Abstract
What is known about radiation exposure to physicians who perform cardiac interventions is reviewed and various factors that affect their exposure are discussed. There are wide variations in the radiation dose (up to 1000-fold) per procedure. Despite extensive improvements in equipment and technology, there has been little or no reduction in dose over time. The wide variation and lack of reduction in operator doses strongly suggests that more attention must be paid to factors influencing the operator dose. Numerous patient, physician and shielding factors influence the operator dose to different degrees. Operators can change some of these factors immediately, at minimal or no cost, with a substantial reduction in dose and potential cancer risk.
INTRODUCTION
Since the introduction of catheter-based interventional procedures, the frequency of these procedures has increased due to their advantages over surgery. These advantages include minimal invasiveness, reduced pain and risk, shorter hospital stay and lower cost(1,2). Cardiac catheterisation procedures are performed for diagnostic, therapeutic or both purposes. During these procedures, catheters, guidewires and other devices are visualised and guided using real-time fluoroscopy. Radiation exposure to the operator is inevitable. Cardiologists and radiologists have become concerned because of reports of brain tumours to cardiologists and other physicians by using fluoroscopy(3,4).
When radiation is used to guide cardiac interventions, the goal is to optimise the radiation dose—to use as much radiation as needed to provide adequate imaging for diagnosis and guidance, but no more radiation than necessary. Since the operator dose is proportional to the patient dose, optimising the patient dose benefits both the patient and the operator. Much has been written about how to properly use the fluoroscopic equipment during cardiac interventions in order to optimise the patient radiation dose(5). However, less attention has been paid to factors that affect the operator radiation dose and how to minimise the operator dose. A recent comprehensive review of operator radiation doses from cardiac interventions highlights the variability of reported operator doses, the importance of controlling the factors that affect the operator dose and the need to incorporate an awareness of the operator dose into daily practice(6).
In this document, what is known about operator radiation doses from various cardiac interventions is reviewed and the various factors, not directly related to the fluoroscopic equipment, that affect the operator dose are discussed.
OPERATOR DOSE
Variability
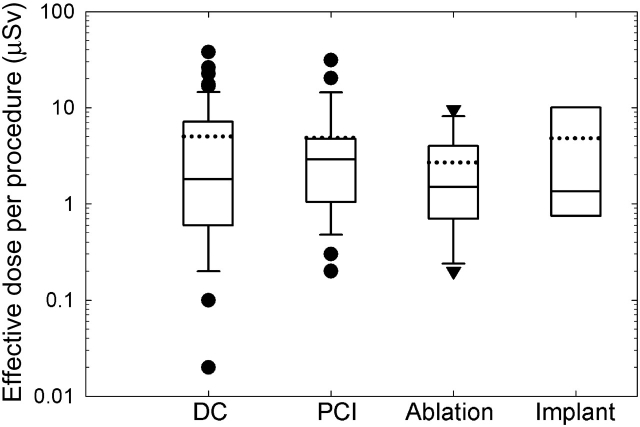
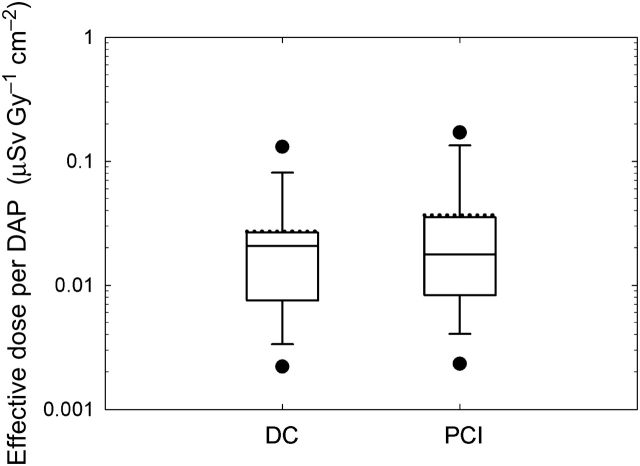
Figure 1 shows a box plot of effective dose estimates to the operator from a single procedure for four types of fluoroscopically guided cardiac procedures. The effective dose estimates were determined from a review of all English language journal articles and other published data reporting radiation exposure to cardiologists from the early 1970s to 2006(6). The average operator dose was quantitatively related to the average patient dose, as would be expected, but there was much greater variation in operator doses than in patient doses. Operator doses varied by two to three orders of magnitude (100–1000 times) for the same type of procedure. For the same patient dose (measured as a dose–area product), occupational doses varied widely (Figure 2). Some of these variations were certainly due to factors related to the fluoroscopic equipment, but some must also be due to operator factors not related to the fluoroscopic equipment. This implies that the radiation dose to the operator during cardiac procedures might be reduced by modifying operator practices.
Figure 1.
Box plot of reported mean effective radiation doses per procedure to an operator performing various fluoroscopically guided cardiac catheterisation procedures: DC, PCI, ablation (ablation of abnormal electrophysiologic pathways) and implant (placement of a permanent transvenous pacemaker or defibrillator). Each reported mean effective dose represents the mean value from one published study under similar exposure conditions. Solid lines in the box plot indicate the first quartile, median and the third quartile. The dotted line indicates the mean value.
