Abstract
Purpose of review
Our understanding of the regulation of mineral ion homeostasis is rather stagnant, and until recently the regulation of phosphate homeostasis was thought to be a passive process mediated largely by the well known calciotrophic hormones PTH and 1,25(OH)2D3. This article summarizes the emerging trends that i) show an active regulation of phosphate homeostasis by FGF-23, a process that appears to be fairly independent of calcium homeostasis, and ii) how altered mineral ion metabolism might affect the aging process.
Recent findings
A major breakthrough in FGF-23 biology has been achieved by the demonstration of strikingly similar physical and biochemical phenotypes of Fgf-23 knockout and klotho hypomorph mice, which eventually led to the identification of klotho as a cofactor in FGF-23 and its receptor interactions. A new regulatory pathway has been defined, where FGF23, in presence of klotho has shown to activate downstream signaling events, by phosphorylation of FGF receptor substrate-2α, ERK, and Egr-1. Furthermore, FGF-23 has emerged as a counter regulatory hormone that influences 1α(OH)ase and NaPi2a activities in the kidney to regulate phosphate homeostasis. Finally, studies also point towards a role of DMP1 in influencing the regulation of phosphate homeostasis, in coordination with FGF-23.
Summary
Recent in vivo mouse genetic studies have expanded our understanding of the biochemical and molecular pathways involved in phosphate homeostasis, and linked FGF-23 to the genesis of such regulation. A clear understanding of the molecular interactions of essential calcium and phosphate regulating factors will enhance our understanding of the coordinated regulation of mineral ion metabolism, and will help us to redefine the molecular pathology of age-associated lesions accompanied by abnormal mineral ion metabolism, that include but are not limited to vascular calcifications, and osteoporosis.
Keywords: Fibroblast growth factor 23, Klotho, Vitamin-D, Mineral ion homeostasis, Ageing
Introduction
Maintaining normal calcium and phosphate homeostasis is crucial for various essential biological activities that include but are not limited to energy metabolism, signaling activities, and normal skeletal growth, development and function; altered mineral metabolism can affect the functionality of almost any tissue or organ system. In spite of its wide biological importance and significance to maintain normal physiologic functions, it is not yet clearly understood how normal mineral ion homeostasis is coordinately regulated. Identification of fibroblast growth factor-23 (FGF-23), as a “phosphatonin” in the year 2000 has significantly enhanced our understanding of mineral metabolism [1,2]. A major breakthrough of how FGF-23 exerts its bioactivities has been achieved by the recent demonstration of strikingly similar physical and biochemical phenotypes of Fgf-23 knockout and klotho hypomorph mice [3] which helped in the identification of klotho as a cofactor in FGF-23 and its receptor interactions [4,5].
Though much progress has been made in recent years in terms of identification of the mineral ion regulating molecules [6–11], it is not yet clear how they interact with each other to coordinately regulate mineral ion homeostasis. For instance, it is presumed that proximal tubules are the most likely site where FGF-23 could exert its bioactivities to regulate and maintain phosphate homeostasis, but the exact mode of action and interaction of FGF-23 with other calcium and phosphate regulating molecules in the kidney is not yet clear. The autocrine, paracrine, or endocrine functions of FGF-23, and how it interacts or influences molecules that are also involved in maintaining mineral ion homeostasis including transient receptor potential cation channel, subfamily V, member 5 (TRPV5), sodium-phosphate co-transporter 2a (NaPi2a), Calbindin28k, Na+/Ca2+-exchanger (NCX1), and plasma membrane ATPase (PMCA1b) in the kidney requires additional studies [11]. Another important aspect that needs further clarification is the interrelationship among FGF-23, klotho and vitamin-D [12].
Fibroblast growth factor 23
FGF-23 is a 30 kDa-secreted protein that is processed by a pro-convertase type enzyme into two smaller fragments of approximately 18 kDa (amino fragment) and 12 kDa (carboxy fragment); the exact functions of these fragments are not clear, and of intense focus of research. FGF-23 is mainly produced in bone by osteocytes [13]. Although the in vivo phosphaturic effect of the full-length synthetic FGF-23 protein is well-documented, the precise in vivo role of C-terminal and N-terminal fragments of FGF-23 needs additional studies [14]. Since the canonical FGF receptor (FGFR) binding domain is not present in C-terminal fragments of FGF-23, any in vivo activity by this fragment would suggest the existence of a novel receptor, in addition to the known classic FGF receptor signaling pathway [15].
Altered regulation of FGF-23 has direct relevance to human diseases; gain-of-function mutations of FGF-23 have shown to be associated with autosomal dominant hypophosphatemic rickets (ADHR) [1]; these mutations have been shown to prevent proteolytic cleavage of the FGF-23 protein, with net effect being phosphate wasting and skeletal defects, perhaps due to enhanced biologic activities of FGF-23. Similarly, increased serum level of FGF-23 in patients with oncogenic osteomalacia (OOM) is believed to be the causative factor for tumor-induced phosphate-wasting [16]. Jonsson et al. demonstrated that a markedly elevated serum level of FGF-23 is associated with renal phosphate wasting in patients with OOM. Patients affected by X-linked hypophosphatemia (XLH), which is caused by inactivating mutations of the gene encoding the phosphate regulating gene with homologies to endopeptidases on the X chromosome (PHEX), exhibit increased FGF-23 serum levels leading to phosphate wasting and osteomalacia in these individuals [17]. Recent studies have found the presence of inactivating mutations in the dentin matrix protein 1 (DMP1) gene in patients affected with autosomal recessive hypophosphatemia (ARHP), a rare genetic disorder with essentially similar clinical features as those seen in patients with OOM, XLH and ADHR [18,19]; such clinical similarities are thought to be due to increased circulating intact FGF-23 protein [18,19]. DMP1 belongs to the Small Integrin-Binding Ligand N-linked Glycoprotein (SIBLING) family, and is thought to be involved in osteoblastic/odontoblastic differentiation, expression of osteocalcin, and extracellular mineralization [20,21]. The other members of SIBLING family include bone sialoprotein (BSP), osteopontin, dentin sialophosphoprotein (DSPP) and matrix extracellular phosphoglycoprotein (MEPE). Genetic ablation of Dmp1 in mice results in increased circulating Fgf-23 serum levels, possibly due to overexpression of the Fgf-23 gene by osteocytes [19]. It is, therefore, likely that the clinical features in patients with ARHP and the phenotypes of Dmp1 null mice are due to increased activity of FGF-23. Phosphate wasting and skeletal mineral deposition defects are also the two main phenotypes of FGF-23 transgenic mice [22–24], with close resemblance to the symptoms described in patients with XLH, OOM, ADHR and ARHP.
In contrast to the transgenic animals, the phenotype of Fgf-23 null animals mimics patients with familial tumoral calcinosis (FTC), a human disorder characterized by ectopic calcifications and elevated serum levels of phosphate due to loss-of-function mutations in the FGF-23 gene [25,26]. Recently missense mutations in the gene encoding the glycosyltransferase polypeptide GalNAc-T3, which is involved in initiation of O-glycosylation, have shown to be associated with hyperostosis-hyperphosphatemia syndrome (HHS) and FTC [27,28]. Both FTC and HHS are autosomal recessive disorders characterized by unusually normal or elevated serum levels of vitamin-D, hyperphosphatemia, and ectopic calcifications. The fact that two different genes can cause the same human disease suggests a possible role for GalNAc-T3-mediated glycosylation in controlling FGF-23 activity. Studies have shown that the secretion of FGF-23 is indeed dependent on O-glycosylation, as GalNAc-T3 can glycosylate the subtilisin-like proprotein convertase (SPC) signal sequence of FGF-23 at Thr178 [29].
