Abstract
Objectives. We examined racial/ethnic disparities in highly active antiretroviral therapy (HAART) use and whether differences are moderated by substance use or insurance status, using data from the Women's Interagency HIV Study (WIHS).
Methods. Logistic regression examined HAART use in a longitudinal cohort of women for whom HAART was clinically indicated in 2005 (N = 1354).
Results. Approximately 3 of every 10 eligible women reported not taking HAART. African American and Hispanic women were less likely than were White women to use HAART. After we adjusted for potential confounders, the higher likelihood of not using HAART persisted for African American but not for Hispanic women. Uninsured and privately insured women, regardless of race/ethnicity, were less likely than were Medicaid enrollees to use HAART. Although alcohol use was related to HAART nonuse, illicit drug use was not.
Conclusions. These findings suggest that expanding and improving insurance coverage should increase access to antiretroviral therapy across racial/ethnic groups, but it is not likely to eliminate the disparity in use of HAART between African American and White women with HIV/AIDS.
The epidemic of HIV/AIDS among women reflects a convergence of medical and social policy issues—including race, substance use, and sexual behavior—that are difficult to disentangle and address. Since the introduction of highly active antiretroviral therapy (HAART) as the standard of care in 1996, mortality rates from AIDS and its complications have declined dramatically.1 However, the decline in AIDS deaths between 1993 and 2001 occurred at a much slower rate among African American men and women than among White men and women.2 One possible explanation for the slower rate of decline is differences in access to quality medical care. In addition, there is growing evidence of lower use of HAART by women of color compared with other women.3
Shapiro et al.4 analyzed data from the HIV Cost and Services Utilization Study, the only nationally representative study of US adults receiving care for HIV infection, and reported that African Americans were less likely than were Whites with similar CD4 counts to obtain combination drug therapy in 1998, 2 years after HAART became the standard of care for HIV infection. However, in a subsequent study that also analyzed HIV Cost and Services Utilization Study data, Cunningham et al.5 reported that racial/ethnic identity was not associated with receipt of HAART when they used a series of nested multivariate models that adjusted for factors that had been found to explain race-associated effects in earlier analyses. In their final analytic model, only insurance coverage and CD4 count were statistically significant predictors of HAART use.
At least 2 studies3,6 have provided evidence that HIV-infected African American women are less likely than HIV-infected White women to receive HAART, and several national studies have indicated that African Americans fare worse than Whites on a number of recognized standards of HIV care.4,5,7 The same studies have also documented significant disparities in HAART use among illicit drug users. These studies assessed the independent effects of race, illicit substance abuse, and insurance coverage on use of medical care by people with HIV/AIDS.
Studies of HIV-infected women have reported mixed findings regarding the roles of race/ethnicity and substance use in receipt of HAART when insurance status is taken into account. Analyzing data from the Women's Interagency HIV Study (WIHS), Cohen et al.3 and Cook et al.6 reported that women who were either African American or illicit drug users were less likely to report using HAART than were their counterparts who were White or nondrug users, respectively. However, the studies' findings differed on how Hispanic women fared relative to White women and on the effects of insurance coverage on receipt of HAART.
Although these studies have substantially contributed to understanding factors associated with receipt of HAART, considerable gaps in knowledge still exist. We investigated the hypothesis that the combination of race/ethnicity and insurance status represents a greater risk than either factor alone for nonuse of HAART and that the association is more complex than the simple “main” effects used in previous research. We believe that continuing to track patterns of HIV care and clinically indicated HAART use, in particular, is important for gauging progress in reducing disparities in care and for informing HIV treatment policies and clinical practices.
METHODS
Data from the WIHS were used for this analysis. The WIHS data were collected at 6 clinical centers nationwide: in Brooklyn, New York; the Bronx, New York; Washington, District of Columbia; Chicago, Illinois; Los Angeles, California; and the San Francisco Bay Area, California. Funded by the National Institutes of Health, the WIHS is a longitudinal, observational study that recruited women from HIV care sites, drug treatment programs, HIV-testing sites, community-based organizations, and sexually transmitted disease clinic programs. A standardized interview-based questionnaire was used to collect information on demographics, medical history, use of antiretroviral medications, and measures of psychosocial history. Detailed information on the study methodology, quality assurance, and baseline characteristics of the enrollees has been reported previously.8
Women who were HIV infected and uninfected were recruited at study inception in 1994 and 1995 and during a second wave of enrollment in 2001 and 2002. Follow-up interviews were conducted at 6-month intervals. Study participants enrolled at the 2 time periods did not differ significantly in terms of race/ethnicity, income, or education. However, by design, the second wave of enrollees were younger and had less-advanced HIV disease than women initially enrolled in 1994 and 1995.9 Since the inception in 1994, the WIHS protocol has included recommendations for referral to needed services of those who reported drug use, domestic abuse, depression, or not seeing a primary care provider.
