Abstract
Proponents of navigated hip arthroplasty have suggested that it may increase the precision of acetabular component placement. We conducted a systematic review and meta-analysis to evaluate the validity of this theory. We searched, in duplicate, MEDLINE, EMBASE and the Cochrane Central Register of Controlled Trials for randomised trials comparing the use of computer navigation with the freehand technique for acetabular cup placement within the desired alignment. We assessed the methodological quality of the studies and abstracted the relevant data. Tests of heterogeneity and publication bias were performed. From the three studies included, there was no evidence of heterogeneity between studies. A total of 250 patients were entered into the analysis. The beneficial odds ratio for the number of outliers was 0.285 (95% confidence interval [CI]: 0.143 to 0.569; p < 0.001). We conclude that navigation in hip arthroplasty improves the precision of acetabular cup placement by decreasing the number of outliers from the desired alignment.
Résumé
On peut penser que l’utilisation de la navigation au cours des prothèses de hanche va améliorer la précision du positionnement cotyloïdien. Nous avons conduit une étude systématique et une méta analyse de façon à valider cette théorieMéthode : les recherches ont été réalisé sur MEDLINE, EMBASE et COCHRANE, essais randomisés comparant l’utilisation de la navigation et l’utilisation des techniques classiques à main levée. Différents tests statistiques ont été réalisés.Résultat : à partir de 3 études inclues, il n’y a pas de différence entre ces 3 études. Un total de 250 patients ont été analysés, le ratio des hanches en dehors de la moyenne a été de 0,285 (95% CI: 0,143 et 0,569; p < 0,001). Nous pouvons affirmer que la navigation au cours de la prothèse totale de hanche permet une meilleure précision du positionnement de la cupule et diminue le nombre de cupules en mauvaise position.
Introduction
The position of the acetabular component is critical to the function and outcome of total hip arthroplasty (THA). Achieving the correct abduction and anteversion could potentially improve the longevity of a THA, improve the range of motion (ROM) and decrease the dislocation rate [1, 8, 14]. Lewinnek et al. recommended an abduction angle of 40 ± 10° and an anteversion angle of 15 ± 10° as the safe zone for cup orientation [10].
The correct placement of implants is guided by pre-operative radiographs and templating, intra-operative anatomical landmarks and mechanical alignment guides on the instrumentation sets. However, patient positioning on the table is variable and mechanical alignment guides have not improved the accuracy of acetabular positioning [2].
Computer-assisted surgery is growing in popularity to help control and minimise the error in cup placement. Two forms of computer-assisted surgery exist for total hip replacements (THR); one is an active system, which uses a robot to implant the cup, and the other is a passive system, whereby the surgeon navigates the instruments and components within a virtual picture intra-operatively. Within the passive systems, there are two variations. Image-based systems require the collection of anatomical data from preoperative computed tomography (CT) or intra-operative fluoroscopy. Imageless systems use a virtual model supplemented by intra-operative registration data. We focus on the passive navigation systems in this paper.
A number of observational-type studies have been published on computer navigation in THR, but the potential for selection bias in these studies limits the generalisation of their results [3, 5, 6, 12, 15–17]. Randomised clinical trials (RCT) represent the best available evidence, as they control for potential confounding errors between groups.
A systematic review of the literature was conducted for RCTs to determine if computer navigation improves the precision of acetabular cup placement in hip arthroplasty. We report our meta-analysis as recommended by the Quality of Reporting of Meta-analyses (QUOROM) statement [11].
Materials and methods
Study identification
Two of the authors (RG and AM) independently completed a computerised search of the electronic databases PubMed, MEDLINE and Ovid MEDLINE (1966 to Mar 2007), and EMBASE (1980 to 2007) with the following search terms (computer OR computer navigation OR navigation) AND (hip arthroplasty OR joint replacement OR joint prosthesis OR arthroplasty). We also searched the Cochrane Database of Systematic Reviews, the Cochrane Central Register of Controlled Trials, the web site of the United Kingdom National Research Register (https://portal.nihr.ac.uk/Pages/NRRArchive.aspx) and http://clinicaltrials.gov/. After reviewing the title of the study, we retrieved the abstract if we felt that it was an appropriate study. We independently reviewed these abstracts and chose the studies that were potentially relevant. The full text article was then reviewed to determine final inclusion into the study. We then reviewed the bibliography of each article that met our inclusion criteria for any further relevant studies.
Eligibility criteria
We included those articles relevant to: (1) those patients undergoing primary THR; (2) the intervention was the use of computer navigation as compared to the freehand technique for placing the acetabular component; (3) the outcome measure was the number of outliers of acetabular cups outside the desired alignment range and (4) the study was a published or unpublished randomised controlled trial.