Figure 2.
Operator effective dose normalised by patient radiation dose (as dose–area product [DAP]).
Changes observed over time
Improvements in technology have reduced the dose rate from X-ray equipment(5,7,8). With these improvements in dose-reduction technology in fluoroscopic equipment over the past several decades, and the introduction of digital cineradiography and flat panel detectors, it is not unreasonable to expect that the operator dose would also decline. In fact, slow but statistically significant declines in the average operator dose have been observed over time for diagnostic cardiac catheterisation (DC) and for electrophysiological ablation procedures(6). This is not true for percutaneous coronary interventions (PCI). In fact, there is some evidence of an increasing operator dose over time for PCI.
Changes over time in radiation doses to patients and physicians can be attributed to changes in procedure protocols and technology. Improvements in procedure protocols and the technology of X-ray equipment, catheters and other devices generally decrease procedure time, fluoroscopy time, cineradiography time and radiation dose for procedures with similar complexity. On the other hand, improved protocols and technologies make possible more complex procedures. Increasingly, complex procedures demand longer fluoroscopy time, cineradiography time or both. The increase in radiation required to complete these more complex procedures negates the effect of technological improvements that might otherwise result in a reduction of the operator dose. The best example of this phenomenon is PCI.
Operator doses for PCI have not decreased over time. Radiation exposure during PCI is strongly correlated with procedure complexity(9–14). The increasing complexity of PCI procedures over time appears to have offset dose reductions due to technology. As the outcomes of PCI have improved and catheter, guidewire, balloon and stent technologies have evolved, PCI procedures have become more complex(14,15). Procedures are now being performed in vessels and lesions that are more challenging and technically difficult, and that could not have been performed a decade ago. Stents are used far more frequently than in the past(16).
Failure to reduce the operator dose from PCI, despite the introduction of dose-reducing technology in fluoroscopic equipment, underscores the importance of understanding the effects of operator practices on the operator dose and of modifying operator practices whenever practicable.
FACTORS THAT AFFECT OPERATOR RADIATION DOSE
Many factors influence the radiation dose to operators who perform fluoroscopically guided interventions. Principal among these are the fluoroscopic system and its operation. Advances in technology have reduced the radiation dose while preserving the image quality. Digital imaging technology in cardiac catheterisation laboratories has reduced scatter dose rates and patient doses when compared with film-based imaging technology(17). A more sensitive image intensifier can also reduce radiation dose(18). The most modern fluoroscopic systems employ flat-panel detectors instead of image intensifiers. Some studies have suggested the possibility of dose reduction using flat panel systems(19,20). Fluoroscopic equipment and its operation have been described in great detail elsewhere and are not discussed further here(5).
Some of the other factors that affect the operator dose cannot be controlled, but many are under the control of the operator. Table 1 summarises factors not related to the fluoroscopic equipment that influence the operator dose in the cardiac catheterisation laboratory and the degree to which they can be controlled by the operator. These are discussed in detail below.
Table 1.
Factors influencing operator radiation dose during fluoroscopically guided cardiac catheterisation procedures.
| Category | Fixed factors | Degreea | Modifiable factors | Degreea |
|---|---|---|---|---|
| Patient | Clinical problem/complexity | + | ||
| Lesion characteristics | + | |||
| Body size | + | |||
| Physician | Height/gender | + | Procedure technique | + + |
| Experience/skill | + | Catheter choice | + | |
| Workload | + | Catheter insertion site | + | |
| Position with respect to patient | + + | |||
| Awareness of exposure | + | |||
| Shielding | Apron | +++ | ||
| Thyroid shield | +++ | |||
| Leaded glasses | + + | |||
| Leaded gloves | + + | |||
| Ceiling-suspended shield | +++ | |||
| Tableside shield | +++ | |||
a‘+’ can change operator radiation dose by less than 100%.
‘++’ can change operator radiation dose by 2- or 3-fold.
‘+++’ can change operator radiation dose by up to an order of magnitude.
Patient factors
Patient factors cannot be modified by the operator. The clinical indication for the procedure and the characteristics of the lesion determine procedure complexity. Complexity is a major determinant of fluoroscopy time and cineradiography time, which in turn determine the patient dose and the scatter dose to the operator(9–14). The patient's body size also has an important effect on the patient dose and therefore on the operator dose(21,22). A good general rule of thumb is that the dose needed to penetrate the patient doubles with every additional 3 cm of patient body thickness(23).
Physician factors
Some physician factors cannot be modified. For example, the operator's height has an effect on the operator dose. The dose rate at eye level decreases by a factor of 2 when the physician's eye level increases from 1.6 to 1.8 m above the floor(24). Gender also has an effect on the operator dose. Theocharopoulos et al. calculated that males in an electrophysiology laboratory received about twice the gonad dose as females in the same type of laboratory(25).
