Abstract
The objective was to evaluate the efficacy of xenografts to improve the outcomes in elderly patients with tibial plateau fractures. Nineteen cases with a mean age of 74 years were followed prospectively from 1998 to 2003. Six patients each belonged to Schatzker types III, IV and V and one patient belonged to type II. Open reduction with fixation and xenograft impaction was carried out. Clinical and radiological union was assessed including infection rate, incorporation of the xenograft and average collapse of the fracture. The average union time was 20 weeks. No patient had wound infection and all had excellent incorporation of the xenograft with union. The average collapse was 4 mm on follow-up. This series shows the use of only an xenograft in acute fixation of these fractures with favourable outcome. Furthermore, it reduces operative time, bleeding and associated co-morbidities, which is of more significance in an elderly age group.
Résumé
évaluer l’efficacité des xénogreffes chez les patients âgés dans le cadre des fractures du plateau tibial. 19 cas, d’âge moyen de 74 ans ont été suivis et traités de façon prospective de 1998 à 2003. 6 patients présentaient des fractures de type Schatzker III, IV, V et 1 patient présentait une fracture de type II. Le traitement chirurgical a consisté en une réduction par voie sanglante avec fixation et utilisation d’une xénogreffe impactée. L’évaluation a été clinique et radiologique avec notamment, évaluation du taux d’infection et du taux d’incorporation de la xénogreffe ainsi que du pourcentage du collapsus fracturaire. le temps moyen de consolidation a été de 20 semaines. Aucun patient ne présentait d’infections profondes. Tous ont eu une excellente incorporation de la xénogreffe. Le pourcentage moyen de tassement a été de 4 mm. En conclusion cette série montre que l’on peut utiliser des xénogreffes dans le traitement de ces fractures avec une bonne évolution. Ce traitement permet de diminuer le temps opératoire, le saignement et les comorbidités qui sont particulièrement significatives chez les patients âgés.
Introduction
Management of tibial plateau fractures in elderly patients remains controversial. An unsatisfactory outcome is associated with comminuted fractures. Underlying osteoporosis does not allow rigid fixation resulting in early failure of fixation. Bone grafting may become necessary along with rigid fixation; however, obtaining adequate quantity of graft can, not only be difficult but may compound the problems further by adding the stress of an additional procedure in already debilitated patients.
Available literature on the outcome of tibial plateau fractures in the elderly is limited [2, 6, 11]. Such patients are managed either non-operatively or eliminated from the series describing operative management of such injuries as strict indications for open reduction and internal fixation do not apply in this group, in contrast to young patients. These fractures do seem to be relatively common injuries in the elderly population as 55–70% of the patients in some of the series have been over the age of 50 years [9, 17]. The outcome reported varies in different series; 70–80% good to excellent results were reported in some series [10, 14], whereas studies based on patient self-assessment and functional outcome described unsatisfactory outcome depicting poor bone quality, failure of fixation, pre-existing degenerative disease and medical co-morbidities as responsible factors [19, 21].
The goals of treatment are restoration of knee mobility, return to pre-injury level of function and prevention of degenerative changes. The spectrum of treatment ranges from cast bracing, external fixator, pre-contoured periarticular plating to primary total knee replacement in combination with structural bone grafting or similar substitutes. Procurement of bone graft is likely to enhance the operative time, blood loss and other related morbidities. Use of femoral head allografts [13] as well as allogenic, frozen, radio-sterilised, spongy bone grafts [23] for the treatment of proximal tibial fractures has been successfully reported in the literature. Allografts or bone substitutes carry the risk of infection and failure to incorporate with the host bone [3]. There is however limited information on the use of xenografts [15]. With the introduction of bovine, solvent-preserved cancellous bone blocks (Tutoplast bovine cancellous bone block, Tutogen, Erlangen, Germany) a European Community-certified bone material is commercially available in standardised sizes. In vitro tests showed a high biomechanical resistance to axial loads, and osseointegration was observed in an animal model [7].