Interestingly, the phenotypes of Fgf-23 knockout mice [3] that include but are not limited to infertility, kyphosis, atherosclerosis, skin atrophy, muscle wasting, T-cell dysregulation, pulmonary emphysema, altered mineral ion metabolism, rickets, and shortened lifespan are essentially very similar to the phenotypes of klotho ablated mice [30,31], and such observations in Fgf-23 null mice have facilitated the identification of a novel FGF-23 signaling pathway that also involves klotho.
FGF-23 and receptor interaction
FGF-23 is a distinct member of FGF family and contains a pro-convertase processing site. Unlike other members of the FGF family, whether FGF-23 also needs heparin-like molecules to activate the fibroblast growth factor receptor (FGFR) system is an ongoing area of research [15]; but FGF-23, in presence of klotho could activate downstream signaling molecules, as determined by activation or phosphorylation of FGF receptor substrate-2a, extracellular signal-regulated kinase (ERK) and early growth response element-1 (Egr-1) [32]; it has been shown that cells exposed to FGF-23 underwent ERK phosphorylation and increased their abundance of Egr-1 protein only after transfection with klotho [4,5]. The full length and/or the extracellular domain of the klotho protein could bind to various FGFRs [5] which have signal-transducing extracellular ligand-binding domains and an intracellular tyrosine kinase domain.
The klotho gene encodes a single-pass transmembrane protein; the extracellular domain of Klotho protein consists of two homologous domains that share sequence homology to the β-glucosidase of bacteria and plants. The klotho extracellular domain does not directly bind to FGF-23, but it enhances FGF-23 binding to its receptor complex with much higher affinity than to FGF receptor alone, implicating klotho as a cofactor in FGF23-FGFR interaction and subsequent signaling [5]. Urakawa et al. from their experiments claimed that only FGFR1(IIIc), in combination with klotho, could induce significant FGF23 signaling, while basic FGF, a universal ligand for FGFRs could generate downstream signaling without klotho, therefore speculating a possibility of klotho to selectively convert FGFR1(IIIc) into a specific FGF23 receptor [4]. Our understanding of FGF-23 and its receptor interactions will pave the way to determine downstream FGF-23 signaling events, identify the FGF-23 responsive genes and, more importantly their collective functions in the regulation of mineral ion metabolism, and their yet to be clarified functions in the aging process.
Possible role of FGF-23 in the premature aging of klotho mutant mice
Aging is a complex biological process that includes multi-organ, multi-system pathologies [33–36]. Suitable mammalian models for aging with a wide range of age-associated pathologies are desirable to study molecular mechanisms of human aging. Klotho mutant mice have shown to generate multiple premature aging-like features, including shortened lifespan, impaired sexual maturation leading to infertility, kyphosis, atherosclerosis, extensive soft tissue calcifications, skin atrophy, muscles wasting, T-cell dysregulation, pulmonary emphysema, osteopenia, abnormal mineral ion metabolism, and impaired vitamin-D homeostasis; the inactivation of the gene that caused such extensive premature aging-like features was perceived as a novel aging gene, and was named klotho, after one of the three Fates who spins the thread of life [30,31]. However, recent studies suggest that premature aging-like features in klotho mutant mice are not the primary cause of klotho inactivation but rather the consequence of altered mineral metabolism due to lack of Fgf-23 activity in these mice [37]. Despite extremely high serum levels of Fgf-23 (about 2,000 fold higher) in klotho ablated mice, Fgf-23 is unable to induce phosphaturia in these animals [4]. Furthermore, deletion of Fgf-23, a molecule that is structurally different from klotho could induce identical phenotypes, as found in the klotho ablated mice [12]. It is, therefore, obvious that the strikingly similar physical, biochemical and morphological phenotypes of these mice, are either due to absence (Fgf-23 null mice) or inability (klotho mutant mice) of Fgf-23 to exert its bioactivities [38]. Yet again, the underlying mechanisms of premature aging-like features of the klotho mutants are due to inability of Fgf-23 to exert its function in absence of klotho that leads to hypervitaminosis-D and altered mineral metabolism. That raises a very important question: if premature aging-like features and short lifespan of klotho null mice are due to the consequences of Fgf-23 inactivity, and not due to direct effects of inactivation of klotho, then how the lifespan of klotho transgenic mice are greatly increased?
How factors regulating mineral ion metabolism affect aging?
The roles of the factors that regulate mineral ion metabolism and affect aging need careful long-term studies. One of the mineral ion regulating molecules that has get particular attention in affecting aging process is vitamin-D; low levels of vitamin-D, that range from chronic hypovitaminosis, insufficiency to deficiency in elderly individuals are associated with osteoporosis or gradual loss of bone and thereby making the elderly individuals more vulnerable to fracture-related complications. Despite molecular understanding of vitamin-D synthesis [39], and apparently obvious pathological effects of its deficiency on skeletal mineralization, the randomized clinical trials of vitamin-D supplementation have produced differential outcomes. For instance, prophylaxis supplementation of vitamin-D to the elderly individuals (75 years or older), by providing a yearly intramuscular injection of ergocalciferol (150,000–300,000 IU) for 5 years did not produce any statistical difference, either in terms of occurrence of fractures or in total mortality between vitamin-D treated or untreated individuals [40]. Dawson-Hughes and coworkers [41] also failed to detect reduction in hip fractures in vitamin-D (cholecalciferol) and calcium supplemented elderly patients, although the investigators did find less non-vertebral fracture [41]. In a separate study conducted on 669 postmenopausal women, after adjustment for age, there was no difference in the risk of vertebral and non-vertebral fractures in women with 25-hydroxyvitamin-D level below 75 nmol/l or below 50 nmol/l, compared to women with higher vitamin-D levels; also there were no significant changes in bone mineral density [42]. In a relatively recent study with 36,282 postmenopausal women receiving calcium (daily dose of 1000 mg of calcium carbonate) and vitamin D supplements (daily dose of 400 IU of vitamin D3) or placebo pills showed a modest benefit in preserving bone mass and only prevented hip fractures in certain age groups of women, but did not prevent other types of fractures or colorectal cancer [43]. During the study a fracture rate of 14 per 10,000 cases per year in the supplemented group compared to 16 per 10,000 per year in the placebo group (such reduction was not statistically significant) were noted; moreover, such vitamin-D and calcium supplementation was also associated with an about 17% increased rate of kidney stone formation [43].
Conversely, the uncontrolled consumption of vitamin-D supplements by the elderly individuals (53 to 73 years old) with osteoporosis has shown to induce occult vitamin-D intoxication, and the resultant effect being diminished bone mass; discontinuation of use of dietary supplements resulted in the normalization of serum levels of 25(OH)2D leading to the recovery of the bone mineral density (annual increase of 1.9% ± 0.6%) and the normalization of the ratio of urinary calcium to creatinine [44]; a 3-year follow-up phase showed that the increase in bone mineral density persisted after initial recovery [44].