Some physician factors can be changed, but only over relatively long periods of time. Physician skill level affects the time required to carry out a procedure and thus the operator radiation dose(26–30). Physicians in training often receive significantly greater radiation doses than staff physicians(31). It has been estimated that cardiology fellows in their first year of training receive 60% more radiation dose than fellows in their second year of training(32). This difference is largely due to longer fluoroscopy times for positioning catheters. Kottou et al.(33) attributed the wide range of operator doses among physicians in the same hospital to differences in physicians' skill and practice.
Other physician factors have a substantial effect on the operator dose and can be modified almost immediately. Coulden and Readman(34) reported wide variations in physicians' practices (e.g. number of views, fluoroscopy time and cineradiography time during routine diagnostic procedures) and observed 4-fold variations in patient doses between hospitals.
Changes in procedure technique can reduce the radiation dose to physicians, either by reducing fluoroscopy time or by increasing the distance between the physician and the patient during the procedure. For example, reduced fluoroscopy time was demonstrated by substituting monorail catheter systems for over-the-wire catheters(35–37). Use of a remotely controlled mechanical pump for contrast media injection demonstrated a 2-fold decrease in the radiation dose to the operator compared with hand injection of contrast material(26,38).
Numerous studies have compared the occupational radiation doses associated with the use of different catheter insertion sites(26,29,39–45). The most common insertion sites for PCI are the femoral and radial/brachial (referred to below as radial) approaches. The catheter insertion site has an effect on the physician's position relative to the patient during cardiac procedures. The radial approach requires the cardiologist to work in closer proximity to the X-ray beam(44). Most studies report higher physician exposures when the radial approach is used. Reasons for the higher doses include closer proximity of the physician to the X-ray field and longer fluoroscopy times. Reported operator doses received with the radial approach were about twice that with the femoral approach(45). The subclavian approach, used for implantation of pacemakers and similar devices, yields operator exposure rates that are considerably higher than when the femoral and radial approaches are used, due to the operator's proximity to the X-ray beam when using the subclavian approach(27,42).
The typical distance between the operator and the centre of the patient's scatter volume is 0.75 m in cardiac procedures(46). Radiation exposure is inversely proportional to the square of the distance from the X-ray source. Increasing the distance between the cardiologist and the patient to 1 m can decrease a physician's occupational radiation dose by about half. One study showed that the radiation dose to physicians who step away from the patient during cineradiography was 9 times less than the dose to physicians who remain next to the patient(47).
The distribution of scattered radiation around the patient is non-uniform and asymmetric(25,47,48). The effective dose received by an operator within a 1.5-m radius from the edge of the table can vary by a factor of 40 depending on the operator's position(25). For posteroanterior and right anterior oblique projections, the scatter dose is highest at the left side of the patient's chest, while for the left anterior oblique (LAO) projection, it is highest at the right side of the patient's chest . The scattered radiation dose was much lower on the opposite side of the patient table and decreases with the distance from patient's chest region. The radiation dose distribution around the patient table explains why the subclavian and radial approaches yield higher exposure rates to the operator in comparison with the femoral approach.
Generally, radiation doses are higher on the left side of the operator's body because the left side is closer to the X-ray beam when the cardiologist is standing at the patient's right side (the usual case for PCI and ablation procedures)(46,49–55). Goni et al.(54) reported significantly higher doses to the cardiologist's left hand. Kicken et al.(56) reported a 1.5–2.5 times greater entrance dose on the operator's left side compared with the operator's front. Chong et al.(53) reported a 6-fold higher exposure to the lens of the left eye when compared with the lens of the right eye. Radiation monitoring badges should be worn on the left side of the body in order to accurately reflect the operator dose.
A physician's awareness of radiation exposure can result in a marked decrease in his or her occupational dose(57,58). When a physician stands at the patient's right groin and uses a femoral approach, the LAO cranial projection results in the highest operator dose rate for radiation scatter(18,24,59). In one study, after cardiologists were informed about the relatively high scatter dose to operators when the LAO projection is used, there was a remarkable reduction in the use of the LAO projection and the average physician dose was reduced about 2.3-fold(58). Awareness of radiation dose levels can be maintained by providing regular education about the radiation dose and radiation protection as part of an ongoing educational programme.
Shielding
Radiation shielding is one of the most efficient and easiest methods to protect staff during fluoroscopic operation. Protective shields used for the cardiac catheterisation procedure include protective clothing and movable shields.
Personal protective shields include aprons, thyroid shields, glasses and gloves. An apron or thyroid shield with a 0.5-mm lead-equivalent thickness will attenuate more than 95% of X rays at the typical X-ray energies used during fluoroscopically guided procedures.
Leaded glasses have been reported to attenuate as little as 35% to as much as >95% of X rays at typical X-ray energies(60–66). This wide variation has many causes. They include physician movement during the procedure, the presence or absence of side shields on the glasses, the location at which the dose was measured under the leaded glasses and scattered X rays from portions of the head, which are not protected by the glasses. During interventional cardiac procedures, side shields are important because scattered X rays generally come from the left side of the operator.
