Abstract
The 2 predominant etiologies of right ventricular tachycardia (VT) are arrhythmogenic right ventricular cardiomyopathy (ARVC) and idiopathic VT arising from the right ventricular outflow tract (RVOT). Both of these arrhythmias can be adrenergically mediated and may be difficult to distinguish clinically. A minor criterion for the diagnosis of ARVC is T wave inversion (TWI) in the right precordial leads during sinus rhythm. However, there have been reports of precordial TWI identified in patients with RVOT tachycardia. The purpose of this study was to determine whether patterns of precordial TWI could differentiate between the two groups. We evaluated a multicenter registry of 229 patients with VT of right ventricular origin. After appropriate exclusions (n=29), 79 patients (58% M, 40±14y) had ARVC, and 121 patients (41% M, 48±14y) had RVOT tachycardia. During sinus rhythm, 37/79 (47%) patients with ARVC and 5/121 (4%) patients with RVOT tachycardia had T-wave inversion in leads V1-V3. For the diagnosis of ARVC, TWI in leads V1-V3 had a sensitivity of 47% and a specificity of 96%. In conclusion, in patients with VT of RV origin, the presence of TWI in electrocardiogram leads V1-V3 supports the diagnosis of ARVC.
Keywords: ventricular tachycardia, arrhythmogenic right ventricular cardiomyopathy, ventricular outflow tract tachycardia, electrocardiography
Introduction
The 2 predominant etiologies of ventricular tachycardia (VT) arising from the right ventricle (RV) are arrhythmogenic right ventricular cardiomyopathy/dysplasia (ARVC) and idiopathic ventricular tachycardia arising from the RV outflow tract (RVOT). Discrimination between these 2 entities is critical, as their prognoses and therapeutic options differ.1,2 T-wave inversion (TWI) in the right precordial leads, as seen in Figure 1, is a minor criterion for the diagnosis of ARVC, and recently has been proposed as a major criterion.3,4 However, there have been reports identifying precordial TWI in 6 to 20% of patients with RVOT tachycardia (Figure 2).5,6,7 Prior investigations examining the discriminatory utility of precordial TWI included relatively small numbers of patients and did not examine closely the extent of TWI that could best differentiate ARVC from RVOT.8 This study uses data from a large population of patients with VT of RV origin to determine whether patterns of precordial TWI could differentiate between ARVC and idiopathic RVOT tachycardia.
Figure 1.
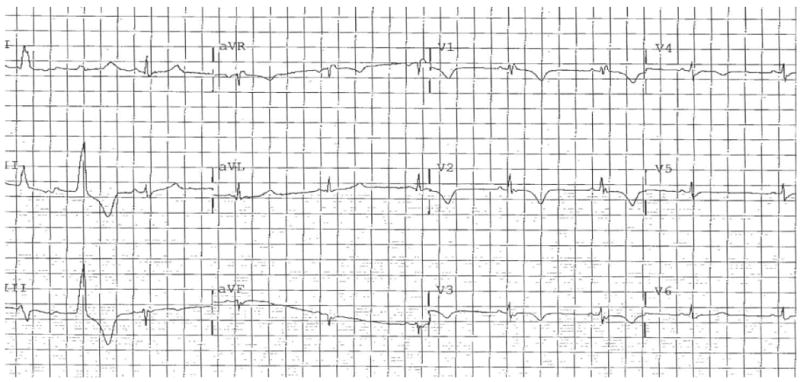
Electrocardiogram from a patient with right ventricular tachycardia, with T-wave inversion in V1 to V4.
Figure 2.
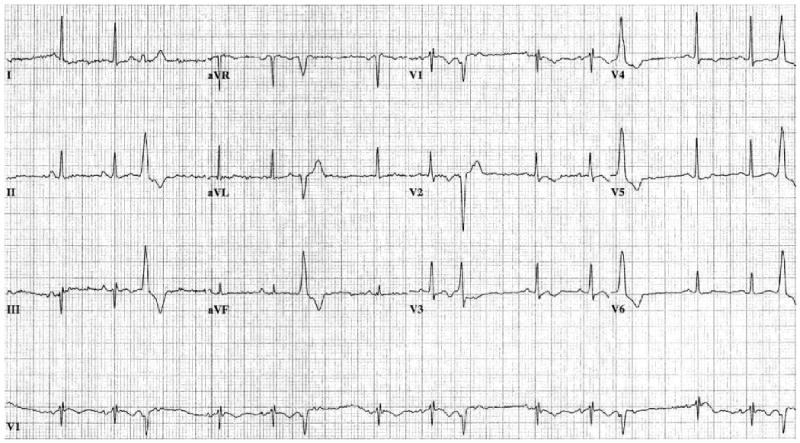
Electrocardiogram from a patient with right ventricular outflow tract tachycardia, with T-wave inversion in leads V1 to V4.
