Abstract
Context:
Insufficient lower extremity strength may be a risk factor for lower extremity injuries such as noncontact anterior cruciate ligament tears. Therefore, clinicians need reliable instruments to assess strength deficiencies.
Objective:
To assess the intrarater, interrater, intrasession, and intersession reliability of a portable fixed dynamometer in measuring the strength of the hip and knee musculature.
Design:
Crossover study.
Setting:
Sports medicine research laboratory.
Patients or Other Participants:
Three raters (A, B, C) participated in this 2-phase study. Raters A and B tested 11 healthy college graduate students (2 men, 9 women) in phase 1. Raters A and C tested 26 healthy college undergraduate students (7 men, 19 women) in phase 2.
Main Outcome Measure(s):
The dependent variables for the study were hip adductor, hip abductor, hip flexor, hip extensor, hip internal rotator, hip external rotator, knee flexor, and knee extensor peak force.
Results:
The phase 1 intrasession intraclass correlation coefficients for sessions 1, 2, and 3 ranged from 0.88 to 0.99 (SEM = 0.08–3.02 N), 0.85 to 0.99 (SEM = 0.26–3.88 N), and 0.92 to 0.96 (SEM = 0.52–2.76 N), respectively. Intraclass correlation coefficients ranged from 0.57 to 0.95 (SEM = 1.72–13.15 N) for phase 1 intersession values, 0.70 to 0.94 (SEM = 1.42–9.20 N) for phase 2 intrarater reliability values, and 0.69 to 0.88 (SEM = 1.20–8.50 N) for phase 2 interrater values.
Conclusions:
The portable fixed dynamometer showed good to high intrasession and intersession reliability values for hip and knee strength. Intrarater and interrater reliability were fair to high, except for hip internal rotation, which showed poor reliability.
Keywords: isometric activity, lower extremity
Key Points
Except for intersession knee flexion, the Evaluator portable fixed dynamometer provided fair to high intrasession and intersession reliability values for hip and knee strength.
Both the intrarater and interrater reliability ranged from fair to high, except for hip internal rotation, which had poor reliability.
The portable fixed dynamometer permitted adequate assessment of hip and knee strength.
Lower extremity strength deficits may be related to lower extremity injury. Thus, reliable baseline muscular strength measures, specifically at the hip and knee, are essential in helping to establish an athlete's physical readiness after injury. Several groups1–5 have reported lower extremity strength differences at the hip in patients with patellofemoral pain syndrome when compared with asymptomatic controls. In recent investigations, Bolgla et al4 reported that participants with patellofemoral pain syndrome displayed 24% less hip external rotator (ER) and 26% less abductor strength then control participants, whereas Souza and Powers2 reported that individuals with patellofemoral pain syndrome were 15% weaker in the hip abductors (ABs) and 16% weaker in the hip extensors (HEs) than asymptomatic individuals. Researchers6–8 have also reported strength deficits at the knee as compared with both the contralateral limb and matched controls 1 to 2 years after anterior cruciate ligament reconstruction. Depending on the surgical technique used (eg, bone-patellar tendon-bone or biceps semitendinosus) and muscle group (ie, knee flexors [KFs] or knee extensors [KEs]) assessed, researchers have found these differences to be as great as 11% to 25%.7,9 Also, strength deficits at the trunk and hip complex may be risk factors for noncontact anterior cruciate ligament tears.10
However, currently unclear is whether strength deficits are contributory in nature or merely the results of these specific conditions. Some investigators11–13 have theorized that the dynamic trunk and hip stabilizers (ie, the muscles) assist in preventing excessive hip adduction and femoral internal rotation during ambulation and other weight-bearing activities, such as walking, running, and landing from a jump, by providing stability in the frontal and transverse planes. However, few prospective studies involving athletes have been conducted to evaluate the association between lower extremity strength and lower extremity injuries. With regard to injury-related strength deficits, muscular weakness may indicate inadequate rehabilitation.14 Furthermore, injury-related muscular weakness might reflect other muscular issues, such as altered muscle firing patterns, central inhibition, or some other compensatory strategy of the hip musculature.14
Given the need for continued investigation into the role of lower extremity strength and its association with injury and reinjury, assessment methods need to be both accessible and reliable. Researchers have measured lower extremity muscular strength using various isometric,15–18 isotonic,19–22 and isokinetic23–26 methods. These assessments can further be classified into 3 categories: tertiary, secondary, and primary.27
Tertiary methods of assessments represent the highest level of strength testing and include such isokinetic devices as the Primus RS (BTE Technologies, Hanover, MD) and Biodex System 4 (Biodex Medical Systems, Shirley, NY).27 Although these devices are considered by some as the gold standard of strength assessment,28 they present several logistic limitations. Isokinetic testing is often quite expensive, lacks portability, and is not very practical when testing large numbers of athletes in succession during mass preparticipation physical examinations. Secondary methods of assessing strength include such devices as handheld dynamometers. Instruments in this category are mobile, provide objective measures, and require little setup time, making them ideal for testing large numbers of athletes at multiple sites. The primary category is the most basic method of assessment, involving minimal cost, administration time, and instruction. A primary strength assessment method is often used at the site of a practice session or competitive event or in a clinical setting when secondary or tertiary assessment is not feasible. Manual muscle testing is an example of such a method.