The study population for this analysis (N = 1354) was limited to the subset of HIV-infected women who self-identified as White, African American or Black, or Hispanic or Latina, and who were clinically eligible for HAART prior to or at visit 22 (in 2005). Clinical eligibility for HAART was based on criteria used in a prior study3 of WIHS participants: either (1) current use of HAART, (2) CD4 count of less than 350/mm3, or (3) a viral load greater than 50 000 copies. Of the 1354 women who met the study eligibility criteria, 12 women became clinically eligible at the current visit by CD4+ cell count (< 350/mm3) or viral load (> 50 000 copies). Of these women, 9 were not on HAART and 3 were on HAART.
Measures
The major outcome of this analysis was current self-reported use of HAART (yes or no). We used an indicator variable of HAART use that was constructed by the WIHS on the basis of guidelines, published by the Department of Health and Human Services, that were in place at the time of each study visit.3 In our study, non-HAART combination antiretroviral therapy, monotherapy, and no therapy were all grouped in the HAART nonuse category.
Sociodemographic and health factors assessed in the multivariate analysis included race/ethnicity (mutually exclusive categories were created for non-Hispanic Whites, non-Hispanic African Americans, and Hispanics), age in years at the study visit, poverty (income at baseline in relation to family size, based on the federal poverty level for the baseline years [http://aspe.hhs.gov/Poverty/figures-fed-reg.shtml]), years of education, employment (yes or no at baseline), HCV serology at baseline, and depressive symptoms (a binary indicator of a score of 23 or higher on the Center for Epidemiologic Studies Depression Scale [CES-D]).10
Indicators of alcohol use (nonuse, light drinker [< 3 drinks per week], moderate drinker [3–13 drinks per week], heavy drinker [> 13 drinks per week])11 and indicators of use of crack, cocaine, or heroin (never, only prior to study enrollment, during the study but not in the prior 6 months, and current use [prior 6 months]) were included in the multivariate analysis.
To classify each woman's health insurance coverage, we created 4 mutually exclusive categories: uninsured, private, Medicare or other, and Medicaid or Medi-Cal. We constructed the categories using a classification hierarchy that is used by the Kaiser Commission on Medicaid and Uninsured and the Urban Institute when analyzing data from the Current Population Survey.12 All participants who reported Medicaid (or Medi-Cal) coverage were assigned to the Medicaid category. The remaining respondents were then assigned to private coverage, Medicare, military-related coverage such as Civilian Health and Medical Program of the Uniformed Services (CHAMPUS), or other (e.g., student, no type specified), in that order. Because of the small number of respondents with CHAMPUS, respondents with private coverage or CHAMPUS were collapsed into a single category. Respondents who reported no public or private source of insurance were classified as uninsured.
Women who identified the AIDS Drug Assistance Program of the Ryan White Care Act as their only resource for paying for medications were classified as uninsured, since the AIDS Drug Assistance Program is not a public or private health insurance plan with a defined benefit package beyond paying for medications. A binary indicator of enrollment in the AIDS Drug Assistance Program was also included in the regression models because, in addition to 72 uninsured women who reported receiving services through the AIDS Drug Assistance Program, 109 women with either public or private insurance coverage also reported receiving services through the AIDS Drug Assistance Program.
To further explore possible factors that might explain use of HAART, we examined the effect of having a usual source of medical care. Women were categorized into 3 groups on the basis of responses to a series of questions about their usual source of medical care. The first question asked whether the woman had seen a “health care provider” since the last study visit. If a woman had seen a health care provider, she was subsequently asked if she saw the same provider or group of providers and was then asked to identify the place of care.
Statistical Analysis
In a cross-sectional analysis, we examined HAART use among women who met the study eligibility criteria prior to or at WIHS visit 22 (in 2005), the most recent visit wave available at the time this analysis was undertaken. We then examined patterns of HAART use and nonuse by the primary independent variables (race/ethnicity, health insurance coverage, and illicit drug use).
