Abstract
Background:
A majority of community-dwelling older adults manage their own medication regimens. This study describes the development and first phase of testing of the Self-Medication Assessment Tool (SMAT), designed to screen for cognitive and functional deficits in relation to medication self-management among community-dwelling geriatric patients.
Objective:
To evaluate the face validity of the SMAT and to determine its acceptability among pharmacists.
Methods:
An instrument was designed, with 5 assessment scales to measure function, cognition, medication recall, and 2 aspects of adherence. The instrument included a standardized test kit and instructions for testers. Focus groups interviews, individual interviews, and surveys were used to determine the reactions of community and hospital-based pharmacists to the tool. Transcripts of the focus group and individual interviews were coded for main themes. Pharmacists’ ratings of usefulness, thoroughness, and ease of use, as well as their willingness to use the instrument, were compared with a neutral rating on a 7-point scale by means of 1-sample t tests.
Results:
Focus group interviews or individual interviews were conducted with 17 pharmacists and 3 pharmacy students (out of a potential population of about 300) who responded to an invitation to participate. The pharmacists felt that the tool would be useful in identifying difficulties with medication management and potential interventions, and they expressed a willingness to use it in their respective practices. Pharmacists working in hospital settings were slightly more willing than community pharmacists to use the tool. Interviewees highlighted ways to improve the tool before testing of its psychometric properties in the planned second phase of this project.
Conclusions:
The SMAT had strong face validity and was particularly acceptable for use by pharmacists in hospital settings.
Keywords: medication therapy management, geriatric assessment, self-care, medication adherence, validation studies
Abstract
Contexte :
Une majorité d’adultes âgés vivant dans la communauté gèrent eux-mêmes la prise de leurs médicaments. Cette étude décrit la mise au point et la phase initiale de la validation d’un outil d’évaluation de l’automédication (OEAM) conçu pour dépister les déficits cognitifs et fonctionnels relatifs à l’augotestion des médicaments chez les patients gériatriques vivant dans la communauté.
Objectif :
Évaluer la validité apparente de l’OEAM et déterminer son acceptabilité chez les pharmaciens.
Méthodes :
Un outil comportant cinq échelles d’évaluation a été conçu pour mesurer les capacités fonctionnelles, la cognition, le rappel des connaissances sur les médicaments et deux aspects de l’observance. L’outil était pourvu d’une trousse de validation standardisée et d’instructions pour les essayeurs. Des entrevues de groupe, des entrevues individuelles et des sondages ont été utilisés pour déterminer les réactions des pharmaciens communautaires et hospitaliers face à l’outil. Les transcriptions des entrevues de groupe et des entrevues individuelles ont été codées pour ce qui est des principaux thèmes. Les notations des pharmaciens quant à l’utilité, à la rigueur et à la facilité d’emploi, ainsi qu’à leur propension à l’utilisation ont été comparées à une notation objective sur une échelle de sept points à l’aide de tests t pour échantillon unique.
Résultats :
Les entrevues de groupe ou individuelles ont été menées chez 17 pharmaciens et trois étudiants en pharmacie (provenant d’une population potentielle d’environ 300) qui ont accepté l’invitation à participer. Les pharmaciens ont estimé que l’outil serait utile pour cerner les difficultés de gestion des médicaments et les interventions potentielles, et ils ont exprimé leur propension à l’utiliser dans leur milieu d’exercice respectif. Les pharmaciens en milieu hospitalier étaient un peu plus enclins à utiliser l’outil que leurs collègues du secteur communautaire. Les interviewés ont souligné des façons d’améliorer l’outil avant d’en tester les propriétés psychométriques dans la deuxième phase anticipée de ce projet.
Conclusions :
L’OEAM avait une validité apparente élevée et son utilisation était particulièrement acceptable par les pharmaciens en milieu hospitalier.
[Traduction par l’éditeur]
Keywords: gestion du traitement médicamenteux, évaluation gériatrique, autosoins, observance du traitement médicamenteux, études de validation
INTRODUCTION
For more than a decade, pharmacists have used screening tools to identify patients eligible for institution-based self-medication programs. Many of these tools have been derived from an instrument that focused on older patients’ functional ability to take medication.1 Evaluations have included assessment of motor skills for opening and closing vials or removing tablets, as well as the ability to read prescription labels and identify tablet colours. Other aspects of screening have included questions about daily routine, adverse effects or allergies with previous medications, recall of the preadmission medication regimen, and medication self-management practices (storage, use of compliance aids, and methods of handling missed doses). Several deficiencies have been identified with this approach, including the inability to score or otherwise quantify the results, poor inter-rater reliability, and undetermined reproducibility of the results.2 Furthermore, cognitive capacity for self-medication is not directly addressed by these tools. As a result, recommendations for patient self-care are often based largely on the clinical skill and experience of the pharmacist who administers the screening tool.
To address the issue of cognitive capacity for self-medication, several researchers have employed various tests in an attempt to predict success in medication self-administration.2–8 Two of these tests specifically attempted to measure capacity for medication self-management. The Drug Regimen Unassisted Grading Scale (DRUGS) incorporated a stepwise progression of 4 tasks: identification, access, dosage, and timing.9,10 This scale allows the assessor to calculate a score that has been found to be useful in identifying early deficits that can increase risk in medication self-management.10 However, the DRUGS was evaluated in only a small cohort of well-educated, highly functioning older adults, and the power of the study was insufficient to detect differences in clinical outcomes. The Brief Medication Questionnaire (BMQ) was designed as a self-report tool for screening medication adherence and identifying barriers to adherence; upon completion of the questionnaire, the patient’s rating on an Adherence Risk Scale can be determined.11 The BMQ successfully predicted adherence levels, although it was tested in only a small cohort of highly educated middle-aged adults.