Because of the size and cost of isotonic and isokinetic dynamometry and the subjectivity of manual muscle testing, researchers16,29–33 have been experimenting with handheld dynamometers. Although this technique affords the clinician portability and is less expensive than traditional isokinetic devices, it is not without disadvantages.28,34 The high forces required of the clinician to counter the force exerted by the patient (patient-tester, force-counterforce) could be problematic when evaluating the larger muscle groups (such as the quadriceps femoris) of athletes.28,29,35 An inability to stabilize against larger muscle groups could result in a great deal of variability among trials. To address many of the concerns associated with handheld dynamometers, investigators35–37 have advocated portable fixed dynamometry. Nadler et al35 and Scott et al36 found that the dynamometer anchoring system (ie, portable fixed dynamometry) had good to high reliability for certain lower extremity movements, such as hip abduction, hip flexion, and hip extension.35,36 Why the authors did not assess the remainder of the muscle groups of the hip is unclear. The selection of the muscle groups evaluated may be a reflection of system constraints. The portable dynamometer anchoring systems used in the aforementioned studies were custom-designed systems comprising a commercial dynamometer attached to an adjustable mechanical platform.35,36 The total weight of the system was 20 lb (9 kg).35 According to Nadler et al,35 the patent is pending. Currently, we know of only 1 company (BTE Technologies) that commercially produces portable fixed dynamometry platform systems. However, numerous companies produce strain gauges and handheld dynamometers, which can be mounted or attached to a fixed structure such as a wall.
The purpose of our study was to assess the intrarater, interrater, intrasession, and intersession reliability of the portable fixed dynamometer Evaluator (BTE Technologies) on the following lower extremity muscle groups: hip adductors (ADs), ABs, hip flexors (HFs), HEs, hip internal rotators (IRs), ERs, KEs, and KFs. We proposed the following hypotheses: (1) the peak outcome measures recorded by a tester would be reliable across multiple test trials, (2) the peak outcome measures recorded by a tester would be reliable across multiple test sessions, and (3) the peak outcome measures among testers would be reliable across sessions. This study is unique in that we investigated the ability of a portable fixed dynamometer to reliably measure the strength of all muscle groups at the hip and knee. This protocol differed from that of Nadler et al35 and Scott et al,36 who only evaluated ABs, HEs, and HFs. We also evaluated ABs and HEs, along with ADs and HFs in a weight-bearing position. Nadler et al14 cited the inability to test ABs and HEs in a weight-bearing position as a major limitation of their 2002 study, in which they investigated the relationship between lower extremity injury and AB to HE strength ratio in collegiate athletes.
METHODS
Study Design
The study was conducted at a sports medicine research laboratory and consisted of 2 phases in a test-retest design. Phase 1 involved 3 test sessions (days 1, 2, and 3) separated by 1 day. During this phase, raters evaluated participants en masse in succession using a 15-minute staggered timing between participants. We chose this method in order to simulate the time constraints of large-scale preparticipation physical examinations. All volunteers signed up for a test time in the sports medicine research laboratory; the test time was consistent across the testing sessions. In phase 1, we assessed the intrasession and intersession reliability of a novel portable fixed dynamometer, the Evaluator. Testing procedures consisted of seated and standing isometric strength measures. In phase 2, intrarater and interrater reliability were evaluated. Phase 2 of this study involved 2 raters and 2 test sessions (days 1 and 2) separated by 7 days. For phase 2, the participants were tested individually. As in phase 1, all volunteers signed up for a test time in the sports medicine research laboratory; the test time was consistent across the testing sessions. The dependent variables for phases 1 and 2 were peak isometric adduction, abduction, hip flexion, hip extension, hip internal rotation, hip external rotation, knee flexion, and knee extension force. The independent variables for phase 1 were test trial (3 levels: trials 1, 2, and 3) and session (3 levels: day 1, 2, and 3). The independent variables for phase 2 were rater (2 levels: raters A and C) and session (2 levels: days 1 and 2).
The participants represented a sample of convenience and were recruited from a university setting. We collected anthropometric measurements (height, mass, leg length, and tibial length) of all volunteers, who were then instructed to perform a brief 8- to 10-minute lower extremity warm-up on an exercise bicycle.
Each participant was asked to identify the dominant limb, which was used for all tests. Limb dominance was determined by asking the individual which leg he or she would use to kick a soccer ball with maximal-force effort. Exclusion criteria were (1) an anterior cruciate ligament tear within the last 2 years, (2) a lower extremity injury within the past 6 months, or (3) a neurologic disorder. We obtained approval for this study through the university institutional review board for the testing of human subjects. All volunteers read and signed an approved informed consent document.
