Abstract
Background
Elementary schools represent both a source of childhood sun exposure and a setting for educational interventions.
Methods
Sun Protection of Florida's Children was a cluster randomized trial promoting hat use at (primary outcome) and outside of schools among fourth-grade students during August 8, 2006, through May 22, 2007. Twenty-two schools were randomly assigned to the intervention (1115 students) or control group (1376 students). Intervention schools received classroom sessions targeting sun protection attitudes and social norms. Each student attending an intervention school received two free wide-brimmed hats. Hat use at school was measured by direct observation and hat use outside of school was measured by self-report. A subgroup of 378 students (178 in the intervention group and 200 in the control group) underwent serial measurements of skin pigmentation to explore potential physiological effects of the intervention. Generalized linear mixed models were used to evaluate the intervention effect by accounting for the cluster randomized trial design. All P values were two-sided and were claimed as statistically significant at a level of .05.
Results
The percentage of students observed wearing hats at control schools remained essentially unchanged during the school year (baseline = 2%, fall = 0%, and spring = 1%) but increased statistically significantly at intervention schools (baseline = 2%, fall = 30%, and spring = 41%) (P < .001 for intervention effect comparing the change in rate of hat use over time at intervention vs control schools). Self-reported use of hats outside of school did not change statistically significantly during the study (control: baseline = 14%, fall = 14%, and spring = 11%; intervention: baseline = 24%, fall = 24%, and spring = 23%) nor did measures of skin pigmentation.
Conclusions
The intervention increased use of hats among fourth-grade students at school but had no effect on self-reported wide-brimmed hat use outside of school or on measures of skin pigmentation.
CONTEXT AND CAVEATS
Prior knowledge
As much as 80% of total lifetime sun exposure occurs during childhood, and many skin cancers are associated with childhood sun exposure to a greater extent than lifetime sun exposure.
Study design
A cluster randomized trial of the promotion of hat use at (primary outcome) and outside of schools among fourth-grade students in Florida. Schools were randomly assigned to use wide-brimmed hats at school or not. Hat use at school was measured by direct observation, and hat use at home study was measured by self-report.
Contribution
At control schools, the percentage of students observed wearing hats essentially did not change during the school year. At intervention schools, the percentage of students observed wearing hats increased statistically significantly during the same time. In contrast, self-reported use of hats outside of school did not change during the school year.
Implications
Hat use appears to increase when students are the target of the intervention. Additional studies aimed at increasing hat use might also target entire schools, teachers, and parents.
Limitations
The intervention targeted fourth-grade students in Florida elementary schools and, therefore, might not be successful in other settings. Self-reported hat use outside of school was not independently verified.
From the Editors
Skin cancer is a growing problem nationally with more than 1 million persons diagnosed each year (1). One in three Americans will develop skin cancer during their lifetime (2). Excessive sun exposure has been associated with the development of most types of skin cancers (3,4). Childhood is a critical period for sun protection because as much as 80% of total lifetime sun exposure occurs during childhood (5,6), and many skin cancers are associated with childhood sun exposure to a greater extent than lifetime sun exposure (7–9).
Increasing the proportion of children who follow sun protective measures is a goal of Healthy People 2010 (10). Unfortunately, sun protection methods are infrequently used for children and, when used, consist primarily of applying sunscreen rather than wearing hats or protective clothing (11–15). Although the use of sunscreen may delay sunburn, it may also lead to an increase in overall sun exposure. Most sun protection campaigns to date have emphasized the use of sunscreens as a method of protecting the skin from the sun and have had less impact on other sun protective behaviors (16–18). The US Preventive Services Taskforce concluded that the current evidence is insufficient to recommend routine skin cancer screening or counseling in clinical settings (19,20). However, on the basis of finding sufficient evidence of effectiveness, the Guide to Community Preventive Services recommends interventions in primary schools to improve sun protection behaviors (21–23).
Sun Protection of Florida's Children project was a school-based sun protection intervention that was less focused on the use of sunscreen but, instead, emphasized the use of hats when children were outdoors. The idea of incorporating hat use, specifically wide-brimmed hats, as a component of the intervention was inspired by studies aimed at primary school students in Australia (24–26). Although the sun protection intervention was comprehensive in scope, a focus on hats was justified for several reasons. The head and neck region receives the most extensive sun exposure and is one of the most common areas to develop skin cancer (27–29). Hats are an effective way of reducing sun exposure to these areas and may prevent associated skin cancers (30). Community-based surveys, however, show that children rarely wear hats when outdoors, parents do not consider hat use an important sun protection method, and physicians rarely counsel parents to encourage their children to wear hats in the sun (31–33). We also designed the intervention to be implemented over the entire school year because interventions that are more frequent and of longer duration have been more successful than single-session studies (24,34–37).
In this article, we describe the Sun Protection of Florida's Children project in more detail and report outcomes through the first year of follow-up. We hypothesized that the intervention would increase the use of hats among targeted children at school (primary outcome) and at times other than school (secondary outcome) when compared with children in control schools who did not receive the intervention.
Participants and Methods
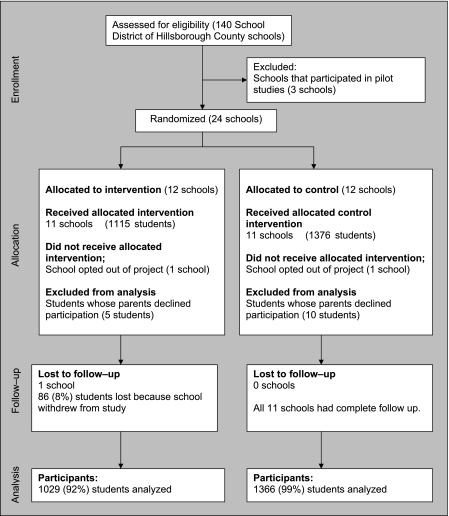
The Sun Protection of Florida's Children project (ClinicalTrials.gov number, NCT 00346021) is a cluster randomized trial, in which participating schools were randomly assigned to either control or intervention status (Figure 1). Block randomization was used by the project's biostatistician to ensure the number of schools assigned to each intervention group was balanced; however, there was no matching or stratification of schools. Participating schools were chosen from Hillsborough County, Florida, which includes Tampa and its surrounding suburbs, as well as largely rural areas in the southern and eastern areas of the county. All 140 kindergartens through grade 5 schools in the School District of Hillsborough County were eligible to participate.
