Abstract
This study evaluated the psychometric properties of the ADHD Stigma Questionnaire (ASQ) among a community sample of 301 adolescents ages 11–19 years at high (n = 192) and low risk (n = 109) for attention deficit hyperactivity disorder (ADHD). Study subjects were drawn from a cohort study assessing ADHD detection and service use. The 26-item ASQ demonstrated good internal consistency. Confirmatory factor analysis using random parceling supported a three factor structure with highly correlated subscales of Disclosure Concerns, Negative Self Image, and Concern with Public Attitudes, and a Schmid-Leiman analysis supported an overall stigma factor. Test-retest stability was assessed after two-weeks (n = 45) and found to be adequate for all three subscales. Construct validity was supported by relationships with related constructs, including clinical maladjustment, depression, self-esteem and emotional symptoms and the absence of a relationship with school maladjustment. Findings indicate that the ASQ has acceptable psychometric properties in a large community sample of adolescents, some of whom met DSM-IV criteria for ADHD.
Keywords: Attention deficit hyperactivity disorder, Validity, Reliability, Factor structure, Community sample, Disclosure concerns, Self stigma, Public stigma
1. Introduction
The Surgeon General identifies stigma surrounding mental illness and its treatment as a potent barrier to help-seeking (U.S. Department of Health and Human Services, 1999). A review of population-based studies highlighted the extent to which stigma surrounds mental illness (Angermeyer and Dietrich, 2006); however, this review also demonstrates that stigma associated with many mental illnesses has been understudied, since most stigma research has focused on depression, schizophrenia, and bipolar disorder. Furthermore, stigma exists at various levels; persons with mental illness not only encounter public stigma, expressed as prejudice and discrimination, but may also suffer from self-stigma, through acceptance of the prejudices that surround them (Ruesch et al., 2005), and their families or intimates may experience courtesy stigma based on kinship or affiliation with the stigmatized person (Goffman, 1963).
A recent study on stigma associated with child mental health conditions identified substantial stigma concerns among participating adults from a nationally representative sample (Pescosolido, 2007). Moreover, when responding to vignettes depicting several stigmatizing conditions including attention deficit hyperactivity disorder (ADHD), depression, “normal troubles” and physical illness, a gradient of rejection of these groups was reported such that individuals with ADHD and depression were rejected the most and those with “normal troubles” and physical illness were rejected the least (Martin et al., 2007). These stigmatizing reactions were higher toward adolescents than children. When presented with similar vignettes, children and adolescents (ages 8–18) participating in a national survey were more likely to make negative attributions about peers with ADHD and depression than peers with asthma, particularly with respect to the likelihood of antisocial behavior and violence (Walker et al., 2008). In addition, participants reported a desire to maintain social distance from peers with ADHD or depression. Social aversion towards people with ADHD was also endorsed by an older sample (i.e., college undergraduates) asked to rate the social desirability of targets with ADHD, minor medical problems, and “no appreciable weakness” (Canu et al, 2008). Because concerns about stigma may be particularly pertinent for adolescents who are developmentally sensitive about others’ opinions and seek peer approval, their stigma perceptions may prevent help-seeking or prompt treatment discontinuation.
In light of these reports, it is surprising that there are currently no specific assessment instruments available to evaluate stigma associated with ADHD. For this study, we hypothesized that assessment tools originally developed to assess relevant stigma constructs in other health conditions might lend themselves to adaptation. In particular, the utility and validity of an instrument designed to assess stigma associated with Human Immunodeficiency Virus (HIV) has been established (Berger et al., 2001), and three of its four subscales address domains potentially relevant to ADHD, namely disclosure concerns, negative self image and negative public perceptions towards affected persons. The HIV Stigma Scale is designed for completion by persons with HIV who are willing to acknowledge their membership in a stigmatized group; thus it inquires about personal experiences, yielding a fourth factor, personalized stigma. This first-person approach precludes the assessment of stigma perceptions with respondents who do not have or do not wish to acknowledge personal experience of the stigmatized condition. In order to broaden the usefulness of an ADHD stigma assessment tool, we deemed it desirable to eliminate the need to admit personal ADHD experience and instead focus on the assessment of public stigma perceptions. The aim of this study is to describe the design of an ADHD Stigma Questionnaire (ASQ) through adaptation of the HIV Stigma Scale, and to examine its psychometric properties. We addressed the following questions: (1) Does confirmatory factor analysis of the ASQ corroborate the hypothesized three-factor structure adapted from the HIV Stigma Scale, omitting the personalized stigma factor? (2) Are the three factors sufficiently represented by an overall stigma factor? (3) Does the ASQ demonstrate acceptable internal consistency? (4) What is the re-test stability of the ASQ? (5) Does the ASQ demonstrate adequate construct validity, as assessed by relationships with related constructs, including clinical maladjustment, depression, self-esteem and emotional symptoms?
2. Methods
2.1. Participants and procedures
Participants were drawn from a longitudinal study designed to produce a representative community sample of students at high and low risk for ADHD and followed over four study waves between 1998 and 2008. Details of the study design are described elsewhere (Bussing et al., 2003); this paper uses data from the initial assessment (i.e., baseline, ADHD risk status determined) and wave 4 (i.e., follow-up, ADHD stigma perceptions assessed).
Baseline parent telephone interviews included inquiries into the child’s health status, parental knowledge and attitudes about ADHD, a structured ADHD detection and service use assessment, and Swanson, Nolan and Pelham Parent Rating Scale, Version IV (SNAP-IV) behavior ratings (Swanson, 1992; Bussing et al, 2008). Based on baseline interview results, children were classified as at “high risk” for ADHD if any of the following applied: (a) current or past ADHD diagnosis or treatment; (b) parents or teachers had expressed concern about a possible ADHD diagnosis; or (c) parents or teachers had expressed other behavioral concerns (not specifically ADHD), and the child was rated in the elevated range (>1.5 SD) on the SNAP-IV parent rating scale. Children without previous ADHD diagnosis, treatment or concern and with normative SNAP-IV scores were classified as “low risk.”
Follow-up parent and child interviews with 192 of the high risk and 109 of the low risk participants were conducted on average 7.8 years later. In-person interviews were conducted simultaneously with parents and adolescents. Parents were interviewed by graduate student research assistants, and adolescents were interviewed by undergraduate research assistants. Interviewers were trained by the study coordinator and were videotaped while conducting practice interviews until acceptable inter-rater reliability was established. Interviewers also completed human subjects training prior to conducting interviews. The study was approved by the University Institutional Review Board and the school district research office. Informed consent and/or assent was obtained from all participants.
