Abstract
To determine trends in characteristics of total hip arthroplasty (THA) in the United States, the National Hospital Discharge Survey (NHDS) was analyzed from 1990 to 2004 for trends in in-hospital mortality and complications, length of hospital stay, demographics, and comorbidities. The number of THAs performed increased by 158%, whereas mortality rates remained low and slightly decreased (from 0.32% to 0.29%). Prevalence of procedure-related complications decreased over time, and length of stay decreased from an average of 8.7 days to 4.5 days. These improvements occurred despite an increase in comorbidities in patients. An increase in both the proportion of discharges to long- and short-term care facilities and in the proportion of procedures performed in smaller hospitals was noted. Multiple temporal changes in outcomes and demographics for THA were found. These changes have implications for clinical care and allocation of health resources.
Résumé
Le but de ce travail est de mettre en évidence les nouvelles données caractéristiques des prothèses totales de hanche aux Etats-Unis. Matériel et méthode: Le National Hospital Discharge Survey (NHDS) a été analysé durant la période de 1990 à 2004 sur le plan de la mortalité, des complications, de la durée de séjour, sur le plan démographique et des comorbidités. Résultat: le nombre de prothèses totales de hanche a augmenté de 158% dans cette période alors que la mortalité reste basse et a même légèrement diminué (0,32% à 0,29%). Le taux de complications et la durée moyenne de séjour diminuent également avec le temps de 8,7 jours à 4,5 jours. Ces améliorations entraînent néanmoins une augmentation des comorbidités chez les patients. Il a été noté une augmentation de la proportion des sorties avec prise en charge des soins de courte ou longue durée et une proportion importante de procédures réalisées dans les petits hôpitaux. les modifications notées sur le devenir et sur les bases démographiques des prothèses totales de hanche, ont une implication clinique sur les soins et sur l’allocation de ressource.
Introduction
Since its introduction in the 1960s, total hip arthroplasty (THA) has become the standard treatment for patients with end stage osteoarthritis. Multiple studies have documented significant quantitative and qualitative improvement in physical function and health related quality of life after THA [1]. It has also been suggested that patients who undergo THA may have increased lifespan compared to those who defer the procedure [2]. Current surveys from the United States and Europe report continued growth in the use of THAs from the 1990s to early 2000 [11, 13, 17]. Current projections for the United States suggest that from 2005 to 2030 the number of THAs will increase by 174% to nearly 600,000 procedures per year [14]. This increase has been accompanied by changes in demographics of patients over the past several decades [7]. However, there are few comprehensive descriptive analyses on nationally representative trends in patient demographics, comorbidity profiles, and in-hospital outcomes such as length of stay, complication rates, and mortality after THA. Examining such information is of importance to all medical and administrative professionals involved in patient care. For example, changes in patient demographics may direct research into new surgical techniques or implant devices that are optimized for subsets of patients. Changes in comorbidity profiles may direct allocation of resources for preoperative testing and perioperative consultations from anesthesiologists, cardiologists, and diabetes specialists. Finally, changes in in-hospital outcomes may direct research and design into perioperative processes to optimize patient care by reducing errors or increasing efficiency from clinical pathways.
Therefore, we analyzed nationally representative data, collected through the National Hospital Discharge Survey (NHDS) from 1990 to 2004, to elucidate changes in the mortality, in in-hospital mortality and complications, length of hospital stay, and demographics (including comorbidity profiles) of patients undergoing primary total hip arthroplasty in the United States over a 15-year study period.
Materials and methods
The National Hospital Discharge Survey (NHDS)
NHDS multi-year data files were obtained from the Centers for Disease Control and Prevention, Atlanta, GA. The plan and operation of the NHDS has been published in detail [8]. In summary, the NHDS includes medical information collected annually since 1965 by the National Center for Health Statistics with the purpose to compile nationally representative data on inpatient use of short-stay hospitals. The hospital universe includes Medicare participating, noninstitutional hospitals of various sizes, exclusive of military, Veterans Affairs, and federal facilities in the 50 states and the District of Columbia. Hospitals included in the survey are required to have an average length of stay of less than 30 days to be considered short-stay, or to be a general medical or surgical hospital, regardless of length of stay. Facilities are also required to have at least six beds for patient use. Periodic updates of the hospital universe are performed to account for changes. To ensure accurate, nationally representative sampling, the NHDS uses a complex three-stage probability design. Information collected in the survey includes diagnosis and procedure codes (ICD-9-CM), age, sex, race, principal expected source of payment (insurance status), length of care, hospital size, United States region, and patient discharge status. Weighted data, with weights derived from census data by the NHDS, were provided to generate unbiased national estimates from the sample (1% of all hospital discharges in the United States). Multiple steps to ensure validity and accuracy of coding and data entry in the NHDS have been previously described [8]. These quality control measures include independent coding of a 5% sample by two different coders with differences adjudicated by a chief coder. Batches of samples with an error rate of more than 5% for medical data and 1% for nonmedical entries are rejected and recoded. In addition, all records are checked for invalid and missing variables, inaccuracies, and outliers, and a detailed review is conducted for most variables for each hospital. The NHDS has been used extensively in the past to analyze temporal trends associated with a wide range of procedures across a variety of medical specialties [5]. Thus, we collected data from the NHDS including diagnosis and procedure codes (ICD-9-CM), patient and hospital demographics, length of stay, discharge disposition, and source of payment. Weighted data (derived from census data by the NHDS) were generated to create national estimates from the sample.