Clearly, there is a need for a comprehensive, evidence-based, self-medication assessment instrument that incorporates not only functional ability, but also tests of cognitive capacity, medication recall, and beliefs about medication use. The instrument needs to be not only reliable and valid for measuring older adults’ capacity for medication self-care, but also acceptable to pharmacists working with older patients. The first phase in the development and testing of the Self-Medication Assessment Tool (SMAT) is described in the present report. The goals of this study were to determine the face validity of the SMAT and its acceptability among pharmacists. The study involved structured individual and focus group interviews with pharmacists who had been asked to examine the SMAT, as well as a short questionnaire in which the respondents were asked to rate the SMAT on a series of dimensions. It was hypothesized that pharmacists’ ratings of the SMAT would be positive.
METHODS
Design of Instrument
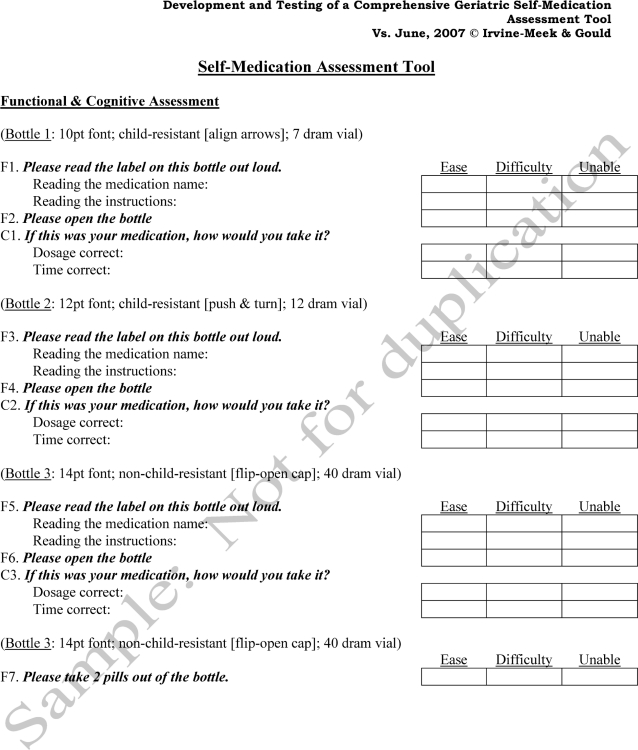
To address identified gaps in existing tools for assessing capacity for self-medication, the researchers designed an instrument with 5 assessment scales to measure function, cognition, medication recall, self-reported adherence, and intentional or purposeful nonadherence. Most of the items in these assessment scales were developed by the authors, although some items were adapted from the BMQ11 and the DRUGS.9 The version of the SMAT used in this study included a standardized kit with the required items for testing functional and cognitive capacity (e.g., a medication organizer) and administration instructions for testers.
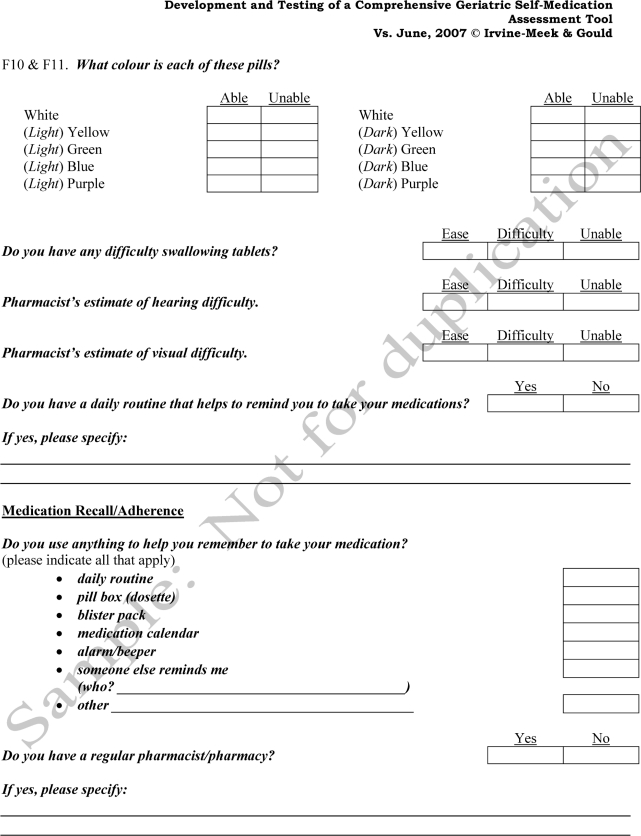
With the SMAT, the patient’s sensory, perceptual, and physical abilities are measured using the 22-item Functional Scale. Each item is scored on either a 2-point scale (able or unable) or a 3-point scale (ease, difficulty, unable). Tasks that are included are opening 3 types of prescription vial closures (align arrows, push and turn, flip open); reading prescription labels in 10-, 12-, and 14-point type; filling a standard weekly pill box; using a blister package filled by a pharmacist; and identifying certain colours. The patient’s hearing, vision, and swallowing ability are also evaluated.
