Abstract
This prospective, randomised case-control study was made to determine effectiveness of low-dose Depo-Medrol applied to the affected nerve root after discectomy. Fifty seven patients with L4–5 or L5-S1 single level disc herniation with unilateral leg pain were selected for the study and were divided in two groups. Twenty eight patients were in the control group and 29 in the steroid group. Discectomy was done after flavotomy in all patients. In the steroid group low-dose 40 mg Depo-Medrol soaked Gelfoam was applied over the affected nerve root after discectomy while in the control group neither saline nor plain Gelfoam was applied to affected root. Postoperatively, patients were asked to evaluate backache using VAS which was compared statistically using the unpaired t test. Statistical difference was significant (p < 0.0001) regarding postoperative VAS during the first month and then it became insignificant. Results show that local application of low-dose Depo-Medrol is helpful in reducing immediate postoperative backache after discectomy, but it is not effective in the long-term.
Résumé
Il s’agit d’une étude prospective randomisée pour montrer les effets de petite dose de dépo-Médrol appliqué sur les racines nerveuses après discectomie. 57 patients présentant une hernie discale L4-L5 ou L5-S1, avec une douleur unilatérale ont été sélectionnés pour cette étude. Deux groupes ont été constitués, 28 patients constituant le groupe contrôle et 29 patients le groupe stéroïde. La discectomie a été réalisée après l’ablation du ligament jaune chez tous les patients. Dans le groupe stéroïde une petite dose de 40 mg de Dépo-Médrol sous forme de gel a été appliquée sur la racine nerveuse après discectomie et sur le groupe contrôle un gel d’origine saline. En post-opératoire les patients ont été questionnés pour évaluer les lombalgies en utilisant la méthode VAS avec tests statistiques. Les résultats sont statistiquement différents en post-opératoire (p < 0,0001), au cours du premier mois puis petit à petit la différence devient non significative. Ces résultats montrent donc que l’application locale d’une petite dose de dépo-médrol permet de diminuer la douleur post-opératoire immédiate après discectomie. Mais ceci n’entraîne pas d’amélioration à long terme.
Introduction
Treatment for lumbar disc herniation is discectomy if conservative treatment fails. Discectomy significantly relieves back pain as well as radicular symptoms after the operation. However, residual back pain and radicular leg pain are not uncommon in a majority of patients who undergo discectomy. This pain may vary in intensity, from mild to severe, and it can cause significant postoperative disability or prolonged hospital stay. Oedema and inflammation of the nerve root or dorsal root ganglions (to a major extent) and handling of the nerve root (to a minor extent) are responsible for creating uncomfortable situations for many patients and may increase the postoperative requirement of anti-inflammatory analgesics or morphine derivatives and exposes the patient to side effects related to these medicines. In addition the inflammation together with surgical intervention might negatively influence the long term results by initiating fibrosis [16] which is considered one of the reasons for the late appearance of pain [3]. Therefore, instead of gaining, patients lose the confidence and potential benefits after discectomy.
Reduction of inflammation and oedema of the affected nerve root should reduce the postoperative pain intensity. Perioperative use of corticosteroids and bupivacaine [6–9, 14] has been reported as effective analgesia and decreases opioid or analgesic use without complications. Local or systematic use of various steroids [1, 13] is described in the literature in lumbar disc patients. Wound infiltration with an anaesthetic agent [9, 14] before the skin incision is also a way of reducing postoperative back pain. All the modalities aim at mobilising the patient early and reducing the disability. However, use of these methods in high doses predispose to the risk of postoperative infections [12, 13]. In addition, the studies describe the success of local steroid application after surgery use in a control group that had received an application of collagen foam or fat graft soaked in saline. However, in clinical practice, we do not know whether these patients received a saline application postoperatively.
In this study, we present a prospective, randomised case-control study of local application of low-dose Depo-Medrol (methylprednisolone) on the affected nerve root postoperatively. We have compared our results with a control group which did not receive local application of Depo-Medrol or saline postoperatively. We assume that local application of low-dose steroid alone is sufficient to reduce the postoperative morbidity without increasing side effects or complications.
