Abstract
Context:
Recommendations on the positioning of the tibiofemoral joint during a valgus stress test to optimize isolation of the medial collateral ligament (MCL) from other medial joint structures vary in the literature. If a specific amount of flexion could be identified as optimally isolating the MCL, teaching and using the technique would be more consistent in clinical application.
Objective:
To determine the angle of tibiofemoral joint flexion between 0° and 20° that causes a difference in the slope of the force-strain line when measuring the resistance to a valgus force applied to the joint.
Design:
Cross-sectional study.
Setting:
University research laboratory.
Patients or Other Participants:
Twelve healthy volunteers (6 men, 6 women: age = 26.4 ± 5.6 years, height = 170.9 ± 8.4 cm, mass = 75.01 ± 14.6 kg).
Intervention(s):
Using an arthrometer, we applied a valgus force, over a range of 60 N, to the tibiofemoral joint in 0°, 5°, 10°, 15°, and 20° of flexion.
Main Outcome Measure(s):
Force-strain measurements were obtained for 5 positions of tibiofemoral joint flexion.
Results:
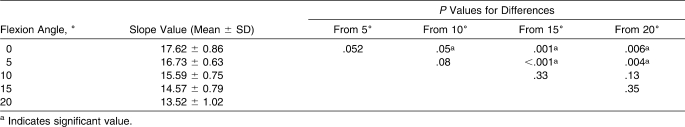
As knee flexion angle increased, slope values decreased (F4,44 = 17.6, P < .001). The slope at full extension was not different from that at 5° of flexion, but it was different from the slopes at angles greater than 10° of flexion. Similarly, the slope at 5° of flexion was not different from that at 10° of flexion, but it was different from the slopes at 15° and 20° of flexion. Further, the slope at 10° of flexion was not different from that at 15° or 20° of flexion. Finally, the slope at 15° of flexion was not different from that at 20° of flexion.
Conclusions:
When performing the manual valgus stress test, the clinician should fully extend the tibiofemoral joint or flex it to 5° to assess all resisting medial tibiofemoral joint structures and again at 15° to 20° of joint flexion to further assess the MCL.
Keywords: knee, collateral ligaments, joint angle, valgus force
Key Points
No difference was noted between the force-strain lines measured in full extension and those measured at 5° and 10° of flexion, but differences were seen at 15° and 20° of flexion.
Resistance to force by the medial joint structures decreased linearly with an increase in joint flexion and was significantly different beyond 15° of flexion.
To assess a medial tibiofemoral joint sprain, the clinician should test the knee between 0° and 10° of flexion to evaluate the medial joint tissues and again at 15° to 20° of flexion to evaluate the medial collateral ligament.
Isolated or combined medial collateral ligament (MCL) ruptures are common tibiofemoral joint injuries in athletic activities.1 A common site of MCL tears is near the femoral insertion, or the posterior proximal region of the joint.2 On examination of a patient with a medial tibiofemoral joint injury, specifically an injury to the MCL, palpation reveals medial knee pain, especially at the site of the injured tissue. The history reveals that the mechanism of injury was a valgus stress caused by a force applied to either the distal portion of the upper leg or the proximal aspect of the lower leg.3–5 This mechanism of injury is supported by strain gauge measurements,4,6 which show that a slightly flexed tibiofemoral joint is a particularly vulnerable position for MCL injury when external rotation and valgus force are applied.7 The severity of injury is based on point tenderness in proximity to the injured tissue, swelling over the anatomical location of the ligament, and the amount of tibiofemoral joint displacement estimated when performing a manual valgus stress test (VST). The VST distinguishes injury to the MCL from injury to the medial meniscus; the latter structure may also be injured with this mechanism.8–10
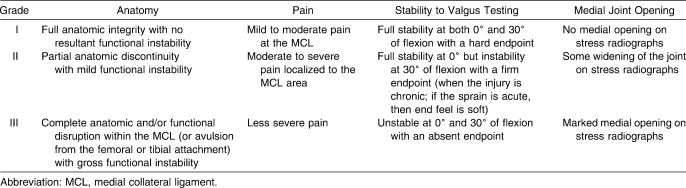
After studying 265 MCL injuries, Fetto and Marshall11 offered a comprehensive grading system of MCL sprains that can be used to make diagnoses and clinical judgments regarding treatment protocols (Table 1). Others9,12,13 have generally agreed with this type of grading scale. Kennedy and Fowler14 went farther by measuring the amount of displacement between the femur and tibia when a valgus force was applied. They found that in normal tibiofemoral joints in full extension, the range of medial laxity was 0.3 to 1.7 mm. When the joint was flexed to 20°, the amount of medial joint displacement was 0.8 to 3.5 mm. We use this grading system in clinical practice when assessing a medial tibiofemoral joint injury and then assigning a grade of severity. When the femur and tibia displace 5 mm or less with the VST, the instability is graded as 1+; 6 to 10 mm, 2+13; and more than 10 mm, 3+.12,15,16
Table 1.