The observations that hypervitaminosis-D is associated with hypercalciuria and bone loss in the affected patients are comparable to the results obtained in some of the experimental studies with excessive vitamin-D activities; for instance, genetically altered mice that were ablated for the sodium phosphate co-transporters 2a (NaPi2a) have very high serum levels of 1,25(OH)2D3, and exhibit hypercalciuria and skeletal anomalies [45]. Similarly, despite hypervitaminosis-D [46–48], such skeletal changes as osteopenia and/or osteomalacia (one would expect in vitamin-D deficiency state) are found both in Fgf-23 and klotho deficient mice [3,12,13,31,47].
Hypervitaminosis-D and premature aging in Fgf-23 and klotho mutant mice
Both Fgf-23 and klotho deficient mice have increased renal expression of the 1α-hydroxylase [1α(OH)ase] gene, accompanied by significantly elevated serum levels of 1,25(OH)2D3 [13,46–48]; such hypervitaminosis-D was associated with infertility, kyphosis, atherosclerosis, skin atrophy, muscle wasting, T-cell dysregulation, pulmonary emphysema, hyperphosphatemia, rickets, and shortened lifespan in both the mutant mice. A significant rescue of these phenotypes has been achieved either by reducing vitamin-D activities or by genetically ablating vitamin-D activities from Fgf-23 and klotho ablated mice [12,48]. Reducing vitamin-D activities in klotho ablated mice by providing a vitamin-D deficient diet prevented formation of ectopic calcifications, gain of fertility, and most importantly prolonged survival, suggesting that the premature aging-like features in klotho mutant mice are the consequence of increased activity of vitamin-D [48]. In the same line, when vitamin-D activities were genetically ablated from Fgf-23 null mice by deleting the 1α(OH)ase gene, most of the phenotypes in Fgf-23 null mice were either reversed or rescued in Fgf-23−/−/1α(OH)ase−/− compound mutants [12,49]; in these compound mutants, the ectopic calcifications and generalized atrophic changes were rescued. It is, therefore, reasonable to conclude that most of the premature aging-like phenotypes in Fgf-23 and klotho deficient mice are due to altered mineral ion homeostasis partly driven by hypervitaminosis-D; such increased vitamin-D activities are most likely the consequence of lack of activity of its counter regulatory hormone, i.e., Fgf-23 [3,12,50,51].
By reducing vitamin-D activities in klotho or Fgf-23 ablated mice, the hyperphosphatemia was reversed, and the resultant effect being the disappearance of ectopic calcifications, and other premature aging-like features [3,48]. In the same line, both TRPV-5 and NaPi2a knockout mice also have hypervitaminosis-D [11,45], but do not show widespread premature aging-like features, as noted in klotho or Fgf-23 ablated mice, possibly because TRPV-5 and NaPi2a null mice do not develop hyperphosphatemia. It, therefore, needs to be reemphasized that altered mineral ion homeostasis in form of hyperphosphatemia is the most important cause that leads to extensive soft tissue calcifications and other phenotypes of Fgf-23 and klotho deficient mice.
Mechanisms of hyperphosphatemia in Fgf-23 and klotho mutant mice
The sodium-dependent phosphate co-transport system in the kidney is mostly composed of the type 2a and type 2c cotransporters, localized in the apical surface of the proximal tubular epithelial cells; in the same line, type 2b cotransporters are present in the apical membrane of the intestinal epithelial cells [52]. The renal type 2a cotransporters are the major determinant that regulates plasma and urinary phosphate balance. NaPi2a levels in the apical surface of the proximal tubular cells is increased by the activity of 1,25(OH)2D3, and is decreased by the activity of FGF-23, and PTH [52,53]. Similarly, the intestinal phosphate transport activity and NaPi2b levels are upregulated by the activity of 1,25(OH)2D3 [54]. Of relevance, high phosphate diet decreases NaPi2a, and low phosphate diet increases NaPi2a levels.
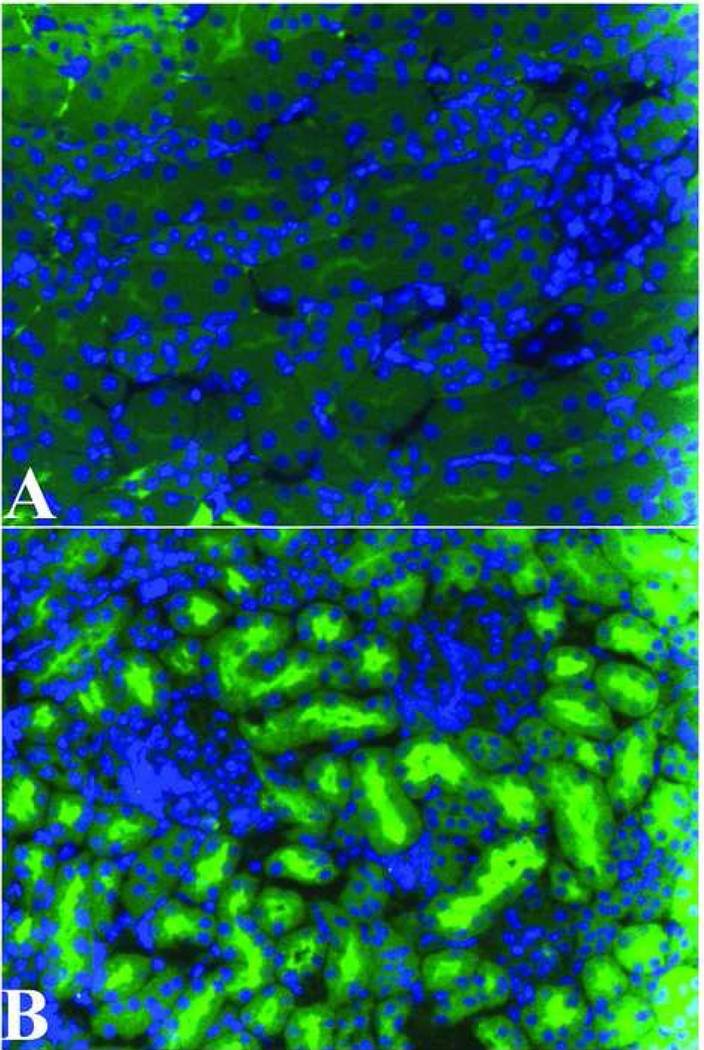
Genomic ablation of the Fgf-23 gene from mice leads to increased renal expression of NaPi2a (Figure-1) [13]; a similar increase in renal expression of NaPi2a was also found in klotho mutant mice [55]. It is mostly believed that increased activity of NaPi2a leads to increased reuptake of phosphate, leading to hyperphosphatemia that is consistently noted in these mutant mice. Low level of PTH is likely to facilitate apical presence of NaPi2a in both Fgf-23 and klotho mutant mice, and thereby increased reabsorption of phosphate. Recent studies have provided genetic evidence to show that the upregulation of NaPi2a in Fgf-23−/− mice is not an epiphenomenon; ablation of NaPi2a from Fgf-23−/− mice reversed hypersphosphatemia to hypophosphatemia by 6 weeks of age in NaPi2a−/−/Fgf-23−/− mice, and thereby providing a genetic evidence of role of NaPi2a in regulating renal phosphate homeostasis in Fgf-23−/− mice [13]. Similar studies will determine whether analogous phenomenon is also present in klotho mutant mice or not.