Patient selection and analysis
Data collected for each year between 1990 and 2004 were obtained, read into a statistical software program (SAS version 8.2, SAS Institute, Cary, NC), and analyzed. Discharges with at least one procedure code (ICD-9-CM) for primary THA (81.51) were included in the sample. To simplify analysis of temporal changes in THAs, three 5-year periods were created (1990–1994, 1995–1999, 2000–2004). Changes in the prevalence of procedures and trends in age, gender, race, disposition status, distribution of procedures by hospital size, and US region as well as length of care were evaluated across time periods. Frequencies of procedure-related complications over time were analyzed by determining cases that listed ICD-9-CM diagnosis codes specifying complications of surgical and medical care (ICD-9-CM 996 to 999) as described previously [21]. In addition, we studied the prevalence of selected adverse diagnoses, including pulmonary embolism, thrombotic events, respiratory insufficiency after trauma or surgery/acute respiratory distress syndrome, acute posthemorrhagic anemia, and psychosis using appropriate ICD-9 diagnosis codes. Trends in comorbidity profiles were analyzed by determining the prevalence of hypertension, diabetes mellitus, obesity, pulmonary, coronary artery, peripheral vascular, and renal disease, as well as disorders in lipid metabolism [21]. ICD-9 diagnosis codes included to determine the presence of comorbidities and adverse diagnosis are listed in Table 4 in the Appendix. Changes in in-hospital mortality between time periods were also assessed.
Table 4.
List of ICD-9 diagnosis codes included to identify comorbidities, adverse diagnosis, and complications among discharges (four- and five-digit codes are included under the respective three- and four-digit codes)
| Comorbidities | |
|---|---|
| Hypertension | 401, 402, 403, 404, 405 |
| Diabetes mellitus | 250 |
| Hypercholesteremia | 2720 |
| Obesity | 278 |
| Cerebrovascular disease | 433, 434, 437, 438 |
| Thromboembolic events | 4511, 4512, 4518, 4519, 4532, 4538, 4539 |
| PVD/atherosclerosis | 440, 4439 |
| Pulmonary disease | 490, 491, 492, 493, 494, 496 |
| Renal disease | 582, 585, 403 |
| Coronary artery disease | 412, 413, 414, 4292 |
| Procedure related complications | |
| Device related complications | 996 |
| Central nervous system | 9970 |
| Cardiac | 9971 |
| Peripheral vascular | 9972 |
| Respiratory | 9973 |
| Gastrointestinal | 9974 |
| Genitourinary | 9975 |
| Other organ specific | 9976–9979 |
| Postoperative shock | 9980 |
| Hematoma/seroma | 9981 |
| Accidental puncture/laceration | 9982 |
| Disruption operative wound | 9983 |
| Postoperative infection | 9985 |
| Other complications of procedure | 9986 – 9989 |
| Complications of medical care | 999 |
| Other adverse events | |
| Acute posthemorrhagic anemia | 2851 |
| Pulmonary embolism | 4151 |
| Psychosis | 291, 292, 293 |
| Pulmonary insufficiency after | 5185 |
| Trauma and surgery/acute respiratory | |
| distress syndrome | |
Intercensal population estimates determined by the United States Census Bureau and provided by the Centers for Disease Control and Health Services in companion data files were used to calculate prevalence of procedures in each 5-year period per 100,000 subjects both unadjusted and then adjusted for demographics of interest (age, gender, etc.). For the purpose of this analysis, the mean incidence determined for variables in our study was compared to the mean population estimate for a given 5-year study period.
Statistical methods
Significance of changes over time was assessed first using chi-square tests and then using Z-scores for categorical variables where appropriate. Significance of differences between time periods for continuous variables was evaluated using a general linear model. A p value of 0.001 was used to define significance.
Results
We identified a total of 2,288,579 discharges of patients having undergone THA from 1990 to 2004.