Medial Collateral Ligament Sprain Grading System, as Suggested by Fetto and Marshall11
Ascertaining the amount of displacement between the femur and tibia on the VST to assign a severity grade is difficult. It is also challenging for some clinicians to manually flex the tibiofemoral joint sufficiently while simultaneously applying a valgus stress to the joint. Small hands, clinician inexperience, lack of strength, and controlling hip motion with a flexed knee joint can all contribute to difficulty in performing this test, especially at angles greater than 20° of flexion. Recommendations for tibiofemoral joint positioning during a VST to optimize isolation of the MCL from other medial joint structures vary in the literature.15 Most clinicians agree that the joint should be fully extended and then flexed while applying the manual valgus force, but the amount of flexion is not consistent.15 For example, Grood et al17 stated that to distinguish between the MCL and other structures that support the medial tibiofemoral joint, flexing the joint only 5° decreased input from the posterior structures, which became slack, and at 25° of flexion, the medial capsule was less supportive in resisting valgus stress. However, others15,18 believe that to isolate the MCL, 20° of knee flexion is appropriate. Popular textbooks19–21 used in teaching the VST indicate a range of 20° to 30° of tibiofemoral joint flexion. In reviewing cadaver studies,18,22–24 we found no consensus on one best position in which to perform the VST.
Evaluation of the severity of MCL sprains depends on the expertise of the clinician with regard to the ability to assess the injury given subjective information, such as the mechanism of injury, location and severity of pain, and sensations of instability. In addition, the clinician often needs expertise in performing a more objective special manual test (ie, the VST). The structures being tested in full extension are different from those being tested in some degree of flexion.7,13–15,17,18,25–27 Flexion determines the amount of tissue aligned to resist the imposed force. If a specific amount of flexion could be agreed upon to optimally isolate the medial knee structures, it would make teaching and using the technique more consistent in clinical application. If resistance to a valgus force on the MCL is the same between 5° and 20° of flexion, then the clinician can perform the VST with the tibiofemoral joint in 5° of flexion, which is easier than performing it at 20°. We have found that holding the limb and joint in a small amount of flexion is more manageable than maintaining a larger amount of flexion while applying a valgus stress. In our initial study28 on this topic, we found a difference in the resistance of the medial tibiofemoral joint when measured in full extension and at 20° of flexion using an arthrometer, but we did not determine the specific angle between 0° and 20° at which the slope of the force-strain line differed from extension. The purpose of our current study was to identify the tibiofemoral joint angle between 0° and 20° of flexion at which the slope of the force-strain line differs for the medial knee structures. We did this by applying a valgus stress to the lateral tibiofemoral joint.
METHODS
We used a 1 × 5 factorial design for this study. The independent variable was tibiofemoral positioning during the following measurements: 0°, 5°, 10°, 15°, and 20° of joint flexion. The dependent variable was the slope value of the force-strain line measured over a range of 0 to 60 N of force.
Participants
Twelve healthy and physically active individuals (6 men, 6 women; mean age = 26.4 ± 5.6 years, height = 170.9 ± 8.4 cm, mass = 75.01 ± 14.6 kg) volunteered for our study. We screened them with a medical health questionnaire; only those (1) without previous knee or hip surgery, (2) free of knee injury in the past 6 months, and (3) without pain in the tibiofemoral joint were included. Participants who exercised regularly were asked not to exercise within 1 hour of testing. All volunteers wore shorts to the testing session and were asked to remove the sock and shoe on the limb to be tested.