The sample for the current study consisted of 301 children and adolescents (171 females and 130 males). Of these, 192 had been classified as high risk for ADHD and 109 as low risk based on findings of the baseline screening interviews. High-risk children ranged in age from 11 to 18 years of age with a mean of 15.0 years (SD = 1.7), and children in the low risk group were between 14 to 19 years of age, with a mean of 16.7 years (SD = 1.3). Among the high risk cohort 53.1% met DSM-IV criteria for ADHD at interviews conducted either at wave 2, using the Diagnostic Interview Schedule for Children, Version 4.0 (Shaffer, 2000), or at wave 4, using the Kiddie-SADS-PL (Present and Lifetime Version) (Kaufman et al., 2003); none of the low risk cohort met ADHD criteria on the Kiddie-SADS-PL at wave 4. Also at wave 4, we determined whether a child was considered to have a history of ADHD problems from the family’s perspective, by the parent’s answer to the question, “Has your child ever had a problem with attention, impulsivity, hyperactivity or behavior in the past?” which was elicited as part of the in-person interview. See Table 1 for further description of study participants.
Table 1.
Participant characteristics
| Overall Sample (n = 301) | High risk at baseline (n = 192) | Low risk at baseline (n = 109) | |
|---|---|---|---|
| Age: | |||
| Baseline: Mean (SD) | 7.8 (1.7) | 7.8 (1.7) | 7.9 (1.8) |
| Range in years | 5–11 | 5–11 | 5–11 |
| Follow-up: Mean (SD) | 15.6 (1.8) | 15.0 (1.7) | 16.7 (1.3) |
| Range in years | 11.6–19.4 | 11.6 – 18.3 | 14–19.4 |
| Disclosed History of ADHD | |||
| Problems (at follow-up) | |||
| Parent - Yes | 176 (58%) | 158 (82%) | 18 (16.5%) |
| Child – Yes | 112 (37%) | 93 (48%) | 19 (17%) |
| Met DSM-IV Criteria for ADHD1 | 102 (34%) | 102 (53%) | 0 |
| SNAP-IV ARI2 (Baseline) | |||
| Inatten: Mean (SD; range) | 1.0 (0.9; 0–3) | 1.4 (0.8; 0–3) | 0.3 (0.3; 0–1.2) |
| Hyp/Imp: Mean (SD; range) | 0.9 (0.8; 0–3) | 1.3 (0.8; 0–3) | 0.3 (0.3; 0–1.7) |
| Vanderbilt ARI (Follow-up)3 | |||
| Inattention: Mean (SD; range) | 0.7 (0.7; 0–3) | 1.4 (0.8; 0–3) | 0.5 (0.5; 0–2.9) |
| Hyp/Imp: Mean (SD; range) | 1.1 (0.8; 0–3) | 0.9 (0.8; 0–3) | 0.2 (0.4; 0–2.4) |
| Gender - Male | 130 (43%) | 88 (46%) | 42 (38%) |
| Race | |||
| Black | 97 (32%) | 70 (36%) | 27 (25%) |
| White | 204 (68%) | 122 (64%) | 82 (75%) |
| Lunch | |||
| Free/subsidized | 156 (52%) | 110 (57%) | 46 (42%) |
| Full pay | 145 (48%) | 82 (43%) | 63 (58%) |
These data are missing for four participants.
ARI = Average Rating Per Item. These data are missing for three participants.
2.2. Adaptation of the ASQ
Adolescents completed the ADHD Stigma Questionnaire (ASQ), a 26-item adaptation of the 40-item HIV Stigma Scale. The HIV Stigma Scale was developed by Berger and associates (2001) in order to measure stigma perceptions of individuals with HIV. Items were based on the literature on stigma and the psychosocial aspects of having HIV. Two rounds of content review were performed and the surviving items were distributed through HIV-related organizations throughout the United States. Of 318 adults who responded, 19% were women, 21% African American, and 8% Hispanic. The results of exploratory factor analysis indicated four factors: personalized stigma, disclosure concerns, negative self-image, and concern with public attitudes. This four-factor structure explained 46% of variance. Extraction of a single higher-order factor provided evidence of an overall stigma factor. Relationships with the related constructs self-esteem, depression, social support, and social conflict provided support for construct validity. Internal consistency reliability was excellent, as coefficient alphas were between .90 and .93 for the subscales and .96 for the overall stigma factor. Test-retest correlations between the original questionnaire and a follow-up questionnaire sent 2–3 weeks later supported the temporal stability of the subscales and the overall instrument.
The adaption process to develop the ASQ consisted of the following steps: First items from the HIV Stigma Scale were re-worded for use in an ADHD population, and these items were subjected to review by eight clinicians and educators in the fields of psychiatry, clinical psychology, social work, education, school psychology, counseling and statistics. Reviewers were asked to determine item relevance for assessing perceived stigma associated with a diagnosis of ADHD. Based on this review process items with poor conceptual fit (i.e., two questions referring to infectious etiology) were eliminated. Furthermore, because the ASQ was intended for use with teachers and non-clinical populations (in addition to individuals diagnosed with ADHD), the language was transformed from the first person to the third person (e.g., “I work hard to keep my ADHD a secret” was changed to “People with ADHD work hard to keep it a secret”). In other words, the focus was shifted to perceptions of public stigma, so participants would not be required to have personal ADHD experiences or reveal their personal ADHD histories. As a result of this transformation, four items were removed from the original scale because the wording in third person became too convoluted (e.g., “Some people close to a person with ADHD are afraid others will reject them if it becomes known that person has ADHD”). Lastly, eight items with low item-total correlations in total and subscale analyses were also eliminated, resulting in a 26-item instrument. As in the original scale, each stigma item was rated on a 4-point Likert scale (1 = strongly disagree, 2 = disagree, 3 = agree, and 4 = strongly agree) with higher scores indicating higher stigma perceptions. A copy of the ASQ is shown in the Appendix.
2.3. Additional Measures
2.3.1. Swanson Nolan and Pelham, Version IV (SNAP-IV)
At wave 1 severity of ADHD problems was assessed using the parent report form of a standardized screening measure, the Swanson-Nolan-and-Pelham-IV (SNAP-IV) checklist. The SNAP-IV is a rating scale consisting of operationalized DSM-IV criteria for ADHD. Internal consistency of the original SNAP-IV was reportedly high (> 0.9 for all symptom clusters), and 2-week test-retest reliability was 0.7 for inattention items, 0.8 for impulsivity items, and 0.9 for hyperactivity items. Norms have been established for the SNAP-IV for elementary-aged children for average ratings per item (ARI) (Swanson, 1992). Scores falling 2-standard deviations above the norm indicate severe symptom levels. Screening and diagnostic utility have also been established (Bussing et al., 2008).