Raters and Other Participants
Raters
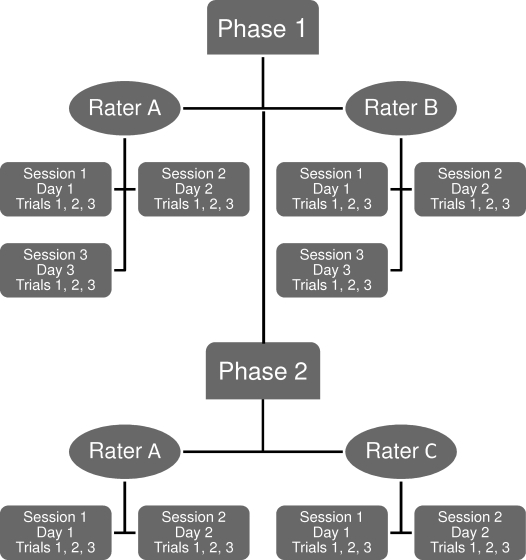
A schematic of the testing sequence for each rater is provided in Figure 1. Raters A and B participated in phase 1 of the study, which evaluated the intrasession and intersession reliability. Rater A assessed only the seated isometric strength protocol, whereas rater B assessed only the standing protocol. Rater A was a 32-year-old male certified athletic trainer with 7 years of clinical experience. Rater B was a 44-year-old female physical therapist with 22 years of clinical experience. Raters A and C participated in phase 2 of the study, which assessed intrarater and interrater reliability. Raters A and C assessed both the seated and standing strength protocols for phase 2 of the study. Rater C was a 29-year-old male doctoral student enrolled in a human movement sciences program. Although rater C had more than 10 years of research experience in biomechanics and exercise science, he was not a licensed allied health professional. All raters in phase 1 and 2 represent a sample of convenience and were selected from a human movement science doctoral program. The training and experience with the device varied among raters. However, all raters received an overview of the basic software functions and testing protocol before the study began. During this time, the raters demonstrated proficiency in both the software operations and testing procedures. Before the start of phase 1, rater A possessed approximately 7 months' experience with the device; rater B received only the stated overview of the basic software functions and testing protocol. Before phase 2 started, rater C had approximately 8 months' experience with the device. We prepared scripted instructions for the participants, which the raters used to explain the requirements of the evaluation to them. The participants received no forms of verbal or visual encouragement other than these instructions. The instructions for the seated strength measures were as follows: “(1) You will receive 1 practice and 3 test trials, (2) You will perform a 5-second contraction with a 10-second rest period, (3) Make sure you give maximum effort, (4) Sit up tall, (5) Arms across your chest, and (6) Begin on the computer's command.” Immediately after item 6 (“Begin on the computer's command”), the rater stated, “Push, push, push,” or “Pull, pull, pull,” depending on the assessment. The instructions for the standing strength measures were similar except for item 4, in which “Sit up tall” was replaced with “Stand up tall.”
Figure 1.
Schematic diagram of testing protocol. In phase 1, rater A assessed hip external rotation and internal rotation and knee flexion and extension, and rater B assessed hip adduction, abduction, flexion, and extension. In phase 2, raters A and C assessed hip adduction, abduction, flexion, extension, internal rotation, and external rotation and knee flexion and extension. Each measure consisted of 3 trials of 5 seconds.
Participants
Thirty-seven participants were recruited for this study and tested in two distinct phases. In phase 1, 11 healthy college graduate students (2 men, 9 women) enrolled in a university postcertification graduate athletic training program were tested. In phase 2, 26 healthy college undergraduate students (7 men, 19 women) were recruited from a university exercise science department for the study.
Instrumentation
All measurements consisted of 3 separate maximum isometric contractions, each 5 seconds in duration, for each muscle group. Each participant received a 10-second rest period between trials. A 10% maximum coefficient of variance was set to ensure a consistent effort by participants in each trial.38,39 If the 3 test trials had a coefficient of variance that was greater than 10%, the low trial (ie, the trial with the worst score) was selected and repeated. All seated measures were assessed using the Evaluator Software System (BTE Technologies) and accompanying hardware, specifically a load cell designed to measure both compression and tensile forces. For the seated measures, the mechanical augmentation of the device allowed tensile force to be measured by enabling opposing forces to be clipped to the load cell. One end of the load cell was attached to an adjustable quick draw, tested at 25 kN, which was attached to a wall. The opposite end of the load cell was attached to an ankle strap proximal to the medial malleolus of the dominant leg (Figure 1). The load cell was interfaced to a laptop computer via a data acquisition box. All standing measures were assessed on a portable platform system using the Evaluator Software System. The portable platform system had an integrated load cell that was interfaced with a desktop computer via a data acquisition box. An ankle cinch strap attached proximal to the medial malleolus of the dominant leg was also attached to the load cell. Both systems were calibrated within 1% of a 25.5-lb (11.6-kg) certified weight. The load cell was calibrated daily to ensure reliability across sessions.
Procedures
Seated Isometric Strength Protocol
The IR, ER, KF, and KE were assessed with the participant in an upright, seated position. The hip and knee of the test extremity were placed in 90° of flexion, so that the tibia of the test extremity was perpendicular to the floor. The load cell was attached to the appropriate anatomical aspect (anterior, posterior, lateral, or medial) of the lower leg proximal to the medial malleolus via an ankle cinch strap. The participant was then instructed to push or pull in the direction opposite the attachment of the load cell (Figure 2).
Figure 2.

Seated strength protocol.
Standing Isometric Strength Protocol
The ADs, ABs, HFs, and HEs were assessed with the participant in a standing position. He or she was placed in standing position with the feet shoulder-width apart and the load cell attached to the appropriate anatomical aspect (anterior, posterior, lateral, or medial) of the lower leg proximal to the medial malleolus via an ankle cinch strap. The participant was then instructed to push or pull in the direction opposite the attachment of the load cell (Figure 3).
Figure 3.