Before testing began, the institutional review boards at our host institutions approved the study protocol, and we obtained informed consent from all participants.
Instrumentation
We applied a valgus force to the medial tibiofemoral joint while the resistance was calculated and represented by the slope of the force-strain line generated by the software (version 1.33) embedded in a LigMaster arthrometer (Sport Tech Inc, Charlottesville, VA). We28 have reported on repeatability and reliability of this arthrometer in a previous paper.
A dual-channel EMG Retrainer (model BF; Chattanooga Group, Hixson, TN) was used to confirm that the vastus medialis and medial hamstrings muscle bellies surrounding the joint were electrically quiet. We used a standard goniometer (model G 800; Whitehall Manufacturing, City of Industry, CA) to accurately place the tibiofemoral joint in 5 different degrees of flexion.
Procedures
Participants were asked which leg they prefer to use to kick a ball a long distance; this was considered the dominant limb for measurement with the arthrometer. We placed superficial sensors from the EMG Retrainer on the vastus medialis and medial hamstrings muscle bellies to sense muscle activity of the limb measured. Although the tendons, fascia, and medial meniscus might have added passive stiffness to the medial joint, we tried to control for medial hamstrings and quadriceps activity, thereby reducing the influence of dynamic stability during data collection.
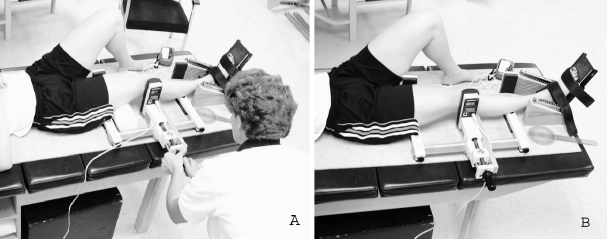
The volunteer was then positioned in the arthrometer and, if the sensor indicated muscle activity, he or she was encouraged to relax the leg being tested. Data were collected only when the biofeedback unit was quiet. The lead author (P.A.A.) positioned and performed all measurements on each volunteer in a single session. Specific positioning has been previously described28 and is shown in Figure 1.
Figure 1.
Limb positioning of the tibiofemoral joint in the arthrometer. The foot plate was used to reduce femoral or tibial rotation (or both) during data collection. Force is applied to the femoral condyle, just superior to the lateral joint line. A, The medial right knee in full extension. B, The same knee is measured in 20° of flexion. A 10.16-cm foam roller was placed under the thigh to promote relaxation of the muscles at the desired angle of joint flexion when each angle was tested. A superficial electromyographic biofeedback device also ensured muscle relaxation during data collection.
We used a Latin square table to counterbalance the order in which the 5 tibiofemoral joint positions were tested. A standard goniometer was used to position the tibiofemoral joint in 5 different degrees of flexion with the participant supine; the center of the fulcrum placed over the lateral epicondyle of the femur; the proximal stationary arm aligned with the lateral midline of the femur, using the greater trochanter of the femur as the bony reference; and the distal movable arm aligned with the lateral midline of the fibula, using the lateral malleolus as the bony reference.29 Foam rollers of different circumferences were placed under the thigh to promote relaxation of the musculature surrounding the joint while maintaining the desired angle between the femur and tibia; for example, a 10.16-cm foam roller held the joint in 20° of flexion (Figure 1).
The valgus force routinely applied by clinicians is unknown, but it is certain to vary. For the purpose of this study, we initially monitored the real-time applied force on the computer screen up to 120 N, but for statistical analysis, data were retrieved for only 60 N. Trials were repeated, typically 3 to 5 times, until 2 trials of slope values within 5% of each other were produced; these were averaged for the statistical analysis. This procedure was used to test the tibiofemoral joint in 0°, 5°, 10°, 15°, and 20° of flexion.
Statistical Analysis
The means and SDs of slope values in our previous study28 were used to calculate the number of participants needed when α was set a priori at P ≤ .05; the power analysis revealed that 11 were needed. We chose to test 12.