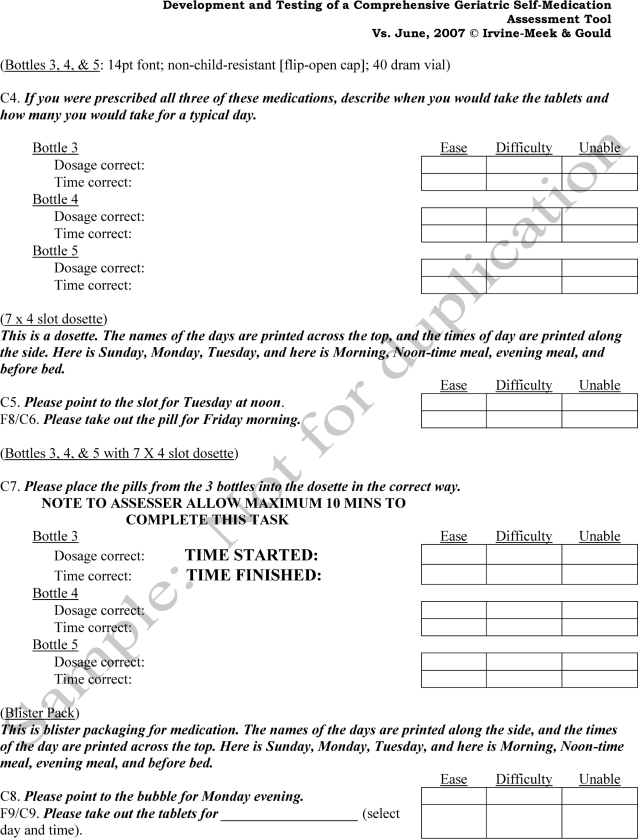
The patient’s ability to make judgements, manipulate information, and interpret instructions is determined using the 22-item Cognitive Scale. It is scored with a 3-point scoring system (ease, difficulty, unable). Tasks that are included are interpreting information on labels, organizing 3 test medications for daily use, organizing 3 test medications in a weekly pill organizer, and accurately locating medications in blister packages filled by a pharmacist.
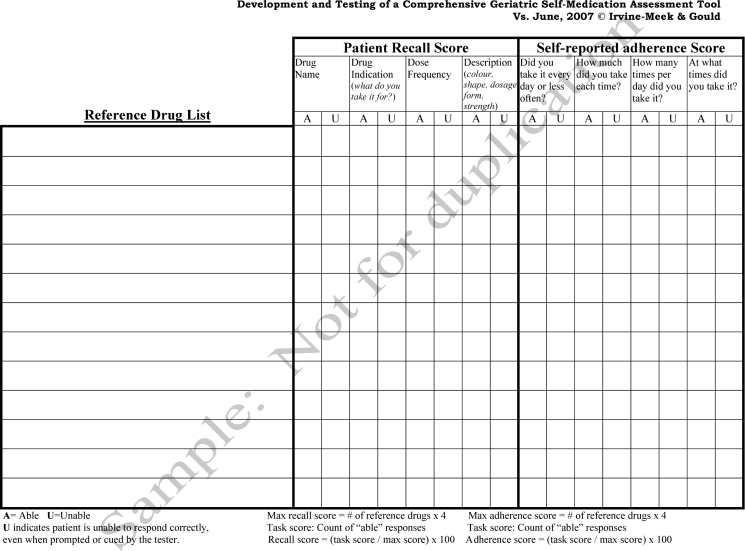
The patient’s ability to remember his or her own medication regimen is measured with the Recall Scale. The patient is asked to recall any or all of 4 items per drug: medication name, indication, dose regimen, and description (colour, shape, strength, and/or dosage form). A reference drug list obtained from the patient’s labelled prescription containers or from computerized pharmacy records is used to determine the maximum score (number of reference drugs multiplied by 4). The patient’s ability to recall each item for each drug is scored as “able” or “unable”. The total of the “able” results is expressed as a percentage of the maximum possible score.
The patient’s assessment of compliance with his or her own medication regimen is determined with the Self-Reported Adherence Scale, which is scored by the same method as the Recall Scale.
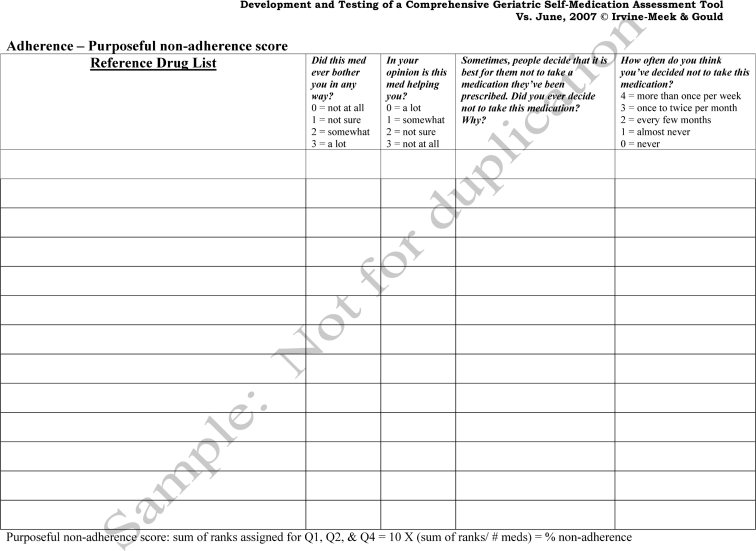
The Purposeful Nonadherence Scale measures the patient’s experiences with adverse effects of medications, belief in the value of medication, and history of stopping a medication without medical advice. For each drug, the patient is asked to choose a ranking for each item (e.g., “Did this medication ever bother you in any way?”). The rankings range from 0 (not at all) to 3 (a lot). The final score for this scale is calculated as the sum of the ranks for the 3 questions divided by the maximum possible score and expressed as a percentage.
Recruitment of Participants
A standardized invitation was sent to 40 community pharmacies and to the pharmacy department managers at 3 regional health authorities in southeastern New Brunswick. The community and hospital managers were asked to forward the invitation to all pharmacists and pharmacy students working at their sites, a total of about 300 individuals. All pharmacists and pharmacy students working in these settings who were willing to participate in the study were enrolled. As such, a nonprobability convenience sample was used. The study’s principal investigators (J.I.-M., O.N.G.) were blinded to the identity of the participants. Ethics approval was obtained from the Southeast Regional Health Authority (now Horizon Health Network) Research Ethics Board and the Mount Allison University Research Ethics Board.