Materials and methods
Patient population
All patients admitted to our institution for removal of lumbar disc herniation from 2004 to 2006 were included in this prospective study. They were treated initially with bed rest, physiotherapy, and nonsteroidal anti-inflammatory medicines. Decision for surgery was taken after four weeks of conservative treatment in all patients. The patients who had undergone discectomy within four weeks had severe leg pain or neurological deficit at the time of operation. The patients’ symptoms were recorded preoperatively. All patients selected for this study had positive straight leg raising (SLR) test on examination. Visual analogue scale (VAS) pain measurement was noted for all patients preoperatively. We excluded the patients who had bilateral radicular symptoms, disc involvement at more than one level, level above L4–5, chronic disc disease, or associated lumbar stenosis on MRI. Therefore, our study includes only those who had L4–5 or L5-S1 disc herniation and unilateral leg symptoms. None of them had any systemic illness, diabetes mellitus, known malignancy, or previous back surgery. There were 57 patients in the study: 29 comprising the steroid group and 28 comprising the control group. Randomisation was performed immediately before surgery by opening a sealed envelope with a note inside indicating to which group the patient was assigned. Postoperatively, all patients were followed up for an average of 31.3 months for the control group and 31.1 months for the steroid group. There were 21 males and seven females in the control group and 25 males and four females in the steroid group with an average age of 30.1 years (range, 19–45 years) and 29.8 years (range, 19–44 years), respectively, for the control and steroid groups.
Operative technique
All patients were operated upon in the same way by a single spine surgeon (KJC). The patients were placed in the prone position after general anaesthesia on a Jackson table with knee joints flexed to 15–20 degrees. A 3–5-cm midline incision was made over the proper segment determined before the incision under an image intensifier television (IITV). No infiltration was made to skin or paraspinal muscles before the incision. After the skin incision, paraspinal muscles were unilaterally stripped from the spinous process and lamina of the vertebra on the side of herniation with the help of cautery. Interspinous and supraspinous ligaments were protected from injury throughout the procedure. After excision of the ligametum flavum, the herniated disc was approached by retracting the nerve root medially and was removed. Following meticulous haemostasis, a 2.5 × 2.5 cm Gelfoam soaked with 40 mg methylprednisolone acetate (Depo-Medrol, Upjohn, Puurs, Belgium) was left on the decompressed nerve root in the steroid group. In the control group, neither saline soaked Gelfoam nor plain Gelfoam was applied to the nerve root. The wound was closed over a mini drain with negative suction which was removed 24–48 hours after the operation.
Postoperative evaluation
Postoperatively, the entire patient group was asked to grade their back pain intensity and VAS score were recorded at two weeks, one month, three months, six months, one year, and final follow-up after the operation. The pain intensity was graded from 0 (no pain) to 10 (most severe pain). All patients were encouraged to walk immediately postoperatively once pain reduced and to resume their routine work after the discharge on regular follow-up. The patients were evaluated symptomatically as well as neurologically immediately postoperatively and at follow-up. We compared VAS scores between control and steroid groups using an unpaired t test. P values less than 0.05 were considered statistically significant (MedCalc Software, version 8.1.1, Mariakerke, Belgium).