This study includes 19 patients at an average age of 74 years with proximal tibial fractures treated using plate or cancellous screw only fixation combined with solvent-preserved gamma-sterilised bovine cancellous bone for filling the defect. Long-term results with regards to infection rate, fracture union, graft incorporation and complications are reported. The study is aimed at evaluating efficacy of xenograft substitutes to improve the outcomes in the reported age range (more than 65), which has been shown to be associated with poorer outcomes [19, 21].
Material and method
A total of 19 patients (9 male and 10 female) at an average age of 74 years (63–86) who underwent operative management of tibial plateau fractures were the subjects of the study. Patients were recruited from 1998 to 2003. The senior author operated all patients. Inclusion criteria included following:
Age at the time of operation (60 years or more)
Articular displacement of 4 mm or more
Varus/valgus instability equivalent to 10° or more
Condylar widening of 5 mm or more
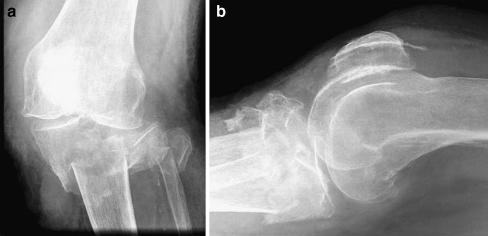
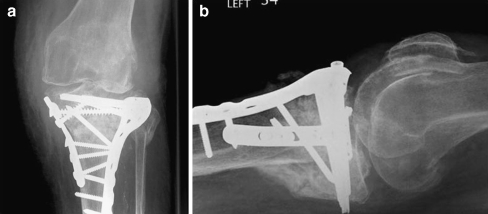
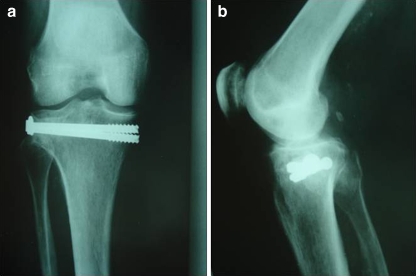
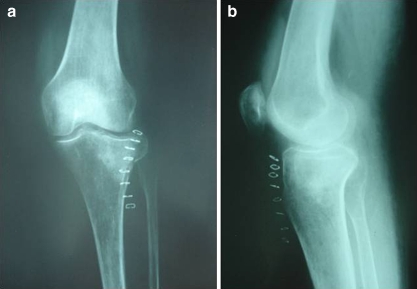
Patients were excluded from the study if they had open fractures or associated diaphyseal or distal tibial fractures. Details relating to mechanism of injury, associated injuries, injury operation interval, associated medical co-morbidities, previous operations, American Society of Anesthesiologists (ASA) grade, residential status, pre-injury mobility level, fracture configuration (Schatzker classification, Fig. 1), type of surgery, hospital stay, complications, re-operations, functional and radiological outcomes were entered in a prospectively maintained database. The surgical technique involved a midline or medial/lateral parapatellar approaches under tourniquet control to achieve exposure. The standard steps in the surgical procedure included adequate exposure, anatomical reduction, restoration of articular surface congruity, filling of the defect with xenograft and fixation with single/dual buttress plating (Fig. 2a,b) or cannulated screw fixation (Fig. 3a,b). In one patient with Schatzker type II fracture, elevation of the depressed fragment was done with filling of the defect with xenograft without any fixation (Fig. 4a,b). Bovine cancellous xenogenous bone granules (Tutoplast) were used as bone graft substitute. The Tutoplast processing of the graft is comprehensive and includes several steps such as delipidisation, hyperosmotic saline bath, oxidative treatment, acetone wash and low-dose gamma irradiation. The post-operative protocol included continuous passive motion on the second day followed by non-weight-bearing mobilisation in a cast brace for a period of 6 weeks. Full weight bearing was commenced 12 weeks post-operatively. The follow-up at 1.5, 3, 6 and 12 months comprised clinical review to assess pain, walking distance, range of movement and stability. Information relating to fracture healing, incorporation of the xenograft and further collapse at the fracture site was entered into the database. Outcome was reported as excellent if patients had stable, painless knees with at least 90° of range of motion and radiological evidence of union and incorporation of the graft.