Figure-1.
Immunolocalization of NaPi2a in control (A) and Fgf-23 null mice kidney (B). Note a markedly increased expression of NaPi2a in the luminal side of the proximal tubular epithelial cells of Fgf-23 null mice (B). Increased expression of NaPi2a causes increased renal uptake of phosphate, leading to hyperphosphatemia in Fgf-23 null mice.
Clinical relevance of in vivo experimental mouse studies
From the experimental studies, it is reasonable to speculate that hypervitaminosis-D, in a hyperphosphatemic microenvironment, could facilitate induction of certain pathologic changes, including soft tissue and vascular calcifications that are mostly noted in the elderly population. A phenomenon appears to be very similar to the adverse effects of long-term use of active vitamin-D metabolites in patients with chronic kidney disease (CKD) with hyperphosphatemia; such treatment could facilitate abnormal calcification to increase the risk of cardiovascular death of CKD patients. Although the etiological diversity, along with multi-stage, multi-factorial events of CKD [56–58] make it clinically difficult to pinpoint one single risk factor, studies have suggested that excessive vitamin-D contribute to risk of increased serum accumulation of calcium, and incidence of calcification, which is associated with reduced survival and morbidity [59,60]. Abnormal tissue calcification is associated with almost half of the cardiovascular deaths among patients undergoing dialysis. Furthermore, continuous use of high calcium dialysate and prolonged administration of vitamin-D are the main underlying cause of tumoral calcinosis in patients with chronic renal failure [61]. Milliner et al. found that the probability of calcinosis was higher in patients receiving vitamin-D therapy [59], and withdrawal of vitamin-D therapy from the patients with tumoral calcinosis could markedly regress the lesion [62], emphasizing that reducing vitamin-D could ameliorate ectopic calcification. It is, however, necessary to mention that in an observational study with 242 patients undergoing hemodialysis, treatment with the vitamin-D analog (alfacalcidol) resulted in a significantly lower number of cardiovascular death when compared to the untreated group of patients [63]. Analyzing available information, the survival benefits and risk of vitamin-D therapy to CKD patients are not clear and an extremely debatable issue [64–66], although the direct impact of vitamin-D on mineral metabolism and calcification is beyond any doubt.
Even though the vitamin-D induced calcification in the disease state might not be comparable to the natural aging, there might be, however, similarities in the underlying mechanisms [67], as molecules involved in the mineral ion metabolism in normal and disease state are similar and a selective group of genes.
Conclusion
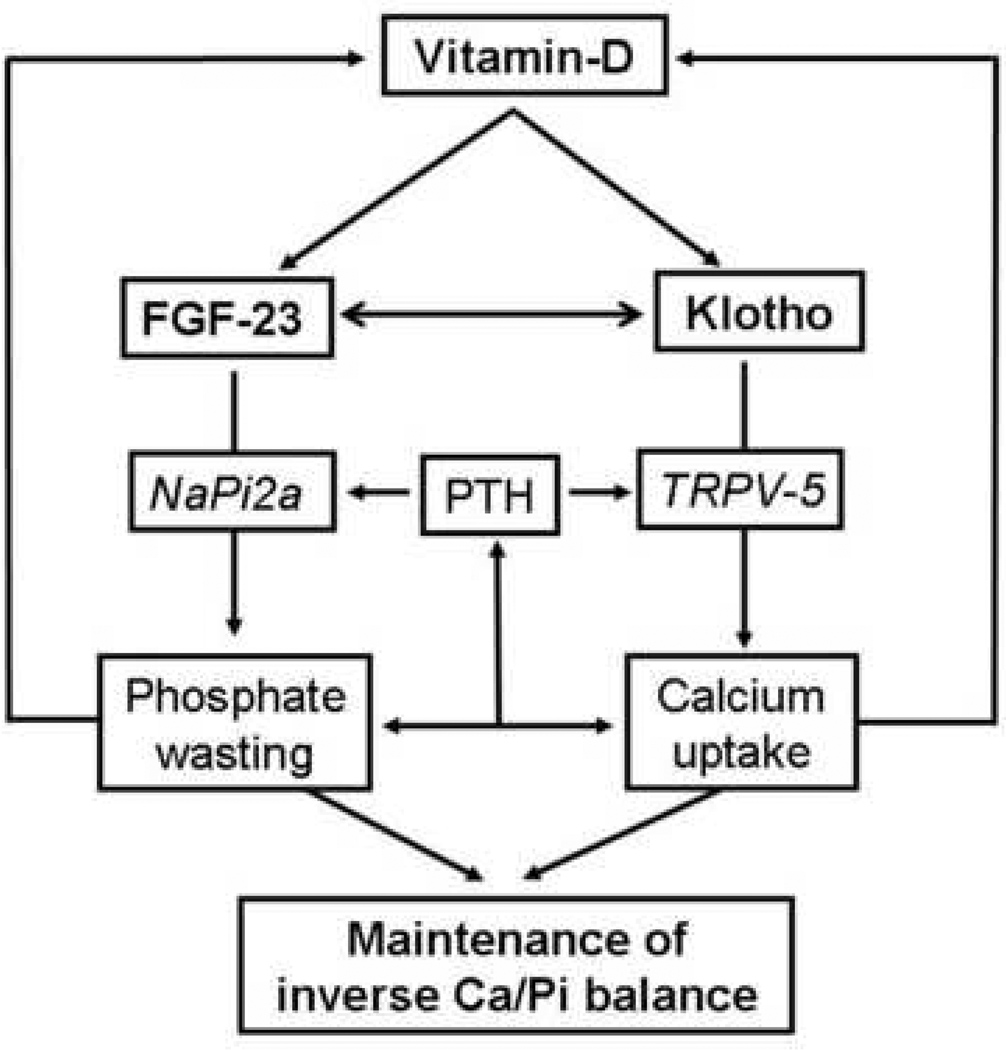
In this brief article, based on recent findings, we have presented our views on effects of altered mineral ion metabolism in generating features that are more likely to be present during aging. We also discussed why we believe that premature aging-like features of klotho mutant mice are actually due to the inability of Fgf-23 to exert its function in these mice. Moreover, lack of Fgf-23 activity in Fgf-23 and klotho mutant mice eliminates the physiologic counter regulation of Fgf-23 and vitamin-D, leading to hypervitaminosis-D and hyperphosphatemia in these mutants and consequently induces most of the premature aging-like features. FGF-23, by affecting the activities of vitamin-D and altering mineral ion homeostasis might play a major role in the aging process that include but are not limited to senile osteoporosis and vascular calcifications. Finally, in this article, we wanted to highlight two important aspects related to aging: 1) can factors regulating mineral ion homeostasis affect the aging process? The in vivo results of Fgf-23 and klotho mutant mice clearly suggest such possibilities; that raises another important question 2) is altered mineral ion metabolism a cause or a consequence of the aging process? The existing observations suggest that some of the age-associated pathologies are actually caused by altered mineral ion metabolism. Further in vivo studies will explain how factors coordinately maintain normal mineral ion homeostasis (Figure-2); at this stage, FGF-23 appears to be a very specific messenger that is produced in bone and conveys signals from the bone to the kidney and possibly to the parathyroid gland to regulate mineral metabolism. Our understanding of the physiologic regulation of mineral ion homeostasis will help us to explain how altered regulation of factors controlling mineral ion homeostasis could adversely affect the aging process.