Experimental results with commercial tungsten or lead surgical gloves indicate that attenuation of scatter radiation at 100 kVp ranges from 21 to 50% depending on the glove model(67). However, protective gloves do not necessarily reduce radiation exposure(68). If the operator's hand is in the primary beam, the automatic brightness control system in modern fluoroscopy units will increase the exposure rate to penetrate the lead shielding in the glove, thereby increasing the hand dose. In addition, difficulties in the manipulation of catheters and guidewires—due to the increased thickness of leaded gloves when compared with standard surgical gloves—can also increase procedural time. The only circumstance in which leaded gloves may be useful is when the operator's hands will be near, but not in, the radiation field. The possible decrease in the radiation dose to the operator's hands must be balanced against the decreased manual dexterity, which is a frequent concomitant of leaded gloves.
The most common types of movable shields are ceiling-suspended tableside shields. Ceiling-suspended screens provide protection for the eyes and upper body and can be used as a substitute for leaded glasses and a thyroid shield. It has been reported that ceiling-suspended shields can reduce the operator dose by a factor of 3–20(24,46). The appropriate use of these screens is important because the operator dose varies with the location of the screen. The ceiling-suspended screen should be placed between the operator and the source of scatter. To protect as much of the upper body as possible, the screen should be placed as close to the scatter source as possible, rather than as close as possible to the operator. Hand protection from a ceiling-suspended screen depends on its position. No significant reduction of hand irradiation was reported by Whitby and Martin(44), whereas an 8-fold reduction was reported by Wyart et al.(69)
A tableside shield extends from the table towards the floor. It protects against stray radiation scattered downwards from the patient towards the operator's gonads, legs and feet. These shields are often mounted on the table. The X-ray tube for the frontal plane should be positioned below the patient during cardiac procedures. This produces a greater scatter radiation level below the patient table than above it. The result is a higher radiation dose to the operator's gonads and legs than to the operator's upper body. A tableside shield reduces the dose to the operator's gonads and legs by a factor of 10–40(25,49).
SUMMARY
Wide variations in the operator dose have been observed for fluoroscopically guided cardiac interventions. These variations may be as much as two to three orders of magnitude and are present even when the effects of variation in the patient dose are excluded. Despite extensive improvements in fluoroscopy equipment and the introduction of various dose-reduction technologies, there has been no reduction in the operator dose for PCI. This is believed to be the result of the increasing complexity of these interventions. The lack of reduction in operator doses and the wide variation in these doses strongly suggest that more attention must be paid to other factors that influence the operator dose. Some, such as patient and lesion characteristics and operator height and gender, are not under the operator's control. Others, such as operator experience, only change over years.
However, an operator can change some factors immediately, with a concomitant immediate reduction in the operator dose. These include procedure techniques, catheter choice, catheter insertion site, operator positioning and the appropriate use of personal protective devices. Awareness of one's own radiation dose is essential, as it provides motivation for incorporating changes in one's practice that will result in a lower radiation dose. Changes in operator practices can be accomplished rapidly by a motivated operator at minimal or no cost and can have a substantial effect on the operator dose.
ACKNOWLEDGEMENTS
This study was supported by the Intramural Research Programme of the National Institute of Health, National Cancer Institute, Division of Cancer Epidemiology and Genetics.
REFERENCES