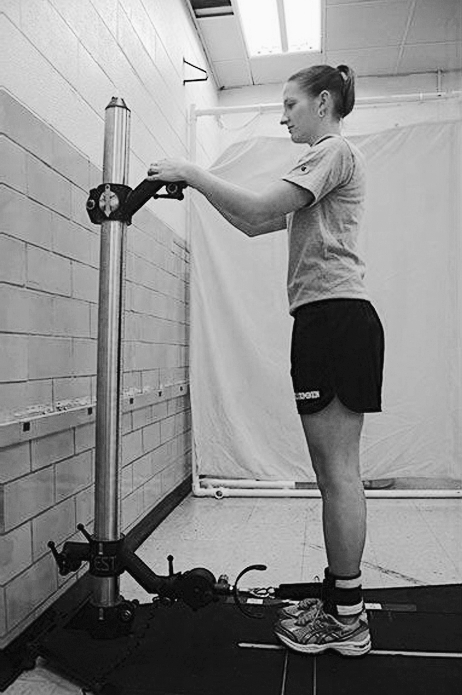
Standing strength protocol.
Statistical Analysis
We collected the force measures in pounds and later converted them to newtons for publication. The raw data collected from both the seated and standing movements were analyzed via intraclass correlation coefficient (ICC). For phase 1 of the study, the intrasession and intersession reliabilities were calculated using an ICC (3,1). For phase 2, the intrarater and interrater reliabilities were also calculated using an ICC (3,1). The aforementioned ICC models were selected in accordance with the criteria set forth by Shrout and Fleiss.40 The ICCs were interpreted according to the criteria set forth by Myers and Blesh41: high reliability, 0.90 to 0.99; good reliability, 0.80 to 0.89; fair reliability, 0.70 to 0.79; poor reliability, 0.60 to 0.69. The α level was set a priori at P ≤ .05. The SEM was calculated for each measure:
In this study, the unit for the SEM was newtons. We used SPSS (version 15; SPSS Inc, Chicago, IL) to analyze the data.
RESULTS
Participant Demographics
Thirty-seven participants were included in this study and tested in 2 distinct phases. Phase 1 consisted of 11 healthy participants (men: age = 22.5 ± 0.70 years, height = 179 ± 1.79 cm, mass = 99.34 ± 19.88 kg; women: age = 23.44 ± 1.01 years, height = 166 ± 5.97 cm, mass = 65.26 ± 9.67 kg). Phase 2 consisted of 26 healthy participants (men: age = 22.00 ± 1.82 years, height = 176 ± 7.46 cm, mass = 75.82 ± 9.25 kg; women: age = 21.16 ± 2.24, height = 164 ± 6.83 cm, mass = 62.68 ± 11.06 kg).
Phase 1
Intrasession Reliability
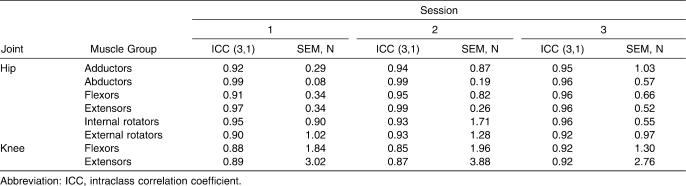
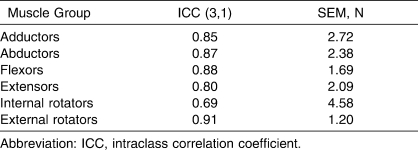
The intrasession ICCs for sessions 1, 2, and 3 ranged from 0.88 to 0.99 (SEM = 0.08–3.02 N), 0.85 to 0.99 (SEM = 0.19–3.88 N), and 0.92 to 0.96 (SEM = 0.52–2.76 N), respectively (Table 1).
Table 1.
Intrasession Reliability Values for Phase 1
Intersession Reliability
The intersession ICCs ranged from 0.43 to 0.76 (SEM = 2.24–13.15 N; Table 2).
Table 2.
Intersession Reliability Values for Phase 1 (Hip Joint)
Phase 2
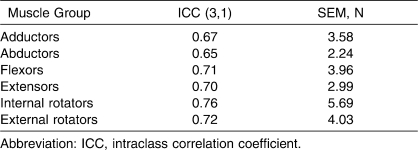
Intrarater Reliability
The intrarater ICCs values for rater A ranged from 0.70 to 0.94 (SEM = 1.42–9.20 N; Table 3).
Table 3.
Intrarater Reliability Values, Rater A (Hip Joint)
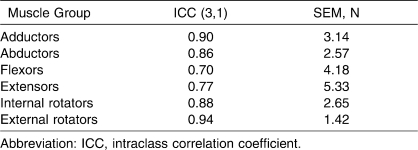
Interrater Reliability
The interrater ICCs between raters A and C ranged from 0.69 to 0.91 (SEM = 1.20–8.50 N; Table 4).
Table 4.
Interrater Reliability Values, Raters A, B, and C (Hip Joint)
DISCUSSION
The results of this study provide support for our hypotheses in that the peak outcome measures recorded by the testers were (1) reliable across multiple test trials, (2) reliable across multiple test sessions with the exception of KFs, and (3) reliable between testers across multiple test sessions. The HF and HE muscle groups showed the weakest ICC values for intrarater reliability (0.70, SEM = 4.18 N, and 0.77, SEM = 5.33 N, respectively), whereas the ICC values for the remainder of the hip and knee muscle groups ranged from 0.86 to 0.94 (SEM = 1.42 to 9.20 N), with the highest values reported for ERs at 0.94 (SEM = 1.42 N).