Figure-2.
Simplified schematic diagram of renal regulation of calcium (Ca) and phosphate (Pi) homeostasis. Vitamin-D could exert stimulatory effects on klotho, FGF-23 and TRPV-5 [48,68,69]; TRPV-5 could induce renal calcium uptake through involving calbindin-D28k [70], while, FGF-23 could induce renal phosphate wasting through influencing the renal NaPi system [13,71], and thereby maintaining physiologic inverse Ca/Pi balance. Serum level of Ca/Pi has direct and indirect feedback through PTH on vitamin-D activities. Klotho by influencing biological activities of both TRPV-5 [72] and FGF-23 [4] could delicately fine tune the physiologic balance of Ca/Pi. There are other molecules that play important roles in regulation of Ca/Pi homeostasis, but to keep the diagram simple, we just cited the most essential factors.
Acknowledgements
We apologize to the authors whose original works could not be cited due to space limitation.
Abbreviations
- 1α(OH)ase
1α-hydroxylase
- ADHR
Autosomal dominant hypophosphatemic rickets
- ARHP
autosomal recessive hypophosphatemia
- CKD
Chronic kidney disease
- DMP1
Dentine matrix protein 1
- Egr-1
Early growth response element-1
- ERK
Extracellular signal-regulated kinase
- FGF
Fibroblast growth factor
- FGFR
Fibroblast growth factor receptor
- FTC
Familial tumoral calcinosis
- HHS
Hyperostosis-hyperphosphatemia syndrome
- NaPi
Sodium-phosphate cotransporter
- OOM
Oncogenic osteomalacia
- SIBLING
Small Integrin-Binding Ligand N-linked Glycoprotein
- TRPV-5
Transient receptor potential cation channel, subfamily V, member 5
- XLH
X-linked hypophosphatemia
References
- 1.ADHR_Consortium: Autosomal dominant hypophosphataemic rickets is associated with mutations in FGF23. The ADHR Consortium. Nat Genet. 2000;26:345–348. doi: 10.1038/81664. [DOI] [PubMed] [Google Scholar]
- 2.Yamashita T, Yoshioka M, Itoh N. Identification of a novel fibroblast growth factor, FGF-23, preferentially expressed in the ventrolateral thalamic nucleus of the brain. Biochem Biophys Res Commun. 2000;277:494–498. doi: 10.1006/bbrc.2000.3696. [DOI] [PubMed] [Google Scholar]
- 3. Razzaque MS, Sitara D, Taguchi T, St-Arnaud R, Lanske B. Premature ageing-like phenotype in fibroblast growth factor 23 null mice is a vitamin-D mediated process. FASEB J. 2006;20:720–722. doi: 10.1096/fj.05-5432fje. This is the one of the earliest reports suggesting strikingly similar physical, biochemical and morphological phenotypes of klotho and Fgf-23 ablated mice; based on preliminary observations the authors speculated an existence of a common hormonal signaling cascade for klotho and FGF-23, which was scientifically validated by subsequent studies.
- 4. Urakawa I, Yamazaki Y, Shimada T, Iijima K, Hasegawa H, Okawa K, Fujita T, Fukumoto S, Yamashita T. Klotho converts canonical FGF receptor into a specific receptor for FGF23. Nature. 2006;444:770–774. doi: 10.1038/nature05315. A role of klotho in FGF-23 and its receptor interaction has been demonstrated.
- 5.Kuro-o M. Klotho as a regulator of fibroblast growth factor signaling and phosphate/calcium metabolism. Curr Opin Nephrol Hypertens. 2006;15:437–441. doi: 10.1097/01.mnh.0000232885.81142.83. [DOI] [PubMed] [Google Scholar]
- 6.Dunstan CR, Zhou H, Seibel MJ. Fibroblast growth factor 23: a phosphatonin regulating phosphate homeostasis? Endocrinology. 2004;145:3084–3086. doi: 10.1210/en.2004-0354. [DOI] [PubMed] [Google Scholar]
- 7.Yu X, White KE. Fibroblast growth factor 23 and its receptors. Ther Apher Dial. 2005;9:308–312. doi: 10.1111/j.1744-9987.2005.00287.x. [DOI] [PubMed] [Google Scholar]
- 8.Yamashita T. Structural and biochemical properties of fibroblast growth factor 23. Ther Apher Dial. 2005;9:313–318. doi: 10.1111/j.1744-9987.2005.00288.x. [DOI] [PubMed] [Google Scholar]
- 9.Kazama JJ, Gejyo F, Shigematsu T, Fukagawa M. Role of circulating fibroblast growth factor 23 in the development of secondary hyperparathyroidism. Ther Apher Dial. 2005;9:328–330. doi: 10.1111/j.1744-9987.2005.00291.x. [DOI] [PubMed] [Google Scholar]
- 10.Fukumoto S. Post-translational modification of Fibroblast Growth Factor 23. Ther Apher Dial. 2005;9:319–322. doi: 10.1111/j.1744-9987.2005.00289.x. [DOI] [PubMed] [Google Scholar]
- 11.Hoenderop JG, Nilius B, Bindels RJ. Calcium absorption across epithelia. Physiol Rev. 2006;85:373–422. doi: 10.1152/physrev.00003.2004. [DOI] [PubMed] [Google Scholar]
- 12. Razzaque MS, Lanske B. Hypervitaminosis D and premature aging: lessons learned from Fgf23 and Klotho mutant mice. Trends Mol Med. 2006;12:298–305. doi: 10.1016/j.molmed.2006.05.002. This timely review article clearly explained the pathologic role of vitamin-D in producing premature aging-like features in both klotho and Fgf-23 ablated mice, and suggested an existence of a common signaling cascade for both klotho and FGF-23.
- 13. Sitara D, Razzaque MS, St-Arnaud R, Huang W, Taguchi T, Erben RG, Lanske B. Genetic ablation of vitamin D activation pathway reverses biochemical and skeletal anomalies in Fgf-23-null animals. Am J Pathol. 2006;169:2161–2170. doi: 10.2353/ajpath.2006.060329. This article showed that the skeletal anomalies in Fgf-23 null mice were due to increased activities of vitamin-D, and genetic ablation of vitamin-D activities could reverse such skeletal changes.
- 14.Shimada T, Muto T, Urakawa I, Yoneya T, Yamazaki Y, Okawa K, Takeuchi Y, Fujita T, Fukumoto S, Yamashita T. Mutant FGF-23 responsible for autosomal dominant hypophosphatemic rickets is resistant to proteolytic cleavage and causes hypophosphatemia in vivo. Endocrinology. 2002;143:3179–3182. doi: 10.1210/endo.143.8.8795. [DOI] [PubMed] [Google Scholar]
- 15. Yu X, Ibrahimi OA, Goetz R, Zhang F, Davis SI, Garringer HJ, Linhardt RJ, Ornitz DM, Mohammadi M, White KE. Analysis of the biochemical mechanisms for the endocrine actions of fibroblast growth factor-23. Endocrinology. 2005;146:4647–4656. doi: 10.1210/en.2005-0670. FGF-23 is shown to bind with classic FGF receptors with modest affinity; a role of heparin or glycosaminoglycan has been proposed.