We used several logistic regression models to assess the likelihood of nonuse of HAART. Model 1 examined the unadjusted likelihood of nonuse of HAART by race/ethnicity. Model 2 examined the adjusted likelihood of nonuse of HAART while controlling for measures of substance abuse (alcohol use; crack, cocaine, or heroin use), health insurance coverage, and other potential confounders (age, income, education, depressive symptoms, enrollment cohort, and study site). Model 3 tested interaction terms for race/ethnicity and insurance coverage to examine the combined effects of these 2 variables and to determine whether the main effects of the 2 variables adequately captured their contribution to HAART nonuse. Model 4 examined the effects of having a usual source of medical care on nonuse of HAART.
RESULTS
Table 1 provides the sociodemographic and health characteristics of the women in the WIHS that met study criteria in 2005 (N = 1354). Slightly more than half of the women were African American and a little over one quarter were Hispanic. At enrollment, the vast majority (72%) of the women had incomes below twice the federal poverty level and slightly more than a third (39%) did not have a high school degree. Half of the women were 40 to 49 years of age in 2005. Although most (56%) of the women reported a history of prior use of crack, cocaine, or heroin, fewer than 10% reported use in the 6 months prior to the study visit. Most of the women were nondrinkers or light drinkers; however, about 11% reported they were either moderate or heavy users of alcohol.
TABLE 1.
Characteristics of Women Clinically Eligible for Highly Active Antiretroviral Therapy (HAART): Women's Interagency HIV Study, 2005
| Characteristic | Women (n = 1354), No. (%) |
| Sociodemographic | |
| Race/ethnicitya | |
| Non-Hispanic African American | 778 (57.5) |
| Hispanic | 390 (28.8) |
| Non-Hispanic White | 186 (13.7) |
| Family poverty level,b % | |
| < 199 | 974 (71.9) |
| ≥ 200 | 344 (25.4) |
| Missing | 36 (2.7) |
| HIV exposure | |
| Injection drug use | 319 (23.6) |
| Heterosexual contact | 586 (43.3) |
| Transfusion | 31 (2.3) |
| No risk Identified | 410 (30.3) |
| Missing | 8 (0.6) |
| Age, y | |
| < 40 | 290 (21.4) |
| 40–49 | 677 (50.0) |
| ≥ 50 | 387 (28.6) |
| Education | |
| Less than high school | 529 (39.1) |
| High school graduate | 394 (29.1) |
| Some college | 338 (25.0) |
| College graduate | 92 (6.8) |
| Insurance coveragec | |
| Medicaid or Medi-Cal | 847 (62.6) |
| Private or CHAMPUS | 203 (15.0) |
| Medicare or other | 57 (4.2) |
| Uninsured | 152 (11.2) |
| Missing | 95 (7.0) |
| AIDS Drug Assistance Program | |
| Yes | 206 (15.2) |
| No | 1118 (82.6) |
| Missing | 30 (2.2) |
| Usual source of care | |
| Physician or clinic | 1026 (75.7) |
| Emergency department or other | 170 (12.6) |
| Unknown | 158 (11.7) |
| Health | |
| CD4 count, cells/mL | |
| Low (< 200) | 211 (15.6) |
| Medium (200–500) | 603 (44.5) |
| High (> 500) | 512 (37.8) |
| Missing | 28 (2.1) |
| HIV RNA viral load,d copies | |
| ≤ 10 000 | 1056 (78.0) |
| > 10 000 | 268 (19.8) |
| Missing | 30 (2.2) |
| HCV infection | |
| Yes | 389 (28.7) |
| No | 925 (68.3) |
| Missing | 40 (3.0) |
| Crack, cocaine, or heroin use | |
| Never | 561 (41.4) |
| Only prior to study enrollment | 320 (23.6) |
| During study, but not currently | 316 (23.3) |
| Current use (within last 6 mo) | 130 (9.6) |
| Missing | 27 (2.0) |
| Alcohol usee | |
| None | 720 (53.2) |
| Light | 460 (34.0) |
| Moderate | 125 (9.2) |
| Heavy | 26 (1.9) |
| Missing | 23 (1.7) |
| Depressive symptoms | |
| Probable (CES-D score ≥ 23) | 345 (25.5) |
| All others (CES-D score < 23) | 970 (71.6) |
| Missing | 39 (2.7) |
Note. CES-D = Center for Epidemiologic Studies Depression scale; CHAMPUS = Civilian Health and Medical Program of the Uniformed Services; RNA = ribonucleic acid.