Figure 1.
Comparison of intervention and control schools in the Sun Protection of Florida's Children project.
On the basis of sample size requirements of the study, 20 schools were needed to assess a 10% absolute difference in hat use among intervention and control schools with 80% power. We enrolled 24 schools, however, to allow for possible attrition. We extended an invitation to all 140 schools to participate and closed accrual after 24 schools agreed to participate (all of which met study eligibility criteria). Of the 140 schools invited, 42 schools declined to enroll through fax or phone communication. For each school, we determined the overall enrollment of fourth-grade students and the school uniform policy (required, voluntary, or none) from school officials. We also examined socioeconomic characteristics of the school's surrounding neighborhood by use of census-derived data (urban vs nonurban, median household income, and percentage of population with less than high school education).
Two schools (one in the intervention group and one in the control group) withdrew from the study after consenting but before any data were collected or intervention activities took place. The control school withdrew because of a change in leadership, and the intervention school withdrew because it determined that it could not comply with all study requirements. A third school withdrew from the intervention arm after baseline data were collected but before receiving the intervention. Missing data because of the withdrawal of schools were ignored in the analysis; missing data were not imputed. The number of students who received the allocated assignment was 1115 for the intervention schools and 1376 for the control schools.
This study was approved by the University of South Florida Institutional Review Board. Activity involving human participants did not commence until after approval from the Institutional Review Board. Written informed assent was obtained from each student before the start of the intervention.
Inclusion Criteria
To be eligible for the study, schools were required to meet the following eligibility criteria: 1) the school had at least one fourth-grade class (with a minimum of 20 students per class), 2) the principal and all fourth-grade teachers agreed to participate, 3) the school provided a minimum amount of outdoor student activities defined as at least one outdoor session (physical education, recess, and/or lunch) lasting at least 20 minutes and occurring a minimum of three times per week, 4) outdoor activities occurred in an area that was exposed to sunlight and could be observed by data monitors, 5) schools had the ability to accommodate the major intervention components, 6) school environment was expected to be stable over the intervention time period (ie, no anticipated changes in leadership or student population served), and 7) if randomly assigned to the control group, schools were willing to delay other sun protection initiatives until the project was completed. It is also important to note that all schools allowed children to wear hats while outdoors at school; this behavior was not specifically prohibited or restricted at any school.
The intervention was based on the Theories of “Reasoned Action” (38) and “Planned Behavior” (39). In brief, the Theory of Reasoned Action posits that intentions to engage in healthy behaviors directly predict actual behaviors and are in part influenced by individual attitudes and the attitudes of peers regarding the behavior (subjective norms). The Theory of Planned Behavior extends this theoretical model further by theorizing that perceptions of behavioral control influence behaviors directly, and also indirectly, by affecting intentions (40). Perceived behavioral control is a person's perception of his or her ability to enact a healthy behavior.
The intervention was therefore structured to accomplish several goals. First, the intervention sessions were designed to increase sun protection knowledge of participating children and foster more positive attitudes in regard to wearing hats. In addition, the intervention was designed to change the subjective norm of wearing hats at school by instilling the belief that peers would also have positive attitudes regarding hats and would be wearing hats when outside. The intervention lasted 23 months from August 2006 to June 2008.
To accomplish these goals, the intervention included the following components that occurred over the school year: 1) Introductory meetings with principals, teachers, and physical education instructors were conducted to explain the project and obtain their informed consent. 2) A package of materials was sent to parents at the start of the school year that explained the project and obtained consent to participate. 3) An initial introductory session with students was conducted to explain the project and obtain assent to participate. 4) A 45-minute comprehensive sun protection educational session for fourth-grade students was carried out in classrooms by a community health education organization (MOREHEALTH). 5) Three 60-minute follow-up sessions addressed the benefits of sun protection (with emphasis on hat use), promoted favorable attitudes about sun protection, and made clear that fourth-grade students were both allowed to wear hats at school and should be wearing hats while outside at school. 6) Each participating child was provided two free wide-brimmed hats (one to use at school and one to use at home). 7) Three brief follow-up sessions were scheduled (one that addressed logistic issues, such as where hats would be stored, how they would be identified for each student, and how they would be distributed before outdoor activities; one that addressed any problems that classes were having; and one that was reserved for hat collection at the end of the school year). At the end of the school year, hats were cleaned and stored over the summer and were to be redistributed to the same students at the start of their fifth-grade school year.
At control schools, similar introductory meetings were held with principals, teachers, and students to explain the project and to obtain informed consent of parents and assent of children. Students at control schools received three to five 60-minute educational sessions on topics in science unrelated to sun protection. The topic of the lessons included learning about the sun as a star, the nature of light and heat, and the reflectance and absorbance of heat energy.
Twenty-two schools were enrolled at the start of the 2006–2007 school year. Data were systematically collected from all participants during the following three time periods: baseline (from August 8, 2006, through September 29, 2006) before intervention activities took place at the specific school, after the intervention was implemented at the school (November 30, 2006, through March 15, 2007), and again in the spring (March 27, 2007, through May 22, 2007).