Fig. 1.
a, b Schatzker type V fracture in patient A
Fig. 2.
a, b Patient A at final follow-up
Fig. 3.
a, b Schatzker type III fracture treated with open reduction and cannulated screw fixation in patient B
Fig. 4.
a, b Elevation with bone grafting with xenograft for Schatzker type II fracture
Results
There were 19 patients, 9 male and 10 female, at an average age of 74 years (63–93). Seventeen patients were alive at the time of writing the paper. Mechanisms of injury included history of fall (low energy) with direct trauma to the proximal tibia in 17 patients and high-energy trauma (vehicle accident) in 2 patients. All patients had unilateral involvement with the right knee being involved in 12 patients and the left knee in 7 patients. Six patients each belonged to Schatzker types II, IV and V and one patient belonged to Schatzker type II. None of the patients had compartment syndrome or neurovascular compromise. The average injury-operation interval was 32 hours (16–72). A midline skin incision was used in 8 patients and parapatellar incisions were used in 11 patients. All patients had open reduction and internal fixation using single or dual buttress plating (13 patients) (Fig. 2a,b) or cancellous screw fixation only (5 patients) (Fig. 3a,b) except in a patient with type II fracture in whom the fracture was elevated and defect filled with xenograft without any additional fixation (Fig. 4a,b). After direct visualisation of the tibial articular surface, menisci and anterior cruciate ligament (ACL) were assessed. The ACL was intact in all of the cases; however, three cases were found to have a medial meniscus tear and one case had a tear of the lateral meniscus. The average operative time was 64 minutes. All patients received a dose of pre-operative and three doses of post-operative antibiotics. Table 1 contains information relating to patient demographics, co-morbidities, ASA grade, injury pattern, associated injuries and details of operation.
Table 1.
Patient characteristics. HT hypertension, DM diabetes mellitus, BA bronchial asthma, MI myocardial infarction, CCF congestive cardiac failure, CKD chronic kidney disease, ASA American Society of Anesthesiologists, CCS cannulated cancellous screws, OR + P1 open reduction and single plating, OR + P2 open reduction and dual plating, EL extension lag
| No. | Age | Sex | Co-morbidities | ASA grade | Schatzker type | Implants for fixation | Associated fracture | Time to union (weeks) | Range of movement | Complications |
|---|---|---|---|---|---|---|---|---|---|---|
| 1 | 82 | F | HT, DM | 2 | II | None | None | 16 | 0–100 | |
| 2 | 76 | M | BA | 1 | IV | CR + CCS | None | 20 | 0–90 | |
| 3 | 86 | F | HT | 1 | III | OR + P1 | Distal radius | 19 | 0–85 | |
| 4 | 85 | M | MI, HT, CKD | 3 | III | CR + CCS | None | 21 | 0–90 | |
| 5 | 80 | F | DM | 2 | IV | OR + P1 | Humerus | 24 | 5–85 | |
| 6 | 64 | M | HT | 1 | V | OR + P2 | None | 17 | 10–90 | Lag |
| 7 | 68 | M | - | 1 | V | OR + P2 | None | 18 | 20–80 | Stiffness, EL |
| 8 | 72 | M | BA | 2 | IV | OR + P1 | None | 21 | 5–90 | |
| 9 | 80 | F | CCF | 3 | III | CR + CCS | Distal radius | 22 | 0–90 | |
| 10 | 77 | F | HT | 1 | IV | OR + P1 | Pubic rami | 20 | 0–85 | |
| 11 | 64 | M | DM | 1 | V | OR + P2 | None | 23 | 15–80 | Stiffness, EL |
| 12 | 78 | M | HT, BA | 2 | III | OR + P1 | None | 17 | 0–90 | |
| 13 | 67 | F | DM | 2 | IV | CR + CCS | None | 19 | 0–100 | |
| 14 | 65 | M | HT | 1 | V | OR + P2 | None | 22 | 10–90 | |
| 15 | 63 | F | DM, BA | 2 | III | OR + P1 | None | 17 | 5–90 | |
| 16 | 70 | F | CCF, CKD | 3 | III | CR + CCS | Distal radius | 23 | 0–95 | |
| 17 | 71 | M | MI | 2 | IV | OR + P1 | None | 21 | 0–90 | |
| 18 | 69 | F | HT | 1 | V | OR + P2 | None | 22 | 10–90 | EL |
| 19 | 71 | F | BA | 2 | V | OR + P2 | None | 20 | 5–85 | Stiffness |
All of the cases were followed for a mean of 1 year (8–14 months). The average time for fracture union was 20 weeks (16–24 weeks). The average range of movement (ROM) at the time of final follow-up was 90°. Two cases were noted to have significant stiffness and restricted ROM and extension lag of 20°. None of the cases were noted to have instability.