Women of “other” racial/ethnic groups are not included in this analysis.
Percentage of the federal poverty level defined by the US Department of Health and Human Services for the baseline years.
“Other” includes women who identified their coverage as student coverage or sources that were not specified.
The mean and median viral loads for the study population were 24 326 and 80, respectively.
Light drinker = < 3 drinks per week; moderate drinker = 3–13 drinks per week; heavy drinker = >13 drinks per week.
Almost two thirds (63%) of the study participants were insured with Medicaid or Medi-Cal and 11% were uninsured (Table 1). The proportion covered by Medicaid or Medi-Cal varied by race/ethnicity: 69% for African American women and 59% for Hispanic women versus 41% for White women. In contrast, a larger percentage of White women (39%) than African American (13%) or Hispanic (7%) women had private insurance.
Approximately 75% of the women identified a physician or clinic as their usual source of medical care and 13% identified an emergency department in a hospital, a drug treatment clinic, a prison clinic, or other source of care. The remaining 12% were classified as “unknown” usual source of medical care because they were mostly women who had not seen a doctor since the last study visit and thus were not asked the follow-up question on place of care.
Self-Reported Use of HAART
As shown in Table 2, 29% of the women clinically eligible for HAART reported not using it in 2005. The crude estimates indicate a higher proportion of nonuse of HAART among African American and Hispanic women than among White women and generally higher rates of nonuse of HAART among uninsured women than among women with Medicaid coverage. Uninsured White women, however, reported lower rates of nonuse than did uninsured African American or Hispanic women (Figure 1).
TABLE 2.
Number and Percentage of Clinically Eligible Women Not Using Highly Active Antiretroviral Therapy (HAART), by Race/Ethnicity and Insurance Status: Women's Interagency HIV Study, 2005
| Women, No. (%) | |
| Overall | 390 (28.8) |
| Race/ethnicity | |
| Non-Hispanic African American | 251 (32.3) |
| Hispanic | 104 (26.7) |
| Non-Hispanic White | 35 (18.8) |
| Insurance status | |
| Medicaid or Medi-Cal | 232 (27.4) |
| Private or CHAMPUS | 60 (29.6) |
| Medicare or other | 17 (29.8) |
| Uninsured | 57 (37.5) |
| Missing | 24 (25.3) |
Note. CHAMPUS = Civilian Health and Medical Program of the Uniformed Services.
FIGURE 1.
Percentage of clinically eligible women not using highly active antiretroviral therapy (HAART), by race/ethnicity and insurance: Women's Interagency HIV Study, 2005.
Table 3 presents the unadjusted odds ratios (ORs) and adjusted odds ratios (AORs) of not using HAART. The unadjusted ORs for nonuse of HAART were higher for African American women (OR = 2.06; 95% confidence interval [CI] = 1.39, 3.07) and Hispanic women (OR = 1.57; 95% CI = 1.02, 2.41) than they were for White women. After adjustment for potential confounders, the likelihood of nonuse of HAART by African American women remained roughly twice that of White women (OR = 2.01; 95% CI = 1.22, 3.31). However, the difference in risk between Hispanic and White women was attenuated when demographic and other differences were controlled for in the adjusted regression analysis.
TABLE 3.