2.3.2 Vanderbilt Assessment Scale – Parent Report
At wave 4, clinical severity of behavior problems was assessed using the parent report form of the Vanderbilt Assessment Scale (Vanderbilt). The Vanderbilt is a scale of child behavior that corresponds to DSM-IV criteria for ADHD, and also acts as a screener for mood and anxiety symptoms, performance in school and relationships at home, in school and in the community. The Vanderbilt Assessment Scales are scored from 0 (Never) to 3 (Very Often) for five dimensions: Inattention; Hyperactivity/Impulsivity; Combined (Inattention and Hyperactivity/Impulsivity); Oppositional Defiant or Conduct Disorder symptoms; and Anxiety or Depression symptoms. Internal consistency for the scale is reportedly high (Cronbach’s alpha was 0.90 or greater; Wolraich et al., 2003). Concurrent validity was calculated based on a comparison with the Computerized Diagnostic Interview Schedule for Children (C-DISC-IV) and found to be relatively high (0.79).
2.3.3 Behavior Assessment System for Children, Self Report of Personality
At wave 4 adolescents completed a norm-referenced adolescent self report measure, the Behavior Assessment System for Children Self Report of Personality (BASC-SRP). The SRP yields 14 scales, grouped into 3 composites (School Maladjustment, Clinical Maladjustment, Personal Adjustment) and an overall summary score, the Emotional Symptom Index (ESI) (Reynolds and Kamphaus, 2002). The School Maladjustment composite is composed of three clinical scales that reflect externalizing problems: Attitude to School, Attitude to Teachers, and Sensation Seeking. The Clinical Maladjustment composite was designed as a global measure of internalizing problems and is composed of five clinical scales: Anxiety, Locus of Control, Social Stress, Somatization, and Atypicality. The Personal Adjustment composite was designed as an overall measure of adaptive functioning and is composed of four clinical scales: Relations with Parents, Interpersonal Relations, Self-Esteem, and Self-Reliance. The Emotional Symptoms Index is composed of Anxiety, Atypicality, Social Stress, Depression, Sense of Inadequacy, Interpersonal Adjustment and Self-Esteem. The BASC has been used in diverse populations and found to have adequate reliability and validity (Reynolds and Kamphaus, 2002). Data from a community sample indicate that average internal consistency (α) for the composites and scales are 0.91 and 0.78, respectively. One-month test-retest reliability has been reported at 0.84 and 0.76 for the composites and scales, respectively. The SRP also demonstrates acceptable construct validity (e.g., Weis and Smenner, 2007).
2.4. Data analysis
2.4.1. Factor structure
Confirmatory factor analysis (CFA) was performed using random parceling, a method that reduces a large number of indicators to yield a better model fit (Little et al., 2002). We elected to create random parcels in consideration of the psychometric characteristics of items compared to parcels (e.g., item-level data tend to violate distributional assumptions) and due to factor-solution and model-fit advantages. Items were randomly selected from the same domain with equal probability for each item, and the average of the items represented a parcel to be loaded onto the latent variable. Because we transformed the instrument from a self stigma to a public stigma perspective, we eliminated the Personalized Stigma subscale, which contained items representing personal experiences an affected person may have had. Instead we assigned these items onto the remaining three factors (Disclosure Concerns, Negative Self-image and Concern with Public Attitudes) according to the type of experience they represented. We examined the three factor model through the following fit statistics: The root mean squared error of approximation (RMSEA) is the discrepancy per degree of freedom of the model and data covariance matrices (Steiger, 1990). Values between 0.080 and 0.051 are thought to represent “a reasonable error of approximation” and values equal to or less than 0.050 represent a “close fit” (Browne and Cudeck, 1993). The goodness-of-fit index (GFI; Jöreskog and Sörbom, 1996) represents the improvement in fit of the model when compared to no model. The comparative index (CFI; Bentler, 1990) demonstrates how much better the model fits compared to the null model. GFI and CFI values greater than or equal to 0.95 indicate good fit (Hu and Bentler, 1999). We also expected a χ2/df ratio smaller than 3. To investigate whether an overall stigma measure would adequately represent the three subscales, we conducted an analysis known as the Schmid-Leiman solution (SLS; see Wolff and Preising (2005) for an excellent discussion of SLS). The SLS calculates the direct relationships between items and first order (“subscale”) and higher order (“general”) factors. In scale development research there is a tradeoff between generality (reflecting an overall measure) and accuracy (reflecting subscales that are more specific measures). SLS yields the relative and independent contributions of first and higher order factors to items, thus facilitating factor analysis interpretation and scale development.
2.4.2. Internal consistency and test-retest reliability
Item-total correlation reliability (Kendall’s tau) was conducted to identify poor performers. To assess internal consistency reliability, coefficient alphas were calculated for the combined 26 items and for the three ASQ subdomains. By convention, a lenient cut-off of 0.60 is common in exploratory research; alpha should be at least 0.70 or higher to retain an item in an “adequate” scale; and a cut-off of 0.80 is required for a “good scale” (Litwin, 2002) Two week test-retest stability was examined using Intraclass Correlations (ICCs) in a subsample of 45 adolescents. According to Chinn (1991), any measure should have an ICC of at least 0.6 to be useful.
2.4.3. Construct validity: Convergent and divergent
Convergent construct validity was assessed by examining relationships between stigma and emotional constructs (i.e., BASC-SRP scores of Clinical Maladjustment, Depression, Self-esteem and Emotional Symptoms) that have been shown to be related (Berger et al., 2001; Link et al., 2001; Quinn & Wigal, 2004; King et al., 2007). In the psychometric evaluation of the HIV Stigma Scale (HSS), the HSS was compared to measures of self-esteem, depression and aspects of social support and social conflict. Based on their approach, we hypothesized that the ASQ and its subscales would share some overlap with scores on the BASC, specifically with the ESI, the Clinical Maladjustment composite (reflecting global internalizing problems), Depression and Self-Esteem. As mentioned above, the original HIV Stigma Scale was evaluated only on patients diagnosed with HIV, whereas in our study, respondents included individuals who had experienced previous ADHD problems and those who did not. Importantly, based on work by Ruesch et al., (2005) we hypothesized that a subjective identification with ADHD problems must be present in order for a relationship between emotional status and ADHD stigma perceptions to emerge, and in the absence of such identification the person would be emotionally indifferent to the degree of ADHD stigma they perceived. In other words, relationships between stigma and emotional constructs were expected to be moderated by a history of ADHD problems. Thus, using a multiple regression approach, construct validity was examined by comparing the relationships between constructs for adolescents who reported a history of ADHD problems (hereafter “ADHD Problem” group) and those who did not (hereafter “No Problem” group). In our analysis, we modeled emotional status as the dependent variable and ADHD stigma perception as the independent variable. In each model we included ADHD problem status and the interaction of problem status and stigma perception. We then tested whether the strength of relationship between emotional status and stigma perception (i.e., the unstandardized regression coefficient estimate of model slope) differed according to ADHD problem status. In other words, we investigated moderating effect by testing for a difference in slopes according to ADHD problem status. We hypothesized that emotional status and stigma perception would be related in the “ADHD problem” group (yielding a positive slope) but would not be related in the “ADHD no problem” group (yielding a zero slope).