Radiological follow-up included measuring change in the grading of osteoarthritis based on the comparison of the pre-operative roentgenograms to those at final follow-up. Average bony collapse was measured to 4 mm. All patients had good clinical and radiological outcome.
Discussion
Comminuted fractures of the tibial plateau pose a difficult treatment issue, which has not been adequately dealt with in the literature. The data based on the outcome of operative treatment of such injuries in young patients cannot be used to make treatment decisions for the elderly population. The pattern of fracture and associated injuries differ in the elderly population. Schatzker types III, IV and V were the main fracture patterns found along with lower incidence of concomitant ligament or meniscal injuries [2, 5]. This can be attributed to lower energy injury and osteoporotic bone, which breaks before the ligaments fail.
The non-operative treatment options include skin or skeletal traction, serial X-rays and immobilisation in a cast brace. This option did not seem viable for our patients, as most patients had displaced comminuted higher-grade Schatzker type fractures. Non-operative management further prolongs the hospital stay leading to subsequent problems like deep venous thrombosis (DVT), pulmonary embolism (PE), higher incidence of hospital-acquired infections, ulcers, etc. In the long run patients run the risk of developing stiffness, rapid progression of arthritis and varus or valgus malalignment. Several studies reported poorer outcome following non-operative management [18].
The technical challenges that make one hesitant to pursue surgical options include:
The high risk of complications following open reduction and dual plating in patients with fragile skin and an already compromised soft tissue envelope
Difficulty in achieving stable rigid fixation due to osteoporosis
Complex fracture configuration with sagittal and coronal plane fracture lines making reconstruction more difficult [16]
Co-existing medical co-morbidities
Pre-existing degenerative changes
Problems of procuring autogenous bone graft and related donor site morbidity to fill the defect resulting after restoration of the articular surface
Several different surgical strategies have been reported for the treatment of tibial plateau fractures. Each of the surgical modalities has merits and demerits. Following poor outcomes of non-operative management less invasive techniques were introduced in the 1980s and 1990s to minimize soft tissue complications. Satisfactory outcomes have been reported with less invasive techniques for lower energy injuries including unicondylar and minimally displaced fractures [4, 12]; however, this technique does not provide adequate fixation in cases of bicondylar or comminuted fractures. Hybrid fixation including combination of lateral internal fixation and medial monolateral external fixation is useful in patients with good bone quality and less comminuted fractures. External fixation systems using beam-loading mechanisms like the Sheffield ring fixator have been reported for patients older than 60 years. This was associated with a higher rate of pin tract infections and valgus malunion requiring further operations [1]. Extension of unicondylar or total knee replacement as a treatment for patients with osteopenic bone and pre-existing arthritis will necessitate the use of modular or custom-made prosthesis and wedges, augmentations, bone graft or substitutes to fill the defect [22]. Though this may be a viable option in some cases, there is clearly lack of evidence with regards to its use in fit and active elderly patients with no pre-existing arthritis and comparison with existing techniques. Open reduction and plating still remains the treatment of choice in most centres as it allows direct control of reduction, anatomical alignment and ability to reconstruct the plateau by filling the gap with bone graft or alternatives. Locked periarticular plating systems with multi-angle screw fixation, combined with bone grafting or equivalent substitutes, help improve the holding strength of the implant.