- 16.Shimada T, Mizutani S, Muto T, Yoneya T, Hino R, Takeda S, Takeuchi Y, Fujita T, Fukumoto S, Yamashita T. Cloning and characterization of FGF23 as a causative factor of tumor-induced osteomalacia. Proc Natl Acad Sci U S A. 2001;98:6500–6505. doi: 10.1073/pnas.101545198. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Jonsson KB, Zahradnik R, Larsson T, White KE, Sugimoto T, Imanishi Y, Yamamoto T, Hampson G, Koshiyama H, Ljunggren O, et al. Fibroblast growth factor 23 in oncogenic osteomalacia and X-linked hypophosphatemia. N Engl J Med. 2003;348:1656–1663. doi: 10.1056/NEJMoa020881. [DOI] [PubMed] [Google Scholar]
- 18. Lorenz-Depiereux B, Bastepe M, Benet-Pages A, Amyere M, Wagenstaller J, Muller-Barth U, Badenhoop K, Kaiser SM, Rittmaster RS, Shlossberg AH, et al. DMP1 mutations in autosomal recessive hypophosphatemia implicate a bone matrix protein in the regulation of phosphate homeostasis. Nat Genet. 2006;38:1248–1250. doi: 10.1038/ng1868. This study performed a genome-wide linkage analysis using SNP array genotyping in three multiplex families, and identified a homozygous defect in the DMP1 gene as a cause of autosomal recessive hypophosphatemia (ARHP).
- 19. Feng JQ, Ward LM, Liu S, Lu Y, Xie Y, Yuan B, Yu X, Rauch F, Davis SI, Zhang S, et al. Loss of DMP1 causes rickets and osteomalacia and identifies a role for osteocytes in mineral metabolism. Nat Genet. 2006;38:1310–1315. doi: 10.1038/ng1905. This study also found DMP1 mutations in patients with ARHP, and showed that some of the features of Dmp1-knockout mice mimic clinical symptoms of ARHP.
- 20.Tartaix PH, Doulaverakis M, George A, Fisher LW, Butler WT, Qin C, Salih E, Tan M, Fujimoto Y, Spevak L, et al. In vitro effects of dentin matrix protein-1 on hydroxyapatite formation provide insights into in vivo functions. J Biol Chem. 2004;279:18115–18120. doi: 10.1074/jbc.M314114200. [DOI] [PubMed] [Google Scholar]
- 21.Narayanan K, Ramachandran A, Hao J, He G, Park KW, Cho M, George A. Dual functional roles of dentin matrix protein 1. Implications in biomineralization and gene transcription by activation of intracellular Ca2+ store. J Biol Chem. 2003;278:17500–17508. doi: 10.1074/jbc.M212700200. [DOI] [PubMed] [Google Scholar]
- 22.Bai X, Miao D, Li J, Goltzman D, Karaplis AC. Transgenic Mice Overexpressing Human Fibroblast Growth Factor 23(R176Q) Delineate a Putative Role for Parathyroid Hormone in Renal Phosphate Wasting Disorders. Endocrinology. 2004;145:5269–5279. doi: 10.1210/en.2004-0233. [DOI] [PubMed] [Google Scholar]
- 23.Larsson T, Marsell R, Schipani E, Ohlsson C, Ljunggren O, Tenenhouse HS, Juppner H, Jonsson KB. Transgenic mice expressing fibroblast growth factor 23 under the control of the alpha1(I) collagen promoter exhibit growth retardation, osteomalacia, and disturbed phosphate homeostasis. Endocrinology. 2004;145:3087–3094. doi: 10.1210/en.2003-1768. [DOI] [PubMed] [Google Scholar]
- 24.Shimada T, Urakawa I, Yamazaki Y, Hasegawa H, Hino R, Yoneya T, Takeuchi Y, Fujita T, Fukumoto S, Yamashita T. FGF-23 transgenic mice demonstrate hypophosphatemic rickets with reduced expression of sodium phosphate cotransporter type IIa. Biochem Biophys Res Commun. 2004;314:409–414. doi: 10.1016/j.bbrc.2003.12.102. [DOI] [PubMed] [Google Scholar]
- 25.Benet-Pages A, Orlik P, Strom TM, Lorenz-Depiereux B. An FGF23 missense mutation causes familial tumoral calcinosis with hyperphosphatemia. Hum Mol Genet. 2005;14:385–390. doi: 10.1093/hmg/ddi034. [DOI] [PubMed] [Google Scholar]
- 26. Frishberg Y, Ito N, Rinat C, Yamazaki Y, Feinstein S, Urakawa I, Navon-Elkan P, Becker-Cohen R, Yamashita T, Araya K, et al. Hyperostosis-hyperphosphatemia syndrome: a congenital disorder of o-glycosylation associated with augmented processing of fibroblast growth factor 23. J Bone Miner Res. 2007;22:235–242. doi: 10.1359/jbmr.061105. Impaired glycosylation of FGF-23 due to mutations in GALNT3 was suggested to be the cause of hyperostosis-hyperphosphatemia syndrome (HHS), an autosomal recessive disease, with severe hyperphosphatemia associated with cortical hyperostosis.
- 27.Frishberg Y, Topaz O, Bergman R, Behar D, Fisher D, Gordon D, Richard G, Sprecher E. Identification of a recurrent mutation in GALNT3 demonstrates that hyperostosis-hyperphosphatemia syndrome and familial tumoral calcinosis are allelic disorders. J Mol Med. 2005;83:33–38. doi: 10.1007/s00109-004-0610-8. [DOI] [PubMed] [Google Scholar]
- 28.Topaz O, Shurman DL, Bergman R, Indelman M, Ratajczak P, Mizrachi M, Khamaysi Z, Behar D, Petronius D, Friedman V, et al. Mutations in GALNT3, encoding a protein involved in O-linked glycosylation, cause familial tumoral calcinosis. Nat Genet. 2004;36:579–581. doi: 10.1038/ng1358. [DOI] [PubMed] [Google Scholar]
- 29. Kato K, Jeanneau C, Tarp MA, Benet-Pages A, Lorenz-Depiereux B, Bennett EP, Mandel U, Strom TM, Clausen H. Polypeptide GalNAc-transferase T3 and familial tumoral calcinosis. Secretion of fibroblast growth factor 23 requires O-glycosylation. J Biol Chem. 2006;281:18370–18377. doi: 10.1074/jbc.M602469200. This study showed that secretion of FGF-23 requires O-glycosylation, and that GalNAc-T3 selectively directs O-glycosylation in a subtilisin-like proprotein convertase recognition sequence motif, which blocks processing of FGF-23. A novel posttranslational regulation of FGF-23 has been proposed.