With respect to divergent validity, we hypothesized that the ASQ would not correlate with the School Maladjustment composite. Divergent validity is represented by examining the relationship between the instrument of interest (in this case the ASQ) and an instrument measuring a different construct (in this case the BASC-SRP School Maladjustment score). Evidence for divergent validity is shown by the lack of a significant correlation between the two measures (Kazdin, 1998). We chose the School Maladjustment score because, despite the claim that the composite reflects resentment toward teachers, low academic achievement, and disruptive and impulse-control problems at school, fully 14 of 33 items come from the subscale “Sensation Seeking,” which describes behaviors that are not clearly school-related (e.g., “Stealing something from a store is exciting,” and “I like to be scared”). Agreement with these items might be more relevant to a child with Conduct Disorder rather than ADHD.
3. Results
3.1. Description of the study cohort
Age, gender distribution, and symptom severity scores at wave 1 baseline and wave 4 follow-up are presented in Table 1.
3.2. Factor structure
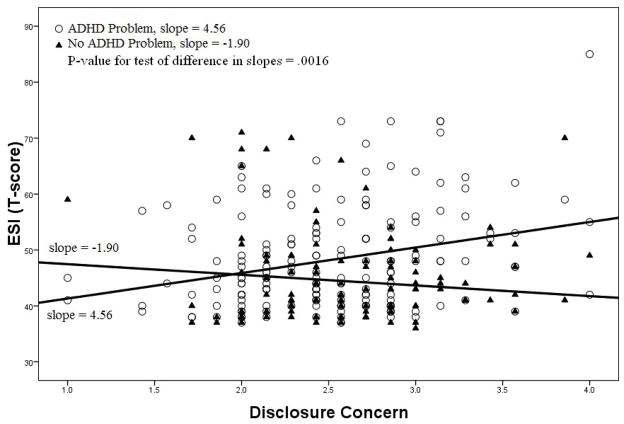
A CFA conducted on the 26-item ASQ supported the parceled 3-factor structure with subscales of Disclosure Concerns, Negative Self-Image, and Concern with Public Attitudes. In contrast to the HIV Stigma Scale, we did not allow items to load on more than one factor. Table 2 demonstrates the frequency with which stigma items were endorsed and identifies on which subscale items were loaded. No individual item loadings are available because of the parceling. CFA results, including parcel loadings, for the 3-factor model are depicted in Figure 1. The CFA resulted in satisfactory fit indices, with [χ2(24) = 47.74, p = 0.003], Goodness of Fit Index = 0.96, Comparative Fit Index = 0.98, Non-normed Index = 0.98 and RMSEA = 0.06.
Table 2.
Endorsement of ASQ items by the entire sample
| Subscale | Item | % Endorsed SA or A1 | |
|---|---|---|---|
| Disclosure Concerns | 17 | Worry that others may judge them | 66.8 |
| 13 | Careful about who they tell | 63.5 | |
| 23 | Told others to keep it a secret | 60.8 | |
| 18 | Regret telling people | 53.9 | |
| 3 | Risky to tell others | 49.5 | |
| 5 | Work hard to keep it a secret | 43.5 | |
| 19 | Feel it was a mistake to tell others | 32.8 | |
| Negative Self Image | 2 | Attitudes make people with ADHD feel worse about themselves | 58.3 |
| 6 | Feel they aren’t as good as others | 44.9 | |
| 8 | Feel damaged | 37.6 | |
| 9 | Feel set apart and isolated | 33.3 | |
| 1 | Feel guilty about having ADHD | 28.1 | |
| 11 | Feel that they are bad | 19.0 | |
| Concern with Public Attitudes | 15 | Worry about others discriminating | 55.8 |
| 24 | Good points tend to be ignored | 52.8 | |
| 21 | Others act like it’s their fault | 49.8 | |
| 26 | Others look for character flaws | 46.3 | |
| 22 | Lose friends when they tell others | 33.6 | |
| 10 | Most people think those w/ADHD are damaged | 31.9 | |
| 16 | Most people are uncomfortable around someone w/ADHD | 26.3 | |
| 25 | People are afraid of someone w/ADHD | 25.6 | |
| 7 | Treated like outcasts | 23.3 | |
| 14 | Others grow distant | 23.3 | |
| 12 | Rejected when others find out | 22.9 | |
| 20 | People don’t want someone w/ADHD around their children | 19.9 | |
| 4 | Lose their jobs because of ADHD | 11.7 |
A = Agree; SA = Strongly Agree.
Fig. 1.
The SLS percentage of extracted variance explained by a general (“overall stigma”) factor was 48.1%, providing ample evidence for an overall stigma factor (Gorsuch, 1983). The high correlations among the three factors (Figure 1) also support the overall stigma score which was constructed as an average of 26 items in the ASQ.
3.3. Internal consistency reliability
Coefficient alphas for the combined 26 items and the three ASQ subdomains suggested good internal consistency reliability, and internal consistency estimates did not increase with removal of any item (see Table 3).
Table 3.
Internal consistency and test-retest reliability
| Factor Name | Number of items | Coefficient Alpha (range of alpha if items deleted) | Two week test-retest ICC (n = 45) |
|---|---|---|---|
| Disclosure Concern | 7 | 0.83 (0.80–0.82) | 0.73 |
| Negative Self Image | 6 | 0.81 (0.75–0.80) | 0.55 |
| Concern with Public Attitudes | 13 | 0.87 (0.86–0.87) | 0.68 |
| All items | 26 | 0.93 (0.92–0.93) | 0.71 |
3.4. Test–retest stability
Test-retest correlations generally supported the temporal stability for all three subscales and for the overall measure. The time interval between the two week test sessions ranged from 9 to 32 days, with a median of 15 days and a mean of 17.7 days. The two-week test-retest ICC for the overall measure was 0.71. ICCs for the subscale scores ranged from 0.55 to 0.73 for two-week test-retest stability (see Table 3).
3.5. Construct validity: Convergent and divergent
Table 4 reports the moderating effect of reported ADHD problem status on the relationships between perceptions of ADHD-related stigma (predictor) and adolescent BASC-SRP scores (outcome).
Table 4.