Results of Unadjusted and Adjusted Logistic Regression for the Likelihood of Clinically Eligible Women Not Using Highly Active Antiretroviral Therapy (HAART): Women's Interagency HIV Study, 2005
| OR (95% CI) |
||||
| Model 1 | Model 2b | Model 3c | Model 4d | |
| Race/ethnicitya | ||||
| Non-Hispanic African American | 2.06* (1.39, 3.07) | 2.01* (1.22, 3.31) | 1.71 (0.89, 3.32) | 2.00* (1.21, 3.31) |
| Hispanic | 1.57* (1.02, 2.41) | 1.37 (0.80, 2.37) | 1.39 (0.69, 2.79) | 1.32 (0.76, 2.28) |
| Non-Hispanic White (Ref) | 1.00 | 1.00 | 1.00 | 1.00 |
| Crack, cocaine, or heroin use | ||||
| Only prior to study enrollment | 0.80 (0.53, 1.21) | 0.82 (0.54, 1.24) | 0.82 (0.54, 1.24) | |
| During study, but not currently | 1.33 (0.89, 1.98) | 1.38 (0.92, 2.07) | 1.34 (0.90, 2.01) | |
| Current use (within last 6 mo) | 1.07 (0.62, 1.84) | 1.11 (0.65, 1.91) | 1.02 (0.59, 1.77) | |
| Never (Ref) | 1.00 | 1.00 | 1.00 | |
| Alcohol use | ||||
| Light | 1.39* (1.03, 1.89) | 1.37* (1.02, 1.86) | 1.42* (1.05, 1.93) | |
| Moderate | 1.72* (1.10, 2.70) | 1.70* (1.08, 2.66) | 1.71* (1.09, 2.67) | |
| Heavy | 2.29 (0.96, 5.47) | 2.27 (0.93, 5.51) | 2.24 (0.93, 5.41) | |
| None (Ref) | 1.00 | 1.00 | 1.00 | |
| Insurance status | ||||
| Uninsured | 2.38* (1.52, 3.73) | 1.73 (0.43, 6.95) | 2.21* (1.39, 3.49) | |
| Private or CHAMPUS | 2.06* (1.25, 3.40) | 2.71 (0.65, 4.50) | 2.09* (1.26, 3.46) | |
| Medicare or other | 1.40 (0.49, 4.00) | 1.43 (0.50, 4.10) | 1.43 (0.50, 4.06) | |
| Medicaid or Medi-Cal (Ref) | 1.00 | 1.00 | 1.00 | |
| AIDS Drug Assistance Program | ||||
| Yes | 0.54* (0.34, 0.85) | 0.53* (0.34, 0.84) | 0.57* (0.37, 0.90) | |
| No (Ref) | 1.00 | 1.00 | 1.00 | |
| Depressive symptoms | ||||
| Probable (CES-D score ≥ 23) | 1.34 (0.99, 1.81) | 1.33 (0.98, 1.79) | 1.36* (1.01, 1.84) | |
| All others (CES-D score < 23) (Ref) | 1.00 | 1.00 | 1.00 | |
| Race/ethnicity × insurance | ||||
| Non-Hispanic African American × uninsured | 1.38 (0.03, 5.99) | |||
| Non-Hispanic African American × private | 1.82 (0.64, 5.14) | |||
| Hispanic × uninsured | 1.40 (0.30, 6.64) | |||
| Hispanic × private | 0.18 (0.03, 1.17) | |||
| Non-Hispanic White × Medicaid (Ref) | 1.00 | |||
| Usual source of care | ||||
| Unknown | 1.70* (1.00, 2.90) | |||
| Physician or clinic | 0.74 (0.49, 1.11) | |||
| Emergency department or other (Ref) | 1.00 | |||
Note. CI = confidence interval; CES-D = Center for Epidemiologic Studies Depression Scale; CHAMPUS = Civilian Health and Medical Program of the Uniformed Service; OR = odds ratio.
Women of “other” racial/ethnic groups were not included in this analysis.
Model 2 included race/ethnicity; age; poverty status; education; employment; insurance coverage; crack, cocaine, or heroin use; alcohol use; HCV infection; CES-D indicator; and study site.
Model 3 included all the variables in model 2 plus the interaction terms for non-Hispanic African American × uninsured, non-Hispanic African American × private, Hispanic × uninsured, and Hispanic × private.
Model 4 included all the variables in model 2 plus a measure of usual source of care. Most of the women in the “unknown” category reported they had not seen a provider since their last visit 6 months ago, and therefore were not asked the question about usual source of care.
P ≤ .05.
Race, Insurance, and Substance Abuse and Use of HAART
Having insurance, as well as the type of insurance, was associated with use of HAART (Table 3, models 2 and 4). Uninsured women were twice as likely as were women with Medicaid or Medi-Cal coverage to report nonuse of HAART (OR = 2.38; 95% CI = 1.52, 3.73; model 2). The odds of not using HAART were also higher for women with private insurance coverage than they were for those with Medicaid or Medi-Cal coverage (OR = 2.06; 95% CI = 1.25, 3.40; model 2). Women enrolled in the AIDS Drug Assistance Program had the lowest odds of not using HAART (OR = 0.54; 95% CI = 0.34, 0.85; model 2), after adjustment for insurance coverage and other factors.
Model 3 (Table 3) tested whether the combined effects of race and insurance coverage had an interactive effect on nonuse of HAART. Although there is no strong evidence to support this hypothesis, marginally statistically significant and almost certainly practically important differences (P < .10) were observed, suggesting that Hispanic women with private coverage may be at lower risk of not using HAART than White women with Medicaid coverage, the comparison group in this analysis. A larger population sample would be needed to determine with confidence whether this subgroup of Hispanic women are truly at lower risk of not using HAART.