We calculated a 1-factor repeated-measures analysis of variance using SPSS (version 14.0; SPSS Inc, Chicago, IL) to determine if differences existed in medial tibiofemoral joint slope values at 5 different degrees of joint flexion. Sidak post hoc pairwise comparisons were calculated to identify where differences existed in the range of angles.
RESULTS
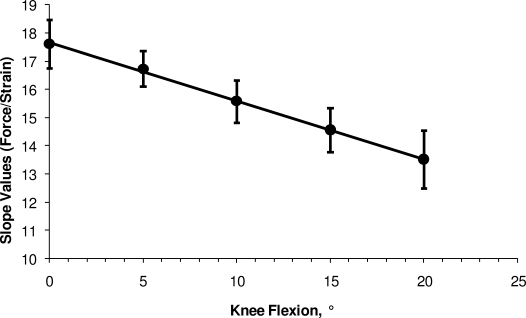
The means and SDs calculated at each of the 5 positions of tibiofemoral joint flexion tested are given in Table 2. Overall results indicated differences in slope values as the degrees of flexion changed (F4,44 = 17.6, P < .001). A partial η2 value of 0.62 indicates a moderate effect size. As the tibiofemoral flexion angle increased, slope values decreased linearly (Figure 2). When Sidak post hoc comparisons were made, further distinctions were evident in slope values among the joint positions (Table 2).
Table 2.
Medial Tibiofemoral Joint Slope Values for Flexion Angles (Measured Over a Range of 0 to 60 N of Force) and P Values for Differences
Figure 2.
The mean slope values measured in 5 knee flexion positions. As the tibiofemoral joint is flexed, the slope values decrease as resistive structures are relaxed. The best-fitting straight line in the plot is expressed by Y = 17.59 − 0.207X.
DISCUSSION
Strain Calculations and Slope Values
Strain is defined as a change in the dimensions of the test sample as a result of the applied force; in our case, an increase in length of the medial structures of the knee as the result of an applied force. The LigMaster arthrometer measures the increase in length and calculates the ensuing strain. The software displays the data as a force-strain relationship on screen. This relationship is linear over the range of 0 to 60 N of force.28
When the applied force is plotted against strain, the slope of the straight line, as observed over the 0-N to 60-N range, is equivalent to the product of the cross-sectional area of all the medial structures subjected to this force and the elastic modulus of these structures. Therefore, when the number of structures to which the force is applied varies as a result of flexing the joint, this product and, therefore, the slope of the line changes accordingly.28 When the medial tibiofemoral joint is examined, especially in full extension, the individual soft tissues act as a unit in resisting the applied force. We noted a decrease in slope values as the joint angle was increased from full extension to 20° of flexion. This finding was expected, because when the tibiofemoral joint is flexed more, fewer tissues are involved in resisting the applied force.6,18,23,24,30 We28 reported the specifics of the mathematics used in the calculations of the slope values in a previous manuscript.
The force-strain relationship according to the arthrometer quantifies and documents the data that we produce when we manually perform a VST on the tibiofemoral joint. The actual displacement is measured in millimeters, similar to and consistent with manually stressing the joint and relating the displacement of the femur and tibia to the grade and severity of the injury to the joint structures. Flexing the joint stretches specific portions of the surrounding soft tissues, especially the layers of the MCL, while creating slack in other structures, as discussed later in this article.