Child's Sun Protection Behavior Survey
The Child's Sun Protection Behavior Survey was a 13-item self-administered instrument designed to assess the frequency with which children used various sun protection methods at school and at home. The questions asked about use of long-sleeve shirts, hats, sunscreen, and sunglasses and clarified the type of hat worn (wide-brimmed vs other types) if hat use was reported. The main outcome assessed with this survey was the child's use of wide-brimmed hats when not at school. This question was worded, “When you were outside playing this weekend or after school, how often did you wear a wide-brimmed hat?” Possible answers were as follows: 1 = “Never”; 2 = “Rarely”; 3 = “Sometimes”; 4 = “Often”; and 5 = “Always.” This question has been previously validated as a measure of children's hat use (21). In addition to the sun protection measure, each student completed a brief demographic survey.
Direct Observation of Hat Use
The primary outcome of the study, hat use at school, was measured by direct observation. Four research assistants underwent standardized training in direct observation of hat use at school. Research assistants first underwent a 60-minute training session in which wide-brimmed hats were defined (ie, a hat with at least a 2-inch brim covering the circumference of the hat) and differentiated from other hats and other forms of head coverings. Each research assistant was then trained in a standardized method of assessing the number of students who were observed in an outdoor school setting and the number observed who were wearing wide-brimmed and other hats. Research assistants used a handheld counter to facilitate measurement. To assess reliability of measurement, all four research assistants conducted measurements simultaneously with the project director. There was perfect agreement between measures taken by the project director and all four research assistants in regard to observed hat use.
Assessment of hat use at schools was based on the principles of valid measurement of sun protection behavior, as described by Milne et al. (41,42). Research assistants used listings of outdoor scheduled activities to schedule their observation sessions to measure hat use among fourth-grade students from each class and school during each of the three data collection periods. For each school, the data collection sessions were at least 8 weeks apart. Research assistants chose inconspicuous vantage points to ensure that student and teacher behaviors were not influenced by the measurement process. Research assistants recorded the following data at each observation session: 1) the total number of students observed, 2) the number of students observed wearing any type of hat, and 3) the number of students wearing wide-brimmed hats. In addition, ambient conditions during the outdoor activity (time of day, temperature, cloud cover, wind speed, and amount of shading) were assessed by each researcher as described previously (21,43).
DermaSpectrometer Measures
We hypothesized that use of hats at school would result in less pronounced sun-induced physiological changes in children's skin. In an exploratory fashion, we conducted an interim analysis of the impact of the intervention on skin pigmentation among a convenience sample of students who agreed to undergo additional measurements (skin pigment assessment and nevi counts) for a 2-year period. We recruited a minimum of 15 students at each school by asking for volunteers (no incentives were used) who were willing to participate in this portion of the study, and a total of 378 students (178 in the intervention group and 200 in the control group) agreed to participate, with 280 (74.1%) completing all three measurements in the first year. For each student, measurements of skin pigmentation were assessed at baseline (August 8, 2006, through September 29, 2006), midyear (November 30, 2006, through March 15, 2007), and again in spring (March 27, 2007, through May 22, 2007). We compared changes in each subject's skin pigmentation over the course of the study, so that each subject served as his or her own control.
We fitted the generalized linear mixed models (to account for clustered data) separately for each intervention group to determine whether or not demographic characteristics differed among students who participated in this part of the study compared with those who did not. Students who volunteered were found to be similar to those who did not volunteer with regard to age (P = .5 for both the intervention and control groups), sex (P = .9 for the intervention group and P = .1 for the control group), and race (P = .6 for the intervention group and P = .98 for the control group).
All measures of skin pigmentation were made with a DermaSpectrometer (Cortex Technology, Hadsund, Denmark). The DermaSpectrometer measures light reflectance at two narrow wavelength bands corresponding to skin erythema (568 nm) and melanin content (655 nm). The DermaSpectrometer then calculates an erythema and melanin index, each ranging from 0% to 100%. DermaSpectrometers have been compared with colorimeters and both provide similar estimates of skin melanin pigmentation (44,45).
We assessed skin pigmentation at a child's forehead as a representative anatomical site that would be protected by hat use. We initially used a pilot test to measure skin pigmentation on 49 fourth-grade students. In the pilot study, we first assessed skin pigmentation at the center of the forehead (just above the glabella) and to the right and left of center. Measures at these three sites were highly correlated (correlation coefficients center-right = .96, center-left = .97, and left-right = .95). Consequently, we selected the center forehead reading as the single standard measurement site. We next confirmed the test–retest reliability of skin pigment measurement by repeating measurements 1 week apart and calculating the interreliability coefficient (correlation coefficient = .86), as described previously by Shrout and Fleiss (46). We also confirmed the interrater reliability of our methods by comparing measurements taken simultaneously by the project director and research assistants (correlation coefficient = .98).
Statistical Analysis
To determine if participating schools were representative of all Hillsborough County schools, we compared characteristics of schools that participated in the study with schools that did not participate in the study. To ensure comparability of intervention and control arms, we compared baseline characteristics between the intervention schools and control schools. Comparisons were made by use of the Fisher exact test for categorical data, the Wilcoxon rank sum test for continuous data at the school level, and the general or generalized linear mixed model for comparisons at the student level by taking into account the cluster randomized trial design. The rate of hat use and its 95% confidence interval were estimated for each intervention and assessment period by use of the exact binomial distribution.
We examined two endpoints regarding hat use: directly observed hat use at schools and self-reported hat use outside of schools. Both outcomes were measured in each of the following three periods: baseline (late August to early September), late fall to early winter, and early spring. The clustered design in which schools rather than students were randomly assigned to an intervention was accounted for in the generalized linear mixed model. Allocation arm (intervention vs control), date of data collection (represented by a linear or quadratic term), and their interaction were included as fixed effects in the generalized linear mixed model. Multiple random effects were also included in the model: the school-specific mean intercepts and slopes (schools were nested within the intervention arm) with random variation among the students.
The random effects were assumed to be independent and distributed as normal distributions. For self-reported hat use, an additional random effect was included to allow for correlation among repeated observations taken on the same student over data collection rounds, with compound symmetry structure. Several fixed covariates were tested in multivariable models as confounding factors (eg, age, sex, race, and school uniform policy). After checking the distribution of the normality assumption, the pigmentation changes were analyzed by use of a generalized linear mixed model for a subset of the students. In addition, pigmentation changes were analyzed by subgroups defined a priori (lighter-skinned vs darker-skinned children).