Results
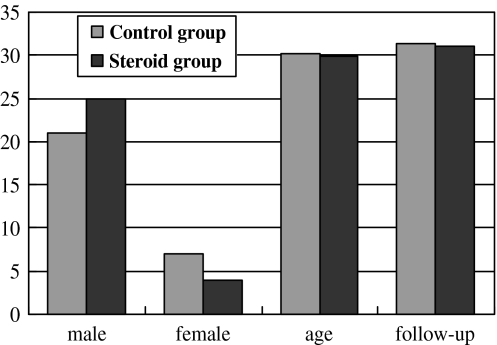
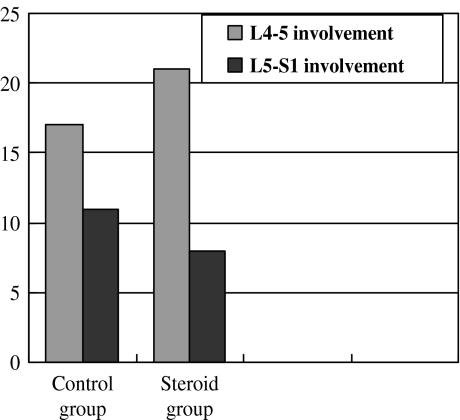
The average duration of symptoms was 5.6 weeks (range, 1–12 weeks) for the control group and 5.9 weeks (range, 2–11 weeks) for the steroid group. Table 1 shows average age and average preoperative and postoperative VAS scores at different follow-up. Statistically the two groups neither differed according to age (p = 0.187) nor according to duration of symptoms (p = 0.639) at the time of operation (Fig. 1). There were 17 with L4–5 and 11 patients with L5-S1 level involvement in the control group, and 21 patients with L4–5 and eight with L5-S1 level involvement in the steroid group, which is also statistically insignificant (p = 0.349) (Fig. 2).
Table 1.
Patient demographics and their visual analogue scale pre- and postoperatively
| Control group | Steroid group | |
|---|---|---|
| No. of patients | 28 | 29 |
| Gender (male vs female) | 18 vs 11 | 25 vs 4 |
| Average age (years ± SD) | 30.14 ± 8.15 | 29.82 ± 7.16 |
| Symptom duration (weeks ± SD) | 5.57 ± 2.67 | 5.89 ± 2.54 |
| Pre-op VAS (avg ± SD) | 7.92 ± 0.44 | 7.77 ± 0.35 |
| Post-op 2-week VAS (avg ± SD) | 3.92 ± 0.26 | 2.96 ± 0.38 |
| Post-op 1-month VAS (avg ± SD) | 3.03 ± 0.17 | 2.54 ± 0.20 |
| Post-op 3-month VAS (avg ± SD) | 3.01 ± 0.14 | 2.90 ± 0.29 |
| Post-op 6-month VAS (avg ± SD) | 3.13 ± 0.15 | 3.12 ± 0.28 |
| Post-op 1-year VAS (avg ± SD) | 3.30 ± 0.20 | 3.37 ± 0.16 |
| Final follow-up VAS (avg ± SD) | 3.45 ± 0.18 | 3.4 ± 0.19 |
| Follow-up (months ± SD) | 31.35 ± 5.17 | 31.20 ± 3.18 |
Values are displayed with their standard deviations (SD) from average (avg)
VAS visual analogue scale
Fig. 1.
Distribution of control and steroid groups according to sex, age, and follow-up period
Fig. 2.
Involvement of L4–5 and L5-S1 levels in the control and steroid groups
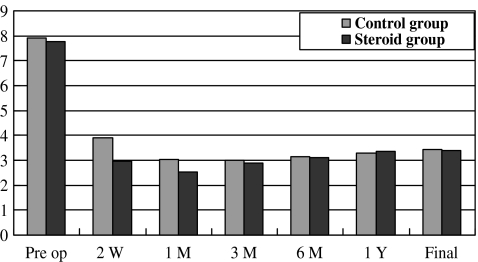
Tables 2 and 3 exhibit the details of each patient profile in the control and steroid groups, respectively. When preoperative VAS scores were compared between two groups, they did not differ statistically from each other (p = 0.372). Postoperatively at two weeks, VAS scores were 3.92 and 2.96 and at one month 3.03 and 2.54 for control and steroid groups, respectively, suggesting significant relief in back pain compared to preoperative status (Fig. 3). However, there was a statistically significant difference in VAS score at two weeks (p < 0.001) and at one month (p < 0.001) postoperatively when comparing control and steroid groups. The difference became insignificant at three months (p = 0.074), six months (p = 0.895), one year (p = 0.185), and at final follow-up (p = 0.325) which suggests that after one month there was no difference in clinical results after operation in either group.
Table 2.