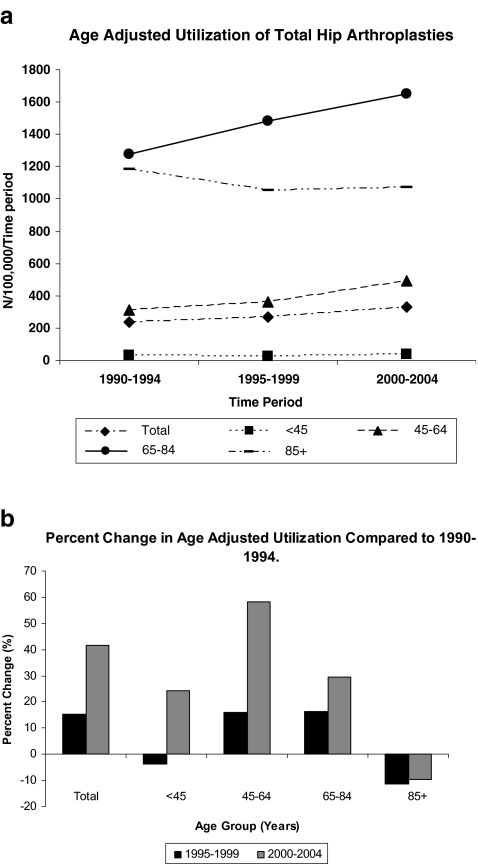
The total number of procedures performed in each time period increased (Table 1). The use of THA (number of procedures per 100,000 civilians) increased for most age categories (Fig. 1a). However, the highest percent of increase was seen in the group of patients aged between 45 and 64 years (Fig. 1b).
Table 1.
Changes in the prevalence of characteristics of discharges with the diagnosis for total hip arthroplasty by period of interest (POI) from 1990–2004
| Primary hip arthroplasties (ICD-9 81.51), 1990–2004, N =2,288,579 | ||||||||
|---|---|---|---|---|---|---|---|---|
| Period | 1990–1994 | 1995–1999 | 2000–2004 | 1990–2004 | ||||
| N (% of total) | 603,528 | 26.37 | 731921 | 31.98 | 953,130 | 41.65 | 2,288,579 | 100.00 |
| Age in years (range)a | 67.03 (6–99) | 67.19 (13–99) | 66.08 (18–99) | 66.68 (6–99) | ||||
| Age groups | ||||||||
| <45a (POI1 and 2 and POI1 and 3 only) | 49,716 | 8.24 | 48,907 | 6.68 | 64,336 | 6.75 | 162,959 | 7.12 |
| 46–64a | 149,393 | 24.75 | 198,905 | 27.18 | 326,889 | 34.30 | 675,187 | 29.50 |
| 65–79a(POI1 and 3 and POI2 and 3 only) | 365,940 | 60.63 | 443,428 | 60.58 | 512,862 | 53.81 | 1,322,230 | 57.78 |
| 85+a | 38,479 | 6.38 | 40,681 | 5.56 | 49,043 | 5.15 | 128,203 | 5.60 |
| Genderb | ||||||||
| Malea | 243,495 | 40.35 | 303,583 | 41.48 | 408,303 | 42.84 | 955,381 | 41.75 |
| Femalea | 360,033 | 59.66 | 428,338 | 58.52 | 544,827 | 57.16 | 1,333,198 | 58.25 |
| Race* | ||||||||
| Whitea | 452,691 | 75.01 | 501,914 | 68.58 | 628,157 | 65.91 | 1,582,762 | 69.16 |
| Blacka | 24,298 | 4.03 | 38,022 | 5.20 | 50,574 | 5.31 | 112,894 | 4.93 |
| Othera | 10,296 | 1.71 | 13,369 | 1.83 | 13,496 | 1.42 | 37,161 | 1.62 |
| Not stateda | 11,6243 | 19.26 | 178,616 | 24.40 | 260,903 | 27.37 | 555,762 | 24.28 |
| Discharge statusb | ||||||||
| Routine discharge to homea | 375,775 | 62.26 | 348,626 | 47.63 | 423,627 | 44.45 | 1,148,028 | 50.16 |
| Left against medical advicea (POI1 and 2 and POI1 and 3 only) | 1,614 | 0.27 | 120 | 0.02 | 168 | 0.02 | 1,902 | 0.08 |
| Discharge to short-term facilitya | 39,737 | 6.58 | 68,572 | 9.37 | 96,170 | 10.09 | 204,479 | 8.94 |
| Discharge to long-term facilitya (POI1 and 2 and POI 1 and 3 only) | 97,139 | 16.10 | 181,079 | 24.74 | 235,263 | 24.68 | 513,481 | 22.44 |
| Alive disposition not stateda | 77,437 | 12.83 | 122,529 | 16.74 | 170,369 | 17.88 | 370,335 | 16.18 |
| Deada (POI 1 and 3 and POI 2 and 3 only) | 1,977 | 0.33 | 2,446 | 0.33 | 2,839 | 0.30 | 7,262 | 0.32 |
| Not stated or reporteda | 9,849 | 1.63 | 8,549 | 1.17 | 24,694 | 2.59 | 43,092 | 1.88 |
| Bed sizeb | ||||||||
| 6–99a | 74,520 | 12.35 | 114,748 | 15.68 | 242,868 | 25.48 | 432,136 | 18.88 |
| 100–199a | 154,988 | 25.68 | 197,771 | 27.02 | 228,501 | 23.97 | 581,260 | 25.40 |
| 200–299a | 134,831 | 22.34 | 146,871 | 20.07 | 194,213 | 20.38 | 475,915 | 20.80 |