The intraclass correlation coefficient (ICC) was estimated by use of the covariance parameters that were estimated from the generalized linear mixed models. For binary data, the estimates were unscaled by use of the average value of the response variable because the estimates of variance were in the logit scale. The statistical analysis was conducted with SAS version 9.1 (SAS Inc, Cary, NC). We used the MIXED procedure for normally distributed continuous data and the GLIMMIX procedure with the logit link function for binary data. To adjust the small number of degrees of freedom in mixed models, the method of Kenward and Roger (47) was used. All P values were from two-sided statistical tests and were claimed as being statistically significant at a level of .05.
The required sample size was determined with a method that takes into account the intraclass correlation coefficient, the expected effect size, and the power of the study. We assumed an intraclass correlation coefficient of .02 and a minimum difference of wearing a hat outdoors (self-report) between the two arms of 10% (control arm = 10% and intervention arm = 20%). Under these assumptions, we anticipated a power of 80% to detect the difference of 10% between the two arms at a statistical significance level of .025 with 10 schools (the average number of fourth-grade students per school was assumed to be 50) for each intervention arm, so that the total included 1000 students. Although the sample justification was based on the self-reported hat use outside of school, we expected that the statistical power for the observed hat use would exceed 80% power, given the resultant sample size.
Results
Characteristics of the 22 participating schools are reported in Table 1 by use of information from the 2000 US Census Bureau (48). There were no statistically significant differences in school or student demographic characteristics between intervention and control schools. We also compared the 22 participating schools with nonparticipating schools in the Hillsborough County School System. There were no differences in school uniform policy, metropolitan vs rural location, size of student population, race or ethnicity of the student population, or census-reported median household income of the school's zip code.
Table 1.
Comparison of intervention schools with control schools among the 22 study participant schools
| Characteristic | Control school (n = 11) | Intervention school (n = 11) | P |
| School uniform policy, No. (%) | |||
| Yes | 7 (53.9) | 6 (46.2) | |
| No | 1 (33.3) | 2 (66.7) | |
| Voluntary | 3 (50.0) | 3 (50.0) | 1.0* |
| School location, No. (%) | |||
| Metropolitan | 7 (46.7) | 8 (53.3) | |
| Nonmetropolitan | 4 (57.1) | 3 (42.9) | 1.0* |
| School type, No. (%) | |||
| Public | 10 (52.6) | 9 (47.4) | |
| Magnet or charter | 1 (33.3) | 2 (66.7) | 1.0* |
| Racial composition†, % | |||
| White | 50.1 | 39.1 | .4‡ |
| Nonwhite | 49.9 | 60.4 | .4‡ |
| Household income of school's zip code§, % | |||
| <$10 000–$14 999 | 11.5 | 19.5 | >.05‡ |
| $15 000–$24 999 | 11.7 | 14.7 | .1‡ |
| $25 000–$34 999 | 13.2 | 12.3 | 1.0‡ |
| $35 000–$49 999 | 17.9 | 15.7 | .2‡ |
| $50 000–$74 999 | 22.2 | 17.0 | .03‡ |
| ≥$75 000 | 23.8 | 20.8 | >.05‡ |
| Mean enrollment, No. (SD) | |||
| 712 (194) | 615 (323) | .1‡ | |
Two-sided Fisher exact test.
Racial composition was self-reported by the participating student.
Two-sided Wilcoxon rank sum test.
Information was obtained for each participating school at www.census.gov.
The primary study outcome (ie, directly observed hat use at school) is reported in Table 2. Hat use remained unchanged at control schools but increased statistically significantly at intervention schools (for control schools, baseline = 2%, fall = 0%, and spring = 1%; and for intervention schools, baseline = 2%, fall = 30%, and spring = 41%; P < .001 for intervention effect comparing the change in rate of hat use over time at intervention vs control schools and ICC = .003). Results were similar when wide-brimmed hat use was assessed (for control schools, baseline = 0%, fall = 0%, and spring 0%; and for intervention schools, baseline = 0%, fall = 25%, and spring = 41%; P < .001 for intervention effect comparing the change in rate of hat use over time at intervention vs control schools). Hat use varied considerably among intervention schools; in the spring assessment period, hat use ranged from a low of 19.1% (26 using hats of 136 total students) to a high of 74.6% (53 using hats of 71 total students). Similar results were obtained in multivariable analyses that controlled for potential differences in baseline characteristics of students and schools and that adjusted for differences in ambient conditions during measurement sessions.
Table 2.
Hat use among intervention and control schools*
| Rate of hat use |
||||
| Baseline | Fall | Spring | P† | |
| Observed rate‡, % (95% CI§) | <.001 | |||
| Control school | 1.7 (1.0 to 2.7) | 0.3 (0.1 to 0.8) | 1.1 (0.6 to 1.8) | |
| Intervention school | 2.0 (1.1 to 3.1) | 29.5 (26.3 to 32.8) | 40.5 (37.2 to 43.8) | |
| Self-reported rate║,% (95% CI§) | .47 | |||
| Control school | 13.5 (11.5 to 15.7) | 14.3 (12.1 to 16.7) | 10.5 (8.6 to 12.7) | |
| Intervention school | 24.3 (21.5 to 27.4) | 24.0 (20.1 to 27.6) | 22. 9 (19.5 to 26.5) | |
CI = confidence interval.
The P value for testing the intervention effect across time from GLIMMIX model. The random coefficient from the GLIMMIX model accounted for a nested cross-sectional design from the cluster randomized trial, in which the linear time trend (baseline, fall, and spring) was treated as a continuous covariate.
Any type of hat use observed.
The 95% CIs were calculated by use of the exact binomial distribution.