The MCL
The medial tibiofemoral ligaments consist of capsular and noncapsular fibers or layers.15 The MCL consists of 2 layers: the superficial medial layer and the anterior layer, the latter of which blends with the deeper middle capsular fibers.22,31 These fibers form a complex structure that is the primary stabilizer of the medial aspect of the joint. The relative positions of the different fibers of the MCL increase the ligament's ability to resist valgus and external rotation stresses, but this depends upon the amount of knee flexion. Portions of the ligament become slack and taut during motion and, therefore, stabilize the tibiofemoral joint at different angles and joint positions.6,17,18,22,24 In full extension, the MCL moves forward, and both the anterior and posterior portions are taut, preventing valgus joint movement.17,23,24 In fact, the anterior fibers are taut in all degrees of flexion as the MCL moves forward, and they resist valgus motion more than the posterior fibers and capsule, which are slack during flexion.17,22,24 A plot of the slope values against flexion (Figure 2) shows a straight line, exactly as we would expect when the ribbon-like MCL is flexed: the anterior portion is stretched, whereas the posterior portion becomes more slack as the knee flexes. Therefore, to test the entire width of the MCL, the examiner only needs to flex the knee enough to “unlock” the joint (ie, to slacken the posterior knee structures), no more than 5°. By increasing joint flexion to 10° or 20°, one can selectively test the anterior portion of the MCL. Therefore, by testing first at 5° and then at 20°, whether the anterior or posterior part (or both) of the MCL is involved in the injury can be determined. A bilateral assessment at the same degree of flexion validates the left-right comparison for both diagnostic and recovery purposes.28
Cadaver Studies on Strain and the MCL
Researchers18,22–24 have studied the strain properties of the MCL in cadaver limbs. Warren et al22 cut the superficial fibers of the MCL but left intact the deep ligaments, posterior capsule, anterior cruciate ligament (ACL), and posterior cruciate ligament (PCL). They noted increased medial joint opening. Haimes et al23 found that the superficial MCL alone was a restraint against abduction at all flexion angles except 0°. Robinson et al18 showed that the superficial fibers of the MCL loaded evenly when the specimen was oriented at about 20° of knee flexion, whereas the deep fibers were most loaded at 0° of extension. Further, although the posterior fibers had different lengths and orientations, most fibers were tensed when the joint was fully extended.18 In the ACL-deficient knee, the greatest strains to the MCL were observed in 0° to 20° of knee flexion, especially in the central and posterior portions of the MCL.31 Similarly, Arms et al24 found that the posterior long fibers of the MCL demonstrated the greatest increases in strain of all MCL fibers between 15° and 35° of joint flexion. We did not measure the tibiofemoral joint in ACL-deficient participants, and we could not study flexion positions greater than 20° because it was difficult to align the pressure actuator with the lateral joint space when the knee was flexed past 20°. However, our results appear, on the whole, to support these findings: resistance to valgus force decreases at 15° and 20° of knee flexion when fewer structures are involved in resisting the induced strain. Given the information gleaned from cadaveric studies and the limitation of the LigMaster arthrometer, we chose to measure the resistance to valgus force at 5 different angles within the 0° to 20° range. Furthermore, we conclude that at 15° to 20° of knee flexion, the superficial MCL is more isolated from these other supportive structures than it is at lesser degrees of flexion.
Medial Knee Restraint and the VST
Clinicians have routinely examined the medial tibiofemoral joint and MCL via the VST. Early on, in describing the tibiofemoral joint abduction stress test, Hughston13,25 and Hughston et al15 suggested positioning the knee in 30° of flexion to isolate the MCL from the other static medial compartment ligaments and structures. Further, they believed that the test should be repeated in full extension to assess other structures but that it was a mistake to assess the MCL with a valgus force in full extension. Hughston et al15 insisted that in full extension the MCL and ACL could be torn and that the test would still be negative, because the PCL and posterior oblique ligament (not the posterior capsule) were taut, which would resist opening of the joint space.
Kennedy and Fowler14 found that when the tibiofemoral joint was flexed to as little as 20° to 30°, these posterior structures relaxed, and they added that the posterior capsule was integral to stabilization against valgus forces in full extension. We concur with this finding, as we observed a change in slope values on flexing the joint.
Others3 have concurred with Hughston13,25 and Hughston et al15 that the functional integrity of the MCL is best tested in 30° of flexion. Some have preferred to flex the knee to 20°10 or 25°8 for testing collateral stability. From this research, it seems that performing the VST anywhere in a range of 20° to 30° of knee flexion is appropriate. Our findings indicate that when increasing the flexion of the tibiofemoral joint, fewer structures are subjected to the valgus force, but we cannot determine the exact amount of flexion at which the superficial portion of the MCL is optimally isolated. Although we could not study flexion positions greater than 20°, extrapolation of the linear relationship in Figure 2 indicates that at 25° and 30° of tibiofemoral joint flexion, the number of medial structures involved in a valgus stress is even fewer than the number involved at 15° and 20° of joint flexion, representing additional differences in force-restraining abilities. Further research is necessary to confirm or refute this suggestion.