| 300–499a | 172,922 | 28.65 | 190,649 | 26.05 | 182,937 | 19.19 | 546,508 | 23.88 |
| 500+a (POI1 and 2 and POI2 and 3 only) | 66,267 | 10.98 | 81,882 | 11.19 | 104,611 | 10.98 | 252,760 | 11.04 |
| Regionb | ||||||||
| Northeasta | 133,397 | 22.10 | 159,541 | 21.80 | 232,522 | 24.40 | 525,460 | 22.96 |
| Midwesta | 172,362 | 28.56 | 201,757 | 27.57 | 256,897 | 26.95 | 631,016 | 27.57 |
| Southerna | 177,790 | 29.46 | 213,484 | 29.17 | 289,605 | 30.39 | 680,879 | 29.75 |
| Westerna | 119,979 | 19.88 | 157,139 | 21.47 | 174,106 | 18.27 | 451,224 | 19.72 |
| Insuranceb | ||||||||
| Medicarea | 377,515 | 62.55 | 434,217 | 59.33 | 409,861 | 43.00 | 1,221,593 | 53.38 |
| Medicaida | 16,690 | 2.77 | 24,135 | 3.30 | 29,507 | 3.10 | 70,332 | 3.07 |
| Privatea | 159,214 | 26.38 | 233,905 | 31.96 | 311,526 | 32.69 | 704,645 | 30.79 |
| Othera | 35,718 | 5.92 | 35,024 | 4.79 | 197,663 | 20.74 | 268,405 | 11.73 |
| Not stateda | 14,391 | 2.38 | 4,640 | 0.63 | 4,573 | 0.48 | 23,604 | 1.03 |
| Length of care in days (range)c | 8.74 (1–315) | 5.17 (1–170) | 4.45 (1–312) | 5.81 (1–315) | ||||
POI period of interest, POI1 = 1990–1994, POI2 = 1995–1999, POI3 = 2000–2004
a Significant differences found between all POIs (or POIs specified in parentheses) within variable using Z-score
b Significant differences found across categories within variable using chi square test
c Significant differences between POI using general linear model
Fig. 1.
a Use of primary total hip arthroplasty in the three study periods expressed as number of total hip arthroplasties performed per 100,000 civilians. The figures show total implantation and age-group adjusted implantation per each 5-year study period. Age adjusted implantations are restricted to the stated age group. Significant differences (P < 0.001) between all time periods for age groups 46–65 and 65–84. Significant differences (P <0.001) for total implantation for 1990–1994 and 2000–2004 only. b Age group adjusted percent change of implantation of primary total hip arthroplasties over time for each 5-year study period. Age adjusted implantations are restricted to the stated age group
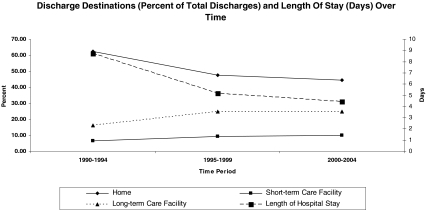
In-hospital mortality rate remained low and slightly decreased (0.33% in 1990–94 to 0.29% in 200–2004, Table 1). Overall, procedure-related complications and adverse diagnoses decreased over the study period (Table 2). The length of hospital stay decreased from an average of 8.7 days in 1990–1994 to 5.2 days in 1995–1999 and to 4.5 days in the most recent time period studied (Fig. 2). A shift in disposition status was seen, with fewer discharges to a primary residence (62.2% in 1990–1994 vs. 44.4% in 2000–2004) and more referrals to long- and short-term care facilities (22.5% in 1990–1994 vs. 34.7% in 2000–2004, Table 1, Fig. 2).
Table 2.
