degree were positively associated with the presence of obesity prevention programs, and having a local board of health was positively associated with the presence of diabetes screening programs. Earlier studies have also suggested that having a full-time director was associated with providing more public health services,14,16 but the director's academic degrees may not be.14,25 Kennedy also found a positive relationship between performance of public health practices and having an LHD director with more public health work experience.16 Mays et al. evaluated the effects that local boards of health had on LHDs performing public health practices, and they found that more public health activities were performed in jurisdictions with policymaking boards of health than in jurisdictions without these entities.17
Previous studies have found that population size is an important predictor of provision of essential public health services.13,16,17,20 For example, in 1998, Mays et al. surveyed the LHD directors of the 497 most populous US communities.17 They found that public health activities were performed significantly more often in communities with larger populations. Another study of a national sample of 425 LHDs found that health departments serving a population of more than 50 000 reported better implementation of performance measures on the basis of the 10 essential public health practices.20 However, Handler et al. did not find jurisdiction size to be correlated with effective public health practice performance in a national stratified random sample of 264 LHDs.14 Overall, we found that population size was not a significant correlate affecting whether LHDs carried out obesity and diabetes programs.
We found a positive association between high-performance LHDs and the presence of obesity prevention and diabetes screening programs. For example, having chronic disease surveillance at LHDs was found to be significantly associated with carrying out obesity prevention and diabetes screening programs. Additionally, conducting risk behavior surveillance was positively associated with the presence of obesity prevention programs. Through properly monitoring disease prevalence and incidence, local public health agencies could identify emerging public health problems and implement timely public health interventions, which is one of the key essential public health services at LHDs. However, our analysis did not permit us to discern whether this association was attributable to the surveillance activity itself or to other agency factors (e.g., other structural capacity characteristics or mission changes) not assessed in the model.
LHDs that had recently conducted a health assessment, developed a health improvement plan, or increased external collaborations were significantly more likely to have obesity prevention programs than were LHDs that did not perform any of these activities. Healthy People 2010 has set objectives for the public health infrastructure and encourages LHDs to meet national performance standards for essential public health services, to review and evaluate their delivery of essential public health services, to have a health improvement plan, and to collaborate on population-based prevention research.40 Partnership and collaboration with nonprofit and managed care organizations, neighborhood jurisdictions, and other government agencies could help improve the capacity and infrastructure of local public health systems.27 A community health assessment collects and assesses a broad range of information on a community's health and well-being, and community health improvement planning helps improve the community's overall health and well-being through specific steps and goals to guide providers of essential public health services in addressing problems and gaps. Unfortunately, only approximately 51% of LHDs had recently completed a community health assessment, and approximately 54% had completed a community health improvement plan in the prior 3 years.28
Finally, our findings suggest an association between diabetes burden and the presence of diabetes screening programs, which indicated a potential positive response to community needs on the part of LHDs. However, LHDs often have limited resources to devote to necessary public health efforts. Furthermore, LHDs with a larger African American population were more likely to have diabetes screening programs (model 1), even though adjustment for diabetes prevalence diminishes this effect (model 2). Given the higher prevalence of diabetes among African American populations,2,41 this finding suggests that LHDs may have made special efforts to be responsive to community needs related to diabetes.
Limitations
This study has a number of limitations. We assessed correlation, not causality, and attributing cause and effect becomes even more difficult in the evaluation of obesity interventions because some LHDs had implemented obesity prevention programs that reached similar target populations at the same time. Although most of the survey questions in the 2005 NPLHD had been used in previous LHD surveys (i.e., 1989, 1992–1993, and 1996–1997) and tested by a pilot survey, the instruments have not been evaluated for validity or reliability. Furthermore, we only assessed general questions on LHDs' implementation of obesity prevention and diabetes screening programs, but other effects that LHDs' public health intervention activities may have had on prevention and control of obesity and diabetes were not explored. There were no standard definitions of obesity prevention or diabetes screening programs. The information in this study about conducting obesity prevention and diabetes screening programs was self-reported, which could introduce social desirability bias. Moreover, it is not clear how the more recent national attention to obesity and the recession in the United States has affected LHDs.
The estimated prevalence of diabetes we used in the model did not reflect actual variability in prevalence and did not include persons with undiagnosed diabetes. The ratio of diagnosed to undiagnosed diabetes may vary geographically. However, because LHDs would be unaware of this component of the overall diabetes burden, this may not affect our findings.