- 1.Thom T., et al. Heart disease and stroke statistics—2006 update—a report from the American Heart Association Statistics Committee and Stroke Statistics Subcommittee. Circulation. 2006;113:E85–E151. doi: 10.1161/CIRCULATIONAHA.105.171600. [DOI] [PubMed] [Google Scholar]
- 2.Togni M., Balmer F., Pfiffner D., Meier W., Zeiher A. M., Meier B. Percutaneous coronary interventions in Europe 1992–2001. Eur. Heart J. 2004;25:1208–1213. doi: 10.1016/j.ehj.2004.04.024. [DOI] [PubMed] [Google Scholar]
- 3.Finkelstein M. M. Is brain cancer an occupational disease of cardiologists? Can. J. Cardiol. 1998;14:1385–1388. [PubMed] [Google Scholar]
- 4.Hardell L., Mild K. H., Pahlson A., Hallquist A. Ionizing radiation, cellular telephones and the risk for brain tumours. Eur. J. Cancer Prev. 2001;10:523–529. doi: 10.1097/00008469-200112000-00007. [DOI] [PubMed] [Google Scholar]
- 5.Hirshfeld J. W., et al. ACCF/AHA/HRS/SCAI clinical competence statement on physician knowledge to optimize patient safety and image quality in fluoroscopically guided invasive cardiovascular procedures—a report of the American College of Cardiology Foundation/American Heart Association/American College of Physicians Task Force on Clinical Competence and Training. J. Am. Coll. Cardiol. 2004;44:2259–2282. doi: 10.1016/j.jacc.2004.10.014. [DOI] [PubMed] [Google Scholar]
- 6.Kim K. P., Miller D. L., Balter S., Kleinerman R. A., Linet M. S., Kwon D., Simon S. L. Occupational radiation doses to operators performing cardiac catheterization procedures. Health Phys. 2008;94:211–227. doi: 10.1097/01.HP.0000290614.76386.35. [DOI] [PubMed] [Google Scholar]
- 7.Chida K., Fuda K., Saito H., Takai Y., Takahashi S., Yamada S., Kohzuki M., Zuguchi M. Patient skin dose in cardiac interventional procedures: conventional fluoroscopy versus pulsed fluoroscopy. Catheter. Cardiovasc. Interv. 2007;69:115–121. doi: 10.1002/ccd.20961. [DOI] [PubMed] [Google Scholar]
- 8.Mahesh M. The AAPM/RSNA physics tutorial for residents—fluoroscopy: patient radiation exposure issues. Radiographics. 2001;21:1033–1045. doi: 10.1148/radiographics.21.4.g01jl271033. [DOI] [PubMed] [Google Scholar]
- 9.Balter S., Bernardi G., Cotelo E., Faulkner K., Miller D. L., Nowotny R., Lopez P. O., Padovani R., Ramirez A., Vano E. Potential radiation guidance levels for invasive cardiology. Med. Phys. 2006;33:2212–2212. [Google Scholar]
- 10.Bernardi G., Padovani R., Morocutti G., Vano E., Malisan M. R., Rinuncini M., Spedicato L., Fioretti P. M. Clinical and technical determinants of the complexity of percutaneous transluminal coronary angioplasty procedures: analysis in relation to radiation exposure parameters. Catheter. Cardiovasc. Interv. 2000;51:1–9. doi: 10.1002/1522-726x(200009)51:1<1::aid-ccd1>3.0.co;2-k. [DOI] [PubMed] [Google Scholar]
- 11.Nikolsky M., et al. An evaluation of fluoroscopy time and correlation with outcomes after percutaneous coronary intervention. J. Invasive Cardiol. 2007;19:208–213. [PubMed] [Google Scholar]
- 12.Padovani R., Bernardi G., Malisan M. R., Vano E., Morocutti G., Fioretti P. M. Patient dose related to the complexity of interventional cardiology procedures. Radiat. Prot. Dosim. 2001;94:189–192. doi: 10.1093/oxfordjournals.rpd.a006469. [DOI] [PubMed] [Google Scholar]
- 13.Peterzol A., Quai E., Padovani R., Bernardi G., Kotre C. J., Dowling A. Reference levels in PTCA as a function of procedure complexity. Radiat. Prot. Dosim. 2006;117:54–58. doi: 10.1093/rpd/nci719. [DOI] [PubMed] [Google Scholar]
- 14.Tsapaki V., Magginas A., Vano E. S. K., Papadakis E., Dafnomili P., Kyrozi E., Kollaros N. V. N., Cokkinos D. Factors that influence radiation dose in percutaneous coronary intervention. J. Interv. Cardiol. 2006;19:237–244. doi: 10.1111/j.1540-8183.2006.00137.x. [DOI] [PubMed] [Google Scholar]
- 15.Huckman R. S., Pisano G. P. Adopting new technologies: Turf battles in coronary revascularization. N. Engl. J. Med. 2005;352:857–859. doi: 10.1056/NEJMp048242. [DOI] [PubMed] [Google Scholar]
- 16.Rosamond W., et al. Heart disease and stroke statistics—2007 update—a report from the American Heart Association Statistics Committee and Stroke Statistics Subcommittee. Circulation. 2007;115:e69–e171. doi: 10.1161/CIRCULATIONAHA.106.179918. [DOI] [PubMed] [Google Scholar]
- 17.McCormick V. A., Schultz C. C., Hollingsworth-Schuler V., Campbell J. M., O'Neill W. W., Ramos R. Reducing radiation dose in the cardiac catheterization laboratory by design alterations and staff education. Am. J. Cardiol. 2002;90:903–905. doi: 10.1016/s0002-9149(02)02724-8. [DOI] [PubMed] [Google Scholar]