Assessment of study quality
Each study was evaluated for its methodological quality. To determine the random allocation sequence, one study used a computerised random number generator [13], one study used sealed envelopes [9] and one did not report their technique [7]. Two studies described a 100% follow-up rate [7, 13], while one did not discuss their follow-up rate [9]. All co-interventions between groups were comparable. All post-operative alignment measurements were taken by an independent observer blinded to the randomisation group of the patient. Two papers discussed analysing the final outcomes by the intention-to-treat principle [7, 13], while one did not [9]. All papers were considered to be of satisfactory quality.
Data extraction
For each eligible study, two of the authors extracted the relevant data for both the intervention and control groups. This included demographic data (age, sex and body mass index [BMI]), the number of acetabular outliers from the desired range, intervention protocol, duration of the study, loss to follow-up and sources of funding.
Study characteristics
All papers were published in English. One study compared the freehand technique with an imageless navigation system [13], one compared freehand to a CT-based navigation system [9] and one study compared all three techniques [7]. Patients undergoing CT-based and imageless navigation were combined into one navigation group in our analysis. Two studies measured the post-operative acetabular position with CT scans and one employed radiographs. All acetabular components were of the press-fit type. One study indicated that the surgeon had experience of 50 prior navigation cases before the commencement of the study.
Statistical analysis
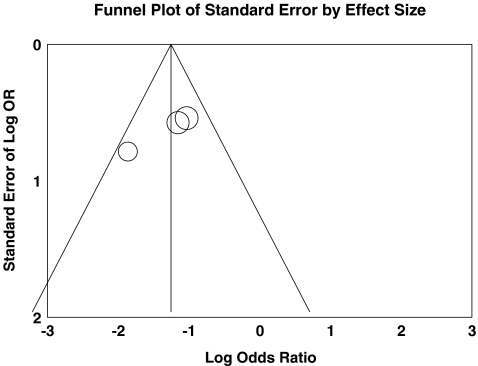
The study heterogeneity was assessed and a p-value of <0.1 was considered to be suggestive of statistical heterogeneity. Publication bias was assessed with funnel plots, which demonstrate the relationship between the sample size of the studies and the precision in estimating the treatment effect. Bias can be seen if the plots are widely skewed compared to a plot resembling an inverted triangle, which represents no bias [4].
For the categorical outcome of acetabular alignment within the desired range, we used the odds ratio as the summary statistic. This ratio represents the odds of acetabular outliers from the accepted range of alignment occurring in the computer navigation group compared with the freehand group. An odds ratio of less than 1 favours the treatment group and the point estimate of the odds ratio is considered to be statistically significant if the 95% confidence interval does not include the value 1. We used the Mantel-Haenszel method to combine the odds ratio for the outcome of interest using the fixed effects model, as there was no evidence of heterogeneity between studies. Analysis was carried out by using Comprehensive Meta-analysis version 1.0 (Englewood, NJ).
Results
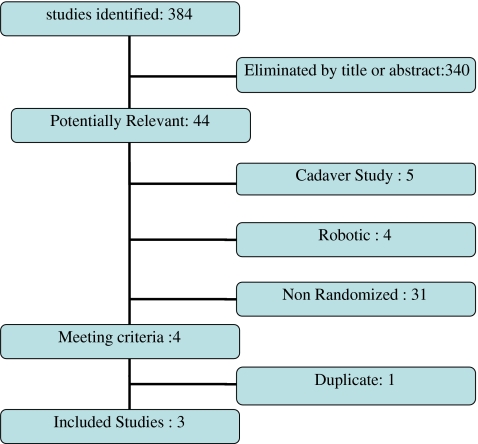
We identified 384 studies from our searches and, after applying our eligibility criteria, we had three manuscripts for systematic review and data synthesis [7, 9, 13]. Forty-four abstracts were potentially relevant; however, we excluded five studies because they were cadaveric studies, four studies were using active navigation systems, such as robots, 31 studies did not fit the criteria of randomised controlled studies and one study was a duplicate. The details of the search is depicted in Fig. 1.
Fig. 1.
Search results and the selection procedure
The patient groups were well matched at baseline for the available demographic data. The navigated group consisted of 140 patients with a mean age of 62.1 years and the freehand group (control group) comprised 110 patients with a mean age of 64.2 years. A total of 250 patients were entered into the analysis. The mean BMI in the control group was 27.2 kg/m2, compared to 26.9 kg/m2 in the navigation group. One study did not report the BMI of their two study groups [9]. Table 1 describes the characteristics of these studies. Table 2 shows the outcome data from the individual studies.
Table 1.
