Case Presentation
A 76-year-old woman with coronary artery disease, left ventricular systolic dysfunction (ejection fraction = 30%), obesity, and a history of deep vein thrombosis presents with dyspnea and hypoxemia. The combination of physical examination findings of an S3, rales in the lower half of both lung fields, and peripheral edema, chest x-ray evidence of cardiomegaly and pulmonary edema, and a pro-brain-type natriuretic peptide level of 2,150 pg/mL (normal <350 pg/mL) confirms the diagnosis of decompensated heart failure. She is admitted to the Cardiology Service for diuretic therapy and optimization of her heart failure regimen. Although she is written for bedrest, her admission orders do not include venous thromboembolism (VTE) prophylaxis. While entering orders, the Medical House Officer caring for the patient receives an electronic alert identifying the patient as high-risk for VTE and recommending that she be prescribed prophylaxis.
Keywords: Anticoagulation, Cardiovascular disease, Computerized decision support, Medical informatics, Venous thromboembolism
OVERVIEW
Computerized decision support systems are finding an increasing number of applications in both the hospital and ambulatory care settings due to continuing advances in medical informatics technology. A strong foundation in evidence-based medicine and well-established clinical guidelines makes the practice of Cardiovascular Medicine ideally suited to capitalize on the benefits of computerized decision support systems. Computerized decision support strategies have already been successfully implemented in several areas of cardiovascular care, including VTE prevention1–3, pulmonary embolism risk stratification4, dyslipidemia screening and treatment5, and anticoagulation management.6
Although most clinicians believe that the use of medical informatics technology, including computerized decision support, should lead to safer, more efficient, and higher quality care, only a small proportion of United States medical centers have adopted such systems.7 Commonly cited barriers to implementation of computerized decision support include the capital investment necessary to purchase medical informatics technology as well as the resources and dedicated staff required to maintain such systems.7, 8 Lack of cultural acceptance of medical informatics technology, limited standardization, and uncertainty of the benefits of computerized decision support represent additional barriers.8, 9
Proven benefits of computerized decision support include improved patient safety, better disease-specific outcomes, and reductions in healthcare costs. Computerized decision support improves patient safety by reducing medical errors, alerting providers to abnormal test results, and suggesting prophylactic interventions such as VTE prophylaxis.9, 10 These systems have also improved outcomes for patients with myocardial infarction, heart failure, and coronary artery disease requiring bypass graft surgery.11 Hospital costs for patients with these disorders are reduced when computerized decision support systems are used.11 Mechanisms for improvement include facilitating communication between providers, increasing access to practice guidelines and reference information, assistance with calculations, performance of real-time safety checks, monitoring adherence to patient care standards, and tracking adverse events.9
ELECTRONIC ALERTS FOR VTE PREVENTION
Patients with cardiovascular disease, especially those with heart failure, are particularly vulnerable to the development of deep vein thrombosis and pulmonary embolism as a result of hospitalization.12, 13 Despite published guidelines for the prevention of VTE,14, 15 under-utilization of prophylaxis in hospitalized medical patients remains problematic in the U.S.,16 Canada,17 and worldwide.18 At Brigham and Women’s Hospital, we undertook a Quality Improvement Initiative to evaluate the effect of an alert-based computerized decision support strategy on prophylaxis utilization and the subsequent 90-day incidence of symptomatic VTE in high-risk hospitalized patients.2
First, we designed a computer program linked to our online medical record and provider order entry program to identify consecutive hospitalized patients who were at high risk for VTE and for whom prophylaxis was not ordered. The computer program used a weighted scoring system of eight common VTE risk factors to identify and enroll 2,506 eligible high-risk patients for whom an order had not been written for prophylactic measures. They were randomized to an intervention group, in which the responsible physician received an electronic alert regarding the risk of VTE and recommendation for prophylaxis, or to a control group, in which no alert was issued. Each physician receiving an electronic alert was required to acknowledge the notification and could then continue withholding prophylaxis or, on the same computer screen, order pharmacological or mechanical prophylaxis. The computer alert screen was also linked to the hospital’s online Venous Thromboembolism Guidebook, which provided prophylactic regimens for various indications according to published guidelines.19 Patients were followed for 90 days to determine the incident rate of symptomatic VTE.