Validity assessment – moderating effect of ADHD diagnosis on relationship between stigma perception (predictor) and emotional status (outcome)
| Overall ASQ | Disclosure Concern | Negative Self Image | Concern with Public Attitudes | |||||
|---|---|---|---|---|---|---|---|---|
|
|
||||||||
| Disclosed History of ADHD Problems at Follow-up | ADHD | ADHD | ADHD | ADHD | ADHD | ADHD | ADHD | ADHD |
| No | Yes | No | Yes | No | Yes | No | Yes | |
| ESI1 | ||||||||
| slope | −0.27 | 6.32 | −1.90 | 4.56 | 1.13 | 4.87 | 0.12 | 5.21 |
| p-value | 0.005 | 0.002 | 0.06 | 0.02 | ||||
| Clin Maladjustment2 | ||||||||
| slope | 1.04 | 7.55 | −1.52 | 5.19 | 2.17 | 5.56 | 1.63 | 6.58 |
| p-value | 0.007 | 0.002 | 0.10 | 0.03 | ||||
| Depression | ||||||||
| slope | −1.97 | 5.59 | −2.34 | 3.45 | −1.11 | 4.30 | −1.39 | 5.03 |
| p-value | < 0.001 | 0.002 | 0.003 | 0.001 | ||||
| Self Esteem | ||||||||
| slope | 0.80 | −4.02 | 2.18 | −3.17 | −0.09 | −3.93 | 0.06 | −2.57 |
| p-value | 0.04 | 0.009 | 0.05 | 0.24 | ||||
| School Maladjustment3 | ||||||||
| slope | −0.91 | 1.43 | −1.44 | −0.27 | −0.57 | 1.57 | −0.37 | 1.81 |
| p-value | 0.30 | 0.55 | 0.26 | 0.30 | ||||
ESI = Emotional Symptoms Index; this encompasses Anxiety, Atypicality, Social Stress, Depression, Sense of Inadequacy, Interpersonal Adjustment and Self-Esteem.
The Clinical Maladjustment composite encompasses Atypicality, Locus of Control, Somatization, Social Stress and Anxiety.
The School Maladjustment composite encompasses Attitude to School, Attitude to Teachers and Sensation Seeking.
3.5.1. Convergent Validity
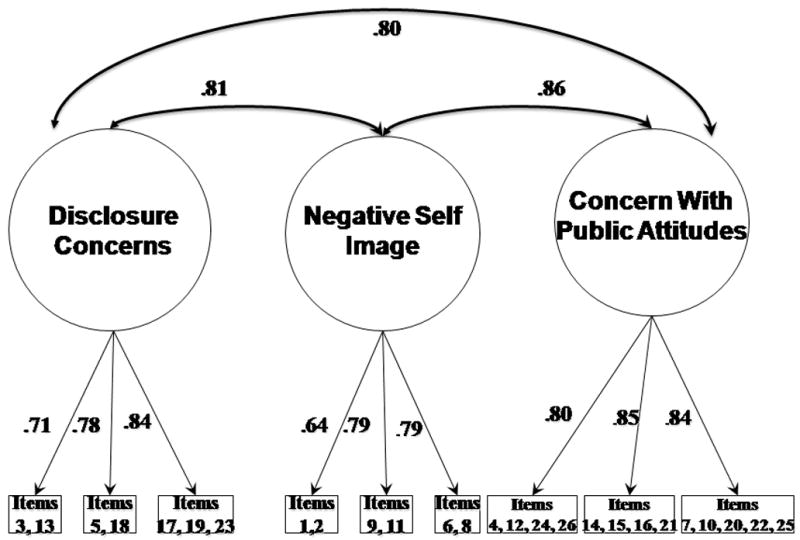
Comparison of the slopes of the relationship between BASC-SRP ESI and ASQ Disclosure Concerns for the ADHD Problem group (n = 176) versus the No Problem group (n = 125) revealed a significant moderating effect such that rising Disclosure Concerns were related to increasing ESI scores for the ADHD Problem group only (p = 0.002). Figure 2 illustrates this relationship. Similar results were found when comparing the ESI and the Concern with Public Attitudes subscale as well as the full ASQ. Comparison of the slopes for the relationship between ESI and ASQ Negative Self-Image reached trend level (p = 0.06). Evidence for a significant moderating effect of a history of ADHD problems on relationships between stigma perceptions and Clinical Maladjustment, Depression and Self-Esteem was also found. A trend level effect was found for the relationship between Clinical Maladjustment and Negative Self-Image (p = 0.10). We did not find evidence for a moderating effect on the relationship between Self-Esteem and Concern with Public Attitudes (p = 0.24). (Due to space limitations, all figures are not reproduced in this paper, but see Table 4 for slopes and p-values.)
Fig. 2.
Comparison of the slope of the relationship between ASQ Disclosure Concerns (predictor) and BASC-SRP Emotional Symptoms Index (outcome) for the ADHD Problem group versus the No Problem group.
3.5.2. Divergent Validity
As hypothesized, we found no significant relationship between adolescent reports of School Maladjustment and the ASQ or any of its subscales for either the ADHD Problem group or the No Problem group (see Table 4; all p’s > 0.05).
4. Discussion
This study investigated the psychometric properties of a measure assessing perceived stigma associated with ADHD. Results of the present study provide support for the use of the ASQ in community samples of adolescents both with and without a history of ADHD-related problems. Factor structure, internal consistency, item selection, test-retest reliability, and construct validity (i.e., convergent and divergent validity) of the ASQ were found acceptable, and results also supported the use of a general stigma factor. Study findings also demonstrated satisfactory reliability of the ASQ. An important strength of the study is that findings are derived from representative sampling of a North Florida school district rather than from a convenience sample. Moreover, our study over-sampled girls and contained a significant number of African American adolescents, resulting in a more inclusive sample than reported in clinical ADHD studies where girls and adolescents from minority backgrounds are thought to be under-represented (Quinn and Wigal, 2004; Hervey-Jumper et al., 2006).