The self-reported rate was measured for a wide-brimmed hat use outside at school.
The use of wide-brimmed hats that was self-reported by students outside of school is shown in Table 2. In general, the rates of self-reported use of hats outside of school were low for all students (intervention schools range = 9.1%–44.9% and control schools range = 6.9%–34.3%). However, in all three data collection periods, intervention students were more likely to report use of wide-brimmed hats than were control students. Self-reported use of hats outside of school did not change statistically significantly during the study (control: baseline = 14%, fall = 14%, and spring = 11%; intervention: baseline = 24%, fall = 24%, and spring = 23%). Relative to control students, use of wide-brimmed hats outside of school increased slightly, but not statistically significantly, over the course of the study (with adjustments of the cluster randomized trial design, baseline odds ratio [OR] = 2.1, 95% confidence interval [CI] = 1.3 to 3.2; fall OR =2.1, 95% CI = 1.2 to 3.7; spring OR = 2.5, 95% CI = 1.5 to 4.4; P = .47 for the intervention). It is important to note that odds ratios overestimate actual rate ratios when outcomes are frequent.
We found similar results in multivariable analyses that adjusted for potential baseline differences in student and school characteristics (P = .8 for the intervention effect and ICC = .0002). We also considered the potential impact of school withdrawals on our results. In a sensitivity analysis of our primary outcome (directly observed hat use), we assigned missing schools the mean values of the opposite randomization arm (ie, a withdrawn intervention school was assigned the mean value for control schools and vice versa). There was no substantial impact on our findings.
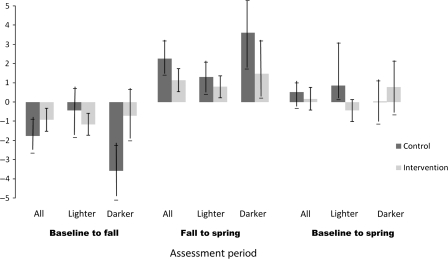
In an exploratory fashion, we assessed changes in skin pigmentation among a subgroup of 378 students (178 in the intervention group and 200 in the control group). For each subject, we recorded the change in skin pigmentation during the following three assessment periods: baseline to fall, fall to spring, and baseline to spring (Figure 2). Among this subgroup, changes in skin pigmentation were similar between control and intervention students. On the basis of the a priori hypothesis, we also stratified our analysis by baseline skin pigmentation. Among children with lighter skin at baseline, no statistically significant differences in skin pigmentation were found between intervention and control students.
Figure 2.
Changes in skin pigmentation among intervention and control students from baseline to fall, fall to spring, and baseline to spring. Pigmentation was assessed by use of a DermaSpectrometer on a subgroup of 378 students (178 in the intervention group and 200 in the control group) during the three assessment periods throughout a school year. We assessed skin pigmentation at a child's forehead as a representative anatomical site that would be protected by hat use. An increase in the DermaSpectrometer readings denotes an increase in melanin, resulting in darkening of the skin. Lighter-skinned students are students with a baseline DermaSpectrometer reading (range = 0–100) that was less than or equal to the median of 20 in the control group and the intervention group. Darker-skinned students were students with a baseline DermaSpectrometer reading (range = 0–100) that is greater than the median of 20 in the control arm and the intervention arm.
Discussion
The Sun Protection of Florida's Children intervention increased use of wide-brimmed hats at school statistically significantly among fourth-grade students at targeted school by the end of the first year, from no hat use at baseline to 42% of students at intervention schools. However, students at intervention schools had no measurable change in skin pigmentation over the course of the study, and the intervention had no apparent effect on use of hats outside of school.
Previous studies have attempted to change sun protection behaviors in school settings. A multicomponent intervention targeting primary schools in Australia, for example, increased the use of wide-brimmed hats (49,24–26). Other school-based interventions have been less successful in changing sun protection behaviors (50–54). A determinant of successful strategies may be both the intensity and duration of the intervention. Interventions relying on single sessions with students have generally not proven successful at modifying sun protection behaviors at school (36,50). Studies (36,49) that were similar to this study and that intervened with students over the course of the school year have proven more successful.
The effects of the Sun Protection of Florida's Children intervention were variable across schools, with some showing little change and others showing 75% adoption of hat use at school. The variation in effect did not appear to be the result of school structure, student demographics, or metropolitan vs nonmetropolitan school setting. Our interactions with schools suggested other possible explanations for the variability in observed hat use at the intervention schools. First, although schools were similar in regard to geographic location and school uniform requirements, they had very different organizational climates. During the first year of our intervention, there were no changes in school leadership; all principals remained and participated for the full first year. Although there were no new principals during the intervention, principals had variable levels of tenure at their schools and variable levels of commitment to the project. We found anecdotally that teachers who did not fully embrace the importance of sun protection during childhood as a means of preventing skin damage were less likely to encourage their students to wear a hat when outside. Differential interest and familiarity with the project may also have accounted for some of the variability in student hat use among intervention schools.
Second, although official policies governing schools are set at the district level, principals and teachers may interpret and implement these policies quite disparately at each school. For example, the School District of Hillsborough County had no official policy that prevented students from wearing a wide-brimmed hat when outside at school. However, some principals and teachers, when asked to describe their individual school policies governing hat use, gave responses that were different from the official district policy. Although our team routinely reminded both principals and teachers of the official school district policy, it is possible that the various rates of hat use resulted in part from differing understanding and interpretation of policy by school officials.
Although the intervention successfully increased use of hats at school, there was no effect on self-reported hat use outside of school. There are several possible explanations for this finding. First, intervention schools had statistically significantly higher self-reported hat use at the start of the study. Although hat use was assessed before formal intervention activities took place at schools, it is possible that teachers (who were aware of the study) influenced students before baseline measurements were conducted. Also, intervention activities were primarily targeted at schools and may not have been sufficiently intense regarding other settings. The theoretical model underpinning the intervention indicates that hat use outside of school would depend on whether students viewed wearing wide-brimmed hats as a normative behavior among family and friends and perceived that they are able to wear hats under many different conditions. Consequently, future interventions may need to more intensely target parents, siblings, and friends to accomplish this goal.