Methods
We evaluated a multicenter registry of patients with VT of RV origin. The source population was derived from the National Institutes of Health supported Multidisciplinary Study of Right Ventricular Dysplasia (n=108)9 and the Cornell University Medical Center registry of idiopathic VT (n=121).
The clinical testing used to diagnose the ARVC population has been published.9 Of the 121 RVOT patients, 115 (95%) had undergone echocardiography, with no findings consistent with ARVC. Of the 62 (51%) magnetic resonance imaging tests performed, 5 MRIs showed minor abnormalities, but none was diagnostic of ARVC. None of the 19 (16%) endocardial biopsies was consistent with ARVC, and only 1 of the 13 (11%) available signal-averaged electrocardiograms was abnormal. On endocardial mapping, all idiopathic VT patients had normal RV endocardial voltage and a focal source of VT originating in the RVOT. No RVOT patient met Task Force criteria for the diagnosis of ARVC, and on follow-up none has been diagnosed as affected by ARVC. No patient with RVOT tachycardia had bundle branch block.
We included only ARVC registry patients who had an available 12-lead electrocardiogram without complete bundle-branch block (n=94) and excluded those patients who ultimately were classified as “unaffected” (n=7). To reduce bias in the analysis of sensitivity, we also excluded ARVC registry patients for whom the presence of T wave inversion was crucial for the diagnosis of ARVC based on Task Force criteria (n=8). After exclusions, the population examined consisted of 79 patients with ARVC and 121 patients with RVOT tachycardia. A reader unaware of the diagnoses examined each patient's sinus rhythm 12-lead electrocardiogram for the presence of TWI in the precordial leads.
All statistical analyses were performed using SPSS Version 16.0 for Windows (SPSS Inc., Chicago, IL). Analyses of differences between groups were performed using Student's t-test for continuous variables and the chi-square test for categorical variables. In all analyses, 2-sided p<0.05 was considered significant. Continuous variables are expressed as mean±SD, and categorical variables are expressed as n (%).
Results
Patients with ARVC were younger than those with RVOT (40±14 vs. 48±14 years, p<0.001) and were more likely to be male (58% vs. 41%, p=0.02). Overall, among the 79 ARVC patients, no TWI was seen in 15 patients (19%). TWI was observed in V1 in 21 patients (27%), V1 and V2 in 6 (8%), V1 through V3 in 12 (15%), V1 through V4 in 14 (18%), V1 through V5 in 5 (6%), and V1 through V6 in 6 (8%). one patient (1%) had TWI limited to V4-V6, and 1 patient (1%) had TWI in V6 only. Among the 121 RVOT patients, no TWI was seen in 40 patients (33%), and TWI was observed in V1 in 62 patients (51%), V1 and V2 in 13 (11%), V1 through V3 in 1 (1%), V1 through V4 in 1 (1%), V1 through V5 in 1 (1%), and V1 through V6 in 2 (2%). One patient (1%) had TWI in V5 and V6 only.
A summary of the extent of right precordial TWI among this population is shown in Table 1. Thirty-seven of 79 (47%) patients with ARVC and 5/121 (4%) patients with RVOT tachycardia had T-wave inversion in leads V1-V3 or beyond. As shown in Table 2, TWI in leads V1-V3 had a sensitivity of 47% and a specificity of 96% for the diagnosis of ARVC.
Table 1.
Number of patients with precordial T-wave inversion based on varying degrees of precordial lead progression.
| Progression of TWI | ARVC (n=79) | RVOT (n=121) |
|---|---|---|
| V2 | 43 (57%) | 13 (11%) |
| V3 | 37 (47%) | 5 (4%) |
| V4 | 25 (32%) | 3 (2%) |
ARVC=arrhythmogenic right ventricular cardiomyopathy. RVOT=right ventricular outflow tract tachycardia. TWI=T-wave inversion.