Our findings support the construction of an overall stigma factor, which can efficiently capture potential impacts of general ADHD stigma perceptions, for example when examining predictors of access to treatment for adolescent ADHD such as predisposing, enabling, and barrier factors (Bussing et al., 2003). Yet, the three stigma subscales originally put forth in the HIV Stigma Scale, namely Disclosure Concerns, Negative Self Image, and Concern with Public Attitudes, were also confirmed as pertinent constructs for the stigma surrounding ADHD, a mental disorder whose etiology, treatment implications and prognosis differ substantially from HIV disease. Thus, for research questions that require a more refined modeling of the components of stigma, the ASQ subscales can be utilized accordingly. Further support for the condition-independent relevance of these three stigma subscales is provided by a recently developed tool measuring stigma associated with mental illness in general (King et al., 2007). Using exploratory factor analysis, the authors identified subscales related to disclosure concerns and public stigma (or discrimination). Interestingly, their third subscale represented possible positive aspects of having a mental illness, rather than signifying negative self-image. This discovery is not surprising in light of the recognition that an individual diagnosed with mental illness has the choice of agreement or disagreement with public stigma about their illness (Ruesch et al., 2005). If the individual sees the negative public beliefs as legitimate, he or she may experience negative emotional reactions (e.g., negative self-image) or exhibit maladaptive behavioral responses (e.g., fail to seek help); however, if the individual disagrees with public beliefs, he or she may find positive aspects to mental illness. As a final argument for the relevance of the stigma subscales, we draw attention to our finding that Negative Self-Image subscale scores were correlated with Concerns about Public Attitudes and Disclosure Concern scores, suggesting that as public stigma perceptions and disclosure concerns increase, self-stigma experiences also rise. These relationships are consistent with the model of public and private responses to mental illness proposed by Ruesch and colleagues (2005), who suggests that individuals diagnosed with a mental disorder may begin to share in the negative stereotyping that accompanies the disorder, leading to increased emotional impairment and negative self-image (i.e., self-stigma).
Convergent validity of the ASQ and its subscales was demonstrated by significant relationships with scores measuring clinical maladjustment (including anxiety and social stress), depression, self-esteem and emotional symptoms. These relationships highlight the importance of evaluating ADHD-related stigma in adolescents with ADHD problems since they suggest that greater stigma perception may contribute to increased symptoms of internalizing disorders and poor adjustment. Identification and prevention of contributors to internalizing disorders in children with ADHD is critical since those with comorbid ADHD and depression display greater social impairment than children with ADHD alone (Blackman et al., 2005). The high prevalence of poor adjustment in adolescents diagnosed with ADHD as children has also been demonstrated by a recent study reporting that only a minority of these adolescents was well-adjusted as defined by simultaneous consideration of emotional, behavioral, and social domains. Notably, in this sample poor adjustment persisted even if improvements in ADHD symptoms were reported (Lee et al., 2008). ADHD stigma reduction intervention may be particularly important in adolescence, when the developmental task of identity consolidation sensitizes teenagers to negative public perceptions. Thus, the ASQ could be a useful measure for both researchers and clinicians for assessing stigma perceptions surrounding ADHD in both affected and unaffected persons.
4.1. Limitations and future directions
As with any adaptation of a disease-specific measure for use with a different condition, questions arise about the integrity of the adaptation. In this case, we adapted an HIV stigma assessment tool for use in a population of adolescents with and without ADHD. One limitation of our adaptation is that we did not augment the measure with additional questions that may be important in an ADHD population. For example, we did not inquire about stigma associated with medication. Questions about stigma associated with medication may be particularly important in this population, and could include beliefs that physicians overmedicate children for behavioral problems, fears about stigma stemming from receiving treatment for mental health issues during childhood, and concerns about physical effects of medication on children (Pescosolido et al., 2007). Stigma related to treatment of mental illness might also vary based on cultural background, with reports suggesting that African-Americans and Latinos prefer counseling for depression over medication (Dwight-Johnson and Lagomasino, 2007).
Future studies should examine the impact of gender and cultural background on the perception of stigma surrounding ADHD. There is evidence that girls report a more negative effect of ADHD on their self-esteem than boys do (Quinn and Wigal, 2004); perceived stigma might be an important mediator of this relationship. Cultural differences might also contribute to perceptions of stigma surrounding ADHD since it has been suggested, for example, that African American parents tend to express a socially constructed view of ADHD, resulting in perceived social stigma, and are subsequently less amenable to the diagnosis than are Caucasian parents (Davison and Ford, 2001). Similarly, results of a recent survey assessing parents’ experiences, attitudes and knowledge about ADHD suggested that parental fear of social stigma (i.e., “being labeled”), fear of over-diagnosis of the disorder and a general lack of knowledge likely inhibit African American and Hispanic parents to seek diagnosis and treatment (Taylor and Leitman, 2003). Additional studies should address parental reports of stigma related to ADHD since children and adolescents are dependent on their parents for treatment seeking. These results may provide insight into the barriers they face when seeking treatment for their children.
Furthermore, beliefs about psychosocial versus biological or genetic explanations of the etiology of ADHD and how these beliefs might differentially affect public stigma about ADHD might be important to assess. This distinction was relevant in an examination of stigma related to anorexia nervosa (Crisafulli et al., 2008). Recently there has been greater emphasis on biological contributions to ADHD; however, this knowledge is not necessarily universally accepted. Differences in the understanding of the etiology of the disorder may be important since it has been reported that, in general, disorders thought to be within an individual’s control (i.e., those with psychosocial causes) may elicit more negative reactions (Weiner, 1993), whereas those thought to be outside an individual’s control (i.e., those with genetic causes) may elicit fewer negative reactions.
4.2. Clinical implications
Although our findings should be interpreted with these limitations in mind, this study demonstrates that higher stigma perceptions are associated with greater disclosure concerns, more negative self-image, and increased concern with public attitudes. Higher stigma perceptions may signal the need for further assessment of emotional symptoms, including depression and self-esteem. If depression and low self-esteem are rooted in a perceived legitimacy of public attitudes, this might signal the need for different treatment strategies for the mood symptoms. For example, rather than prescribing medication (which may carry its own stigma), bibliotherapy, psychoeducation and a referral to a support group for people with ADHD might be more appropriate.
Adolescents represent a unique and understudied population in which to examine stigma perceptions due to the particular importance placed upon the opinions of others at this developmental level. Because stigmatizing reactions to ADHD have been shown to be highest toward adolescents (Martin et al., 2007), and because stigma surrounding mental illness may prevent help-seeking (U.S. Department of Health and Human Services, 1999) or cause premature discontinuation of treatment (Ruesch et al., 2005), the evaluation of the stigma perceptions of children and adolescents may be a critical aspect of provision of care. More research is needed to understand the stigma experiences of children and adolescents. Efforts should focus on appropriate methods of assessing stigma, based on comprehensive conceptual models (e.g., the Etiology and Effects of Stigma model; Martin, 2007).
Acknowledgments
This research was funded by grants from the NIMH to Dr. Bussing (RO1 MH57399). The authors thank Wei Hou and Phillip Smith for their statistical consultation, and Dana Mason, Daliana Ferrero, and Sherine Presley for their contributions to the data collection for this study.
Appendix
Attention Deficit Hyperactivity Disorder (ADHD) STIGMA Questionnaire
This study asks about some of the social and emotional aspects of having ADHD. For most of the questions, just circle the letters that go with your answer. There are no right or wrong answers, we would just like your opinions. Feel free to write in comments as you go through the questions.