This study has several limitations that should be considered when interpreting its results. First, we used a multicomponent intervention and it was not possible to ascertain the relative importance of each component. Second, we were not able to independently verify students’ reported use of hats outside of school settings. We assessed skin pigmentation changes among a convenience sample of student volunteers, who may not be representative of all participants. Also, our analysis of pigment changes was exploratory and our sample size was not adequately powered to definitively test this outcome. Finally, this intervention targeted fourth-grade students in Florida elementary schools and, therefore, our strategies might not be successful in other grade levels or settings.
This study was successful in encouraging elementary school students to wear a wide-brimmed hat when at school during the first year of follow-up. Results from the second year of follow-up will be reported separately when available and should allow us to determine whether intervention effects can be sustained and whether sun protection altered the development of new nevi.
Future studies should consider the following suggestions. First, we believe principals and, especially, teachers play a critical role in school-based interventions and should be targeted as an integral determinant of success. Convincing principals and teachers to model targeted sun protection behaviors will help persuade students of the importance of sun protection while outdoors. Future studies should incorporate fidelity measures to gauge the extent to which teachers and principals are modeling hat use behaviors by asking teachers and principals to self-report their use of sun protection behaviors. It may also be appropriate to ask students to report on the frequency of teacher and principal hat use at school or to measure such behavior by direct observation. Capturing this information may allow researchers to assess the extent to which the intervention is actually changing school culture.
Second, to improve hat use when students are not at school, intervention strategies must target parents more intensely than did the Sun Protection of Florida's Children project. Strategies to convince parents to model targeted behaviors should be a component of future sun protection projects. Future studies should also consider enlisting the help of parent organizations and organizations that provide services to children (eg, scouts, athletic teams, and after-school programs) as a means of reinforcing these important health behaviors when students are not at school. To capture appropriate role modeling of sun protection behaviors, it may also be helpful to assess parent hat use by self-report or the report of their children.
In addition, future interventions should attempt to assist students in developing higher perceived behavioral control for hat use outside of school under a variety of circumstances (eg, wearing a hat during sporting events, wearing a hat while at the beach, or wearing a hat among peers). Finally, our project strictly targeted fourth-grade students. Future studies should consider implementing a school-wide intervention in which hat use can be embedded into the culture and become an expected behavior of all students.
Funding
National Cancer Institute (RO1 CA103965-01A2).
Footnotes
The authors had full responsibility for the design of the study, the collection of the data, the analysis and interpretation of the data, the decision to submit the manuscript for publication, and the writing of the manuscript.
References
- 1.Jemal A, Siegel R, Ward E, et al. Cancer statistics, 2008. CA Cancer J Clin. 2008;58(2):71–96. doi: 10.3322/CA.2007.0010. [DOI] [PubMed] [Google Scholar]
- 2.Miller D, Weinstock M. Nonmelanoma skin cancer in the United States: incidence. J Am Acad Dermatol. 1994;30(5 Pt 1):774–778. doi: 10.1016/s0190-9622(08)81509-5. [DOI] [PubMed] [Google Scholar]
- 3.Holman C, Armstrong B, Heenan P, et al. The causes of malignant melanoma: results from the West Australian Lions Melanoma Research Project. Recent results. Cancer Res. 1986;102:18–37. doi: 10.1007/978-3-642-82641-2_3. [DOI] [PubMed] [Google Scholar]
- 4.Weinstock M, Colditz G, Willett W, et al. Nonfamilial cutaneous melanoma incidence in women associated with sun exposure before 20 years of age. Pediatrics. 1989;84(2):199–204. [PubMed] [Google Scholar]
- 5.Truhan AP. Sun protection in childhood. Clin Pediatr. 1991;30(12):676–681. doi: 10.1177/000992289103001205. [DOI] [PubMed] [Google Scholar]
- 6.Preston DS, Stern RS. Nonmelanoma cancers of the skin. N Engl J Med. 1992;327(23):1649–1662. doi: 10.1056/NEJM199212033272307. [DOI] [PubMed] [Google Scholar]
- 7.American Academy of Pediatrics Committee on Environmental Health. Ultraviolet light: a hazard to children. Pediatrics. 1999;104(2):328–333. [PubMed] [Google Scholar]
- 8.Gallagher RP, Hill GB, Bajdik CD, et al. Sunlight exposure, pigmentary factors, and risk of nonmelanocytic skin cancer. I. Basal cell carcinoma. Arch Dermatol. 1995;131(2):157–163. [PubMed] [Google Scholar]
- 9.Berneburg M, Surber C. Children and sun protection. Br J Dermatol. 2009;161(suppl 3):33–39. doi: 10.1111/j.1365-2133.2009.09447.x. [DOI] [PubMed] [Google Scholar]