Electronic alerts more than doubled the rate of VTE prophylaxis orders (33.5% versus 14.5%, p<0.0001) compared with the control group. The risk of symptomatic VTE was reduced by 41% (hazard ratio, 0.59; 95% confidence interval 0.43–0.81; p=0.001) among patients for whom an electronic alert was issued. No significant difference in mortality or rates of major or minor bleeding was observed between the two groups.
While this trial demonstrated the potential power of alert-based computerized decision support systems, these strategies have some important limitations. One particular concern is that the alert might lose efficacy over time, a process known as alert fatigue. At the conclusion of the trial, we discontinued randomization and issued alerts for all patients in a cohort that was high-risk for VTE and not ordered for prophylaxis.20 Compared with the previous randomized controlled trial, electronic alerts maintained efficacy over time and resulted in a similar increase in VTE prophylaxis utilization.20 In another trial of electronic alerts for the prevention of VTE in hospitalized patients, the reduction of VTE events was maintained over time.1
Another potential limitation of computerized decision support for disease prevention is that computer algorithms for risk scoring systems may not capture all factors that increase an individual’s risk and therefore may fail to identify at-risk patients. An analysis of a validated VTE risk scoring system suggested that the integration of additional risk factors would improve sensitivity for patients at the lower end of the risk scale.21 Computerized decision support systems may facilitate more complicated risk scoring systems because they are ideally suited to perform complex risk calculations that incorporate and weigh numerous risk factors.
An additional concern is that electronic alerts may be easy to ignore and that a “human” alerting system may be a more effective form of decision support. We recently designed and conducted a randomized controlled trial of 2,493 patients at high risk for VTE but not receiving prophylaxis to evaluate a decision support strategy that employed a “human” rather than electronic alerting system for the prevention of VTE in hospitalized patients.22 The alert consisted of a direct page from a hospital staff member to the Attending Physician. The hospital staff member advised the Attending Physician to prescribe VTE prophylaxis for these high-risk patients. The primary end point was reduction in symptomatic VTE within 90 days of randomization. Although the “human” alert more than doubled the rate of VTE prophylaxis compared with controls (46.0% versus 20.6%, p<0.0001), the 21% reduction in symptomatic VTE (2.7% versus 3.4%; hazard ratio, 0.79; 95% confidence interval, 0.50–1.25) did not achieve statistical significance and was less than that observed in our previous trial of electronic alerts. Although there was no head-to-head comparison between the two alerting modalities, we believe that a computer alerting system is inherently more effective. An electronic alerting system may be more difficult to ignore because the alert occurs at the point of care and forces the clinician to acknowledge the alert before continuing to use the computer.