Because of a lack of obesity prevalence data, we were not able to explore the association between prevalence of obesity and LHDs carrying out obesity prevention programs. We treated the responses as though they were a random sample and only examined variables collected in NPLHD, which may have caused unexpected bias. Those states with low response rates are likely not well represented. Additionally, other information (e.g., community socioeconomic characteristics, organizational culture, turnover rate) that could also be associated with LHDs' public health activities was not included. Unfortunately, this information could not be fully investigated in this analysis. We did not include PhD-level education in the measurement, which may lead to a weaker association. Finally, the study data did not permit us to examine the influence of the administrative relationship between local and state health departments, which could have influenced LHD activities.17,27
Conclusions
The obesity and diabetes epidemics pose an immense challenge for local public health agencies, many of which may not have a well-developed infrastructure for chronic disease prevention and control. However, LHDs are the foundation of local public health infrastructure, and they are in a unique position to coordinate and initiate policy and environmental changes; thus, they have a special responsibility in the effort to prevent obesity and diabetes.
Acknowledgments
We thank the National Association of County and City Health Officials and the Centers for Disease Control and Prevention for providing the data for this analysis.
Human Participant Protection
No protocol approval was necessary because data were obtained from secondary sources.
References
- 1.Flegal KM, Carroll MD, Ogden CL, Johnson CL. Prevalence and trends in obesity among US adults, 1999–2000. JAMA 2002;288(14):1723–1727 [DOI] [PubMed] [Google Scholar]
- 2.Ogden CL, Carroll MD, Curtin LR, McDowell MA, Tabak CJ, Flegal KM. Prevalence of overweight and obesity in the United States, 1999–2004. JAMA 2006;295(13):1549–1555 [DOI] [PubMed] [Google Scholar]
- 3.Ogden CL, Carroll MD, McDowell MA, Flegal KM. Obesity Among Adults in the United States—No Change Since 2003–2004 Hyattsville, MD: National Center for Health Statistics; 2007. NCHS Data Brief 1 [Google Scholar]
- 4.Miniño AM, Heron MP, Murphy SL, Kochankek KD. Deaths: final data for 2004. Natl Vital Stat Rep 2007;55(19). [PubMed] [Google Scholar]
- 5.Harris MI, Flegal KM, Cowie CC, et al. Prevalence of diabetes, impaired fasting glucose, and impaired glucose tolerance in US adults. The third National Health and Nutrition Examination Survey, 1988–1994. Diabetes Care 1998;21(4):518–524 [DOI] [PubMed] [Google Scholar]
- 6.Centers for Disease Control and Prevention National diabetes fact sheet: United States, 2005. Available at: http://www.cdc.gov/diabetes/pubs/pdf/ndfs_2005.pdf. Accessed November 19, 2007
- 7.Centers for Disease Control and Prevention National diabetes fact sheet, 2007. Available at: http://www.cdc.gov/diabetes/pubs/pdf/ndfs_2007.pdf. Accessed June 26, 2008
- 8.Beitsch LM, Brooks RG, Menachemi N, Libbey PM. Public health at center stage: new roles, old props. Health Aff (Millwood) 2006;25(4):911–922 [DOI] [PubMed] [Google Scholar]
- 9.Brownson RC, Bright FS. Chronic disease control in public health practice: looking back and moving forward. Public Health Rep 2004;119(3):230–238 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Centers for Disease Control and Prevention The burden of chronic diseases and their risk factors: national and state perspectives. Available at: http://www.cdc.gov/nccdphp/burdenbook2004/pdf/burden_book2004.pdf. Accessed June 26, 2008
- 11.Frieden TR. Asleep at the switch: local public health and chronic disease. Am J Public Health 2004;94(12):2059–2061 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Steinbrook R. Facing the diabetes epidemic—mandatory reporting of glycosylated hemoglobin values in New York City. N Engl J Med 2006;354(6):545–548 [DOI] [PubMed] [Google Scholar]
- 13.Freund CG, Liu Z. Local health department capacity and performance in New Jersey. J Public Health Manag Pract 2000;6(5):42–50 [DOI] [PubMed] [Google Scholar]
- 14.Handler AS, Turnock BJ. Local health department effectiveness in addressing the core functions of public health: essential ingredients. J Public Health Policy 1996;17(4):460–483 [PubMed] [Google Scholar]
- 15.Honore PA, Simoes EJ, Jones WJ, Moonesinghe R. Practices in public health finance: an investigation of jurisdiction funding patterns and performance. J Public Health Manag Pract 2004;10(5):444–450 [DOI] [PubMed] [Google Scholar]
- 16.Kennedy VC. A study of local public health system performance in Texas. J Public Health Manag Pract 2003;9(3):183–187 [DOI] [PubMed] [Google Scholar]