- 30.Kuro-o M. M: Disease model: human aging. Trends Mol Med. 2001;7:179–181. doi: 10.1016/s1471-4914(01)01921-9. [DOI] [PubMed] [Google Scholar]
- 31.Nabeshima Y. Klotho: a fundamental regulator of aging. Ageing Res Rev. 2002;1:627–638. doi: 10.1016/s1568-1637(02)00027-2. [DOI] [PubMed] [Google Scholar]
- 32. Nabeshima Y. Toward a better understanding of Klotho. Sci Aging Knowledge Environ. 2006;2006:pe11. doi: 10.1126/sageke.2006.8.pe11. This recent review article nicely compiled the diverse effects of klotho.
- 33.Sethe S, Scutt A, Stolzing A. Aging of mesenchymal stem cells. Ageing Res Rev. 2006;5:91–116. doi: 10.1016/j.arr.2005.10.001. [DOI] [PubMed] [Google Scholar]
- 34.Galvin JE, Ginsberg SD. Expression profiling in the aging brain: a perspective. Ageing Res Rev. 2005;4:529–547. doi: 10.1016/j.arr.2005.06.009. [DOI] [PubMed] [Google Scholar]
- 35.Dirks AJ, Hofer T, Marzetti E, Pahor M, Leeuwenburgh C. Mitochondrial DNA mutations, energy metabolism and apoptosis in aging muscle. Ageing Res Rev. 2006;5:179–195. doi: 10.1016/j.arr.2006.03.002. [DOI] [PubMed] [Google Scholar]
- 36.Zha Y, Le VT, Higami Y, Shimokawa I, Taguchi T, Razzaque MS. Life-long suppression of growth hormone-insulin-like growth factor I activity in genetically altered rats could prevent age-related renal damage. Endocrinology. 2006;147:5690–5698. doi: 10.1210/en.2006-0302. [DOI] [PubMed] [Google Scholar]
- 37. Lanske B, Razzaque MS. Premature aging in klotho mutant mice. cause or consequence? Ageing Res Rev. 2007 doi: 10.1016/j.arr.2007.02.002. Based on recent understanding of klotho and FGF-23 interactions, this review convincingly explained why the premature aging-like features of klotho deficient mice, is not a primary cause of klotho inactivity, rather a consequence of inability of Fgf-23 to act.
- 38.Renkema KY, Nijenhuis T, van der Eerden BC, van der Kemp AW, Weinans H, van Leeuwen JP, Bindels RJ, Hoenderop JG. Hypervitaminosis D mediates compensatory Ca2+ hyperabsorption in TRPV5 knockout mice. J Am Soc Nephrol. 2005;16:3188–3195. doi: 10.1681/ASN.2005060632. [DOI] [PubMed] [Google Scholar]
- 39.Dusso AS, Brown AJ, Slatopolsky E. Vitamin D. Am J Physiol Renal Physiol. 2005;289:F8–F28. doi: 10.1152/ajprenal.00336.2004. [DOI] [PubMed] [Google Scholar]
- 40.Heikinheimo RJ, Inkovaara JA, Harju EJ, Haavisto MV, Kaarela RH, Kataja JM, Kokko AM, Kolho LA, Rajala SA. Annual injection of vitamin D and fractures of aged bones. Calcif Tissue Int. 1992;51:105–110. doi: 10.1007/BF00298497. [DOI] [PubMed] [Google Scholar]
- 41.Dawson-Hughes B, Harris SS, Krall EA, Dallal GE. Effect of calcium and vitamin D supplementation on bone density in men and women 65 years of age or older. N Engl J Med. 1997;337:670–676. doi: 10.1056/NEJM199709043371003. [DOI] [PubMed] [Google Scholar]
- 42.Garnero P, Munoz F, Sornay-Rendu E, Delmas PD. Associations of vitamin D status with bone mineral density, bone turnover, bone loss and fracture risk in healthy postmenopausal women. The OFELY study. Bone. 2006 doi: 10.1016/j.bone.2006.09.026. [DOI] [PubMed] [Google Scholar]
- 43.Jackson RD, LaCroix AZ, Gass M, Wallace RB, Robbins J, Lewis CE, Bassford T, Beresford SA, Black HR, Blanchette P, et al. Calcium plus vitamin D supplementation and the risk of fractures. N Engl J Med. 2006;354:669–683. doi: 10.1056/NEJMoa055218. [DOI] [PubMed] [Google Scholar]
- 44.Adams JS, Lee G. Gains in bone mineral density with resolution of vitamin D intoxication. Ann Intern Med. 1997;127:203–206. doi: 10.7326/0003-4819-127-3-199708010-00004. [DOI] [PubMed] [Google Scholar]
- 45.Beck L, Karaplis AC, Amizuka N, Hewson AS, Ozawa H, Tenenhouse HS. Targeted inactivation of Npt2 in mice leads to severe renal phosphate wasting, hypercalciuria, and skeletal abnormalities. Proc Natl Acad Sci U S A. 1998;95:5372–5377. doi: 10.1073/pnas.95.9.5372. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Shimada T, Kakitani M, Yamazaki Y, Hasegawa H, Takeuchi Y, Fujita T, Fukumoto S, Tomizuka K, Yamashita T. Targeted ablation of Fgf23 demonstrates an essential physiological role of FGF23 in phosphate and vitamin D metabolism. J Clin Invest. 2004;113:561–568. doi: 10.1172/JCI19081. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Sitara D, Razzaque MS, Hesse M, Yoganathan S, Taguchi T, Erben RG, Jueppner H, Lanske B. Homozygous ablation of fibroblast growth factor-23 results in hyperphosphatemia and impaired skeletogenesis, and reverses hypophosphatemia in Phex-deficient mice. Matrix Biol. 2004;23:421–432. doi: 10.1016/j.matbio.2004.09.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Tsujikawa H, Kurotaki Y, Fujimori T, Fukuda K, Nabeshima Y. Klotho, a gene related to a syndrome resembling human premature aging, functions in a negative regulatory circuit of vitamin D endocrine system. Mol Endocrinol. 2003;17:2393–2403. doi: 10.1210/me.2003-0048. [DOI] [PubMed] [Google Scholar]
- 49.Razzaque MS, St-Arnaud R, Taguchi T. Lanske B: FGF-23, vitamin D and calcification:the unholy triad. Nephrol Dial Transplant. 2005;20:2032–2035. doi: 10.1093/ndt/gfh991. [DOI] [PubMed] [Google Scholar]
- 50.Saito H, Maeda A, Ohtomo S, Hirata M, Kusano K, Kato S, Ogata E, Segawa H, Miyamoto K, Fukushima N. Circulating FGF-23 is regulated by 1alpha,25-dihydroxyvitamin D3 and phosphorus in vivo. J Biol Chem. 2005;280:2543–2549. doi: 10.1074/jbc.M408903200. [DOI] [PubMed] [Google Scholar]
- 51. Liu S, Tang W, Zhou J, Stubbs JR, Luo Q, Pi M, Quarles LD. Fibroblast growth factor 23 is a counter-regulatory phosphaturic hormone for vitamin D. J Am Soc Nephrol. 2006;17:1305–1315. doi: 10.1681/ASN.2005111185. Presence of a vitamin D-responsive element in the promoter region of FGF-23 was claimed to be mediating transcriptional activation of FGF-23 following induction with vitamin- D.