Prevalence of procedure related complications (ICD-9-CM codes 996 to 999) among discharges undergoing total hip arthroplasty from 1990–2004
| Procedure related complications (ICD-9 996–999) | ||||||||
|---|---|---|---|---|---|---|---|---|
| 1990–1994 | 1995–1999 | 2000–2004 | 1990–2004 | |||||
| Complications | N | % | N | % | N | % | N | % |
| Complications affecting specific body systems (ICD-9 997) | ||||||||
| Central nervous systema | 140 | 0.02 | 1,752 | 0.24 | 2,025 | 0.21 | 3,917 | 0.17 |
| Cardiaca | 5,108 | 0.85 | 7,276 | 0.99 | 9,036 | 0.95 | 21,420 | 0.94 |
| Peripheral vasculara | 1,991 | 0.33 | 339 | 0.05 | 1,354 | 0.14 | 3,684 | 0.16 |
| Respiratorya | 8,652 | 1.43 | 8,807 | 1.20 | 9,274 | 0.97 | 26,733 | 1.17 |
| Gastrointestinala | 7,107 | 1.18 | 7,521 | 1.03 | 7,157 | 0.75 | 21,785 | 0.95 |
| Genitourinarya | 9,612 | 1.59 | 6,345 | 0.87 | 8,877 | 0.93 | 24,834 | 1.09 |
| Other (organ specific)a | 584 | 0.10 | 2,804 | 0.38 | 1,177 | 0.12 | 4,565 | 0.20 |
| Other complications of procedure (ICD-9 998) | ||||||||
| Postoperative shock a | 449 | 0.07 | 49 | 0.01 | 524 | 0.06 | 1022 | 0.05 |
| Hematoma/seromaa | 8,304 | 1.38 | 12,494 | 1.71 | 13,700 | 1.44 | 34,498 | 1.51 |
| Accidental puncture/lacerationa | 156 | 0.03 | 549 | 0.08 | 551 | 0.06 | 1,256 | 0.06 |
| Disruption operative wounda | 192 | 0.03 | 0 | 0.00 | 684 | 0.07 | 876 | 0.04 |
| Postoperative infectiona | 4,160 | 0.69 | 4,739 | 0.65 | 1,884 | 0.20 | 10,783 | 0.47 |
| Other complications of procedurea | 20,598 | 3.41 | 16,113 | 2.20 | 16,242 | 1.70 | 52,953 | 2.31 |
| Complications of medical care (ICD-9 999) | ||||||||
| Complications of medical carea | 2,694 | 0.45 | 702 | 0.10 | 1,604 | 0.17 | 5,000 | 0.22 |
| Prevalence of selected adverse diagnosis in patients undergoing total hip arthroplasty | ||||||||
| Diagnosis | N | % | N | % | N | % | N | % |
| Acute posthemorrhagic anemiab | 127,813 | 21.18 | 194,150 | 26.53 | 170,291 | 17.87 | 492,254 | 21.51 |
| Psychosisb | 7,032 | 1.17 | 5,937 | 0.81 | 12,844 | 1.35 | 25,813 | 1.13 |
| Thrombotic eventsb | 3,588 | 0.60 | 1,941 | 0.27 | 3,082 | 0.32 | 8,611 | 0.38 |
| Pulmonary insufficiency after trauma and surgery/ARDSb | 175 | 0.03 | 737 | 0.10 | 1,905 | 0.20 | 2,817 | 0.12 |
| Pulmonary embolismb | 2,787 | 0.46 | 2,193 | 0.30 | 2,481 | 0.26 | 7,461 | 0.33 |
| Patients with any procedure related complicationa | 91,953 | 15.24 | 85,661 | 11.70 | 89,089 | 9.35 | 266,703 | 11.654 |
a Significant difference between all periods of interest (POI)
b Significant difference between all time periods
Fig. 2.
Discharge disposition as percent of all discharges (%) (left y-axis) and average hospital stay (days) (right y-axis) over time. Note that total percent of discharge dispositions may not add up to 100% as only selected disposition options are shown. Significant differences (P < 0.001) for all discharge destinations between all time periods, except for “long-term care facility” between 1995–1999 and 2000–2004. Significant differences (P < 0.001) for average hospital stay between all time periods
Trends in the prevalence of comorbidities are shown in Table 3. An increase in the prevalence of hypertension, diabetes mellitus, hypercholesteremia, obesity, pulmonary disease, and coronary artery disease was found over time. Hypertension was the most common comorbidity, occurring in nearly half of all patients in the most recent time period studied.
Table 3.
Prevalence of comorbidities among discharges undergoing total hip arthroplasty from 1990–2004
| 1990–1994 | 1995–1999 | 2000–2004 | 1990–2004 | |||||
|---|---|---|---|---|---|---|---|---|
| Time period | N | % | N | % | N | % | N | % |
| Hypertensiona | 157,120 | 26.03 | 271,410 | 37.08 | 430,515 | 45.17 | 859,045 | 37.54 |
| Diabetes mellitusa | 41,354 | 6.85 | 59,594 | 8.14 | 105,337 | 11.05 | 206,285 | 9.01 |
| Hypercholesteremiaa | 10,393 | 1.72 | 26,570 | 3.63 | 61,871 | 6.49 | 98,834 | 4.32 |
| Obesitya | 13,399 | 2.22 | 26,234 | 3.58 | 47,833 | 5.02 | 87,466 | 3.82 |
| Cerebrovascular diseasea | 6,306 | 1.05 | 5,318 | 0.73 | 6,362 | 0.67 | 17,986 | 0.79 |
| Peripheral vascular diseasea | 7,122 | 1.18 | 7,627 | 1.04 | 7,954 | 0.84 | 22,703 | 0.99 |
| Pulmonary Diseasea | 50,676 | 8.40 | 73,123 | 9.99 | 96,482 | 10.12 | 220,281 | 9.63 |
| Renal diseasea (POI 1 and 3 and POI 2 and 3 only) | 4,686 | 0.78 | 5,735 | 0.78 | 10,933 | 1.15 | 21,354 | 0.93 |
| Coronary artery diseasea | 45,641 | 7.56 | 69,302 | 9.47 | 107,542 | 11.28 | 222,485 | 9.72 |
a Significant difference between all time periods or between time periods indicated in parenthesis
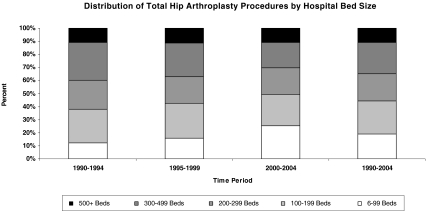
The proportion of cases performed at hospitals with less than 99 patient beds more than doubled over the 15-year study period from 12.3% in 1990–1994 to 25.5% in 2000–2004, while procedures in hospitals with a bed size of 200–499 decreased (50.9% vs. 39.4%, respectively) (Fig. 3).