- 17.Mays GP, Halverson PK, Baker EL, Stevens R, Vann JJ. Availability and perceived effectiveness of public health activities in the nation's most populous communities. Am J Public Health 2004;94(6):1019–1026 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Mete C, Cioffi JP, Lichtveld MY. Are public health services available where they are most needed? An examination of local health department services. J Public Health Manag Pract 2003;9(3):214–223 [DOI] [PubMed] [Google Scholar]
- 19.Suen J, Magruder C. National profile: overview of capabilities and core functions of local public health jurisdictions in 47 states, the District of Columbia, and 3 US territories, 2000–2002. J Public Health Manag Pract 2004;10(1):2–12 [DOI] [PubMed] [Google Scholar]
- 20.Turnock BJ, Handler A, Hall W, Potsic S, Nalluri R, Vaughn EH. Local health department effectiveness in addressing the core functions of public health. Public Health Rep 1994;109(5):653–658 [PMC free article] [PubMed] [Google Scholar]
- 21.Turnock BJ, Handler AS, Miller CA. Core function–related local public health practice effectiveness. J Public Health Manag Pract 1998;4(5):26–32 [DOI] [PubMed] [Google Scholar]
- 22.Slater SJ, Powell LM, Chaloupka FJ. Missed opportunities: local health departments as providers of obesity prevention programs for adolescents. Am J Prev Med 2007;33(4, suppl):S246–S250 [DOI] [PubMed] [Google Scholar]
- 23.Handler A, Issel M, Turnock B. A conceptual framework to measure performance of the public health system. Am J Public Health 2001;91(8):1235–1239 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Centers for Disease Control and Prevention Diabetes data & trends. Available at: http://www.cdc.gov/diabetes/statistics/index.htm. Accessed June 26, 2008
- 25.Scutchfield FD, Knight EA, Kelly AV, Bhandari MW, Vasilescu IP. Local public health agency capacity and its relationship to public health system performance. J Public Health Manag Pract 2004;10(3):204–215 [DOI] [PubMed] [Google Scholar]
- 26.Donabedian A. Explorations in Quality Assessment and Monitoring: The Definition of Quality and Approaches to Its Assessment Vol 1 Ann Arbor, MI: Health Administration Press; 1980 [Google Scholar]
- 27.Mays GP, McHugh MC, Shim K, et al. Institutional and economic determinants of public health system performance. Am J Public Health 2006;96(3):523–531 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.National Association of County and City Health Officials 2005 National Profile of Local Health Departments Washington, DC: National Association of County and City Health Officials; 2006 [Google Scholar]
- 29.Candib LM. Obesity and diabetes in vulnerable populations: reflection on proximal and distal causes. Ann Fam Med 2007;5(6):547–556 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.American Diabetes Association Standards of medical care in diabetes—2007. Diabetes Care 2007;30(suppl 1):S4–S41 [DOI] [PubMed] [Google Scholar]
- 31.US Preventive Services Task Force Screening for obesity in adults: recommendations and rationale. Ann Intern Med 2003;139(11):930–932 [DOI] [PubMed] [Google Scholar]
- 32.US Preventive Services Task Force Screening for type 2 diabetes mellitus in adults: US Preventive Services Task Force recommendation statement. Ann Intern Med 2008;148(11):846–854 [DOI] [PubMed] [Google Scholar]
- 33.Centers for Medicare and Medicaid Services Diabetes screening: overview. Available at: http://www.cms.hhs.gov/DiabetesScreening. Accessed December 12, 2007
- 34.US Dept of Veterans Affairs VHA/DOD clinical practice guidelines for the management of diabetes mellitus in the primary care setting. Available at: http://www.va.gov/diabetes/docs/Clinical_Practice_Guidelines.doc. Accessed April 9, 2010
- 35.US Indian Health Service Guidelines for care of adults with prediabetes and/or the metabolic syndrome in clinical settings: September 2008. Available at: http://www.ihs.gov/MedicalPrograms/Diabetes/HomeDocs/Tools/ClinicalGuidelines/PreDiabetes_Guidelines_0209.pdf. Accessed April 9, 2010 [DOI] [PubMed]
- 36.Hoerger TJ, Hicks KA, Sorensen SW, et al. Cost-effectiveness of screening for prediabetes among overweight and obese US adults. Diabetes Care 2007;30(11):2874–2879 [DOI] [PubMed] [Google Scholar]
- 37.Indiana State Dept of Health Survey of diabetes community education and screening programs offered through local health departments in Indiana. Available at: https://secure.in.gov/isdh/files/survey-2.pdf. Accessed November 16, 2007
- 38.Lanza A, Albright A, Zucker H, Martin M. The Diabetes Detection Initiative: a pilot program of selective screening. Am J Health Behav 2007;31(6):632–642 [DOI] [PubMed] [Google Scholar]
- 39.US Dept of Health and Human Services Diabetes Detection Initiative (DDI). Available at: http://ndep.nih.gov/ddi/index.htm. Accessed November 16, 2007
- 40.US Dept of Health and Human Services Healthy People 2010: Understanding and Improving Health 2nd ed Washington, DC: US Government Printing Office; 2000 [Google Scholar]
- 41.Cowie CC, Rust KF, Byrd-Holt DD, et al. Prevalence of diabetes and impaired fasting glucose in adults in the US population: National Health and Nutrition Examination Survey 1999–2002. Diabetes Care 2006;29(6):1263–1268 [DOI] [PubMed] [Google Scholar]