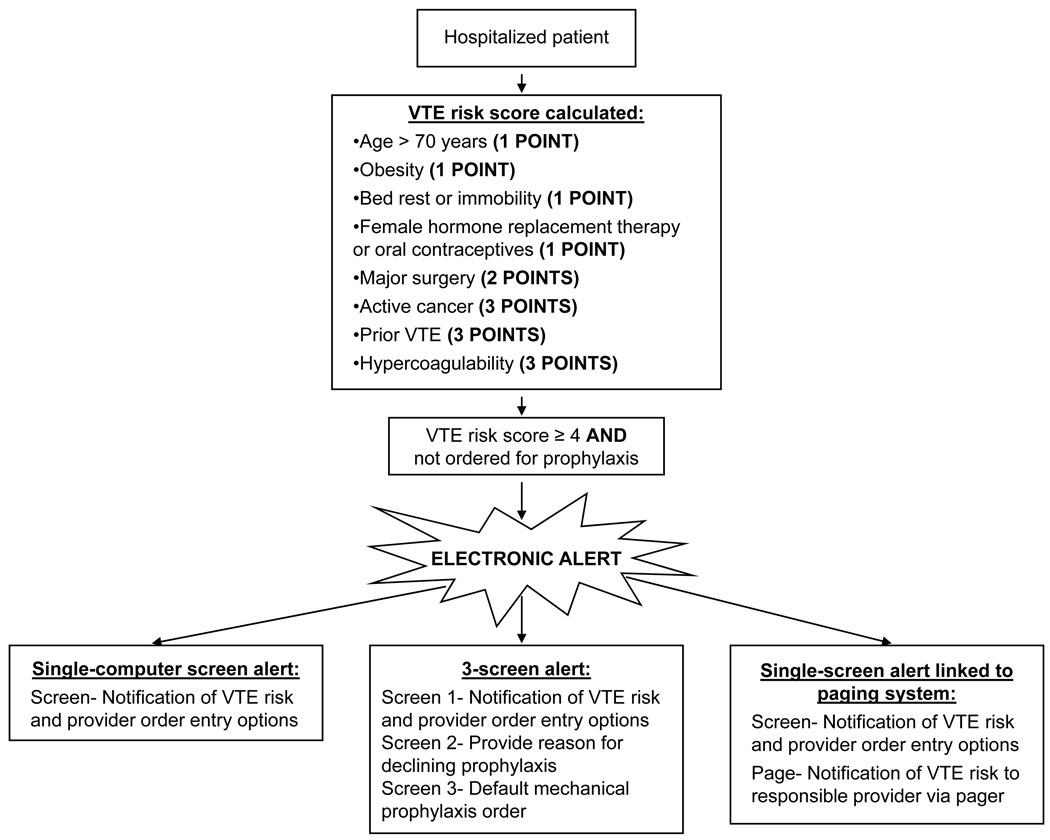
Many of these limitations can be overcome by adapting the computerized decision support strategy to meet the specific clinical need. Various schemas for alert-based decision support for VTE prevention in hospitalized patients can be employed to maximize efficacy (Figure 1). For example, a serial-screen alerting system forcing the provider to explain why prophylactic measures are being omitted and then providing default, or “opt-out,” options for VTE prophylaxis may encourage the clinician to reconsider the patient’s risk or follow links to reference materials, such as the American College of Chest Physicians practice guidelines for VTE prevention.14
Figure 1.
Flow diagram for alert-based computerized decision support strategies for venous thromboembolism prevention in hospitalized patients. VTE, venous thromboembolism.
OTHER APPLICATIONS IN CARDIOVASCULAR MEDICINE
Computerized decision support systems have the potential to complement Quality Improvement Initiatives in Cardiovascular Medicine, such as the American Heart Association’s Get With The Guidelines program, as well as the goals of The Joint Commission. A wide variety of common cardiovascular conditions could benefit from the application of computerized decision support strategies (Table 1). With a growing population requiring anticoagulation and limited resources to meet this demand, outpatient anticoagulant management may be one of the first areas of cardiovascular care in which computerized decision support systems becomes critical.
Table 1.
Potential applications of computerized decision support systems in Cardiovascular Medicine.
|
A recent 5-year multicenter randomized controlled trial compared the use of a commercial computer-assisted oral anticoagulation dosage program with standard medical staff dosing for the management of 2,631 patients across the European Union.6 Primary end points were the relative incidence of clinical bleeding or thrombotic events and time-in-target International Normalized Ratio (INR) range. While the incidence of clinical bleeding or thrombotic events was similar, time-in-target range improved modestly in the group managed by the computer-assisted dosage program compared with standard care (66.8% versus 63.4%). After adjustment for age, gender, and INR, the improvement in time-in-target range was significant (difference of 3.5%; 95% confidence interval, 2.3%–4.9%; p<0.001).
The study also demonstrated an important limitation of computer-assisted anticoagulant dosing. Although the computer program failed to provide a dose in only 5.7% of occasions, medical staff chose to override the suggested dose one-third of the time.6 This observation indicates that current computer-assisted warfarin dosing programs may require the back-up of experienced clinicians.23 Perhaps with refined dosing algorithms that incorporate warfarin pharmacogenomics24, 25, such computer programs may offer more reliable dosing and help improve patient safety.