Fig. 3.
Distribution of procedure volume by hospital bed size from 1990 to 2004. Significant differences (P < 0.001) for all hospital sizes between all time periods, except for 500+ between 1990–1994 and 2000–2004
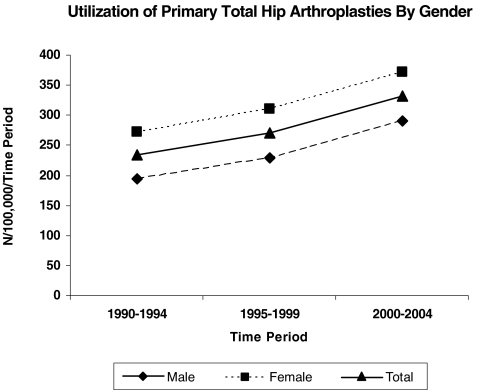
Average patient age decreased, accompanied by a shift of patients from the 65–84-year age group to the 45–64-year age group (Table 1). Females made up almost 60% of all procedures at all time periods (Fig. 4). However, the proportion of male patients undergoing THA increased by approximately 1% per time period (40.3% in 1990–1994 vs. 42.8% in 2000–2004). While the proportion of discharges categorized in the white race group decreased over time, the number for whom no race was listed increased, thus limiting the interpretation of trend data in regard to the race category.
Fig. 4.
Use of primary total hip arthroplasty for total population and restricted to either male or female gender for each 5-year study period. P < 0.001 for total and gender adjusted use between 1990–1994 and 2000–2004 (both genders)
Discussion
Multiple trends over time were noted in our analysis. From 1990 to 2004, the number of THAs increased by 158%. The increase in the number of THAs cannot be explained solely by an increase in the nation’s population or by ageing. The census count in the United States rose by approximately 18% over the time of the study [24], and the population older than 65 years increased by approximately 30% [7]. Thus, use of primary THA is increasing at a greater rate than population growth or ageing. This observation of increased implantation of THA has been reported by others for the United States and Europe [11, 13, 17], and will impact planning for allocation of medical resources for health care providers and payers.
The increased performance of THAs was coupled with a slightly reduced rate of in-hospital mortality and adverse events. Several factors may have contributed. The increased volume and use of THAs in itself may have contributed to decreased in-hospital mortality, as increased surgical volume has been consistently associated with reduced mortality and adverse events [11]. Concurrent advances during this same time period in anesthesia and perioperative care have been shown to be associated with a tenfold reduction in anesthesia related mortality, and this benefit may have also been transferred to perioperative care of THA [16].
During our study period, incidences of adverse events in general decreased. For example, incidences of several important diagnosis codes such as pulmonary embolism, shock, and infections decreased. This is in keeping with improved and more standardized care in thromboprophylaxis, perioperative medicine, and antibiotic administration [3, 12]. The reduction in risk of pulmonary embolism may be reassuring as much effort and creation of practice guidelines have been devoted to reduction of this complication [12].
Hospital length of stay substantially decreased during the study period by 50% from 8.7 to 4.5 days on average. This may reflect the increased use of “fast track” clinical pathways whereby multidisciplinary and multimodal teams create more efficient means to rehabilitate and discharge patients after THA [4]. Alternatively, the decreased length of hospital stay was also paralleled by a nearly 50% increased rate of discharges to short- and long-term care facilities. Thus, the apparent decreased length of hospital stay may represent a shift in disposition to rehabilitation centers. As specialized rehabilitation centers are typically less costly than hospitals [15], either explanation suggests a reduction in health costs. Although costs are decreased by rapid hospital discharge, further reductions in hospital stay may shift the monitoring period for serious complications to an out-of-hospital environment. Parvizi recently noted that most serious complications after total joint replacement may take up to 4 days to occur and that 58% of patients had no early identifiers for serious complications [22]. Thus, further reductions in length of stay will require development of better outpatient monitoring and rescue processes for these serious complications.
Despite the reduction in in-hospital mortality, complications, and length of stay, the most recent study period was also associated with a greater incidence of risk factors and comorbidities in the THA patients, especially with an increase in diagnoses of hypertension, diabetes, coronary artery disease, and obesity. These comorbidities in THA patients reflect the declining health status of the general US population. The National Center for Health Statistics has published data showing that the proportion of adults in the United States over the age of 20 who suffer from hypertension and diabetes has increased in the time periods 1988–1994 and 2001–2004 (21.7% to 25.3%, and 8.4% to 10.3%, respectively) [20]. Coronary artery disease remains the top health issue in the United States and is thus reflected in the THA population [6]. Rates of obesity continue to increase with two-thirds of Americans qualifying as overweight. The National Health and Nutrition Examination Survey has noted an increased incidence in obesity from the time period 1988–1994 to 1999–2000 (15% to 30%) [7]. These are important findings for perioperative care, as previous studies have identified obesity, diabetes, and greater overall comorbidity burden as risk factors for prolonged wound drainage, wound infection, and myocardial infarction after THA [9, 19, 23].