- 10.U.S. Department of Health and Human Services Office of Disease Prevention and Health Promotion. Healthy People 2010 Prevention Agenda Web site. http://www.health.gov/healthypeople/prevagenda/. Accessed December 18, 2009. [PubMed] [Google Scholar]
- 11.Glanz K, Lew RA, Song V, Cook VA. Factors associated with skin cancer prevention practices in a multiethnic population. Health Educ Behav. 1999;26(3):344–359. doi: 10.1177/109019819902600305. [DOI] [PubMed] [Google Scholar]
- 12.Hall HI, May DS, Lew RA, Koh HK, Nadel M. Sun protection behaviors of the U.S. white population. Prev Med. 1997;26(4):401–407. doi: 10.1006/pmed.1997.0168. [DOI] [PubMed] [Google Scholar]
- 13.Olson A, Dietrich A, Sox C, et al. Solar protection of children at the beach. Pediatrics. 1997;99(6):1–5. doi: 10.1542/peds.99.6.e1. [DOI] [PubMed] [Google Scholar]
- 14.Morris J, McGee R, Bandaranayake M. Sun protection behaviours and the predictors of sunburn in young children. J Paediatr Child Health. 1998;34(6):557–562. doi: 10.1046/j.1440-1754.1998.00307.x. [DOI] [PubMed] [Google Scholar]
- 15.Donavan DT, Singh SN. Sun-safety behavior among elementary school children: the role of knowledge, social norms, and parental involvement. Psychol Rep. 1999;84(3 pt 1):831–836. doi: 10.2466/pr0.1999.84.3.831. [DOI] [PubMed] [Google Scholar]
- 16.Dietrich A, Olson A, Sox C, et al. A community-based randomized trial encouraging sun protection for children. Pediatrics. 1998;102(6):1–8. doi: 10.1542/peds.102.6.e64. [DOI] [PubMed] [Google Scholar]
- 17.Milne E, English DR, Johnston R, et al. Improved sun protection behaviour in children after two years of the Kidskin intervention. Aust N Z J Public Health. 2000;24(5):481–487. doi: 10.1111/j.1467-842x.2000.tb00497.x. [DOI] [PubMed] [Google Scholar]
- 18.Hughes BR, Altman DG, Newton JA. Melanoma and skin cancer: evaluation of a health education programme for secondary schools. Br J Dermatol. 1993;128(4):412–417. doi: 10.1111/j.1365-2133.1993.tb00201.x. [DOI] [PubMed] [Google Scholar]
- 19.Screening for skin cancer: an update of the evidence for the U.S. Preventive Services Task Force. Ann Intern Med. 2009;150(3):194–198. doi: 10.7326/0003-4819-150-3-200902030-00009. [DOI] [PubMed] [Google Scholar]
- 20.2009. U.S. Preventive Services Task Force, Agency for Healthcare Research and Quality Web site. About USPSTF. http://www.ahrq.gov/clinic/uspstfab.htm. Accessed October 10, 2009. [Google Scholar]
- 21.Hunter SG, Wells KJ, Jacobsen JB, et al. Assessment of elementary school students’ sun protection behaviors. Pediatr Dermatol. 2009 doi: 10.1111/j.1525-1470.2009.00940.x. http://www2.interscience.wiley.com/journal/121481321/issue. Accessed October 9, 2009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Task Force on Community Preventive Services. Recommendations to prevent skin cancer by reducing exposure to ultraviolet radiation. Am J Prev Med. 2004;27(5):467–470. doi: 10.1016/j.amepre.2004.08.003. [DOI] [PubMed] [Google Scholar]
- 23.Centers for Disease Control and Prevention. Preventing skin cancer. Findings of the Task Force on Community Preventive Services on reducing exposure to ultraviolet light. MMWR Recomm Rep. 2003;52(RR-15):1–12. [PubMed] [Google Scholar]
- 24.Milne E, English DR, Johnston R, et al. Reduced sun exposure and tanning in children after 2 years of a school-based intervention (Australia) Cancer Causes Control. 2001;12(5):387–393. doi: 10.1023/a:1011294023498. [DOI] [PubMed] [Google Scholar]
- 25.Milne E, Johnston R, Cross D, Giles-Corti B, English DR. Effect of a school-based sun-protection intervention on the development of melanocytic nevi in children. Am J Epidemiol. 2002;155(8):739–745. doi: 10.1093/aje/155.8.739. [DOI] [PubMed] [Google Scholar]
- 26.English DR, Milne E, Jacoby P, Giles-Corti B, Cross D, Johnston R. The effect of a school-based sun protection intervention on the development of melanocytic nevi in children: 6-year follow-up. Cancer Epidemiol Biomarkers Prev. 2005;14(4):977–980. doi: 10.1158/1055-9965.EPI-04-0531. [DOI] [PubMed] [Google Scholar]
- 27.Bastiaens MT, Hoefnagel JJ, Bruijn JA, Westendorp RG, Vermeer BJ, Bouwes Bavinck JN. Differences in age, site distribution, and sex between nodular and superficial basal cell carcinoma indicate different types of tumors. J Invest Dermatol. 1998;110(6):880–884. doi: 10.1046/j.1523-1747.1998.00217.x. [DOI] [PubMed] [Google Scholar]
- 28.Merimsky O, Fishman P, Feldman I, et al. Malignant melanoma of the head and neck. Clinical and immunological considerations. Am J Clin Oncol. 1996;19(4):363–367. doi: 10.1097/00000421-199608000-00008. [DOI] [PubMed] [Google Scholar]
- 29.Lange JR, Palis BE, Chang DC, Soong SJ, Balch CM. Melanoma in children and teenagers: an analysis of patients from the National Cancer Data Base. J Clin Oncol. 2007;25(11):1363–1368. doi: 10.1200/JCO.2006.08.8310. [DOI] [PubMed] [Google Scholar]
- 30.Diffey BL, Cheeseman J. Sun protection with hats. Br J Dermatol. 1992;127(1):10–12. doi: 10.1111/j.1365-2133.1992.tb14816.x. [DOI] [PubMed] [Google Scholar]
- 31.Geller AC, Robinson J, Silverman S, Wyatt SA, Shifrin D, Koh HK. Do pediatricians counsel families about sun protection? A Massachusetts survey. Arch Pediatr Adolesc Med. 1998;152(4):372–376. doi: 10.1001/archpedi.152.4.372. [DOI] [PubMed] [Google Scholar]