- 18.Camm A. J., Reid J., Raphael M., Wilde P., Boyle R., Clarke M., Qureshi S., Rothman M., Shaw A. Radiation hazards to the cardiologist—a report of a Subcommittee of the British-Cardiac-Society. Br. Heart J. 1993;70:489–496. doi: 10.1136/hrt.70.5.489. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Tsapaki V., Kottou S., Kollaros N., Dafnomili P., Koutelou M., Vano E., Neofotistou V. Comparison of a conventional and a flat-panel digital system in interventional cardiology procedures. Br. J. Radiol. 2004;77:562–567. doi: 10.1259/bjr/83257582. [DOI] [PubMed] [Google Scholar]
- 20.Vano E., Geiger B., Schreiner A., Back C., Beissel J. Dynamic flat panel detector versus image intensifier in cardiac imaging: dose and image quality. Phys. Med. Biol. 2005;50:5731–5742. doi: 10.1088/0031-9155/50/23/022. [DOI] [PubMed] [Google Scholar]
- 21.Ector J., Dragusin O., Adriaenssens B., Huybrechts W., Willems R., Ector H., Heidbuechel H. Obesity is a major determinant of radiation dose in patients undergoing pulmonary vein isolation for atrial fibrillation. J. Am. Coll. Cardiol. 2007;50:234–242. doi: 10.1016/j.jacc.2007.03.040. [DOI] [PubMed] [Google Scholar]
- 22.Cusma J. T., Bell M. R., Wondrow M. A., Taubel J. P., Holmes D. R. Real-time measurement of radiation exposure to patients during diagnostic coronary angiography and percutaneous interventional procedures. J. Am. Coll. Cardiol. 1999;33:427–435. doi: 10.1016/s0735-1097(98)00591-9. [DOI] [PubMed] [Google Scholar]
- 23.Detorie M., Mahesh M., Schueler B. A. Reducing occupational exposure from fluoroscopy. J. Am. Coll. Radiol. 2007;4:335–337. doi: 10.1016/j.jacr.2007.01.018. [DOI] [PubMed] [Google Scholar]
- 24.Pratt T. A., Shaw A. J. Factors affecting the radiation-dose to the lens of the eye during cardiac-catheterization procedures. Br. J. Radiol. 1993;66:346–350. doi: 10.1259/0007-1285-66-784-346. [DOI] [PubMed] [Google Scholar]
- 25.Theocharopoulos N., Damilakis J., Perisinakis K., Manios E., Vardas P., Gourtsoyiannis N. Occupational exposure in the electrophysiology laboratory: quantifying and minimizing radiation burden. Br. J. Radiol. 2006;79:644–651. doi: 10.1259/bjr/76128583. [DOI] [PubMed] [Google Scholar]
- 26.Grant S. C. D., Faragher E. B., Hufton A. P., Bennett D. H. Use of a remotely controlled mechanical pump for coronary arteriography—a study of radiation exposure and quality implications. Br. Heart J. 1993;70:479–484. doi: 10.1136/hrt.70.5.479. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Limacher M. C., Douglas P. S., Germano G., Laskey W. K., Lindsay B. D., McKetty M. H., Moore M. E., Park J. K., Prigent F. M., Walsh M. N. Radiation safety in the practice of cardiology. J. Am. Coll. Cardiol. 1998;31:892–913. doi: 10.1016/s0735-1097(98)00047-3. [DOI] [PubMed] [Google Scholar]
- 28.Park T. H., Eichling J. O., Schechtman K. B., Bromberg B. I., Smith J. M., Lindsay B. D. Risk of radiation induced skin injuries from arrhythmia ablation procedures. Pace. 1996;19:1363–1369. doi: 10.1111/j.1540-8159.1996.tb04216.x. [DOI] [PubMed] [Google Scholar]
- 29.Larrazet F., Dibie A., Philippe F., Palau R., Klausz R., Laborde F. Factors influencing fluoroscopy time and dose-area product values during ad hoc one-vessel percutaneous coronary angioplasty. Br. J. Radiol. 2003;76:473–477. doi: 10.1259/bjr/21553230. [DOI] [PubMed] [Google Scholar]
- 30.Tsapaki V., Kottou S., Vano E., Faulkner K., Giannouleas J., Padovani R., Kyrozi E., Koutelou M., Vardalaki E., Neofotistou V. Patient dose values in a dedicated Greek cardiac centre. Br. J. Radiol. 2003;76:726–730. doi: 10.1259/bjr/73325000. [DOI] [PubMed] [Google Scholar]
- 31.Renaud L. A 5-year follow-up of the radiation exposure to in-room personnel during cardiac catheterization. Health Phys. 1992;62:10–15. doi: 10.1097/00004032-199201000-00002. [DOI] [PubMed] [Google Scholar]
- 32.Watson L. E., Riggs M. W., Bourland P. D. Radiation exposure during cardiology fellowship training. Health Phys. 1997;73:690–693. doi: 10.1097/00004032-199710000-00016. [DOI] [PubMed] [Google Scholar]
- 33.Kottou S., Neofotistou V., Tsapaki V., Lobotessi H., Manetou A., Molfetas M. G. Personnel doses in haemodynamic units in Greece. Radiat. Prot. Dosim. 2001;94:121–124. doi: 10.1093/oxfordjournals.rpd.a006454. [DOI] [PubMed] [Google Scholar]