Data Collection
The procedure for conducting and scoring the focus group and individual interviews was based on the methodology published by Krueger and Casey.12 Two research assistants were present at each interview. One research assistant (H.W.) assumed the role of moderator, asked the questions, and guided the group discussions (for focus groups). The other research assistant (L.E.T.) took field notes and was responsible for audiotaping the session.
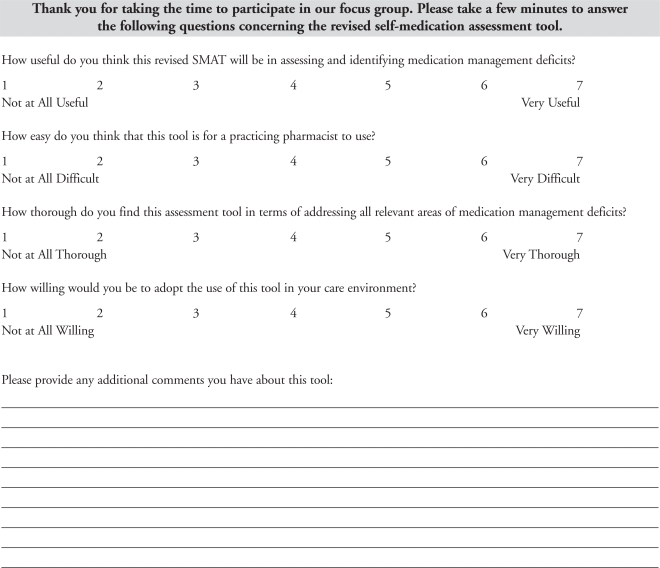
The moderator read a standardized script at the beginning of each interview and presented the SMAT. Participants were then given about 10 minutes to become familiar with the SMAT and to seek clarification if needed. A structured interview format was used. Participants were asked to comment on the perceived effectiveness of each section of the SMAT for assessing the self-management abilities of an elderly person; the suitability of the length of the instrument; the suitability of the language used for a wide range of patients; the ease of use of the instrument in terms of instructions provided, scoring system, and interpretation of scores; the ease of use for a pharmacist new to direct patient care; the need for changes to the instrument for use in the participant’s practice environment; and the major drawbacks of the tool. Each participant was also asked to complete a brief demographics survey and to answer a series of 4 rating questions on the usefulness, thoroughness, and ease of use of the tool (reverse-coded) and his or her willingness to adopt the tool (Online Appendix 1 at www.cjhp-online.ca/index.php/cjhp/issue/view/75). A 7-point rating scale, ranging from “not at all” to “very”, was used in this survey.
Data Analysis
The main themes of each interview were identified using content analysis of transcriptions of the interviews. The themes were organized according to the section of the instrument to which they pertained, and the comments were sorted into the following thematic categories: additional areas that participants felt should be examined, major drawbacks, major benefits, and concerns regarding administration. Relevant examples of quotations from the interviews were compiled to support these main themes. A series of 1-sample t tests was used to test the hypothesis that participants’ ratings were, on average, significantly more positive than the middle point on the 7-point scale. The results of the demographic questionnaire were used to classify participants on the basis of their practice location and years of practice.
RESULTS
A total of 17 pharmacists and 3 pharmacy students agreed to participate. The interview groups varied in size: 1 group of 5 persons, 1 group of 3 persons, 4 groups of 2 persons each, and 4 interviews with individual participants. The majority of pharmacists (13/17) had more than 5 years of experience. Eleven pharmacists and 1 student were working in a hospital setting, and 5 pharmacists and 2 students were working in a community setting. One pharmacist reported the work setting as “other”. The majority of pharmacists spent more than 50% of their time providing direct patient care.
Main Themes
Participants commented on various components of the instrument during the structured interviews. Examples are reported verbatim in Table 1, and the themes are summarized below. These comments prompted modifications to the SMAT, which are described in the Discussion section of this article.
Table 1.
Selected Comments from Participants for Each Section of the Original Self-Medication Assessment Tool
| Relevant Section | Participants’ Comments |
|---|---|
| Functional | I think that [the vials] are good because they start out more difficult and then when you can assess yes or not, or cannot open the bottle, that kind of answers that and then you go bigger. So you aren’t concentrating on that part when you are trying to ask other questions. I don’t know what is mostly used in community, if it is 12 or 14 or whatever, but shouldn’t the tool have that font on there, whatever it is? Even if we know that everyone is going to fail at 10, well, if that is what they are using in community then we have to go with 10. That is reality. I think that everything you have there would definitely weed out someone with functional problems. Yes, I think it’s very useful. Do you have auxiliary labels on those bottles? ... I think those would be good to see if they can interpret them. [With regard to hearing and vision assessment] I don’t know how comfortable I would be making that call. The hearing would be easier, but as far as their visual, obviously if they can’t read anything … but it could be hard. I think that it would just be much more subjective. |
| Cognitive | I am just wondering if someone would question if they can take all three in the morning. You might get the odd person who may wonder. And they may ask you as you are doing the assessment, and then what do you say? Score them as difficulty? If I had a patient that I gave the three bottles to, how would I ascertain the ease, difficulty, and unable if they were able to do it on one bottle and not the other? ... If they made only one mistake on all three bottles they are going to fall under difficulty and I am not sure if that is valid. That is a difficult task. I like the idea of getting them to fill a dosette and everything. Because it is a lot more hands-on because sometimes they can tell you what they want to do, but can they actually do it? |
| Reference drug list | Is it always checked with the community pharmacy? ... How do you know if they are giving you everything? I think that if you are going to do it at all that it is worth the call. |
| Recall section | I mean, a lot of patients may not necessarily know what the drug name is, what it is used for, and they may not know the strength but may still take it properly because they understand that it is something that needs to be taken each day. So I don’t know how well they will do in that. I think they would be well answered. I think the general public are more educated on their drugs now. Some patients are very knowledgeable about their medications and others just aren’t. but they are still really good at taking their medications but really don’t know a lot about why they are taking it. And not that it is a good thing, but that is sometimes the way it is. |
| Self-reported adherence | The question is, do you take it the way it was prescribed? The way you are supposed to take it? That is more what you want to ask. Because maybe I am only taking it twice a week. |
| Purposeful nonadherence | Sometimes it can be cost. A lot of seniors are on a limited budget. I like the way that you are putting the onus on the patient to have made the decision as to whether or not they are taking it. How often have YOU decided not to take it. And I like too that it is not asking specifically for side effects but is rather very general, “does it bother you”. That is very open ended … |