Our data identified a substantial shift in performance of THA away from large medical centers and towards smaller facilities (<100 beds). This may represent the increasing popularity and availability of the procedure in smaller communities. However, multiple studies have identified a large surgical volume and performance in a teaching center as independent positive factors to decrease mortality, postoperative complications, and length of stay after THA in the United States and Europe [10, 11, 18]. In addition, some data suggest that costs are lower in high volume medical centers [18]. Thus, future monitoring may be needed to determine if the shift to smaller facilities with presumably less surgical volumes will negatively impact the current trends of improving outcomes.
Patient demographics also changed during the study period, and these changes may affect future practice and policy. There was a substantial decrease in patient age towards the <65-year-old category. Interestingly, age <60 has been identified as an independent risk factor for primary implant failure after THA [25]. Thus, the ever younger population undergoing THA may require a greater burden of revision THAs in the future [14]. As revision THAs are associated with greater complications, this projected increase in use may increase consumption of medical resources [25]. There were only marginal changes in the gender distribution of patients undergoing THAs during the 15 years of the study. The average ratio of men to women remained approximately 1:1.4, which is within the range reported in other studies [17]. Research suggests that osteoarthritis is both more prevalent and incapacitating in females than males, which may explain discrepancies in implantation found between genders [7].
In conclusion, we identified increased THA use with concomitant reductions in in-hospital mortality, adverse events, and length of stay. These trends may be used for future planning of allocation of perioperative resources such as specialist consultations, creation of clinical processes to optimize care, and building of new hospitals or rehabilitation centers. THAs were performed in younger patients with more comorbidities. This trend may result in a higher revision burden and greater risk for perioperative complications in the next decades.
Acknowledgments
This study was performed with funds provided by the Hospital for Special Surgery Young Investigator Award (Dr. Memtsoudis) and by the Department of Anesthesiology, Hospital for Special Surgery. No conflicts of interest arise from any part of this study for any of the authors.
Appendix
References
- 1.Ackerman IN, Graves SE, Bennell KL, Osborne RH. Evaluating quality of life in hip and knee replacement: psychometric properties of the World Health Organization quality of life short version instrument. Arthritis Rheum. 2006;55:583–590. doi: 10.1002/art.22107. [DOI] [PubMed] [Google Scholar]
- 2.Barrett J, Losina E, Baron JA, Mahomed NN, Wright J, Katz JN. Survival following total hip replacement. J Bone Jt Surg Am. 2005;87:1965–1971. doi: 10.2106/JBJS.D.02440. [DOI] [PubMed] [Google Scholar]
- 3.Bhattacharyya T, Hooper DC. Antibiotic dosing before primary hip and knee replacement as a pay-for-performance measure. J Bone Jt Surg Am. 2007;89:287–291. doi: 10.2106/JBJS.F.00136. [DOI] [PubMed] [Google Scholar]
- 4.Brunenberg DE, Steyn MJ, Sluimer JC, Bekebrede LL, Bulstra SK, Joore MA. Joint recovery programme versus usual care: an economic evaluation of a clinical pathway for joint replacement surgery. Med Care. 2005;43:1018–1026. doi: 10.1097/01.mlr.0000178266.75744.35. [DOI] [PubMed] [Google Scholar]
- 5.Centers for Disease Control and Prevention (2007) Selected articles using National Hospital Discharge Survey (NHDS) or National Survey of Ambulatory Surgery (NSAS) data. http://www.cdc.gov/nchs/data/hdasd/NHDS2007articleupdate.pdf. Accessed 10 March 2008
- 6.Chambers TA, Bagai A, Ivascu N. Current trends in coronary artery disease in women. Curr Opin Anaesthesiol. 2007;20:75–82. doi: 10.1097/ACO.0b013e3280146455. [DOI] [PubMed] [Google Scholar]
- 7.Crowninshield RD, Rosenberg AG, Sporer SM. Changing demographics of patients with total joint replacement. Clin Orthop Relat Res. 2006;443:266–272. doi: 10.1097/01.blo.0000188066.01833.4f. [DOI] [PubMed] [Google Scholar]