A wide variety of bone graft substitutes are available. Kwiatkowski et al. successfully reported use of frozen allogenic spongy bone graft for proximal tibial fractures [13]. Villas et al. reported use of femoral head allografts without any complications [23]. Segur et al. reported use of allografts in conjunction with internal fixation and reported 100% incorporation [20]. The limitations of allograft include potential risk of disease transmission in spite of stringent donor selection and screening. The demand for allografts has been rising fast because of the usefulness in revision arthroplasty and spine surgery; however, femoral heads of living donors remain the only source. As the search for newer and better materials continues, the authors successfully report use of xenografts in their series of tibial plateau fractures.
Several other studies have reported their functional results using Rasmussen criteria [20]. Though our study did not include any scoring system, all criteria except quadriceps power in Rasmussen’s system were included to report outcome as either good or poor.
There is no risk of transmission of infection by the material, due to the sterilisation procedures performed [8]. Animal studies showed a proper osteointegration of the material [7], which was not reproduced in the series by Schultheiss et al. where they reported delayed incorporation of bovine cancellous blocks to that of autogenous tricortical iliac crest bone grafts for reconstruction of thoracolumbar fractures [15]. One of the reasons could be that to overcome the antigenicity of xenogenous tissues, the grafts are submitted to a chemical process that ensures their biotolerance, but also reduces their osteoinductive potential. We noticed 95% incorporation at an average of 5 months for tibial plateau fractures.
Cancellous bone autograft remains the optimum standard to which other bone substitutes must be compared. We accept this as one of the limitations as there is no comparison of xenogenous to autogenous tissue in our series. We believe that the xenogenous tissue holds sufficient osteoconductive potential to act as a scaffold in support of the subchondral bone of the tibial articular surface. Cancellous chips or powder, which were used in the study, are incorporated solely by enchondral bone formation along the osteoconductive framework of the graft, which strengthens the reconstruction over time subject to compressive forces with weight bearing in tibial plateau fractures.
The importance of preparation of a bleeding host bed and stable host graft interface to achieve incorporation cannot be underestimated. This along with a meticulous surgical technique and adequate graft material to prevent post-operative collapse ensures better outcome.
References
- 1.Ali AM, Burton M, Hashmi M, Saleh M. Treatment of displaced bicondylar tibial plateau fractures (OTA-41C2&3) in patients older than 60 years of age. J Orthop Trauma. 2003;17(5):346–352. doi: 10.1097/00005131-200305000-00005. [DOI] [PubMed] [Google Scholar]
- 2.Biyani A, Reddy NS, Chaudhury J, Simison AJ, Klenerman L. The results of surgical management of displaced tibial plateau fractures in the elderly. Injury. 1995;26(5):291–297. doi: 10.1016/0020-1383(95)00027-7. [DOI] [PubMed] [Google Scholar]
- 3.Caldwell PE, Shelton WR. Indications for allografts. Orthop Clin North Am. 2005;36(4):459–467. doi: 10.1016/j.ocl.2005.05.008. [DOI] [PubMed] [Google Scholar]
- 4.Duwelius PJ, Rangitsch MR, Colville MR, Woll TS. Treatment of tibial plateau fractures by limited internal fixation. Clin Orthop. 1997;339:47–57. doi: 10.1097/00003086-199706000-00007. [DOI] [PubMed] [Google Scholar]
- 5.Su EP, Westrodge GH, Rana AJ, Kapoor K, Helfet DL. Operative treatment of tibial plateau fractures in patients older than 55 years. Clin Orthop Relat Res. 2004;421:240–248. doi: 10.1097/01.blo.0000119247.60317.bc. [DOI] [PubMed] [Google Scholar]