Our HF measures were lower than those reported by Scott et al,36 who noted ICC values of 0.87 and 0.85. The disparity in these results may reflect difference in testing positions. Scott et al36 used a seated testing protocol, whereas we used a standing protocol. The seated testing position used by Scott et al36 may have allowed for better standardization across multiple trials. However, Nadler et al,14 who used an identical seated testing position to that of Scott et al,36 cited a limitation of the dynamometer anchoring system as the inability of the device to test the ABs and HEs in a more functional weight-bearing position. Although the weight-bearing position may be more functional, it appears that the seated position used by Scott et al36 was a more reliable testing position for HFs. The seated testing position may help to control any unwanted accessory motion at the hips and trunk by the participant during testing, producing more reliable results. When using standing testing protocols, the clinician must ensure that the participant is performing the task in an erect position, with upper body motion minimized and the person's stabilization maintained. However, we chose the standing HF task because of its ease of setup and similarity in testing position to AD, AB, and HE assessments, allowing for rapid test times. Hand positioning may have accounted for varied measures among trials and sessions. For the standing measures, participants were permitted to use the upright as a means of stabilization by grasping it with the near hand, which may have been a means of generating more force. Although the raters instructed the participants not to push or pull in attempts to generate more force, this possibility remains a limitation of the study. We chose to measure AD, AB, HF, and HE strength in standing position because it more closely mimics functional weight-bearing activities, but given the difficulty in measuring hip internal-external rotator and knee flexor-extensor strength in standing position, we opted for a seated testing protocol. We based the decision to use standing or seated position on 2 considerations: (1) the ability to collect strength data with a given protocol and (2) the ability to test multiple participants in succession quickly and easily using a single tester.
Scott et al36 also assessed the intrarater reliability of ABs and HEs, noting results similar to ours. Rater A in our study obtained AB and HE ICC values of 0.86 (SEM = 2.57 N) and 0.77 (SEM = 5.33 N), respectively, using the Evaluator standing protocol. Tester A in Scott et al36 noted AB and HE intrarater ICC values of 0.84 and 0.59, whereas tester B recorded values of 0.76 and 0.72.
The interrater ICC values ranged from 0.69 to 0.91 (SEM = 1.20–8.50 N), with the lowest value seen for IRs (0.69, SEM = 4.58 N). Interestingly, the highest values were reported for ERs (0.91, SEM = 1.20 N). These results may reflect the difference in the clinical experiences between raters A and C. Although the same testing position was used for both IRs and ERs, slight variations in joint positioning during the IR testing setup between raters may have led to the poor values (ICC < 0.70). Failure of the rater to note excessive accessory motion at the hip or knee may have led to slight variations in joint positioning during the IR measures between raters and the poor values (ICC < 0.70). This accessory motion may have altered joint positioning such that the shank (tibia-fibula) placement was not perpendicular to the floor (ie, in neutral hip internal-external rotation) during the actual contraction. Although we recommend the use of a firm medial-lateral thigh stabilizer to minimize transverse-plane motion, we did not use this type of support in our study. In addition, failure to place the shank (tibia-fibula) perpendicular to the floor (ie, in neutral hip internal-external rotation) during the test setup may have also led to variations in joint positioning. Variations in the joint angles between sessions can result in changes to the mechanical advantage and tension of the test musculature, altering force production.37 We did not attempt to quantify joint positioning through goniometric measures, which is a limitation of the study. Hip transverse-plane and knee sagittal-plane positioning was visually determined using the floor as a horizontal plane of reference. By placing the shank in a position perpendicular to the floor, we were able to approximate the hip (neutral internal-external rotation) and knee (90° of flexion) positioning.
The phase 1 intersession values of the raters (rater A: seated protocol, rater B: standing protocol) showed poor to fair reliability (ICC = 0.43 to 0.76) for all measures, with the lowest values reported for AB (ICC = 0.65, SEM = 2.24 N) and KF (ICC = 0.43, SEM = 7.67 N). Nadler et al35 reported higher intersession ICC values for ABs (0.95) and HEs (0.94), but they used side-lying and prone testing positions for abduction and hip extension. Although we chose to evaluate hip abduction and extension in a weight-bearing position, it appears that side-lying abduction and hip extension testing protocols displayed high intersession ICC values (≥0.94). Nadler et al35 did not evaluate KF and KE strength. However, Ford-Smith et al34 reported intersession ICC values for right and left KF strength of 0.83 and 0.82 and for right and left KE strength of 0.90 and 0.88. Our intersession KF and KE ICC values were 0.43 (SEM = 7.67 N) and 0.67 (SEM = 13.15 N). The intrasession reliability of the Evaluator dynamometer for phase 1 of the study, which involved a single tester, displayed good to high reliability values for the hip and knee, ranging from 0.85 to 0.99 (SEM = 0.08 to 3.88 N).
Another limitation to our study is that the use of a 10% coefficient of variance could have skewed the results of the analysis. Of 1279 trials, 30 (2%) were eliminated because the coefficient exceeded the 10% threshold. We chose the 10% value to ensure the participants' consistent efforts among trials because there was no incentive for the participants to provide 100% effort.38,42,43 The coefficient of variance is a measure of absolute reliability and is unaffected by the range of measures of the sample population.44 The value, therefore, provides an indicator of variability among trials, regardless of participants' rankings within the sample population,44 and can be indispensable to clinicians for gauging patient effort and identifying malingerers.