| Scoring | Well, you would have a validated score and you could say with that score you know what the patient needs. You have something black and white that you can tell this person needs a blister pack or dosettes or is just not able. You have something in writing rather than just someone’s opinion. So I think it would be really useful. To get back to your question of whether or not we like the scoring … for me, I like it. I mean it’s got ease, unable, but it also has that grey area in the middle so it’s simple but it allows for a little leeway for the middle if they are not fully incapable but have some difficulty. |
| Perceived benefits to patient care | It would be useful to show to the family. So they aren’t thinking, “Oh, she doesn’t understand my mom.” It can say this is what a validated tool says regardless of what you or [I think], and this would be the best course of action based on this tool. I would say that would be the biggest benefit. Whether it is a functional or cognitive thing, something has happened that has caused them to be admitted to hospital. So then I need to use something to establish whether or not we can safely send them back home. They may not see their pharmacist for a month, or they may not see them at all … but if the individual is able to go home but not quite as functional as they were before they may not make it back to the drug store … but if I already got that information then I can provide that information to a community pharmacist and give the appropriate recommendations. |
Functional Assessment
Participants’ comments on the tasks used to measure functional ability (Table 1) drew attention to the following issues. The hands-on nature of the assessment was deemed beneficial for effectively assessing difficulties with medication management. The use of different types of vial closures and various font sizes for the printing on labels was appreciated, as was the use of various medication organizers to identify manipulation or vision issues. Concern was expressed that the 10-point font for label printing was too small and would lead to frustration on the part of elderly patients. Some participants recommended that the assessment kit include medications dispensed in manufacturer’s boxes or blister packages, as well as commonly used auxiliary labels. Concerns were expressed about scoring for the colour identification task (e.g., whether the word “purple” would be acceptable as a descriptor for the colour lavender and what background and pill size would be used for the test). Finally, although participants saw the value of questions pertaining to pharmacists’ assessments of hearing difficulty, visual impairment, and ability to swallow pills, some were not comfortable assigning a score to these capabilities.
Cognitive Assessment
Participants’ comments on the tasks used to assess patients’ cognitive ability (Table 1) drew attention to the following issues. There was general agreement that the tasks of filling a weekly pill organizer and locating medications in the blister packages were appropriate. It was felt that these tasks would allow a pharmacist to identify patients experiencing difficulty with a pill organizer at home and would provide information that the pharmacist would find helpful for making appropriate recommendations. Participants expressed concern about the label directions, which consisted of only the number of tablets and the number of times per day that the medication should be taken. They anticipated that patients would want to have more specific instructions, such as “take with food”, for completing this task. Participants were also concerned that a patient’s request for additional information would constitute cueing and would affect the score. Feedback from one focus group interview concerned the use of 3 vials for the question “If you were prescribed all three of these medications, describe when you would take the tablets and how many you would take for a typical day.” These participants were of the opinion that the use of 3 medication vials would be too complex for many patients. However, participants in another focus group commented that using more than 3 vials for this question would be appropriate. Finally, some participants proposed a change to the scoring scheme for the medication organization task. For this task, the original tool specified that the patient be asked to make a plan of action for 3 medications to be taken in a typical day, with scoring on a single 3-point scale (ease, difficulty, unable). Interviewees felt that it would be difficult to assess performance using only a single score for the 3 medications.
Reference Drug List
Participants commented on the use of a “reference drug list” as the basis for the recall, self-reported adherence, and purposeful nonadherence scores. Participants were generally unsure of the origin of the reference drug list and whether the medications on the list would be verified with the patient’s community pharmacy (Table 1). It was also noted that patients’ interpretation of the terms “drugs” and “medications” might affect their recall of nonprescription medications and non-oral dosage forms such as inhalers.
Patient Recall Score
Participants’ comments on the descriptors used to assess recall (Table 1) drew attention to the following issues. There was general agreement that the 4 descriptors used for each drug were important; however, it was anticipated that patients would not obtain high scores on this section of the tool. Some participants were unsure how much prompting would be required from the tester and how prompted responses would be scored.
Self-Reported Adherence
Participants had few comments on the questions about self-reported adherence (Table 1). The only issue of concern dealt with the possibility of redundancy between the questions in this section and the questions for either the recall score or the purposeful nonadherence score.
Purposeful Nonadherence
Both pharmacists and pharmacy students commented that the 3 questions for measuring purposeful nonadherence would likely yield reliable information, as the language used in these questions was nonconfrontational and invited honest answers (Table 1). The inclusion of a direct question about the cost of medications was recommended.
Scoring
Participants raised the following issues related to scoring (Table 1). There was general agreement with the 3 types of scoring choices offered, but participants consistently requested clarification about the use of cueing. Participants in all groups expressed few concerns about calculation of the final score for each section of the tool and felt that the scoring methods would be easy to learn with practice. Finally, the weighting of the various sections was questioned, with participants asking which ones would receive the most emphasis. In particular, a change to the scoring system for the medication organization task was suggested.