- 52. Tenenhouse HS. Regulation of phosphorus homeostasis by the type iia na/phosphate cotransporter. Annu Rev Nutr. 2005;25:197–214. doi: 10.1146/annurev.nutr.25.050304.092642. A comprehensive review of renal regulation of phosphate transport by Na/Pi 2a, and also discussed influence of other regulatory molecules.
- 53.Murer H, Hernando N, Forster I, Biber J. Proximal tubular phosphate reabsorption: molecular mechanisms. Physiol Rev. 2000;80:1373–1409. doi: 10.1152/physrev.2000.80.4.1373. [DOI] [PubMed] [Google Scholar]
- 54.Xu H, Bai L, Collins JF, Ghishan FK. Age-dependent regulation of rat intestinal type IIb sodium-phosphate cotransporter by 1,25-(OH)(2) vitamin D(3) Am J Physiol Cell Physiol. 2002;282:C487–C493. doi: 10.1152/ajpcell.00412.2001. [DOI] [PubMed] [Google Scholar]
- 55. Segawa H, Yamanaka S, Ohno Y, Onitsuka A, Shiozawa K, Aranami F, Furutani J, Tomoe Y, Ito M, Kuwahata M, et al. Correlation between hyperphosphatemia and type II Na/Pi cotransporter activity in klotho mice. Am J Physiol Renal Physiol. 2006 doi: 10.1152/ajprenal.00248.2006. This article clearly demonstrated the role of NaPi2a in inducing hyperphosphatemia in klotho ablated mice.
- 56.Eddy AA. Can renal fibrosis be reversed? Pediatr Nephrol. 2005;20:1369–1375. doi: 10.1007/s00467-005-1995-5. [DOI] [PubMed] [Google Scholar]
- 57.Taguchi T, Razzaque MS. The collagen-specific molecular chaperone HSP47: is there a role in fibrosis? Trends Mol Med. 2007;13:45–53. doi: 10.1016/j.molmed.2006.12.001. [DOI] [PubMed] [Google Scholar]
- 58.Liu Y. Renal fibrosis: new insights into the pathogenesis and therapeutics. Kidney Int. 2006;69:213–217. doi: 10.1038/sj.ki.5000054. [DOI] [PubMed] [Google Scholar]
- 59.Milliner DS, Zinsmeister AR, Lieberman E, Landing B. Soft tissue calcification in pediatric patients with end-stage renal disease. Kidney Int. 1990;38:931–936. doi: 10.1038/ki.1990.293. [DOI] [PubMed] [Google Scholar]
- 60.Goldsmith DJ, Covic A, Sambrook PA, Ackrill P. Vascular calcification in long-term haemodialysis patients in a single unit: a retrospective analysis. Nephron. 1997;77:37–43. doi: 10.1159/000190244. [DOI] [PubMed] [Google Scholar]
- 61.Cofan F, Garcia S, Combalia A, Campistol JM, Oppenheimer F, Ramon R. Uremic tumoral calcinosis in patients receiving longterm hemodialysis therapy. J Rheumatol. 1999;26:379–385. [PubMed] [Google Scholar]
- 62.Seyahi N, Apaydin S, Sariyar M, Serdengecti K, Erek E. Intracranial calcification and tumoural calcinosis during vitamin D therapy. Nephrology (Carlton) 2004;9:89–93. doi: 10.1111/j.1440-1797.2003.00237.x. [DOI] [PubMed] [Google Scholar]
- 63.Shoji T, Shinohara K, Kimoto E, Emoto M, Tahara H, Koyama H, Inaba M, Fukumoto S, Ishimura E, Miki T, et al. Lower risk for cardiovascular mortality in oral 1alpha-hydroxy vitamin D3 users in a haemodialysis population. Nephrol Dial Transplant. 2004;19:179–184. doi: 10.1093/ndt/gfg513. [DOI] [PubMed] [Google Scholar]
- 64.Zisman AL, Hristova M, Ho LT, Sprague SM. Impact of Ergocalciferol Treatment of Vitamin D Deficiency on Serum Parathyroid Hormone Concentrations in Chronic Kidney Disease. Am J Nephrol. 2007;27:36–43. doi: 10.1159/000098561. [DOI] [PubMed] [Google Scholar]
- 65.Mazzaferro S, Pasquali M, Pugliese F, Barresi G, Carbone I, Francone M, Sardella D, Taggi F. Serum Levels of Calcification Inhibition Proteins and Coronary Artery Calcium Score: Comparison between Transplantation and Dialysis. Am J Nephrol. 2007;27:75–83. doi: 10.1159/000099095. [DOI] [PubMed] [Google Scholar]
- 66.Abboud H, Coyne D, Smolenski O, Anger M, Lunde N, Qiu P, Hippensteel R, Pradhan RS, Palaparthy RV, Kavanaugh A, et al. A comparison of dosing regimens of paricalcitol capsule for the treatment of secondary hyperparathyroidism in CKD stages 3 and 4. Am J Nephrol. 2006;26:105–114. doi: 10.1159/000092033. [DOI] [PubMed] [Google Scholar]
- 67.Lanske B, Razzaque MS. Vitamin-D and aging: old concepts and new insights. J Nutr Biochem. 2007 doi: 10.1016/j.jnutbio.2007.02.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Kolek OI, Hines ER, Jones MD, LeSueur LK, Lipko MA, Kiela PR, Collins JF, Haussler MR, Ghishan FK. 1alpha,25-Dihydroxyvitamin D3 upregulates FGF23 gene expression in bone: the final link in a renal-gastrointestinal-skeletal axis that controls phosphate transport. Am J Physiol Gastrointest Liver Physiol. 2005;289:G1036–G1042. doi: 10.1152/ajpgi.00243.2005. [DOI] [PubMed] [Google Scholar]
- 69.Bai S, Favus MJ. Vitamin D and calcium receptors: links to hypercalciuria. Curr Opin Nephrol Hypertens. 2006;15:381–385. doi: 10.1097/01.mnh.0000232878.50716.26. [DOI] [PubMed] [Google Scholar]
- 70.Hoenderop JG, Nilius B, Bindels RJ. Molecular mechanism of active Ca2+ reabsorption in the distal nephron. Annu Rev Physiol. 2002;64:529–549. doi: 10.1146/annurev.physiol.64.081501.155921. [DOI] [PubMed] [Google Scholar]
- 71.Shimada T, Hasegawa H, Yamazaki Y, Muto T, Hino R, Takeuchi Y, Fujita T, Nakahara K, Fukumoto S, Yamashita T. FGF-23 is a potent regulator of vitamin D metabolism and phosphate homeostasis. J Bone Miner Res. 2004;19:429–435. doi: 10.1359/JBMR.0301264. [DOI] [PubMed] [Google Scholar]
- 72. Chang Q, Hoefs S, van der Kemp AW, Topala CN, Bindels RJ, Hoenderop JG. The beta-glucuronidase klotho hydrolyzes and activates the TRPV5 channel. Science. 2005;310:490–493. doi: 10.1126/science.1114245. This study shows that klotho hydrolyzes extracellular sugar residues on TRPV5, entrapping the channel in the plasma membrane, and thereby maintaining durable calcium channel activity and membrane calcium permeability in the kidney.