- 6.Foltin E. Osteoporosis and fracture patterns: a study of split-compression fractures of the lateral tibial condyle. Int Orthop. 1998;12(4):299–303. doi: 10.1007/BF00317828. [DOI] [PubMed] [Google Scholar]
- 7.Günther KP, Scharf HP, Pesch HJ, Puhl W. Integration properties of bone substitute materials. Experimental studies on animals. Orthopade. 1996;27(2):105–117. doi: 10.1007/s001320050208. [DOI] [PubMed] [Google Scholar]
- 8.Hofmann A, Hofmann C, Gotzen L. Effect of various bone disinfection and sterilization methods on osteoblast function. A comparative in vitro study. Unfallchirurg. 2000;103(5):380–388. doi: 10.1007/s001130050554. [DOI] [PubMed] [Google Scholar]
- 9.Hohl M, Luck JV. Fractures of the tibial condyle: a clinical and experimental study. J Bone Joint Surg Am. 1956;38-A(5):1001–1018. [PubMed] [Google Scholar]
- 10.Hsu CJ, Chang WN, Wong CY. Surgical treatment of tibial plateau fracture in elderly patients. Arch Orthop Trauma Surg. 2001;121(1–2):67–70. doi: 10.1007/s004020000145. [DOI] [PubMed] [Google Scholar]
- 11.Keating JF. Tibial plateau fractures in the older patient. Bull Hosp Jt Dis. 1999;58(1):19–23. [PubMed] [Google Scholar]
- 12.Koval KJ, Sanders R, Borrelli J, Helfet D, DiPasquale T, Mast JW. Indirect reduction and percutaneous screw fixation of displaced tibial plateau fractures. J Orthop Trauma. 1992;6(3):340–346. doi: 10.1097/00005131-199209000-00012. [DOI] [PubMed] [Google Scholar]
- 13.Kwiatkowski K, Cejmer W, Sowiski T. Frozen allogenic spongy bone grafts in filling the defects caused by fractures of proximal tibia. Ann Transplant. 1999;4(3–4):49–51. [PubMed] [Google Scholar]
- 14.Levy O, Salai M, Ganel A, Mazor J, Oran A, Horoszowski H. The operative results of tibial plateau fractures in older patients: a long-term follow-up and review. Bull Hosp Jt Dis. 1993;53(1):15–16. [PubMed] [Google Scholar]
- 15.Schultheiss M, Sarkar M, Arand M, Kramer M, Wilke HJ, Kinzl H, Hartwig E. Solvent-preserved, bovine cancellous bone blocks used for reconstruction of thoracolumbar fractures in minimally invasive spinal surgery–first clinical results. Eur Spine J. 2005;14(2):192–196. doi: 10.1007/s00586-004-0764-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Moore TM, Patzakis MJ, Harvey JP. Tibial plateau fractures: definition, demographics, treatment rationale, and long-term results of closed traction management or operative reduction. J Orthop Trauma. 1987;1(2):97–119. doi: 10.1097/00005131-198702010-00001. [DOI] [PubMed] [Google Scholar]
- 17.Rasmussen PS. Tibial condylar fractures. Impairment of knee joint stability as an indication for surgical treatment. J Bone Joint Surg Am. 1973;55(7):1331–1350. [PubMed] [Google Scholar]
- 18.Schatzker J, McBroom R, Bruce D. The tibial plateau fracture: the Toronto experience 1968–1975. Clin Orthop. 1979;138:94–104. [PubMed] [Google Scholar]
- 19.Schwartsman R, Brinker MR, Beaver R, Cox DD. Patient self-assessment of tibial plateau fractures in 40 older adults. Am J Orthop. 1998;27(7):512–519. [PubMed] [Google Scholar]
- 20.Segur JM, Torner P, Garcia S, Combalia A, Suso S, Ramon R. Use of bone allograft in tibial plateau fractures. Arch Orthop Trauma Surg. 1998;117(6–7):357–359. doi: 10.1007/s004020050265. [DOI] [PubMed] [Google Scholar]
- 21.Stevens DG, Beharry R, McKee MD, Waddell JP, Schemitsch EH. The long-term functional outcome of operatively treated tibial plateau fractures. J Orthop Trauma. 2001;15(5):312–320. doi: 10.1097/00005131-200106000-00002. [DOI] [PubMed] [Google Scholar]
- 22.Nau T, Pflegerl E, Erhart J, Vecsei V. Primary total knee arthroplasty for periarticular fractures. J Arthroplasty. 2003;18(8):968–971. doi: 10.1016/S0883-5403(03)00280-8. [DOI] [PubMed] [Google Scholar]
- 23.Villas C, Mora G, Arriola FJ. Use of bone allografts in the surgical repair of tibial plateau fractures (in Spanish) Rev Med Univ Navarra. 1996;40(3):13–18. [PubMed] [Google Scholar]