General Comments
Participants also identified themes related to the instrument in general, rather than its individual sections (Table 1). Overall, participants felt that the greatest benefit of the tool was its objectivity and the hands-on nature of the assessment. It was felt that recommendations based on concrete scores and information would be received and implemented more readily by patients and their families than more subjective recommendations. Recommended enhancements were the inclusion of other dosage forms (e.g., inhalers and injectables) and lifestyle questions (e.g., sleep patterns and eating habits). All participants, particularly pharmacists in community practice, expressed a concern about the time that would be required for a pharmacist to complete the assessment. Pharmacy students were confident that they would be able to administer the assessment, if given some practice.
Pharmacists’ Ratings of the Tool
Interview participants used a 7-point scale to rate the SMAT for its usefulness, thoroughness, and ease of use and to rate their willingness to use the tool (Table 2). One-sample t tests indicated that respondents rated the SMAT significantly higher than the midpoint on the scale in terms of usefulness, thoroughness, and willingness to use (Table 2). The percentage of participants rating the SMAT at the top 2 scores on the scale (i.e., 6 or 7 out of 7) for each item was also determined: 70% (14/20) for usefulness, 35% (7/20) for ease of use, 60% (12/20) for thoroughness, and 55% (11/20) for willingness to use. In exploratory analyses, the overall sample was subdivided according to practice setting: hospital (n = 12) and community (n = 7) (1 pharmacist worked in neither setting). Independent group t tests used to compare the ratings of these 2 groups showed a tendency for pharmacists and pharmacy students working in hospital settings to be more willing to use the SMAT than those working in community settings (p = 0.08, effect size [η2] = 0.17).
Table 2.
Ratings of the Self-Medication Assessment Tool
| Sample | Usefulness | Thoroughness | Ease of Use | Willingness to Use |
|---|---|---|---|---|
| Full sample (n = 20) | ||||
| Mean (SD) | 5.9 (1.1) | 5.6 (1.1) | 3.5 (1.7) | 5.3 (1.7)* |
| Range | 3–7 | 3–7 | 1–6 | 1–7 |
| Result on t test† | 9.27 (p < 0.001) | 8.46 (p < 0.001) | 0.13 (p = 0.89) | 4.44 (p < 0.001) |
| Working in hospital (n = 12) | ||||
| Mean (SD) | 5.8 (1.2) | 5.6 (1.2) | 3.7 (1.6) | 5.8 (1.3) |
| Range | 3–7 | 3–7 | 1–6 | 3–7 |
| Working in the community (n = 7) | ||||
| Mean (SD) | 6.3 (0.95) | 5.9 (1.2) | 3.3 (2.0) | 4.4 (2.2) |
| Range | 5–7 | 4–7 | 1–6 | 1–7 |
| Result on t test‡ | 0.95 (p = 0.35) | 0.49 (p = 0.64) | 0.46 (p = 0.65) | 1.9 (p = 0.08) |
SD = standard deviation.
n = 19 because one participant did not answer the question.
Means were compared with the midpoint of the 7-point scale using a 1-sample t test.
Mean ratings for pharmacists and students working in hospital settings were compared with mean ratings for those working in community pharmacies. One participant did not indicate location of practice.
DISCUSSION
Interviews and a questionnaire were used to evaluate the face validity of the SMAT, an instrument that incorporates evidence-based components to determine functional, cognitive, and recall capabilities, as well as self-reported adherence and purposeful nonadherence. The study presented here is the first phase of a larger project, the second phase of which involved determining the psychometric properties of the SMAT in a patient cohort (manuscript in preparation). For the second phase of the project, the researchers modified the tool according to several of the recommendations arising from the current study (Online Appendix 2, www.cjhp-online.ca/index.php/cjhp/issue/view/75).
Discussions during the group and individual interviews focused on evaluations of the different sections of the tool, and in some cases participants made specific suggestions for modifying the tool. For the section on functional ability, a common concern was the use of 10-point type on one of the labels. Several participants felt that this font size was quite small, but they were unsure of the font sizes used in community pharmacies. The investigators subsequently determined that prescription bottles used in community practice often carry type that is smaller than 10-point, and the original labels used in the SMAT were retained.
Few comments were made about the colours used in the colour-identification task, other than inquiries about how the tablets would be packaged. The lack of comments for this task was unexpected, because colour perception is important to medication adherence, and we anticipated that participants would identify concerns in this area. Colour vision changes with advancing age,13–19 and cognition may also play a role in an individual’s ability to recognize colours.20 The inability to perceive certain colours may present a barrier to self-medication and should be considered when recommending adherence aids. Therefore, in the modified version of the SMAT (see Online Appendix 2, at www.cjhp-online.ca/index.php/cjhp/issue/view/75), the importance of colour recognition was increased, with patients being tested on their ability to recognize the colour of 10 tablets (with the selection of colours being based on a review of the colour perception literature): white (presented twice), pale yellow, dark yellow, pale green, dark green, pale blue, dark blue, pale purple, and dark purple.
Some participants expressed concerns about the subjectivity involved in assessing hearing, vision, and swallowing deficits. These evaluations were therefore removed from the formal scoring system, although the pharmacist administering the SMAT is encouraged to consider these issues when making recommendations for adherence aids.
On the basis of their clinical experience, the participants in this study strongly endorsed the dosette-filling task in the cognitive assessment, although some proposed that the use of 3 vials created a task that was too complex for elderly patients. In a recently published survey of pillbox use in a sample of community-dwelling older adults, 93% of participants were able to fill pillboxes themselves with an average (± standard deviation) of 6.8 ± 3.4 medications.21 Given the frequency of complex regimens in this population, the research team felt it was important to continue using 3 test medications for this task. However, the scoring systems for the organization and dosette-filling tasks were modified on the basis of interview feedback. Specifically, each medication is now rated individually, rather than testers being asked to provide a combined score for all 3 medications. This change has accomplished the dual objectives of giving more weight to these important skills and simplifying the scoring system for cases in which the patient can manage 1 medication but has difficulty with 2 or more medications.