Demographic data of the study patients
| Study | Mean age (SD) | Mean BMI kg/m2 (SD) | ||
|---|---|---|---|---|
| Control | Navigation | Control | Navigation | |
| Kalteis et al., n = 90 | 64.7 (8.6) | 63.5 (8.6) | 28.5 (4.1) | 27.7 (3.85) |
| Leenders et al., n = 100 | 64.9 | 61 | ||
| Parratte et al., n = 60 | 62.6 (9.6) | 61.2 (13.15) | 25.2 (4.1) | 25.6 (4.53) |
Table 2.
Data for the individual studies of acetabular alignment and outliers from the desired alignment
| Study | Percentage of outliers | Mean abduction angles (SD) | Mean anteversion angles | |||
|---|---|---|---|---|---|---|
| Control | Navigation | Control | Navigation | Control | Navigation | |
| Kalteis et al., n = 90 | 16/30 (53%) | 7/60 (11.7%) | 43.7 (7.3) | 42.4 (4) | 22 (14.2) | 13.0 (5.4) |
| Leenders et al., n = 100 | 13/50 (26%) | 2/50 (4%) | 46 | 47 | ||
| Parratte and Argenson, n = 60 | 17/30 (57%) | 6/30 (20%) | 34.0 (7.62) | 34.0 (5.7) | 16.2 (9.6) | 14.4 (4.5) |
Figure 2 shows a funnel plot for these studies, reporting acetabular outliers from the accepted range of alignment. The studies are distributed within the 95% confidence interval axis.
Fig. 2.
Funnel plot calculation demonstrating no evidence of publication bias
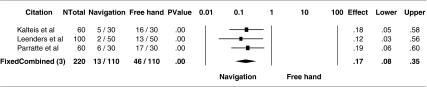
The number of acetabular outliers in the navigation group was 15/140 (10.7%), compared to 46/110 (41.8%) in the freehand group. The statistically significant beneficial odds ratio for the number of outliers was 0.285 (95% CI: 0.143 to 0.569; p < 0.001). There was no evidence of statistical heterogeneity between studies (p = 0.88; Fig. 3).
Fig. 3.
Odds ratio for outliers from the accepted range comparing the navigation and control groups
Two studies commented on complications [7, 13], while one study did not [9]. Overall, there were no reported complications in the navigation group and one dislocation in the freehand group (1.3%). Two studies [7, 13] commented on an increased surgical time for computer navigation, ranging from 8 to 17 min.
Discussion
The results of our study show that computer navigation significantly improved the surgeon’s ability to place the acetabular cup within the desired alignment as defined by Lewinnek et al. [10]. It is unclear at present whether this improved surgical precision will translate to improved long-term clinical outcomes.
A further important finding of our study is that, despite computer navigation becoming an increasingly popular tool amongst surgeons, there are only three randomised trials documenting its efficacy, and all with small numbers.
The cost issues surrounding computer navigation in THR have not been well explored. Whether these systems prove to be cost-effective in the long-term by reducing the revision burden remains to be seen.
Our meta-analysis has several potential limitations. From an internal validity point of view, the interventions were not consistent throughout the studies. One study compared freehand technique to a CT-based system, one compared freehand technique with an imageless system and the final study compared all three methods. Patients undergoing CT-based and imageless navigation were combined into one navigation group in our analysis. We feel that this is justified because CT-based navigation and imageless navigation were compared in a randomised trial and were found to have no significant differences in any outcome measures (p = 0.23) [13]. Moreover, although we didn’t find any evidence of publication bias, funnel plots have limited power in detecting bias if the number of studies is small. From an external validity point of view, one study [13] excluded those patients weighing greater than 100 kg, and this may limit the generalisation of their findings to the more obese patients.
In conclusion, our meta-analysis shows that computer navigation decreased the number of acetabular cups implanted outside the desired range of alignment. At present, there is a need for a well-designed RCT to report on both clinical and radiographic outcome parameters, complications and survival rates, quality of life years gained and cost analyses.