Alcohol use was related to nonuse of HAART; however, crack, cocaine, or heroin use, regardless of whether it occurred prior to or during the study period, was not. The odds of not using HAART were higher for light drinkers (OR = 1.39; 95% CI = 1.03, 1.89; model 2) and moderate drinkers (OR = 1.72; 95% CI = 1.10, 2.70; model 2) than for nondrinkers.
Other Factors Associated With HAART Use
To probe 1 possible explanation for the higher odds of not using HAART among the privately insured, we examined whether having a usual source of medical care affected the study's findings. Model 4 (Table 3) provides evidence that women with an “unknown” usual source of care had a higher likelihood of not using HAART than the reference group of women whose usual source of care was an emergency department, drug clinic, or othersource (OR = 1.70; 95% CI = 1.00, 2.90; model 4). Most of the women with “unknown” usual source of care had not seen a provider in the last 6 months and thus were not asked the question about their usual source of care. There was, however, no statistically significant difference in nonuse of HAART between women who identified their usual source of care as a physician or clinic and women who identified it as an emergency department, drug clinic, or other source. Moreover, adjusting for having a usual source of care did not alter the greater odds of not taking HAART among privately insured women and African American women compared with their respective counterparts. It did, however, affect the relationship between depressive symptoms and HAART use. Adjusting for usual source of medical care resulted in women with depressive symptoms having statistically significant higher odds of not using HAART than women not reporting depressive symptoms (OR = 1.36; 95% CI = 1.01, 1.84; model 4).
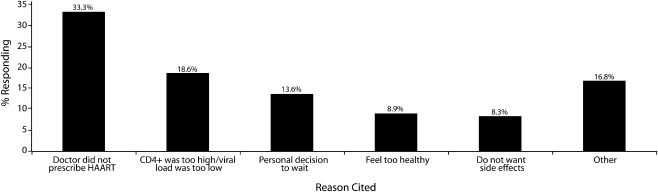
When women who were eligible for HAART but not using it were asked their main reason for not doing so (Figure 2), 33% replied that their doctor did not prescribe it. The next 2 most frequent reasons were that their CD4 count was too high or viral load too low (19%) and that it was a personal decision to wait (14%).
FIGURE 2.
Reasons cited for not taking highly active antiretroviral therapy (HAART): Women's Interagency HIV Study, 2005.
DISCUSSION
This analysis provides evidence that disparities in use of HAART persist among women with HIV/AIDS even when the potential interactive effects of race and insurance coverage are considered. African American women were twice as likely as White women to report nonuse of HAART, even after we controlled for differences in insurance status and other population characteristics such as having a usual source of medical care. For Hispanic women, the higher unadjusted risk of not using HAART did not persist after we controlled for population differences. Nonetheless, the latter finding warrants deeper investigation to identify the specific population characteristics that might be contributing to this elevated unadjusted risk. With clear evidence that HAART use slows the progression of HIV disease and reduces HIV-related mortality, improving our understanding of the factors associated with the continuing disparity is critically important.
Although there was no evidence that race/ethnicity and insurance coverage interact in the way hypothesized to increase risk of HAART nonuse, we found compelling evidence that lack of insurance was associated with a higher risk of not using HAART. This finding held true for women of all 3 racial/ethnic groups. Moreover, among women with similar insurance and other characteristics, being enrolled in the AIDS Drug Assistance Program significantly reduced the likelihood of not using HAART. On the basis of this analysis, the AIDS Drug Assistance Program is clearly operating effectively as a safety net for uninsured and underinsured women. Our results on the effects of insurance status are consistent with prior research and analysis,5,7,13 although they differ somewhat from those of previous studies that examined factors associated with HAART use in the WIHS.3,6,14 Possible explanations for differing results are inclusion of both the first and second waves of WIHS enrollees, changes occurring as women age, and use of more refined definitions of insurance coverage in the current analysis.
A large body of research has already demonstrated that having health insurance improves access to care. The results of this study provide evidence that providers of HIV care may consider an individual's insurance status when deciding whether to prescribe medications. It is also conceivable that providers do not consider insurance status when prescribing medications, but that women who are uninsured are unable to obtain the medications. For this reason, future studies on access to HIV medical care would benefit from assessments of insurance coverage that use comparable definitions to facilitate comparisons across studies and better understand barriers to treatment.