This set of questions asks about some of the experiences, feelings, and opinions people with ADHD might have and how they are treated. Please do your best to answer each question.
For each item, circle your answer: Strongly disagree (SD), disagree (D), agree (A), or strongly agree (SA).
| Strongly Disagree (SD) | Disagree (D) | Agree (A) | Strongly Agree (SA) | |
|---|---|---|---|---|
| 1. People who have ADHD feel guilty about it. | SD | D | A | SA |
| 2. People’s attitudes about ADHD may make persons with ADHD feel worse about themselves. | SD | D | A | SA |
| 3. Someone who has ADHD would think it’s risky to tell others about it. | SD | D | A | SA |
| 4. People with ADHD lose their jobs when their employers find out. | SD | D | A | SA |
| 5. People with ADHD work hard to keep it a secret. | SD | D | A | SA |
| 6. Someone with ADHD feel they aren’t as good a person as others because they have ADHD. | SD | D | A | SA |
| 7. People with ADHD are treated like outcasts. | SD | D | A | SA |
| 8. People with ADHD feel damaged because of it. | SD | D | A | SA |
| 9. After learning they have ADHD, a person may feel set apart and isolated from the rest of the world. | SD | D | A | SA |
| 10. Most people think that a person with ADHD is damaged. | SD | D | A | SA |
| 11. A person with ADHD feels that they are bad because of it. | SD | D | A | SA |
| 12. Most people with ADHD are rejected when others find out. | SD | D | A | SA |
| 13. People who have ADHD are very careful about who they tell. | SD | D | A | SA |
| 14. Some people who learn of another person having ADHD grow distant. | SD | D | A | SA |
| 15. After learning they have ADHD, people worry about others discriminating against them. | SD | D | A | SA |
| 16. Most people are uncomfortable around someone with ADHD. | SD | D | A | SA |
| 17. People with ADHD worry that others may judge them when they learn that they have ADHD | SD | D | A | SA |
| 18. People with ADHD regret having told some people that they have ADHD. | SD | D | A | SA |
| 19. As a rule, People with ADHD feel that telling others that they have ADHD was a mistake. | SD | D | A | SA |
| 20. People don’t want someone with ADHD around their children once they know that person has ADHD. | SD | D | A | SA |
| 21. Some people act as though it’s the person’s fault that they have ADHD. | SD | D | A | SA |
| 22. People with ADHD have lost friends by telling them they have ADHD. | SD | D | A | SA |
| 23. People with ADHD have told others close to them to keep the fact that they have ADHD a secret. | SD | D | A | SA |
| 24. The good points of people with ADHD tend to be ignored. | SD | D | A | SA |
| 25. People seem afraid of a person with ADHD once they learn they have ADHD. | SD | D | A | SA |
| 26. When people learn that someone has ADHD, they look for flaws in their character. | SD | D | A | SA |
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- Angermeyer MC, Dietrich S. Public beliefs about and attitudes towards people with mental illness: A review of population studies. Acta Psychiatrica Scandinavica. 2006;113:163–179. doi: 10.1111/j.1600-0447.2005.00699.x. [DOI] [PubMed] [Google Scholar]
- Bentler PM. Comparative fit indexes in structural models. Psychological Bulletin. 1990;107:238–246. doi: 10.1037/0033-2909.107.2.238. [DOI] [PubMed] [Google Scholar]
- Berger BE, Ferrans CE, Lashley FR. Measuring stigma in people with HIV: Psychometric assessment of the HIV Stigma Scale. Research in Nursing & Health. 2001;24:518–529. doi: 10.1002/nur.10011. [DOI] [PubMed] [Google Scholar]
- Blackman GL, Ostrander R, Herman KC. Children with ADHD and depression: A multisource, multimethod assessment of clinical, social, and academic functioning. Journal of Attention Disorders. 2005;8(4):195–207. doi: 10.1177/1087054705278777. [DOI] [PubMed] [Google Scholar]
- Browne MW, Cudeck R. Alternative ways of assessing model fit. In: Bollen KA, Long JS, editors. Testing structural equation models. Sage Publications; Newbury Park: 1993. [Google Scholar]
- Bussing R, Fernandez M, Harwood M, Hou W, Garvan CW, Eyberg SM, Swanson JM. Parent and teacher SNAP-IV ratings of Attention-Deficit Hyperactivity Disorder. Assessment. 2008 doi: 10.1177/1073191107313888. in press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bussing R, Zima B, Gary F, Garvan C. Barriers to detection, help-seeking, and service use for children with ADHD symptoms. Journal of Behavioral Health Services & Research. 2003;30(2):176–189. doi: 10.1007/BF02289806. [DOI] [PubMed] [Google Scholar]
- Canu WH, Newman ML, Morrow TL, Pope DLW. Social appraisal of adult ADHD: Stigma and influences of the Beholder’s Big Five personality traits. Journal of Attention Disorders. 2008;11(6):700–710. doi: 10.1177/1087054707305090. [DOI] [PubMed] [Google Scholar]
- Chinn S. Repeatability and method comparison. Thorax. 1991;46:454–456. doi: 10.1136/thx.46.6.454. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Crisafulli M, von Holle A, Bulik C. Attitudes towards Anorexia Nervosa: The impact of framing on blame and stigma. International Journal of Eating Disorders. 2008;41:333–339. doi: 10.1002/eat.20507. [DOI] [PubMed] [Google Scholar]
- Davison JC, Ford DY. Perceptions of Attention Deficit Hyperactivity Disorder in one African American community. The Journal of Negro Education. 2001;70(4):264–274. [Google Scholar]
- Dwight-Johnson M, Lagomasino I. Addressing depression treatment preferences of ethnic minority patients. General Hospital Psychiatry. 2007;29:179–181. doi: 10.1016/j.genhosppsych.2007.02.001. [DOI] [PubMed] [Google Scholar]
- Goffman E. Stigma: Notes on the management of spoiled identity. Prentice Hall; Englewood Cliffs, New Jersey: 1963. [Google Scholar]
- Gorsuch RL. Factor analysis. 2. Erlbaum; Hillsdale, New Jersey: 1983. [Google Scholar]
- Hervey-Jumper H, Douyon K, Franco K. Deficits in diagnosis, treatment and continuity of care in African-American children and adolescents with ADHD. Journal of the National Medical Association. 2006;98(2):233–238. [PMC free article] [PubMed] [Google Scholar]