Our results indicate that the design of the Evaluator dynamometer allows for adequate assessment of the lower extremity musculature. The Evaluator's reliability, portability, and rapid testing protocols make it ideal for lower extremity strength assessments during large-scale preparticipation physical examinations, but the results of our study should not be generalized to other raters of similar characteristics because we used a Shrout and Fleiss ICC (3,1) model. Future investigations with randomized selection of raters for intersession, intrasession, intrarater, and interrater reliability are warranted before generalizations can be made. Future authors should also focus on the development of protocols aimed at reliable assessing ankle dorsiflexion, plantar flexion, inversion, and eversion. Lastly, prospective studies are needed to further evaluate the relationship of muscular strength capacity to injury prediction and inform the subsequent development of injury prevention programs.
In order to determine an individual's physical readiness to return to play after injury, objective and reliable baseline strength values are essential. Baseline strength values provide a clinician with a point of comparison when establishing return-to-play criteria. Our study is one of the few to evaluate all the muscle groups at the hip and knee and to assess the strength of the ADs, ABs, HFs, and HEs in a weight-bearing position. From our findings, it appears that the weight-bearing measures provide good interrater reliability for ABs (ICC = 0.87, SEM = 2.38 N) and HF (ICC = 0.88, SEM = 1.69). The more functional weight-bearing position also displayed good to high intrarater reliability values for ADs (ICC = 0.90, SEM = 3.14 N) and ABs (ICC = 0.86, SEM = 2.57 N), with fair values for HEs (ICC = 0.77, SEM = 5.33 N). Given these results, we recommend the more functional weight-bearing testing position for these specific measures.
This study also demonstrated that it is possible to assess the strength of all hip and knee muscle groups in a limited amount of time. The mean test time for the seated strength measures for sessions 1 and 2 of phase 2 ranged from 5 minutes, 13 seconds, to 6 minutes, 23 seconds, whereas the standing measures for sessions 1 and 2 required 6 minutes, 14 seconds, to 6 minutes, 39 seconds. The mean test time for session 1 was 9 minutes, 20 seconds. Finally, the mean test time for session 2 was 8 minutes, 20 seconds. We remind readers that the test times represent only single-limb measures and that total testing times could be as long as 20 minutes. However, the ability of the Evaluator dynamometer to assess lower extremity muscular strength at the hips and knees in approximately 20 minutes makes it ideal for use when evaluating large numbers of athletes in succession.
CONCLUSIONS
The Evaluator dynamometer showed fair to high intrasession and intersession reliability values for hip and knee strength, with the exception of the intersession KF ICC values collected during phase 1. Intrarater and interrater reliability ranged from fair to high except for the IR measure, which showed poor reliability. These results suggest that the design of the Evaluator dynamometer allows for adequate assessment of the lower extremity musculature.
REFERENCES
- 1.Ireland M. L., Willson J. D., Ballantyne B. T., Davis I. M. Hip strength in females with and without patellofemoral pain. J Orthop Sports Phys Ther. 2003;33(11):671–676. doi: 10.2519/jospt.2003.33.11.671. [DOI] [PubMed] [Google Scholar]
- 2.Souza R. B., Powers C. M. Differences in hip kinematics, muscle strength, and muscle activation between subjects with and without patellofemoral pain. J Orthop Sports Phys Ther. 2009;39(1):12–19. doi: 10.2519/jospt.2009.2885. [DOI] [PubMed] [Google Scholar]
- 3.Robinson R. L., Nee R. J. Analysis of hip strength in females seeking physical therapy treatment for unilateral patellofemoral pain syndrome. J Orthop Sports Phys Ther. 2007;37(5):232–238. doi: 10.2519/jospt.2007.2439. [DOI] [PubMed] [Google Scholar]
- 4.Bolgla L. A., Malone T. R., Umberger B. R., Uhl T. L. Hip strength and hip and knee kinematics during stair descent in females with and without patellofemoral pain syndrome. J Orthop Sports Phys Ther. 2008;38(1):12–18. doi: 10.2519/jospt.2008.2462. [DOI] [PubMed] [Google Scholar]
- 5.Piva S. R., Goodnite E. A., Childs J. D. Strength around the hip and flexibility of soft tissues in individuals with and without patellofemoral pain syndrome. J Orthop Sports Phys Ther. 2005;35(12):793–801. doi: 10.2519/jospt.2005.35.12.793. [DOI] [PubMed] [Google Scholar]