Still other clinicians11,32,33 believed there were good reasons to perform the VST with the tibiofemoral joint in full extension to assess the injured MCL. A small increase in joint displacement at 0° of flexion would indicate complete MCL compromise, whereas gross instability would indicate complete MCL rupture with capsular or ACL rupture,32 and extreme valgus opening would indicate a possible PCL rupture.11 Our study supports the notion that, for diagnostic purposes, it is beneficial to test the medial tibiofemoral joint both in full extension and at up to 10° of flexion manually. Using an arthrometer such as the LigMaster allows the clinician to reliably examine the medial structures up to 20° of flexion.
We tested the tibiofemoral joint of healthy volunteers in this study to best represent MCL integrity. Effusion, spasm, or locking, often present with acute tibiofemoral joint sprains, can prevent full extension and compromise the accuracy and reliability of the VST.11 Our study has demonstrated decreasing force-strain slopes with increased flexion, which is consistent with cadaveric studies that have shown these positional differences and support clinical testing at 5° and 20° of flexion. It is likely that at full extension and 5° and 10° of flexion, essentially the same medial structures are involved, but beyond 10°, the more posterior elements become slack, including the posterior fibers of the MCL itself. It is not possible to determine the degree of flexion at which to best isolate the entire superficial portion of the MCL. The sensitivity and specificity of the VST must be evaluated at different positions in knee-injured patients, with and without independently verified MCL injuries, if one is to make more informed clinical recommendations.
CONCLUSIONS
As the tibiofemoral joint is increasingly flexed, progressively fewer medial structures participate in resisting valgus stress. The observed linear decrease in the number of participating structures is likely to continue beyond 20° of flexion, the upper limit allowed by our equipment. Based on findings by other authors, it appears that the posterior structures are most likely to become slack with increasing flexion. No specific degree of flexion could be determined at which the entire superficial MCL is optimally isolated. However, studies that use computed tomography or magnetic resonance imaging may provide such an answer. We found no statistical difference between the force-strain slopes measured in full extension and at 5° and 10° of flexion; a difference was observed at 15° and 20° of joint flexion. This result is clinically relevant for 2 reasons. First, when a clinician is manually applying a valgus force to assess injury to the medial knee joint structures, complete extension is not required. This fact is relevant because an acute injury to the medial knee may generate joint effusion or tenderness (or both) that could result in the patient's inability to withstand a full-extension position. Second, we demonstrated that resistance to force by the medial joint structures decreases linearly with degree of joint flexion and changes statistically beyond 15° of flexion. Thus, 15° to 20° of flexion may come closer to optimally isolating the superficial portion of the MCL. To assess a medial tibiofemoral joint sprain, the knee should be tested at between 0° and 10° of knee flexion to assess all the medial joint tissues and again at 15° to 20° of flexion to further assess the MCL. By testing first at 5° and then at 20°, the clinician can determine whether the anterior or posterior part or both parts of the MCL are involved in the injury. Identifying the structures that resist valgus stress and testing MCL integrity in the 20° to 30° range of tibiofemoral joint flexion are areas for future research.
Acknowledgments
We thank Lynchburg College and the Foundation for Independent Colleges for financial support to conduct this study and Kevin Lynch for technical assistance.