- Hu LT, Bentler PM. Cutoff criteria for fit indexes in covariance structure analysis: Conventional criteria versus new alternatives. Structural Equation Modeling. 1999;6(1):1–55. [Google Scholar]
- Jöreskog K, Sörbom D. LISREL 8: User’s reference guide. 2. Scientific Software International; Chicago, Illinois: 1996. [Google Scholar]
- Kaufman J, Schweder AE. The Schedule for Affective Disorders and Schizophrenia for School Age Children: Present and Lifetime Version (K-SADS-PL) In: Hersen M, Segal DM, Hilsenroth M, editors. The Comprehensive Handbook of Psychological Assessment (CHOPA), Volume 2: Personality Assessment. John Wiley and Sons; New York: 2003. [Google Scholar]
- Kazdin A. Research design in clinical psychology. 3. Allyn & Bacon; Boston, Massachusetts: 1998. [Google Scholar]
- King M, Dinos S, Shaw J, Watson R, Stevens S, Passetti F, Weich S, Serfaty M. The Stigma Scale: Development of a standardised measure of the stigma of mental illness. British Journal of Psychiatry. 2007;190(3):248–254. doi: 10.1192/bjp.bp.106.024638. [DOI] [PubMed] [Google Scholar]
- Landis J, Koch G. The measurement of observer agreement for categorical data. Biometrics. 1977;33(1):159–174. [PubMed] [Google Scholar]
- Lee SS, Lahey BB, Owens EB, Hinshaw SP. Few preschool boys and girls with ADHD are well-adjusted during adolescence. Journal of Abnormal Child Psychology. 2008;36(3):373–383. doi: 10.1007/s10802-007-9184-6. [DOI] [PubMed] [Google Scholar]
- Link BG, Struening EL, Neese-Todd S, Asmussen S, Phelan JC. Stigma as a barrier to recovery: The consequences of stigma for the self-esteem of people with mental illnesses. Psychiatric Services. 2001;52:1621–6. doi: 10.1176/appi.ps.52.12.1621. [DOI] [PubMed] [Google Scholar]
- Little TD, Cunningham WA, Shahar G, Widaman KF. To parcel or not to parcel: Exploring the question, weighing the merits. Structural Equation Modeling. 2002;9:151–173. [Google Scholar]
- Litwin MS. The Survey Kit series. Vol. 8. Sage Publications; Thousand Oaks, California: 2002. How to assess and interpret survey psychometrics. [Google Scholar]
- Martin JK, Pescosolido BA, Olafsdottir S, Mcleod JD. The construction of fear: Americans’ preferences for social distance from children and adolescents with mental health problems. Journal of Health and Social Behavior. 2007;48(1):50–67. doi: 10.1177/002214650704800104. [DOI] [PubMed] [Google Scholar]
- Pescosolido B. Culture, children, and mental health treatment: Special section on the National Stigma Study – Children. Psychiatric Services. 2007;58(5):611–612. doi: 10.1176/ps.2007.58.5.611. [DOI] [PubMed] [Google Scholar]
- Pescosolido B, Perry B, Martin J, McLeod J, Jensen P. Stigmatizing attitudes and beliefs about treatment and psychiatric medications for children with mental illness. Psychiatric Services. 2007;58(5):613–618. doi: 10.1176/ps.2007.58.5.613. [DOI] [PubMed] [Google Scholar]
- Quinn P, Wigal S. Perceptions of girls and ADHD: Results from a national survey. Medscape General Medicine. 2004;6(2):2. Retrieved June 24, 2008 from http://www.pubmedcentral.nih.gov/articlerender.fcgi?artid=1395774. [PMC free article] [PubMed]
- Reynolds C, Kamphaus R. The clinician’s guide to the Behavior Assessment System for Children. The Guilford Press; New York: 2002. [Google Scholar]
- Ruesch N, Angermeyer M, Corrigan P. Mental illness stigma: Concepts, consequences, and initiatives to reduce stigma. European Psychiatry. 2005;20:529–539. doi: 10.1016/j.eurpsy.2005.04.004. [DOI] [PubMed] [Google Scholar]
- Shaffer D, Fisher P, Lucas CP, Dulcan MK, Schwab-Stone ME. NIMH Diagnostic Interview Schedule for Children Version IV (NIMH DISC-IV): Description, differences from previous versions, and reliability of some common diagnoses. Journal of the American Academy of Child & Adolescent Psychiatry. 2000;39(1):28–38. doi: 10.1097/00004583-200001000-00014. [DOI] [PubMed] [Google Scholar]
- Steiger JH. Structural model evaluation and modification: An interval estimation approach. Multivariate Behavioral Research. 1990;25:173–118. doi: 10.1207/s15327906mbr2502_4. [DOI] [PubMed] [Google Scholar]
- Swanson JM. School-based assessments and interventions for ADD students. KC Publishing; Irvine, California: 1992. [Google Scholar]
- Taylor H, Leitman R. Barriers to the diagnosis and treatment of Attention Deficit Hyperactivity Disorder (ADHD) among African American and Hispanic children. Health Care News. 2003;3(7):1–4. Retrieved June 24, 2008, from http://www.harrisinteractive.com/news/newsletters/healthnews/HI_HealthCareNews2003Vol3_Iss07.
- U.S. Department of Health and Human Services. Mental Health: A Report of the Surgeon General—Executive Summary. Rockville, MD: U.S. Department of Health and Human Services, Substance Abuse and Mental Health Services Administration, Center for Mental Health Services, National Institutes of Health, National Institute of Mental Health; 1999. [Google Scholar]
- Walker JS, Coleman D, Lee J, Squire PN, Friesen BJ. Children’s stigmatization of childhood depression and ADHD: Magnitude and demographic variation in a national sample. Journal of the American Academy of Child & Adolescent Psychiatry. 2008;47 (8):912–920. doi: 10.1097/CHI.0b013e318179961a. [DOI] [PubMed] [Google Scholar]
- Weiner B. On sin versus sickness. A theory of perceived responsibility and social motivation. American Psychologist. 1993;48:957–965. doi: 10.1037//0003-066x.48.9.957. [DOI] [PubMed] [Google Scholar]
- Weis R, Smenner L. Construct validity of the Behavior Assessment System for Children (BASC) Self-Report of Personality: Evidence from adolescents referred to residential treatment. Journal of Psychoeducational Assessment. 2007;25 (2):111–126. [Google Scholar]
- Wolff H, Preising K. Exploring item and higher order factor structure with the Schmid–Leiman solution: Syntax codes for SPSS and SAS. Behavior Research Methods. 2005;37(1):48–58. doi: 10.3758/bf03206397. [DOI] [PubMed] [Google Scholar]
- Wolraich ML, Lambert W, Doffing MA, Bickman L, Simmons T, Worley K. Psychometric properties of the Vanderbilt ADHD Diagnostic Parent Rating Scale in a referred population. Journal of Pediatric Psychology. 2003;28(8):559–568. doi: 10.1093/jpepsy/jsg046. [DOI] [PubMed] [Google Scholar]