- 34.Coulden R. A., Readman L. P. Coronary angiography—an analysis of Radiographic Practice in the UK. Br. J. Radiol. 1993;66:327–331. doi: 10.1259/0007-1285-66-784-327. [DOI] [PubMed] [Google Scholar]
- 35.Linnemeier T. J., Klette M. A., Rothbaum D. A., Landin R. J., Ball M. W., Riddell R. V. Rail-type systems reduce radiation exposure and procedure time compared to over-the-wire coronary angioplasty systems. Circulation. 1992;86(Suppl II):I–445. [Google Scholar]
- 36.Linnemeier T. J., Mccallister S. H., Lips D. L., Klette M. A., Rothbaum D. A., Ball M. W., Landin R. J., Hodes Z. I., Riddell R. V. Radiation exposure—comparison of rapid exchange and conventional over-the-wire coronary angioplasty systems. Catheter. Cardio. Diagn. 1993;30:11–14. doi: 10.1002/ccd.1810300104. [DOI] [PubMed] [Google Scholar]
- 37.Mooney M. R., Douglas J. S., Mooney J. F., Madison J. D., Brandenburg R. O., Fernald R., Vantassel R. A. Monorail Piccolino catheter—a new rapid exchange ultralow profile coronary angioplasty system. Catheter. Cardiovasc. Diagn. 1990;20:114–119. doi: 10.1002/ccd.1810200210. [DOI] [PubMed] [Google Scholar]
- 38.Grant S. C. D., Bennett D. H., Mather J. M. Reduction of radiation exposure to the cardiologist during coronary angiography by the use of a remotely controlled mechanical pump for injection of contrast-medium. Catheter. Cardiovasc. Diagn. 1992;25:107–109. doi: 10.1002/ccd.1810250206. [DOI] [PubMed] [Google Scholar]
- 39.Johnson L. W., Moore R. J., Balter S. Review of radiation safety in the cardiac-catheterization laboratory. Catheter. Cardiovasc. Diagn. 1992;25:186–194. doi: 10.1002/ccd.1810250304. [DOI] [PubMed] [Google Scholar]
- 40.Lange H. W., von Boetticher H. Randomized comparison of operator radiation exposure during coronary angiography and intervention by radial or femoral approach. Catheter. Cardiovasc. Interv. 2006;67:12–16. doi: 10.1002/ccd.20451. [DOI] [PubMed] [Google Scholar]
- 41.Le Heron J. C., Mitchell A. W. Scattered radiation doses during cardiac studies using a U-arm type fluoroscopy system. Australas Radiol. 1985;29:335–340. doi: 10.1111/j.1440-1673.1985.tb01725.x. [DOI] [PubMed] [Google Scholar]
- 42.Lindsay B. D., Eichling J. O., Ambos H. D., Cain M. E. Radiation exposure to patients and medical personnel during radiofrequency catheter ablation for supraventricular tachycardia. Am. J. Cardiol. 1992;70:218–223. doi: 10.1016/0002-9149(92)91278-c. [DOI] [PubMed] [Google Scholar]
- 43.Mann J. T., Cubeddu G., Arrowood M. Operator radiation exposure in PTCA: comparison of radial and femoral approaches. J. Invasive Cardiol. 1996;8:D22–D25. [PubMed] [Google Scholar]
- 44.Whitby M., Martin C. J. A study of the distribution of dose across the hands of interventional radiologists and cardiologists. Br. J. Radiol. 2005;78:219–229. doi: 10.1259/bjr/12209589. [DOI] [PubMed] [Google Scholar]
- 45.Wholey M. H. Clinical dosimetry during angiographic examination—comments on coronary arteriography. Circulation. 1974;50:627–631. doi: 10.1161/01.cir.50.3.627. [DOI] [PubMed] [Google Scholar]
- 46.Vano E., Gonzalez L., Guibelalde E., Fernandez J. M., Ten J. I. Radiation exposure to medical staff in interventional and cardiac radiology. Br. J. Radiol. 1998;71:954–960. doi: 10.1259/bjr.71.849.10195011. [DOI] [PubMed] [Google Scholar]
- 47.Jeans S. P., Faulkner K., Love H. G., Bardsley R. A. An investigation of the radiation-dose to staff during cardiac radiological studies. Br. J. Radiol. 1985;58:419–428. doi: 10.1259/0007-1285-58-689-419. [DOI] [PubMed] [Google Scholar]
- 48.Balter S. Stray radiation in the cardiac catheterisation laboratory. Radiat. Prot. Dosim. 2001;94:183–188. doi: 10.1093/oxfordjournals.rpd.a006468. [DOI] [PubMed] [Google Scholar]
- 49.Balter S., Sones F. M., Brancato R. Radiation exposure to operator performing cardiac angiography with U-arm systems. Circulation. 1978;58:925–932. doi: 10.1161/01.cir.58.5.925. [DOI] [PubMed] [Google Scholar]
- 50.Gustafsson M., Lunderquist A. Personnel exposure to radiation at some angiographic procedures. Radiology. 1981;140:807–811. doi: 10.1148/radiology.140.3.7280251. [DOI] [PubMed] [Google Scholar]
- 51.Kaude J., Svahn G. Absorbed, gonad and integral doses to patient and personnel from angiographic procedures. Acta Radiol. Diagn. 1974;15:454–464. doi: 10.1177/028418517401500412. [DOI] [PubMed] [Google Scholar]