REFERENCES
- 1.Miyasaka K. C., Daniel D. M., Stone M. L., Hirshman P. The incidence of knee ligament injuries in the general population. Am J Knee Surg. 1991;4(1):3–8. [Google Scholar]
- 2.Lee J. I., Song I. S., Jung Y. B., et al. Medial collateral ligament injuries of the knee: ultrasonographic findings. J Ultrasound Med. 1996;15(9):621–625. doi: 10.7863/jum.1996.15.9.621. [DOI] [PubMed] [Google Scholar]
- 3.LaPrade R. F., Wentorf F. Acute knee injuries: on-the-field and sideline evaluation. Physician Sportsmed. 1999;27(10):55–62. doi: 10.3810/psm.1999.10.1025. [DOI] [PubMed] [Google Scholar]
- 4.Kennedy J. C., Hawkins R. J., Willis R. B. Strain gauge analysis of knee ligaments. Clin Orthop Relat Res. 1977;129:225–229. doi: 10.1097/00003086-197711000-00031. [DOI] [PubMed] [Google Scholar]
- 5.Kennedy J. C., Hawkins R. J., Willis R. B., Danylchuk K. D. Tension studies of human knee ligaments: yield point, ultimate failure, and disruption of the cruciate and tibial collateral ligaments. J Bone Joint Surg Am. 1976;58(3):350–355. [PubMed] [Google Scholar]
- 6.Hull M. L., Berns G. S., Varma H., Patterson H. A. Strain in the medial collateral ligament of the human knee under single and combined loads. J Biomech. 1996;29(2):199–206. doi: 10.1016/0021-9290(95)00046-1. [DOI] [PubMed] [Google Scholar]
- 7.Gardiner J. C., Weiss J. A., Rosenberg T. D. Strain in the human medial collateral ligament during valgus loading of the knee. Clin Orthop Relat Res. 2001;391:266–274. doi: 10.1097/00003086-200110000-00031. [DOI] [PubMed] [Google Scholar]
- 8.Meislin R. J. Managing collateral ligament tears of the knee. Physician Sportsmed. 1996;24(3):67–76. doi: 10.3810/psm.1996.03.1274. [DOI] [PubMed] [Google Scholar]
- 9.Petersen W., Laprell H. Combined injuries of the medial collateral ligament and the anterior cruciate ligament: early ACL reconstruction versus late ACL reconstruction. Arch Orthop Trauma Surg. 1999;119(506):258–262. doi: 10.1007/s004020050405. [DOI] [PubMed] [Google Scholar]
- 10.Hillard-Sembell D., Daniel D. M., Stone M. L., Dobson B. E., Fithian D. C. Combined injuries of the anterior cruciate and medial collateral ligaments of the knee: effect of treatment on stability and function of the joint. J Bone Joint Surg Am. 1996;78(2):169–176. doi: 10.2106/00004623-199602000-00002. [DOI] [PubMed] [Google Scholar]
- 11.Fetto J. F., Marshall J. L. Medial collateral ligament injuries of the knee: a rationale for treatment. Clin Orthop Relat Res. 1978;132:206–218. [PubMed] [Google Scholar]
- 12.Mirowitz S. A., Shu H. H. MR imaging evaluation of knee collateral ligaments and related injuries: comparison of T1-weighted, T2-weighted, and fat-saturated T2-weighted sequences. Correlation with clinical findings. J Magn Reson Imaging. 1994;4(5):725–732. doi: 10.1002/jmri.1880040516. [DOI] [PubMed] [Google Scholar]
- 13.Hughston J. C. The importance of the posterior oblique ligament in repairs of acute tears of the medial ligaments in knees with and without an associated rupture of the anterior cruciate ligament: results of long-term follow-up. J Bone Joint Surg Am. 1994;76(9):1328–1344. doi: 10.2106/00004623-199409000-00008. [DOI] [PubMed] [Google Scholar]
- 14.Kennedy J. C., Fowler P. J. Medial and anterior instability of the knee: an anatomical and clinical study using stress machines. J Bone Joint Surg Am. 1971;53(7):1257–1270. [PubMed] [Google Scholar]
- 15.Hughston J. C., Andrews J. R., Cross M. J., Moschi A. Classification of knee ligament instabilities, part I: the medial compartment and cruciate ligaments. J Bone Joint Surg Am. 1976;58(2):159–172. [PubMed] [Google Scholar]