- 6.Hiemstra L. A., Webber S., MacDonald P. B., Kriellaars D. J. Contralateral limb strength deficits after anterior cruciate ligament reconstruction using a hamstring tendon graft. Clin Biomech (Bristol, Avon) 2007;22(5):543–550. doi: 10.1016/j.clinbiomech.2007.01.009. [DOI] [PubMed] [Google Scholar]
- 7.Hiemstra L. A., Webber S., MacDonald P. B., Kriellaars D. J. Knee strength deficits after hamstring tendon and patellar tendon anterior cruciate ligament reconstruction. Med Sci Sports Exerc. 2000;32(8):1472–1479. doi: 10.1097/00005768-200008000-00016. [DOI] [PubMed] [Google Scholar]
- 8.Nakamura N., Horibe S., Sasaki S., et al. Evaluation of active knee flexion and hamstring strength after anterior cruciate ligament reconstruction using hamstring tendons. Arthroscopy. 2002;18(6):598–602. doi: 10.1053/jars.2002.32868. [DOI] [PubMed] [Google Scholar]
- 9.Bizzini M., Gorelick M., Munzinger U., Drobny T. Joint laxity and isokinetic thigh muscle strength characteristics after anterior cruciate ligament reconstruction: bone patellar tendon bone versus quadrupled hamstring autografts. Clin J Sport Med. 2006;16(1):4–9. doi: 10.1097/01.jsm.0000188040.97135.43. [DOI] [PubMed] [Google Scholar]
- 10.Claiborne T. L., Armstrong C. W., Gandhi V., Pincivero D. M. Relationship between hip and knee strength and knee valgus during a single leg squat. J Appl Biomech. 2006;22(1):41–50. doi: 10.1123/jab.22.1.41. [DOI] [PubMed] [Google Scholar]
- 11.Leetun D. T., Ireland M. L., Willson J. D., Ballantyne B. T., Davis I. M. Core stability measures as risk factors for lower extremity injury in athletes. Med Sci Sports Exerc. 2004;36(6):926–934. doi: 10.1249/01.mss.0000128145.75199.c3. [DOI] [PubMed] [Google Scholar]
- 12.Hollman J. H., Kolbeck K. E., Hitchcock J. L., Koverman J. W., Krause D. A. Correlations between hip strength and static foot and knee posture. J Sport Rehabil. 2006(1);15:15–23. [Google Scholar]
- 13.Jacobs C. A., Uhl T. L., Mattacola C. G., Shapiro R., Rayens W. S. Hip abductor function and lower extremity landing kinematics: sex differences. J Athl Train. 2007;42(1):76–83. [PMC free article] [PubMed] [Google Scholar]
- 14.Nadler S. F., Malanga G. A., DePrince M., Stitik T. P., Feinberg J. H. The relationship between lower extremity injury, low back pain, and hip muscle strength in male and female collegiate athletes. Clin J Sport Med. 2000;10(2):89–97. doi: 10.1097/00042752-200004000-00002. [DOI] [PubMed] [Google Scholar]
- 15.Meldrum D., Cahalane E., Conroy R., Fitzgerald D., Hardiman O. Maximum voluntary isometric contraction: reference values and clinical application. Amyotroph Lateral Scler. 2007;8(1):47–55. doi: 10.1080/17482960601012491. [DOI] [PubMed] [Google Scholar]
- 16.Bohannon R. W. Isometric strength data. Arch Phys Med Rehabil. 1997;78(5):566–567. doi: 10.1016/s0003-9993(97)90181-7. [DOI] [PubMed] [Google Scholar]
- 17.Andrews A. W., Thomas M. W., Bohannon R. W. Normative values for isometric muscle force measurements obtained with hand-held dynamometers. Phys Ther. 1996;76(3):248–259. doi: 10.1093/ptj/76.3.248. [DOI] [PubMed] [Google Scholar]
- 18.Hogrel J. Y., Payan C. A., Ollivier G., et al. Development of a French isometric strength normative database for adults using quantitative muscle testing. Arch Phys Med Rehabil. 2007;88(10):1289–1297. doi: 10.1016/j.apmr.2007.07.011. [DOI] [PubMed] [Google Scholar]
- 19.Cheng A. J., Rice C. L. Fatigue and recovery of power and isometric torque following isotonic knee extensions. J Appl Physiol. 2005;99(4):1446–1452. doi: 10.1152/japplphysiol.00452.2005. [DOI] [PubMed] [Google Scholar]
- 20.Knapik J. J., Wright J. E., Mawdsley R. H., Braun J. Isometric, isotonic, and isokinetic torque variations in four muscle groups through a range of joint motion. Phys Ther. 1983;63(6):938–947. doi: 10.1093/ptj/63.6.938. [DOI] [PubMed] [Google Scholar]
- 21.Kovaleski J. E., Heitman R. H., Trundle T. L., Gilley W. F. Isotonic preload versus isokinetic knee extension resistance training. Med Sci Sports Exerc. 1995;27(6):895–899. [PubMed] [Google Scholar]
- 22.Stauber W. T., Barill E. R., Stauber R. E., Miller G. R. Isotonic dynamometry for the assessment of power and fatigue in the knee extensor muscles of females. Clin Physiol. 2000;20(3):225–233. doi: 10.1046/j.1365-2281.2000.00250.x. [DOI] [PubMed] [Google Scholar]
- 23.Cometti G., Maffiuletti N. A., Pousson M., Chatard J. C., Maffulli N. Isokinetic strength and anaerobic power of elite, subelite and amateur French soccer players. Int J Sports Med. 2001;22(1):45–51. doi: 10.1055/s-2001-11331. [DOI] [PubMed] [Google Scholar]
- 24.Deighan M. A., De Ste Croix M. B. A., Armstrong N. Reliability of isokinetic concentric and eccentric knee and elbow extension and flexion in 9/10 year old boys. Isokinet Exerc Sci. 2003;11(2):109–115. [Google Scholar]