Participants requested clarification of the source of the reference drug list. The reference drug list is key to the recall, self-reported adherence, and purposeful nonadherence sections of the tool. The drug list is compiled using a process established by the Safer Healthcare Now! initiative22 and is based on multiple sources, including the patient’s prescription containers, community pharmacy and hospital records, and interviews with the patient and/or family members.
In considering the recall section, participants stated that asking patients to describe their medications is an important aspect of the SMAT. Indeed, patients who understand their disease, the need for treatment, and the role of their medications are generally more likely to adhere to medication regimens.23 Evidence is also available that the ability to recall one’s own medication regimen is associated with the Mini Mental State Examination (MMSE) score and that a decline may predict the need for future assistance with medication self-management, as well as other aspects of daily living.9,10,24 As shown with the BMQ tool, recall screening can be highly sensitive to sporadic noncompliance.11 The issue of how to phrase recall questions was addressed by many interviewees in the present study. In the SMAT, recall is scored on the basis of a description of the medication, its name, and the relevant indication. A fourth identifier, “drug strength”, was changed to “dosage” in the modified version of the tool, such that patients receive a point for reporting the number of tablets used.
In general, participants in this study judged that the SMAT provided a thorough assessment of a patient’s ability to manage oral medications. This view, coming from a diverse group that included both pharmacists and students, seems particularly compelling. However, participants in all focus groups suggested that a complete picture of medication management abilities would require assessment of inhaled, injectable, and topical medications. Unfortunately, the inclusion of more complex medication systems would reduce the general usability of the instrument. Nonetheless, the dexterity tasks in the functional section of the SMAT may provide information that is applicable to multiple dosage forms. For example, reduced hand strength (as well as male sex and MMSE score < 24) has been identified as a predictor of non-adherence in older adults with chronic obstructive pulmonary disease who use metered dose inhalers.25 In phase 2 of this project, measures of manual dexterity and cognitive ability in older adults, as well as scores on the Medication Complexity Index,26 will be related to SMAT scores.
Despite the lack of statistical power with the small sample used in this study, the results of the survey support the findings of the content analysis. Specifically, respondents were overall very satisfied with the SMAT and rated it highly in terms of usefulness and thoroughness; they also expressed strong willingness to use the instrument. Exploratory analyses (which admittedly also had small samples) revealed that pharmacists working in hospital settings may be more willing to use the SMAT than those working in community settings. This preliminary finding must be replicated with a larger sample before firm conclusions can be drawn. However, if replicated, this finding may be related to concerns expressed in the interviews about the anticipated amount of time needed to administer the tool. Specifically, these differences between groups may be related to multiple factors such as staffing, the role of pharmacy technicians, the availability of private areas for patient interviews, and access to patients’ diagnostic and laboratory information.27
CONCLUSIONS
The results from focus group and individual interviews confirmed adequate levels of face validity and usability for the new SMAT. This evaluation by practising pharmacists allowed the researchers to modify the tool for use in phase 2 of this project, which will determine concurrent validity, test–retest reliability, and inter-rater reliability in a geriatric population. Widespread adoption of this comprehensive self-medication assessment instrument has the potential to identify elderly patients at risk of problems in self-management of medications. It would allow hospital and community pharmacists, physicians, and other health care providers to implement interventions that would reduce the risk of medication misadventures. The usefulness of the SMAT as perceived by other health professionals such as home care nurses would be an interesting avenue for future research.
Acknowledgments
The authors would like to thank the Medbuy Research, Education and Development Fund and the Friends of the Moncton Hospital for funding support. The authors are also grateful to the pharmacists and pharmacy students who agreed to participate in the study.
Online Appendix 1. Questionnaire used for face validity ratings of the Self-Medication Assessment Tool (SMAT)
Online Appendix 2. Updated version of Self-Medication Assessment Tool.