Table 2.
Sensitivity and specificity for the diagnosis of ARVC, using precordial lead progression of T-wave inversion as the test criterion.
| Progression of TWI | Sensitivity | Specificity |
|---|---|---|
| V2 | 57% | 89% |
| V3 | 47% | 96% |
| V4 | 32% | 98% |
ARVC=arrhythmogenic right ventricular cardiomyopathy. TWI=T-wave inversion.
Discussion
The main finding of this investigation is that the pattern of precordial T-wave inversion can differentiate ARVC from idiopathic VT arising from the RVOT. In patients with VT arising from the RVOT, the presence of T-wave inversion in electrocardiogram leads V1-V3 during sinus rhythm supports the diagnosis of ARVC, with very high specificity. Our findings lend support to the proposal that right precordial TWI be considered a major criterion in the ARVC Task Force Criteria.
Prior studies in the ARVC population have shown varying prevalences of right precordial T-wave inversion. TWI in V1-V3 has been reported in 36 to 96% of ARVC patients, with a prevalence of 47% seen in our population.7,8,10,11 This degree of interstudy discrepancy may be related to differing extents of myocardial involvement among the populations, since TWI is known to be more pronounced in patients with ARVC who have extensive disease than in those with localized RV involvement.8,12 Since the electrocardiogram changes in ARVC develop with progressive fibrofatty replacement of right ventricular tissue,13 the relatively low prevalence of TWI in our ARVC population may be the result of a relatively high proportion of patients with early disease. This hypothesis is supported by the fact that all ARVC registry patients had been diagnosed within three years prior to inclusion in the study. T-wave inversion in V1 through V3 is present in fewer than 3% of healthy young adults.14
While the specificity of right precordial TWI was excellent for the discrimination of ARVC from RVOT, the sensitivity was only moderate. Other electrocardiogram findings may be helpful in making the correct diagnosis, with localized right precordial QRS prolongation, terminal activation delay, and/or the presence of epsilon waves being the most valuable for diagnosing ARVC in prior analyses.10,15 Further study would be required to compare the relative significance of each of these findings.
Acknowledgments
Supported in part by United States National Institute of Health (NIH) grants U0165652, U01HL65691, and U01HL65594.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Goy JJ, Trauxe F, Fromer M, Schläpfer J, Vogt P, Kappenberger L. Ten-years follow-up of 20 patietns with idiopathic ventricular tachycardia. Pacing Clin Electrophysiol. 1990;13:1142–1147. doi: 10.1111/j.1540-8159.1990.tb02172.x. [DOI] [PubMed] [Google Scholar]
- 2.Hulot JS, Jouven X, Empana JP, Frank R, Fontaine G. Natural History and Risk Stratification of Arrhythmogenic Right Ventricular Dysplasia/Cardiomyopathy. Circulation. 2004;110:1879–1884. doi: 10.1161/01.CIR.0000143375.93288.82. [DOI] [PubMed] [Google Scholar]
- 3.McKenna WJ, Thiene G, Nava A, Fontaliran F, Blomstrom-Lundqvist C, Fontaine G, Camerini F. Diagnosis of arrhythmogenic right ventricular dysplasia/cardiomyopathy. Task Force of the Working Group Myocardial and Pericardial Disease of the European Society of Cardiology and of the Scientific Council on Cardiomyopathies of the International Society and Federation of Cardiology. Br Heart J. 71:215–218. doi: 10.1136/hrt.71.3.215. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Marcus F, McKenna WJ, Sherrill D, Basso C, Bauce B, Bluemke DA, Calkins H, Corrado D, Corrado D, Cox MGPJ, Daubert JP, Fontaine G, Gear K, Hauer RNW, Nava A, Picard MH, Protonotarios N, Saffitz JE, Sanborn DMY, Tandri H, Thiene G, Towbin JA, Tsatsopolou A, Wichter T, Zareba W. Diagnosis of Arrhythmogenic Right Ventricular Cardiomyopathy/Dysplasia (ARVC/D): Proposed Modification of the Task Force Criteria. Circulation. 2009 in press. [Google Scholar]