Current computerized decision support tools for anticoagulant management range from commercial software systems to free internet-based dosing programs, such as WarfarinDosing.org.26 WarfarinDosing.org takes into account clinical factors such as age, gender, ethnicity, target INR and coadministered medications in addition to warfarin pharmacogenomic data, if available, to provide initiation and maintenance doses.26 The website also offers additional decision support tools including reference materials, patient education resources, and a clinical prediction rule for major bleeding.26
IMPLEMENTATION OF COMPUTERIZED DECISION SUPPORT
Clinical trials that focused on the use computerized decision support as part of Quality Improvement Initiatives have demonstrated several critical requirements to successful implementation (Table 2). First, computerized decision support technology must be integrated as part of a larger quality improvement effort and linked to an incentive system.7, 8 Furthermore, a cultural shift toward greater acceptance and incorporation of medical informatics technology is required to encourage consistent use of decision support tools.27 Computerized decision support systems should be integrated into daily workflow and coupled with provider order entry software.28 Computerized decision support strategies should be limited to key decisions and provide simple messages, in order to avoid alert fatigue and should offer recommendations in addition to assessments.28, 29 Alert-based, or automatic, decision support systems are more successful than on-demand, or user-initiated, systems.5, 30 Finally, successful implementation of computerized decision support systems should be measured by clinical outcomes, not simply by provider behavior.29
Table 2.
Keys to successful implementation of computerized decision support in the care of cardiovascular patients.
|
Case Presentation
As a result of the electronic alert, the House Officer reviewed the online educational material regarding options for VTE prophylaxis and ordered enoxaparin 40 mg subcutaneously once daily. The patient was successfully treated for decompensated heart failure and was discharged home after a 4-day hospitalization. During the 90 days of follow-up, she did not suffer deep vein thrombosis or pulmonary embolism.
This case presentation highlights the benefit of computerized decision support in the routine care of the Cardiovascular Medicine patient. Computerized decision support strategies have applications in the prevention, diagnosis, and management of common cardiovascular disorders and offer the promise of improved patient safety, better outcomes, and reduced healthcare costs.
ABBREVIATIONS
- INR
International Normalized Ratio
- VTE
venous thromboembolism
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
DISCLOSURES
None.
REFERENCES
- 1.Lecumberri R, Marques M, Diaz-Navarlaz MT, Panizo E, Toledo J, Garcia-Mouriz A, Paramo JA. Maintained effectiveness of an electronic alert system to prevent venous thromboembolism among hospitalized patients. Thromb Haemost. 2008;100:699–704. doi: 10.1160/th08-05-0337. [DOI] [PubMed] [Google Scholar]
- 2.Kucher N, Koo S, Quiroz R, Cooper JM, Paterno MD, Soukonnikov B, Goldhaber SZ. Electronic alerts to prevent venous thromboembolism among hospitalized patients. N Engl J Med. 2005;352:969–977. doi: 10.1056/NEJMoa041533. [DOI] [PubMed] [Google Scholar]