References
- 1.Meyer ME, Schuna AA. Assessment of geriatric patients’ functional ability to take medication. DICP. 1989;23(2):171–174. doi: 10.1177/106002808902300214. [DOI] [PubMed] [Google Scholar]
- 2.Maddigan SL, Farris KB, Keating N, Wiens CA, Johnson JA. Predictors of older adults’ capacity for medication management in a self-medication program: a retrospective chart review. J Aging Health. 2003;15(2):332–352. doi: 10.1177/0898264303251893. [DOI] [PubMed] [Google Scholar]
- 3.Levy HB. Self-administered medication-risk questionnaire in an elderly population. Ann Pharmacother. 2003;37(7):982–987. doi: 10.1345/aph.1C305. [DOI] [PubMed] [Google Scholar]
- 4.Schepers GP, Won HK, Bieliauskas LA, Galecki AT, Kogikyan RV. A long-term-care setting pilot study evaluating predictors of success in medication self-administration. J Am Med Dir Assoc. 2000;1(3):103–108. [PubMed] [Google Scholar]
- 5.Pereles L, Romonko L, Murzyn T, Hogan D, Silvius J, Stokes E, et al. Evaluation of a self-medication program. J Am Geriatr Soc. 1996;44(2):161–165. doi: 10.1111/j.1532-5415.1996.tb02433.x. [DOI] [PubMed] [Google Scholar]
- 6.Palmer HM, Dobson KS. Self-medication and memory in an elderly Canadian sample. Gerontologist. 1994;34(5):658–664. doi: 10.1093/geront/34.5.658. [DOI] [PubMed] [Google Scholar]
- 7.Ruscin JM, Semla TP. Assessment of medication management skills in older outpatients. Ann Pharmacother. 1996;30(10):1083–1088. doi: 10.1177/106002809603001003. [DOI] [PubMed] [Google Scholar]
- 8.Gray SL, Mahoney JE, Blough DK. Medication adherence in elderly patients receiving home health services following hospital discharge. Ann Pharmacother. 2001;35(5):539–545. doi: 10.1345/aph.10295. [DOI] [PubMed] [Google Scholar]
- 9.Edelberg HK, Shallenberger E, Wei JY. Medication management capacity in highly functioning community-living older adults: detection of early deficits. J Am Geriatr Soc. 1999;47(5):592–596. doi: 10.1111/j.1532-5415.1999.tb02574.x. [DOI] [PubMed] [Google Scholar]
- 10.Edelberg HK, Shallenberger E, Hausdorff JM, Wei JY. One-year follow-up of medication management capacity in highly functioning older adults. J Gerontol A Biol Sci Med Sci. 2000;55(10):M550–M553. doi: 10.1093/gerona/55.10.m550. [DOI] [PubMed] [Google Scholar]
- 11.Svarstad BL, Chewning BA, Sleath BL, Claesson C. The brief medication questionnaire: a tool for screening patient adherence and barriers to adherence. Patient Educ Couns. 1999;37(2):113–124. doi: 10.1016/s0738-3991(98)00107-4. [DOI] [PubMed] [Google Scholar]
- 12.Krueger RA, Casey M. Focus groups: a practical guide for applied research. Thousand Oaks (CA): Sage Publications; 2009. [Google Scholar]
- 13.Faubert J. Visual perception and aging. Can J Exp Psychol. 2002;56(3):164–176. doi: 10.1037/h0087394. [DOI] [PubMed] [Google Scholar]
- 14.Wijk H, Berg S, Bergman B, Hanson AB, Sivik L, Steen B. Colour perception among the very elderly related to visual and cognitive function. Scand J Caring Sci. 2002;16(1):91–102. doi: 10.1046/j.1471-6712.2002.00063.x. [DOI] [PubMed] [Google Scholar]
- 15.Wijk H, Berg S, Sivik L, Steen B. Color discrimination, color naming and color preferences in 80-year olds. Aging (Milano) 1999;11(3):176–185. [PubMed] [Google Scholar]
- 16.Cho NC, Poulsen GL, Ver Hoeve JN, Nork TM. Selective loss of S-cones in diabetic retinopathy. Arch Ophthalmol. 2000;118(10):1393–1400. doi: 10.1001/archopht.118.10.1393. [DOI] [PubMed] [Google Scholar]
- 17.Felius J, de Jong LA, van den Berg TJ, Greve EL. Functional characteristics of blue-on-yellow perimetric thresholds in glaucoma. Invest Ophthamol Vis Sci. 1995;36(8):1665–1674. [PubMed] [Google Scholar]
- 18.Fiorentini A, Porciatti V, Morrone MC, Burr DC. Visual ageing: unspecific decline of the responses to luminance and colour. Vision Res. 1996;36(21):3557–3566. doi: 10.1016/0042-6989(96)00032-6. [DOI] [PubMed] [Google Scholar]
- 19.Phipps JA, Guymer RH, Vingrys AJ. Loss of cone function in age-related maculopathy. Invest Ophthamol Vis Sci. 2003;44(5):2277–2283. doi: 10.1167/iovs.02-0769. [DOI] [PubMed] [Google Scholar]
- 20.Wijk H, Berg S, Sivik L, Steen B. Colour discrimination, colour naming and colour preferences among individuals with Alzheimer’s disease. Int J Geriat Psychiatry. 1999;14(12):1000–1005. [PubMed] [Google Scholar]
- 21.Gould ON, Todd L, Irvine-Meek J. Adherence devices in a community sample: How are pillboxes used? Can Pharm J. 2009;142(1):28–35. [Google Scholar]
- 22.Medication reconciliation (acute care) 2008Safer Healthcare Now! [website] Edmonton (AB)Canadian Patient Safety Institute; [cited 2009 Apr 3]. Available from: www.saferhealthcarenow.ca/EN/Interventions/medrec_acute [Google Scholar]
- 23.MacLaughlin EJ, Raehl CL, Treadway AK, Sterling TL, Zoller DP, Bond CA. Assessing medication adherence in the elderly: Which tools to use in clinical practice? Drugs Aging. 2005;22(3):231–255. doi: 10.2165/00002512-200522030-00005. [DOI] [PubMed] [Google Scholar]
- 24.Raehl CL, Bond CA, Woods T, Patry RA, Sleeper RB. Individualized drug use assessment in the elderly. Pharmacotherapy. 2002;22(10):1239–1248. doi: 10.1592/phco.22.15.1239.33473. [DOI] [PubMed] [Google Scholar]
- 25.Gray SL, Williams DM, Pulliam CC, Sirgo MA, Bishop AL, Donohue AF. Characteristics predicting incorrect metered-dose inhaler technique in older subjects. Arch Intern Med. 1996;156(9):984–988. [PubMed] [Google Scholar]
- 26.George J, Phun YT, Bailey MJ, Dong DC, Stewart K. Development and validation of the medication regimen complexity index. Ann Pharmacother. 2004;38(9):1369–1376. doi: 10.1345/aph.1D479. [DOI] [PubMed] [Google Scholar]
- 27.Jones EJM, MacKinnon NJ, Tsuyuki RT. Pharmaceutical care in community pharmacies: practice and research in Canada. Ann Pharmacother. 2005;39(9):1527–1533. doi: 10.1345/aph.1E456. [DOI] [PubMed] [Google Scholar]