- 5.Markowitz SM, Litvak BL, Ramirez de Arellano EA, Markisz JA, Stein KM, Lerman BB. Adenosine-sensitive ventricular tachycardia: right ventricular abnormalities delineated by magnetic resonance imaging. Circulation. 1997;96:1192–200. doi: 10.1161/01.cir.96.4.1192. [DOI] [PubMed] [Google Scholar]
- 6.Kazmierczak J, De Sutter J, Tevernier R, Cuvelier C, Dimmer C, Jordaens L. Electrocardiographic and morphometric features in patients with ventricular tachycardia of right ventricular origin. Heart. 1998;79:388–393. doi: 10.1136/hrt.79.4.388. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.O'Donnell D, Cox D, Bourke J, Mitchell L, Furniss S. Clinical and electrophysiological differences between patients with arrhythmogenic right ventricular dysplasia and right ventricular outflow tract tachycardia. Eur Heart J. 2003;24:801–810. doi: 10.1016/s0195-668x(02)00654-1. [DOI] [PubMed] [Google Scholar]
- 8.Nasir K, Bomma C, Tandri H, Roguin A, Dalal D, Prakasa K, Tichnell C, James C, Spevak PJ, Marcus F, Calkins H. Electrocardiographic features of arrhythmogenic right ventricular dysplasia/cardiomyopathy according to disease severity: A need to broaden diagnostic criteria. Circulation. 2004;110:1527–1534. doi: 10.1161/01.CIR.0000142293.60725.18. [DOI] [PubMed] [Google Scholar]
- 9.Marcus FI, Zareba W, Calkins H, Towbin JA, Basso C, Bluemke DA, Estes NA, 3rd, Picard MH, Sanborn D, Thiene G, Wichter T, Cannom D, Wilber DJ, Scheinman M, Duff H, Daubert J, Talajic M, Krahn A, Sweeney M, Garan H, Sakaguchi S, Lerman BB, Kerr C, Kron J, Steinberg JS, Sherrill D, Gear K, Brown M, Severski P, Polonsky S, McNitt S. Arrhythmogenic right ventricular cardiomyopathy/dysplasia: clinical presentation and diagnostic evaluation: results from the North American Multidisciplinary Study. Heart Rhythm. 2009;6(7):984–92. doi: 10.1016/j.hrthm.2009.03.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Peters S, Trummel M. Diagnosis of arrhythmogenic right ventricular dysplasia-cardiomyopathy: Value of standard ECG revisited. Ann Noninvasive Electrocardiol. 2003;8:238–245. doi: 10.1046/j.1542-474X.2003.08312.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Ma KJ, Li N, Wang HT, Chu JM, Fang PH, Yao Y, Ma J, Hua W, Zhang S, Wang FZ, Li Z, Pu JL. Clinical study of 39 Chinese patients with arrhythmogenic right ventricular dysplasia/cardiomyopathy. Chin Med J. 2009;122:1133–1138. [PubMed] [Google Scholar]
- 12.Nava A, Canciani B, Juja G, Martini B, Daliento L, Scognamiglio R, Thiene G. Electrovectorcardiographic study of negative T waves on precordial leads in arrhythmogenic right ventricular dysplasia: relationship with right ventricular volumes. J Electrocardiol. 1988;21:239–245. doi: 10.1016/0022-0736(88)90098-2. [DOI] [PubMed] [Google Scholar]
- 13.Marcus FI, Zareba W. The electrocardiogram in right ventricular cardiomyopathy/dysplasia. How can the electrocardiogram assist in understanding the pathologic and functional changes of the heart in this disease? J Electrocardiol. 2009;42:136e1–136e5. doi: 10.1016/j.jelectrocard.2008.12.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Marcus FI. Prevalence of T wave inversion beyond V1 in young normal individuals and usefulness for the diagnosis of arrhythmogenic right ventricular cardiomyopathy/dysplasia. Am J Cardiol. 2005;95:1070–1071. doi: 10.1016/j.amjcard.2004.12.060. [DOI] [PubMed] [Google Scholar]
- 15.Jain R, Dalal D, Daly A, Tichnell C, James C, Evenson A, Jain R, Abraham T, Tan BY, Tandri H, Russell SD, Judge D, Calkins H. Electrocardiographic features of arrhythmogenic right ventricular dysplasia. Circulation. 2009;120:477–487. doi: 10.1161/CIRCULATIONAHA.108.838821. [DOI] [PMC free article] [PubMed] [Google Scholar]