- 32.Easton AN, Price JH, Boehm K, Telljohann SK. Sun protection counseling by pediatricians. Arch Pediatr Adolesc Med. 1997;151(11):1133–1138. doi: 10.1001/archpedi.1997.02170480063009. [DOI] [PubMed] [Google Scholar]
- 33.Davy L, Boyett T, Weathers L, Campbell R, Roetzheim R. Sun protection counseling by pediatricians. Ambul Pediatr. 2002;2(3):207–211. doi: 10.1367/1539-4409(2002)002<0207:spcbp>2.0.co;2. [DOI] [PubMed] [Google Scholar]
- 34.Buller DB, Reynolds KD, Yaroch A, et al. Effects of the sunny days, healthy ways curriculum on students in grades 6 to 8. Am J Prev Med. 2006;30(1):13–22. doi: 10.1016/j.amepre.2005.08.046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Escoffery C, Glanz K, Hall D, Elliott T. A multi-method process evaluation for a skin cancer prevention diffusion trial. Eval Health Prof. 2009;32(2):184–203. doi: 10.1177/0163278709333154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Buller DB, Taylor AM, Buller MK, Powers PJ, Maloy JA, Beach BH. Evaluation of the sunny days, healthy ways sun safety curriculum for children in kindergarten through fifth grade. Pediatr Dermatol. 2006;23(4):321–329. doi: 10.1111/j.1525-1470.2006.00270.x. [DOI] [PubMed] [Google Scholar]
- 37.Gritz ER, Tripp MK, James AS, et al. Effects of a preschool staff intervention on children's sun protection: outcomes of sun protection is fun! Health Educ Behav. 2007;34(4):562–577. doi: 10.1177/1090198105277850. [DOI] [PubMed] [Google Scholar]
- 38.Fishbein M. A theory of reasoned action: some application and implications. In: Howe HE, Page MM, editors. Beliefs, Attitudes, and Values: Nebraska Symposium on Motivation 1979. Lincoln, NB: University of Nebraska Press; 1980. pp. 65–116. [PubMed] [Google Scholar]
- 39.Fishbein M, Ajzen I. Belief, Attitude, Intention, and Behavior. Reading, MA: Addison-Wesely; 1975. [Google Scholar]
- 40.Ajzen I. From intentions to actions: a theory of planned behavior. In: Kuhl J, Beckmann J, editors. Action-Control: From Cognition to Behavior. Heidelberg, Germany: Springer; 1985. pp. 11–39. [Google Scholar]
- 41.Milne E, Corti B, English R, Cross D. Costa C, Johnston R. The use of observational methods for monitoring sun-protection activities in schools. Health Educ Res. 1999;14(2):167–175. doi: 10.1093/her/14.2.167. [DOI] [PubMed] [Google Scholar]
- 42.Milne E, English DR, Corti B, et al. Direct measurement of sun protection in primary schools. Prev Med. 1999;29(1):45–52. doi: 10.1006/pmed.1999.0501. [DOI] [PubMed] [Google Scholar]
- 43.National Weather Service Web site. 2006–2007. http://www.nws.noaa.gov/. Accessed April 22, 2007. [Google Scholar]
- 44.Clarys P, Alewaeters K, Lambrecht R, Barel AO. Skin color measurements: comparison between three instruments: the Chromameter, the DermaSpectrometer, and the Mexameter. Skin Res Technol. 2000;6(4):230–238. doi: 10.1034/j.1600-0846.2000.006004230.x. [DOI] [PubMed] [Google Scholar]
- 45.Shriver MD, Parra EJ. Comparison of narrow-band reflectance spectroscopy and tristimulus colorimetry for measurements of skin and hair color in persons of different biological ancestry. Am J Phys Anthropol. 2000;112(1):17–27. doi: 10.1002/(SICI)1096-8644(200005)112:1<17::AID-AJPA3>3.0.CO;2-D. [DOI] [PubMed] [Google Scholar]
- 46.Shrout PE, Fleiss JL. Intraclass correlations: uses in assessing rater reliability. Psychol Bull. 1979;86(2):420–428. doi: 10.1037//0033-2909.86.2.420. [DOI] [PubMed] [Google Scholar]
- 47.Kenward M, Roger JH. Small sample inference for fixed effects from restricted maximum likelihood. Biometrics. 1997;53(3):983–997. [PubMed] [Google Scholar]
- 48.American Fact Finder. US Census Bureau Web site. 2000. http://factfinder.census.gov/. Accessed March 8, 2006. [Google Scholar]
- 49.Giles-Corti B, English DR, Costa C, Milne E, Cross D, Johnston R. Creating SunSmart schools. Health Educ Res. 2004;19(1):98–109. doi: 10.1093/her/cyg003. [DOI] [PubMed] [Google Scholar]
- 50.Gooderham MJ, Guenther L. Sun and the skin: evaluation of a sun awareness program for elementary school students. J Cutan Med Surg. 1999;3(5):230–235. doi: 10.1177/120347549900300502. [DOI] [PubMed] [Google Scholar]
- 51.Barankin B, Liu K, Howard J, Guenther L. Effects of a sun protection program targeting elementary school children and their parents. J Cutan Med Surg. 2001;5(1):2–7. doi: 10.1177/120347540100500102. [DOI] [PubMed] [Google Scholar]
- 52.Buller DB, Buller MK, Beach B, Ertl G. Sunny days, healthy ways: evaluation of a skin cancer prevention curriculum for elementary school-aged children. J Am Acad Dermatol. 1996;35(6):911–922. doi: 10.1016/s0190-9622(96)90115-2. [DOI] [PubMed] [Google Scholar]
- 53.Grant-Petersson J, Dietrich A, Sox C, Winchell C, Stevens M. Promoting sun protection in elementary schools and child care settings: the SunSafe Project. J Sch Health. 1999;69(3):100–106. doi: 10.1111/j.1746-1561.1999.tb07216.x. [DOI] [PubMed] [Google Scholar]
- 54.Naldi L, Chatenoud L, Bertuccio P, et al. Improving sun-protection behavior among children: results of a cluster-randomized trial in Italian elementary schools. The “SoleSi SoleNo-GISED”. Project. J Invest Dermatol. 2007;127(8):1871–1877. doi: 10.1038/sj.jid.5700835. [DOI] [PubMed] [Google Scholar]