- 16.Shelbourne K. D., Nitz P. A. The O'Donoghue triad revisited: combined knee injuries involving anterior cruciate and medial collateral ligament tears. Am J Sports Med. 1991;19(5):474–477. doi: 10.1177/036354659101900509. [DOI] [PubMed] [Google Scholar]
- 17.Grood E. S., Noyes F. R., Butler D. L., Suntay W. J. Ligamentous and capsular restraints preventing straight medial and lateral laxity in intact human cadaver knees. J Bone Joint Surg Am. 1981;63(8):1257–1269. [PubMed] [Google Scholar]
- 18.Robinson J. R., Bull A. M. J., Amis A. A. Structural properties of the medial collateral ligament complex of the human knee. J Biomech. 2005;38(5):1067–1074. doi: 10.1016/j.jbiomech.2004.05.034. [DOI] [PubMed] [Google Scholar]
- 19.Prentice W. E. The knee and related structures. Arnheim's Principles of Athletic Training. 13th ed. Boston, MA: McGraw Hill Co; 2009. pp. 654–695. [Google Scholar]
- 20.Shultz S. J., Houglum P. A., Perrin D. H. Knee and thigh. In: Perrin D. H., editor. Examination of Musculoskeletal Injuries. 2nd ed. Champaign, IL: Human Kinetics; 2005. pp. 429–471. [Google Scholar]
- 21.Konin J. G., Wiksten D. L., Isear J. A., Brader H. Special Tests for Orthopedic Examination. 3rd ed. Thorofare, NJ: Slack Inc; 2006. p. 301. [Google Scholar]
- 22.Warren L. F., Marshall J. L., Girgis F. The prime static stabilizer of the medial side of the knee. J Bone Joint Surg Am. 1974;56(4):665–674. [PubMed] [Google Scholar]
- 23.Haimes J. L., Wroble R. R., Grood E. S., Noyes F. R. Role of the medial structures in the intact and anterior cruciate ligament–deficient knee: limits of motion in the human knee. Am J Sports Med. 1994;22(3):402–409. doi: 10.1177/036354659402200317. [DOI] [PubMed] [Google Scholar]
- 24.Arms S., Boyle J., Johnson R., Pope M. Strain measurement in the medial collateral ligament of the human knee: an autopsy study. J Biomech. 1983;16(7):491–496. doi: 10.1016/0021-9290(83)90063-5. [DOI] [PubMed] [Google Scholar]
- 25.Hughston J. C. Knee ligament injury in athletes. J Med Assoc Ala. 1966;36(3):243–251. [Google Scholar]
- 26.Hughston J. C., Eilers A. F. The role of the posterior oblique ligament in repairs of acute medial (collateral) ligament tears of the knee. J Bone Joint Surg Am. 1973;55(5):923–940. [PubMed] [Google Scholar]
- 27.Mommersteeg T. J. A., Blankevoort L., Huiskes R., Kooloos J. G. M., Kauer J. M. G. Characterization of the mechanical behavior of human knee ligaments: a numerical-experimental approach. J Biomech. 1996;29(2):151–160. doi: 10.1016/0021-9290(95)00040-2. [DOI] [PubMed] [Google Scholar]
- 28.Aronson P. A., Rijke A. M., Ingersoll C. D. Bilateral medial tibiofemoral joint stiffness in full extension and 20° of knee flexion. J Athl Train. 2008;43(2):157–163. doi: 10.4085/1062-6050-43.2.157. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Norkin C. C., White D. J. Measurement of Joint Motion: A Guide to Goniometry. Philadelphia, PA: FA Davis Co; 1985. p. 88. [Google Scholar]
- 30.Gardiner J. C., Weiss J. A. Subject-specific finite element analysis of the human medial collateral ligament during valgus knee loading. J Orthop Res. 2003;21(6):1098–1106. doi: 10.1016/S0736-0266(03)00113-X. [DOI] [PubMed] [Google Scholar]
- 31.Sullivan D., Levy I. M., Sheskier S., Torzilli P. A., Warren R. F. Medial restraints to anterior-posterior motion of the knee. J Bone Joint Surg Am. 1984;66(6):930–936. doi: 10.2106/00004623-198466060-00015. [DOI] [PubMed] [Google Scholar]
- 32.Moeller J. L., Lamb M. M. Anterior cruciate ligament injuries in female athletes: why are women more susceptible? Physician Sportsmed. 1997;25(4):31–54. doi: 10.3810/psm.1997.04.1272. [DOI] [PubMed] [Google Scholar]
- 33.Lonergan K. T., Taylor D. C. Medial collateral ligament injuries of the knee: an evolution of surgical reconstruction. Tech Knee Surg. 2002;1(2):137–145. [Google Scholar]