- 3.Durieux P, Nizard R, Ravaud P, Mounier N, Lepage E. A clinical decision support system for prevention of venous thromboembolism: effect on physician behavior. JAMA. 2000;283:2816–2821. doi: 10.1001/jama.283.21.2816. [DOI] [PubMed] [Google Scholar]
- 4.Donze J, Le Gal G, Fine MJ, Roy PM, Sanchez O, Verschuren F, Cornuz J, Meyer G, Perrier A, Righini M, Aujesky D. Prospective validation of the Pulmonary Embolism Severity Index. A clinical prognostic model for pulmonary embolism. Thromb Haemost. 2008;100:943–948. doi: 10.1160/th08-05-0285. [DOI] [PubMed] [Google Scholar]
- 5.van Wyk JT, van Wijk MA, Sturkenboom MC, Mosseveld M, Moorman PW, van der Lei J. Electronic alerts versus on-demand decision support to improve dyslipidemia treatment: a cluster randomized controlled trial. Circulation. 2008;117:371–378. doi: 10.1161/CIRCULATIONAHA.107.697201. [DOI] [PubMed] [Google Scholar]
- 6.Poller L, Keown M, Ibrahim S, Lowe G, Moia M, Turpie AG, Roberts C, van den Besselaar AM, van der Meer FJ, Tripodi A, Palareti G, Shiach C, Bryan S, Samama M, Burgess-Wilson M, Heagerty A, Maccallum P, Wright D, Jespersen J. A multicentre randomised assessment of the DAWN AC computer-assisted oral anticoagulant dosage program. Thromb Haemost. 2009;101:487–494. [PubMed] [Google Scholar]
- 7.Jha AK, DesRoches CM, Campbell EG, Donelan K, Rao SR, Ferris TG, Shields A, Rosenbaum S, Blumenthal D. Use of electronic health records in U.S. hospitals. N Engl J Med. 2009;360:1628–1638. doi: 10.1056/NEJMsa0900592. [DOI] [PubMed] [Google Scholar]
- 8.Bates DW. The effects of health information technology on inpatient care. Arch Intern Med. 2009;169:105–107. doi: 10.1001/archinternmed.2008.542. [DOI] [PubMed] [Google Scholar]
- 9.Bates DW, Gawande AA. Improving safety with information technology. N Engl J Med. 2003;348:2526–2534. doi: 10.1056/NEJMsa020847. [DOI] [PubMed] [Google Scholar]
- 10.Halpern SD, Ubel PA, Asch DA. Harnessing the power of default options to improve health care. N Engl J Med. 2007;357:1340–1344. doi: 10.1056/NEJMsb071595. [DOI] [PubMed] [Google Scholar]
- 11.Amarasingham R, Plantinga L, Diener-West M, Gaskin DJ, Powe NR. Clinical information technologies and inpatient outcomes: a multiple hospital study. Arch Intern Med. 2009;169:108–114. doi: 10.1001/archinternmed.2008.520. [DOI] [PubMed] [Google Scholar]
- 12.Piazza G, Goldhaber SZ. Pulmonary embolism in heart failure. Circulation. 2008;118:1598–1601. doi: 10.1161/CIRCULATIONAHA.108.803965. [DOI] [PubMed] [Google Scholar]
- 13.Piazza G, Goldhaber SZ. Acute Pulmonary Embolism, Part I: Epidemiology and Diagnosis. Circulation. 2006;114:e28–e32. doi: 10.1161/CIRCULATIONAHA.106.620872. [DOI] [PubMed] [Google Scholar]
- 14.Geerts WH, Bergqvist D, Pineo GF, Heit JA, Samama CM, Lassen MR, Colwell CW. Prevention of venous thromboembolism: American College of Chest Physicians evidence-based clinical practice guidelines (8th edition) Chest. 2008;133:381S–453S. doi: 10.1378/chest.08-0656. [DOI] [PubMed] [Google Scholar]
- 15.Prevention and treatment of venous thromboembolism. International Consensus Statement (guidelines according to scientific evidence) Int Angiol. 2006;25:101–161. [PubMed] [Google Scholar]
- 16.Amin A, Stemkowski S, Lin J, Yang G. Thromboprophylaxis rates in US medical centers: success or failure? J Thromb Haemost. 2007;5:1610–1616. doi: 10.1111/j.1538-7836.2007.02650.x. [DOI] [PubMed] [Google Scholar]
- 17.Kahn SR, Panju A, Geerts W, Pineo GF, Desjardins L, Turpie AG, Glezer S, Thabane L, Sebaldt RJ. Multicenter evaluation of the use of venous thromboembolism prophylaxis in acutely ill medical patients in Canada. Thromb Res. 2007;119:145–155. doi: 10.1016/j.thromres.2006.01.011. [DOI] [PubMed] [Google Scholar]