References
- 1.Schutte H, Jr, Lipman AJ, Bannar SM, Livermore JT, Ilstrup D, Morrey BF. Effects of acetabular abduction on cup wear rates in total hip arthroplasty. J Arthroplasty. 1998;13:621–626. doi: 10.1016/S0883-5403(98)80003-X. [DOI] [PubMed] [Google Scholar]
- 2.DiGioia AM, Jaramaz B, Plakseychuk AY, Moody JE, Jr., Nikou C, Labarca RS, Levison TJ, Picard F. Comparison of a mechanical acetabular alignment guide with computer placement of the socket. J Arthroplasty. 2002;17:359–364. doi: 10.1054/arth.2002.30411. [DOI] [PubMed] [Google Scholar]
- 3.DiGioia AM, Plakseychuk AY, Levison TJ, Jaramaz B. Mini-incision technique for total hip arthroplasty with navigation. J Arthroplasty. 2003;18:123–128. doi: 10.1054/arth.2003.50025. [DOI] [PubMed] [Google Scholar]
- 4.Egger M, Davey Smith G, Schneider M, Minder C. Bias in meta-analysis detected by a simple, graphical test. BMJ. 1997;315:629–634. doi: 10.1136/bmj.315.7109.629. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Haaker RG, Tiedjen K, Ottersbach A, Rubenthaler F, Stockheim M, Stiehl JB. Comparison of conventional versus computer-navigated acetabular component insertion. J Arthroplasty. 2007;22:151–159. doi: 10.1016/j.arth.2005.10.018. [DOI] [PubMed] [Google Scholar]
- 6.Jolles BM, Genoud P, Hoffmeyer P. Computer-assisted cup placement techniques in total hip arthroplasty improve accuracy of placement. Clin Orthop Relat Res. 2004;426:174–179. doi: 10.1097/01.blo.0000141903.08075.83. [DOI] [PubMed] [Google Scholar]
- 7.Kalteis T, Handel M, Bäthis H, Perlick L, Tingart M, Grifka J. Imageless navigation for insertion of the acetabular component in total hip arthroplasty: is it as accurate as CT-based navigation? J Bone Joint Surg Br. 2006;88(2):163–167. doi: 10.1302/0301-620X.88B2.17163. [DOI] [PubMed] [Google Scholar]
- 8.Kennedy JG, Rogers WB, Soffe KE, Sullivan RJ, Griffen DG, Sheehan LJ. Effect of acetabular component orientation on recurrent dislocation, pelvic osteolysis, polyethylene wear, and component migration. J Arthroplasty. 1998;13:530–534. doi: 10.1016/S0883-5403(98)90052-3. [DOI] [PubMed] [Google Scholar]
- 9.Leenders T, Vandevelde D, Mahieu G, Nuyts R. Reduction in variability of acetabular cup abduction using computer assisted surgery: a prospective and randomized study. Comput Aided Surg. 2002;7:99–106. doi: 10.3109/10929080209146021. [DOI] [PubMed] [Google Scholar]
- 10.Lewinnek GE, Lewis JL, Tarr R, Compere CL, Zimmerman JR. Dislocations after total hip-replacement arthroplasties. J Bone Joint Surg Am. 1978;60:217–220. [PubMed] [Google Scholar]
- 11.Moher D, Cook DJ, Eastwood S, Olkin I, Rennie D, Stroup DF. Improving the quality of reports of meta-analyses of randomised controlled trials: the QUOROM statement. Quality of Reporting of Meta-analyses. Lancet. 1999;354:1896–1900. doi: 10.1016/S0140-6736(99)04149-5. [DOI] [PubMed] [Google Scholar]
- 12.Murphy SB, Ecker TM, Tannast M. THA performed using conventional and navigated tissue-preserving techniques. Clin Orthop Relat Res. 2006;453:160–167. doi: 10.1097/01.blo.0000246539.57198.29. [DOI] [PubMed] [Google Scholar]
- 13.Parratte S, Argenson JN. Validation and usefulness of a computer-assisted cup-positioning system in total hip arthroplasty. A prospective, randomized, controlled study. J Bone Joint Surg Am. 2007;89:494–499. doi: 10.2106/JBJS.F.00529. [DOI] [PubMed] [Google Scholar]
- 14.Paterno SA, Lachiewicz PF, Kelley SS. The influence of patient-related factors and the position of the acetabular component on the rate of dislocation after total hip replacement. J Bone Joint Surg Am. 1997;79:1202–1210. doi: 10.2106/00004623-199708000-00013. [DOI] [PubMed] [Google Scholar]
- 15.Sugano N, Nishii T, Miki H, Yoshikawa H, Sato Y, Tamura S. Mid-term results of cementless total hip replacement using a ceramic-on-ceramic bearing with and without computer navigation. J Bone Joint Surg Br. 2007;89(4):455–460. doi: 10.1302/0301-620X.89B4.18458. [DOI] [PubMed] [Google Scholar]
- 16.Weil Y, Mattan Y, Kandel L, Eisenberg O, Liebergall M. Navigation-assisted minimally invasive two-incision total hip arthoplasty. Orthopedics. 2006;29(3):200–206. doi: 10.3928/01477447-20060301-10. [DOI] [PubMed] [Google Scholar]
- 17.Wixson RL, MacDonald MA. Total hip arthroplasty through a minimal posterior approach using imageless computer-assisted hip navigation. J Arthroplasty. 2005;20(7 Suppl 3):51–56. doi: 10.1016/j.arth.2005.04.024. [DOI] [PubMed] [Google Scholar]