- 8.Dennison C, Pokras R (2000) Design and operation of the National Hospital Discharge Survey: 1988 redesign. Vital and health statistics. Series 1–42. CDC, National Center for Health Statistics,Hyattsville, MD [PubMed]
- 9.Gandhi R, Petruccelli D, Devereaux PJ, Adili A, Hubmann M, Beer J. Incidence and timing of myocardial infarction after total joint arthroplasty. J Arthroplast. 2006;21:874–877. doi: 10.1016/j.arth.2005.10.007. [DOI] [PubMed] [Google Scholar]
- 10.Husted H, Hansen HC, Holm G, Bach-Dal C, Rud K, Andersen KL, Kehlet H. Length of stay in total hip and knee arthroplasty in Denmark I: volume, morbidity, mortality and resource utilization. A national survey in orthopaedic departments in Denmark. Ugeskr Laeger. 2006;168:2139–2143. [PubMed] [Google Scholar]
- 11.Judge A, Chard J, Learmonth I, Dieppe P. The effects of surgical volumes and training centre status on outcomes following total joint replacement: analysis of the Hospital Episode Statistics for England. J Public Health (Oxf) 2006;28:116–124. doi: 10.1093/pubmed/fdl003. [DOI] [PubMed] [Google Scholar]
- 12.Krotenberg R. Current recommendations for extended out-of-hospital thromboprophylaxis following total hip arthroplasty. Am J Orthop. 2004;33:180–184. [PubMed] [Google Scholar]
- 13.Kurtz S, Mowat F, Ong K, Chan N, Lau E, Halpern M. Prevalence of primary and revision total hip and knee arthroplasty in the United States from 1990 through 2002. J Bone Jt Surg Am. 2005;87:1487–1497. doi: 10.2106/JBJS.D.02441. [DOI] [PubMed] [Google Scholar]
- 14.Kurtz S, Ong K, Lau E, Mowat F, Halpern M. Projections of primary and revision hip and knee arthroplasty in the United States from 2005 to 2030. J Bone Jt Surg Am. 2007;89:780–785. doi: 10.2106/JBJS.F.00222. [DOI] [PubMed] [Google Scholar]
- 15.Lavernia CJ, D’Apuzzo MR, Hernandez VH, Lee DJ, Rossi MD. Postdischarge costs in arthroplasty surgery. J Arthroplast. 2006;21:144–150. doi: 10.1016/j.arth.2006.05.003. [DOI] [PubMed] [Google Scholar]
- 16.Lienhart A, Auroy Y, Pequignot F, Benhamou D, Warszawski J, Bovet M, Jougla E. Survey of anesthesia-related mortality in France. Anesthesiology. 2006;105:1087–1097. doi: 10.1097/00000542-200612000-00008. [DOI] [PubMed] [Google Scholar]
- 17.Lohmander LS, Engesaeter LB, Herberts P, Ingvarsson T, Lucht U, Puolakka TJ. Standardized incidence rates of total hip replacement for primary hip osteoarthritis in the 5 Nordic countries: similarities and differences. Acta Orthop. 2006;77:733–740. doi: 10.1080/17453670610012917. [DOI] [PubMed] [Google Scholar]
- 18.Martineau P, Filion KB, Huk OL, Zukor DJ, Eisenberg MJ, Antoniou J (2005) Primary hip arthroplasty costs are greater in low-volume than in high-volume Canadian hospitals. Clin Orthop Relat Res 152–156 [DOI] [PubMed]
- 19.Namba RS, Paxton L, Fithian DC, Stone ML. Obesity and perioperative morbidity in total hip and total knee arthroplasty patients. J Arthroplast. 2005;20:46–50. doi: 10.1016/j.arth.2005.04.023. [DOI] [PubMed] [Google Scholar]
- 20.National Center for Health Statistics (2006) Health, United States, 2006. Available at: http://www.cdc.gov/nchs/data/hus/hus06.pdf. Accessed 10 March 2008
- 21.Nowygrod R, Egorova N, Greco G, Anderson P, Gelijns A, Moskowitz A, McKinsey J, Morrissey N, Kent KC. Trends, complications, and mortality in peripheral vascular surgery. J Vasc Surg. 2006;43:205–216. doi: 10.1016/j.jvs.2005.11.002. [DOI] [PubMed] [Google Scholar]
- 22.Parvizi J, Mui A, Purtill JJ, Sharkey PF, Hozack WJ, Rothman RH. Total joint arthroplasty: when do fatal or near-fatal complications occur? J Bone Jt Surg Am. 2007;89:27–32. doi: 10.2106/JBJS.E.01443. [DOI] [PubMed] [Google Scholar]
- 23.Patel VP, Walsh M, Sehgal B, Preston C, DeWal H, Cesare PE. Factors associated with prolonged wound drainage after primary total hip and knee arthroplasty. J Bone Jt Surg Am. 2007;89:33–38. doi: 10.2106/JBJS.F.00163. [DOI] [PubMed] [Google Scholar]
- 24.US Census Bureau (2006) National intercensal estimates (1990–2000). Available at: http://www.census.gov/popest/archives/EST90INTERCENSAL/US-EST90INT-datasets.html. Accessed 10 March 2008
- 25.Zhan C, Kaczmarek R, Loyo-Berrios N, Sangl J, Bright RA. Incidence and short-term outcomes of primary and revision hip replacement in the United States. J Bone Jt Surg Am. 2007;89:526–533. doi: 10.2106/JBJS.F.00952. [DOI] [PubMed] [Google Scholar]