- 18.Cohen AT, Tapson VF, Bergmann JF, Goldhaber SZ, Kakkar AK, Deslandes B, Huang W, Zayaruzny M, Emery L, Anderson FA., Jr Venous thromboembolism risk and prophylaxis in the acute hospital care setting (ENDORSE study): a multinational cross-sectional study. Lancet. 2008;371:387–394. doi: 10.1016/S0140-6736(08)60202-0. [DOI] [PubMed] [Google Scholar]
- 19.Piazza G, Goldhaber SZ. Venous Thromboembolism Guidebook, Fifth Edition. Crit Pathways in Cardiol. 2006;5:211–227. doi: 10.1097/01.hpc.0000243629.32681.b6. [DOI] [PubMed] [Google Scholar]
- 20.Baroletti S, Munz K, Sonis J, Fanikos J, Fiumara K, Paterno M, Goldhaber SZ. Electronic alerts for hospitalized high-VTE risk patients not receiving prophylaxis: a cohort study. J Thromb Thrombolysis. 2008;25:146–150. doi: 10.1007/s11239-007-0081-1. [DOI] [PubMed] [Google Scholar]
- 21.Arya R, Paneesha S, McManus A, Parsons N, Scriven N, Farren T, Nokes T, Smith H, O'Shaughnessy D, Rose P. More on thromboprophylaxis: Quantifying risk for venous thromboembolism. Thromb Haemost. 2009;101:791–794. [PubMed] [Google Scholar]
- 22.Piazza G, Rosenbaum EJ, Pendergast W, Jacobson JO, Pendleton RC, McLaren GD, Elliott CG, Stevens SM, Patton WF, Dabbagh O, Paterno MD, Catapane E, Li Z, Goldhaber SZ. Physician alerts to prevent symptomatic venous thromboembolism in hospitalized patients. Circulation. 2009;119:2196–2201. doi: 10.1161/CIRCULATIONAHA.108.841197. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Dorsey JL. Software support for 'doing the right thing right'. Thromb Haemost. 2009;101:413–414. [PubMed] [Google Scholar]
- 24.Klein TE, Altman RB, Eriksson N, Gage BF, Kimmel SE, Lee MT, Limdi NA, Page D, Roden DM, Wagner MJ, Caldwell MD, Johnson JA. Estimation of the warfarin dose with clinical and pharmacogenetic data. N Engl J Med. 2009;360:753–764. doi: 10.1056/NEJMoa0809329. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Anderson JL, Horne BD, Stevens SM, Grove AS, Barton S, Nicholas ZP, Kahn SF, May HT, Samuelson KM, Muhlestein JB, Carlquist JF. Randomized trial of genotype-guided versus standard warfarin dosing in patients initiating oral anticoagulation. Circulation. 2007;116:2563–2570. doi: 10.1161/CIRCULATIONAHA.107.737312. [DOI] [PubMed] [Google Scholar]
- 26.Warfarin Dosing. [Accessed June 2, 2009];WarfarinDosing.org. 2009 Available at: http://www.warfarindosing.org/Source/Home.aspx.
- 27.Marco P, Lopez-Abadia E, Lucas J. More on thromboprophylaxis: electronic alerts in hospitalized patients at risk of venous thromboembolism. Thromb Haemost. 2008;100:525–526. [PubMed] [Google Scholar]
- 28.Kawamoto K, Houlihan CA, Balas EA, Lobach DF. Improving clinical practice using clinical decision support systems: a systematic review of trials to identify features critical to success. BMJ. 2005;330:765. doi: 10.1136/bmj.38398.500764.8F. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Durieux P. Electronic medical alerts--so simple, so complex. N Engl J Med. 2005;352:1034–1036. doi: 10.1056/NEJMe058016. [DOI] [PubMed] [Google Scholar]
- 30.Garg AX, Adhikari NK, McDonald H, Rosas-Arellano MP, Devereaux PJ, Beyene J, Sam J, Haynes RB. Effects of computerized clinical decision support systems on practitioner performance and patient outcomes: a systematic review. JAMA. 2005;293:1223–1238. doi: 10.1001/jama.293.10.1223. [DOI] [PubMed] [Google Scholar]