- 25.Hill C., Croce R., Miller J., Cleland F. Muscle torque relationships between hand-held dynamometry and isokinetic measurements in children ages 9–11. J Strength Cond Res. 1996;10(2):77–82. [Google Scholar]
- 26.Hsu A. L., Tang P. F., Jan M. H. Test-retest reliability of isokinetic muscle strength of the lower extremities in patients with stroke. Arch Phys Med Rehabil. 2002;83(8):1130–1137. doi: 10.1053/apmr.2002.33652. [DOI] [PubMed] [Google Scholar]
- 27.Kollock R. O., Onate J. A., Van Lunen B. L. Clinical evaluation & testing: assessing muscular strength at the hip joint. Athl Ther Today. 2008;13(2):18–24. [Google Scholar]
- 28.Martin H. J., Yule V., Syddall H. E., Dennison E. M., Cooper C., Aihie Sayer A. Is hand-held dynamometry useful for the measurement of quadriceps strength in older people? A comparison with the gold standard Biodex dynamometry. Gerontology. 2006;52(3):154–159. doi: 10.1159/000091824. [DOI] [PubMed] [Google Scholar]
- 29.Bohannon R. W. Hand-held dynamometry: factors influencing reliability and validity. Clin Rehabil. 1997;11(3):263–264. [PubMed] [Google Scholar]
- 30.Friel K., McLean N., Myers C., Caceres M. Ipsilateral hip abductor weakness after inversion ankle sprain. J Athl Train. 2006;41(1):74–78. [PMC free article] [PubMed] [Google Scholar]
- 31.Krause D. A., Schlagel S. J., Stember B. M., Zoetewey J. E., Hollman J. H. Influence of lever arm and stabilization on measures of hip abduction and adduction torque obtained by hand-held dynamometry. Arch Phys Med Rehabil. 2007;88(1):37–42. doi: 10.1016/j.apmr.2006.09.011. [DOI] [PubMed] [Google Scholar]
- 32.Tyler T. F., McHugh M. P., Mirabella M. R., Mullaney M. J., Nicholas S. J. Risk factors for noncontact ankle sprains in high school football players: the role of previous ankle sprains and body mass index. Am J Sports Med. 2006;34(3):471–475. doi: 10.1177/0363546505280429. [DOI] [PubMed] [Google Scholar]
- 33.Tyler T. F., Nicholas S. J., Mullaney M. J., McHugh M. P. The role of hip muscle function in the treatment of patellofemoral pain syndrome. Am J Sports Med. 2006;34(4):630–636. doi: 10.1177/0363546505281808. [DOI] [PubMed] [Google Scholar]
- 34.Ford-Smith C. D., Wyman J. F., Elswick R. K., Jr, Fernandez T. Reliability of stationary dynamometer muscle strength testing in community-dwelling older adults. Arch Phys Med Rehabil. 2001;82(8):1128–1132. doi: 10.1053/apmr.2001.24291. [DOI] [PubMed] [Google Scholar]
- 35.Nadler S. F., DePrince M. L., Hauesien N., Malanga G. A., Stitik T. P., Price E. Portable dynamometer anchoring station for measuring strength of the hip extensors and abductors. Arch Phys Med Rehabil. 2000;81(8):1072–1076. doi: 10.1053/apmr.2000.7165. [DOI] [PubMed] [Google Scholar]
- 36.Scott D. A., Bond E. Q., Sisto S. A., Nadler S. F. The intra- and interrater reliability of hip muscle strength assessments using a handheld versus a portable dynamometer anchoring station. Arch Phys Med Rehabil. 2004;85(4):598–603. doi: 10.1016/j.apmr.2003.07.013. [DOI] [PubMed] [Google Scholar]
- 37.Gagnon D., Nadeau S., Gravel D., Robert J., Belanger D., Hilsenrath M. Reliability and validity of static knee strength measurements obtained with a chair-fixed dynamometer in subjects with hip or knee arthroplasty. Arch Phys Med Rehabil. 2005;86(10):1998–2008. doi: 10.1016/j.apmr.2005.04.013. [DOI] [PubMed] [Google Scholar]
- 38.Matheson L. How do you know that he tried his best? Reliability crisis in industrial rehabilitation. Ind Rehabil Q. 1988;1(1):11–12. [Google Scholar]
- 39.Matheson L. N., Dakos M. Re-visiting “how do you know he tried his best” …the coefficient of variation as a determinant of consistent effort. 2000. p. 9. http://www.epicrehab.com/FreeResources/CV-and-Effort.pdf. Accessed November 10, 2008.
- 40.Shrout P. E., Fleiss J. L. Intraclass correlations: uses in assessing rater reliability. Psychol Bull. 1979;86(2):420–428. doi: 10.1037//0033-2909.86.2.420. [DOI] [PubMed] [Google Scholar]
- 41.Myers C. R., Blesh T. E. Measurement in Physical Education. New York, NY: Ronald Press Co; 1962. pp. 62–63. [Google Scholar]
- 42.McCleary R. W., Andersen J. C. Test-retest reliability of reciprocal isokinetic knee extension and flexion peak torque measurements. J Athl Train. 1992;27(4):362–365. [PMC free article] [PubMed] [Google Scholar]
- 43.Lechner D. E., Bradbury S. F., Bradley L. A. Detecting sincerity of effort: a summary of methods and approaches. Phys Ther. 1998;78(8):867–888. doi: 10.1093/ptj/78.8.867. [DOI] [PubMed] [Google Scholar]
- 44.Atkinson G., Nevill A. M. Statistical methods for assessing measurement error (reliability) in variables relevant to sports medicine. Sports Med. 1998;26(4):217–238. doi: 10.2165/00007256-199826040-00002. [DOI] [PubMed] [Google Scholar]