- 52.Rueter F. G. Physician and patient exposure during cardiac-catheterization. Circulation. 1978;58:134–139. doi: 10.1161/01.cir.58.1.134. [DOI] [PubMed] [Google Scholar]
- 53.Chong N. S., Yin W. H., Chan P., Cheng M. C., Ko H. L., Jeng S. C., Lee J. J. S. Evaluation of absorbed radiation dose to working staff during cardiac catheterization procedures. Chin. Med. J. 2000;63:816–821. [PubMed] [Google Scholar]
- 54.Goni H., Papadopoulou D., Yakoumakis E., Stratigis N., Benos J., Siriopoulou V., Makri T., Georgiou E. Investigation of occupational radiation exposure during interventional cardiac catheterisations performed via radial artery. Radiat. Prot. Dosim. 2005;117:107–110. doi: 10.1093/rpd/nci763. [DOI] [PubMed] [Google Scholar]
- 55.Lima F. R. A., Khoury H. J., Hazin C. A., Luz L. P. Doses to the operating staff during interventional cardiology procedures. The 10th International Congress of the International Radiation Protection Association; Hiroshima. 2000. [Google Scholar]
- 56.Kicken P. J. H., Kemerink G. J., Schultz F. W., Zoetelief J., Broerse J. J., van Engelshoven J. M. A. Dosimetry of occupationally exposed persons in diagnostic and interventional arteriography. Part II: Assessment of effective dose. Radiat. Prot. Dosim. 1999;82:105–114. [Google Scholar]
- 57.Huyskens C. J., Hummel W. A. Data-analysis on patient exposures in cardiac angiography. Radiat. Prot. Dosim. 1995;57:475–480. [Google Scholar]
- 58.Pitney M. R., Allan R. M., Giles R. W., Mclean D., Mccredie M., Randell T., Walsh W. F. Modifying fluoroscopic views reduces operator radiation exposure during coronary angioplasty. J. Am. Coll. Cardiol. 1994;24:1660–1663. doi: 10.1016/0735-1097(94)90171-6. [DOI] [PubMed] [Google Scholar]
- 59.Kuon E., Dahm J. B., Empen K., Robinson D. M., Reuter G., Wucherer M. Identification of less-irradiating tube angulations in invasive cardiology. J. Am. Coll. Cardiol. 2004;44:1420–1428. doi: 10.1016/j.jacc.2004.06.057. [DOI] [PubMed] [Google Scholar]
- 60.Agarwal S. K., Friesen E. J., Huddleston A. L., Rao R. P. Effectiveness of glass lenses in reducing exposure to eyes. Radiology. 1978;129:810–811. doi: 10.1148/129.3.810. [DOI] [PubMed] [Google Scholar]
- 61.Bergstrom K., Jorulf H., Lofroth P. O. Eye lens protection for radiological personnel. Radiology. 1977;124:839–840. doi: 10.1148/124.3.839. [DOI] [PubMed] [Google Scholar]
- 62.Richman A. H., Chan B., Katz M. Effectiveness of lead lenses in reducing radiation exposure. Radiology. 1976;121:357–359. doi: 10.1148/121.2.357. [DOI] [PubMed] [Google Scholar]
- 63.Cousin A. J., Lawdahl R. B., Chakraborty D. P., Koehler R. E. The case for radioprotective eyewear facewear—practical implications and suggestions. Invest. Radiol. 1987;22:688–692. doi: 10.1097/00004424-198708000-00012. [DOI] [PubMed] [Google Scholar]
- 64.Dash H., Leaman D. M. Operator radiation exposure during percutaneous trans-luminal coronary angioplasty. J. Am. Coll. Cardiol. 1984;4:725–728. doi: 10.1016/s0735-1097(84)80398-8. [DOI] [PubMed] [Google Scholar]
- 65.Marshall N. W., Faulkner K., Clarke P. An investigation into the effect of protective devices on the dose to radiosensitive organs in the head and neck. Br. J. Radiol. 1992;65:799–802. doi: 10.1259/0007-1285-65-777-799. [DOI] [PubMed] [Google Scholar]
- 66.Mcparland B. J., Nosil J., Burry B. A survey of the radiation exposures received by the staff at 2 cardiac-catheterization laboratories. Br. J. Radiol. 1990;63:885–888. doi: 10.1259/0007-1285-63-755-885. [DOI] [PubMed] [Google Scholar]
- 67.Vano E., Fernandez J. M., Delgado V., Gonzalez L. Evaluation of tungsten and lead surgical gloves for radiation protection. 1995;68:855–858. doi: 10.1097/00004032-199506000-00016. [DOI] [PubMed] [Google Scholar]
- 68.Balter S. Radiation safety in the cardiac catheterization laboratory: operational radiation safety. Catheter. Cardiovasc. Interv. 1999;47:347–353. doi: 10.1002/(sici)1522-726x(199907)47:3<347::aid-ccd23>3.0.co;2-n. [DOI] [PubMed] [Google Scholar]
- 69.Wyart P., Dumant D., Gourdier M., Nassar F., Bouthillon J. C., Chestier Y. Contribution of self-surveillance of the personnel by electronic radiation dosemeters in invasive cardiology. Arch. Mal. Coeur. Vaiss. 1997;90:233–238. [PubMed] [Google Scholar]