An unexpected finding in this study was that women with public insurance were more likely to use HAART than those with private insurance. Several possible explanations for this finding could be explored in future studies; these include the comprehensiveness of the private insurance coverage (e.g., copayments and deductibles) and resources at the site of care of the privately insured (e.g., HIV experience level of physicians, support services available to assist women in navigating the health system).
Unlike in prior research, including a recent analysis of this same cohort,15 use of illicit drugs was not associated with nonuse of HAART, but alcohol use was. This finding should be interpreted with caution since some individuals may use both alcohol and illicit drugs. It may be that the effects of illicit drug use in previous studies resulted from measures of drug use that served as a proxy for co-occurring but unmeasured alcohol use. The current findings provide evidence that analysis of the impact of substance abuse should include use of alcohol as well as types of illicit drugs. Because behaviors involving the use of alcohol and other drugs often have similar origins and consequences, determining which behavior represents the true risk may be less important than determining how to reduce the chances that either behavior results in underuse of HIV medications.
It will be especially important to determine if the link between alcohol use and not taking HAART is a result of provider behavior, patient behavior, or some combination of the two. Previous research suggests that physicians may be less aggressive in prescribing HIV medications when a patient has a history of substance abuse and that patients with substance abuse problems may be less likely to seek medical care or follow a prescribed regimen.16 Because one third of the women not taking HAART reported that their physician did not prescribe it, this study provides evidence of the need to better understand the decisions made by physicians, especially when a women is either uninsured or has a substance abuse problem. Although a survey of infectious disease physicians reported that most physicians follow guidelines for prescribing HAART,17,18 a patient's history of alcohol or other drug use may consciously or unconsciously influence clinical decision making.19
There was also fairly robust evidence that having depressive symptoms was associated with elevated risk of HAART nonuse. The elevation in odds reached statistical significance when women's usual source of care was included in the model. The magnitude of the effect was quite stable across all specifications of the model, suggesting that this effect is real and not an artifact of model specification. The finding supports previous research15 reporting that mental health status and access to mental health services and treatment are important components of comprehensive HIV care.
In summary, our results demonstrate that disparities in HIV care by race/ethnicity persist among women living with HIV/AIDS. These results have important policy implications. Concerted efforts to address disparities in HIV care are warranted. They also provide evidence that efforts to expand health insurance coverage would likely improve access to HIV medications for all women, and that it is important to develop more effective ways of intervening with women who have alcohol or other drug problems. Because the WIHS cohort is considered to be representative only of women in the cities where participants were recruited—and at the time they were recruited—these findings are not necessarily generalizable to all women in the United States with HIV infection. However, the persistence of disparities in use of HAART between African American and White women in this longitudinal cohort study is one more indication of the need for a clearer understanding of the causal factors that lead to this disparity. It also suggests that it is time to identify evidence-based interventions to improve access and eliminate less-than-optimal HAART use and HIV care.
Acknowledgments
The Women's Interagency HIV Study (WIHS) is funded by the National Institute of Allergy and Infectious Diseases (UO1-AI-35004, UO1-AI-31834, UO1-AI-34994, UO1-AI-34989, UO1-AI-34993, and UO1-AI-42590) and the National Institute of Child Health and Human Development (UO1-HD-32632). The WIHS is cofunded by the National Institute on Drug Abuse, the National Cancer Institute, and the National Institute on Deafness and Other Communication Disorders. Funding is also provided by the National Center for Research Resources (UCSF-CTSI grant UL1 RR024131). The National Institute on Drug Abuse provided primary funding for our study.
Data in this article were collected by the WIHS Collaborative Study Group with centers (principal investigators) at New York City/Bronx Consortium (Kathryn Anastos); Brooklyn, NY (Howard Minkoff); Washington, DC, Metropolitan Consortium (Mary Young); The Connie Wofsy Study Consortium of Northern California (Ruth Greenblatt); Los Angeles County/Southern California Consortium (Alexandra Levine); Chicago Consortium (Mardge Cohen); and Data Coordinating Center (Stephen Gange). We acknowledge Richard Hopely for his responsiveness and meticulous computer programming throughout this project and thank Alejandra Martin for her support as a research assistant. Finally, and most importantly, we gratefully acknowledge the women who participated in the WIHS.
Note. The contents of this article are solely the responsibility of the authors and do not necessarily represent the official views of the National Institutes of Health.
Human Participant Protection
This study was approved by the institutional review boards of the respective universities of the 3 lead coauthors (George Washington University, Massachusetts General Hospital, and Wake Forest University School of Medicine). The WIHS principal investigators obtained institutional review board approval at each of their collaborating institutions.
References
- 1.Palella FJ, Delaney KM, Moorman AC, et al. Declining morbidity and mortality among patients with advanced human immunodeficiency virus infection. N Engl J Med 1998;338(13):853–860 [DOI] [PubMed] [Google Scholar]
- 2.Levine RS, Briggs NC, Kilbourne BS, et al. Black–White mortality from HIV in the United States before and after introduction of highly active antiretroviral therapy in 1996. Am J Public Health 2007;97(10):1884–1892 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Cohen MH, Cook JA, Grey DD, et al. Medically eligible women who do not use HAART: the importance of abuse, drug use, and race. Am J Public Health 2004;94(7):1147–1151 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Shapiro MF, Morton SC, McCaffrey D, et al. Variations in the care of HIV-infected adults in the United States. JAMA 1999;281(24):2305–2315 [DOI] [PubMed] [Google Scholar]
- 5.Cunningham WE, Mardson LW, Andersen RM, et al. Prevalence and predictors of highly active antiretroviral therapy use in patients with HIV infection in the United States. J Acquir Immune Defic Syndr 2000;25(2):115–123 [DOI] [PubMed] [Google Scholar]
- 6.Cook JA, Cohen MH, Grey D, et al. Use of highly active antiretroviral therapy in a cohort of HIV-seropositive women. Am J Public Health 2002;92(1):82–87 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Keruly J, Convisor R, Moore R. Association of medical insurance with receipt of antiretroviral therapy. Am J Public Health 2002;92(5):852–857 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Barkan SE, Melnick SL, Preston-Martin S, et al. The Women's Interagency HIV Study. Epidemiology 1998;9(2):117–125 [PubMed] [Google Scholar]
- 9.Bacon MC, von Wyl V, Alden C, et al. The Women's Interagency HIV Study: an observational cohort brings clinical sciences to the bench. Clin Vaccine Immunol 2005;12(9):1013–1019 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Radloff LS. The CES-D Scale: a self-report depression scale for research in the general population. Appl Psychol Meas 1977;1(3):385–401 [Google Scholar]
- 11.Dufour M. What is moderate drinking? Defining “drinks” and “drinking levels.” National Institute for Alcohol Use and Alcoholism. Alcohol Res Health 1999;23(1):5–14 [PMC free article] [PubMed] [Google Scholar]
- 12.Kaiser Commission on Medicaid and the Uninsured The Uninsured: A Primer Washington, DC: Henry J. Kaiser Family Foundation; October 2008:32 [Google Scholar]
- 13.Kahn JG, Haile B, Kates J, Chang S. Health and federal budgetary effects of increasing access to antiretroviral medications for HIV by expanding Medicaid. Am J Public Health 2001;91(9):1464–1473 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Burke-Miller JK, Cook JA, Cohen MH, et al. Longitudinal relationships between use of highly active antiretroviral therapy and satisfaction with care among women living with HIV/AIDS. Am J Public Health 2006;96(6):1044–1051 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Cook JA, Grey DD, Burke-Miller JK, et al. Illicit drug use, depression, and their association with highly active antiretroviral therapy in HIV-positive women. Drug Alcohol Depend 2007;89:74–81 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Gerbert B, Bronstone A, Clanon K, et al. Combination antiretroviral therapy: health care providers confront emerging dilemmas. AIDS Care 2000;12(4):409–421 [DOI] [PubMed] [Google Scholar]
- 17.Bogart LM, Catz SL, Kelly JA, Benotsch EG. Factors influencing physicians' judgments of adherence and treatment decisions for patients with HIV disease. Med Decis Making 2001;21(1):28–36 [DOI] [PubMed] [Google Scholar]
- 18.Stone VE, Mansourati FF, Poses RM, Mayer KH. Relation of physician specialty and HIV/AIDS experience to choice of guideline recommended antiretroviral therapy. J Gen Intern Med 2001;16:360–368 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Bogart LM, Kelly JA, Catz SL, et al. Impact of medical and non-medical factors on physician decision making for HIV/AIDS antiretroviral treatment. J Acquir Immune Defic Syndr 2000;23:396–404 [DOI] [PubMed] [Google Scholar]