Distribution, involvement of levels, and pre- and postoperative visual analogue scales with preoperative symptom duration and follow-up duration of each patient in the control group
| No. | Sex | Age (years) | Level | Duration (weeks) | SLR | Pre-op VAS | PO 2W VAS | PO 1M VAS | PO 3M VAS | PO 6M VAS | PO 1Y VAS | Final VAS | Follow-up (months) |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | M | 23 | L4-5 | 1 | + | 7.8 | 3.8 | 3.2 | 3.1 | 3.3 | 3.5 | 3.6 | 24 |
| 2 | M | 23 | L5-S1 | 4 | + | 7.5 | 4.2 | 3.3 | 3.2 | 3.1 | 3.4 | 3.5 | 27 |
| 3 | M | 43 | L5-S1 | 6 | + | 7.9 | 3.9 | 3.1 | 3.2 | 3.1 | 3.3 | 3.4 | 26 |
| 4 | F | 20 | L4-5 | 7 | + | 8.2 | 4.1 | 3.1 | 3.3 | 3.2 | 3.4 | 3.3 | 48 |
| 5 | M | 42 | L4-5 | 8 | + | 7.3 | 3.7 | 2.9 | 3.1 | 3.2 | 3.6 | 3.5 | 36 |
| 6 | F | 28 | L4-5 | 3 | + | 8 | 4 | 3.2 | 3 | 3.2 | 3.4 | 3.4 | 37 |
| 7 | F | 32 | L4-5 | 2 | + | 8.1 | 4.1 | 3 | 3.1 | 3.3 | 3.5 | 3.6 | 29 |
| 8 | M | 31 | L5-S1 | 2 | + | 6.9 | 3.7 | 2.9 | 3.1 | 2.9 | 3.2 | 3.7 | 28 |
| 9 | M | 19 | L4-5 | 4 | + | 7.4 | 3.6 | 2.8 | 2.9 | 3.4 | 3.3 | 3.7 | 27 |
| 10 | M | 38 | L5-S1 | 5 | + | 7.7 | 3.8 | 3.1 | 2.9 | 3.2 | 3.1 | 3.5 | 31 |
| 11 | M | 18 | L4-5 | 9 | + | 8.1 | 4.1 | 3.2 | 3 | 3.1 | 3.5 | 3.4 | 33 |
| 12 | M | 22 | L4-5 | 6 | + | 7.6 | 3.5 | 2.6 | 2.8 | 3.1 | 3.3 | 3.6 | 34 |
| 13 | M | 26 | L5-S1 | 7 | + | 8.5 | 3.6 | 3 | 3.1 | 3.1 | 3.4 | 3.5 | 32 |
| 14 | F | 27 | L5-S1 | 8 | + | 9 | 3.7 | 2.9 | 2.9 | 3.2 | 3.3 | 3.2 | 35 |
| 15 | F | 28 | L4-5 | 5 | + | 8.3 | 4.1 | 3.2 | 3.2 | 3.3 | 3.6 | 3.6 | 37 |
| 16 | M | 36 | L4-5 | 4 | + | 8.5 | 4.2 | 3.3 | 3.1 | 3.4 | 3.5 | 3.4 | 36 |
| 17 | F | 26 | L4-5 | 3 | + | 7.9 | 3.9 | 3.1 | 3.2 | 2.9 | 3.1 | 3.3 | 29 |
| 18 | M | 31 | L4-5 | 6 | + | 8.1 | 3.8 | 3 | 2.9 | 3 | 3.1 | 3.2 | 27 |
| 19 | M | 38 | L5-S1 | 4 | + | 7.8 | 4.3 | 2.9 | 2.8 | 2.9 | 2.6 | 2.9 | 26 |
| 20 | M | 33 | L4-5 | 3 | + | 7.7 | 3.9 | 3.1 | 3.1 | 3.2 | 3.1 | 3.2 | 31 |
| 21 | M | 36 | L5-S1 | 7 | + | 7.4 | 4.2 | 3.1 | 3 | 3.2 | 3.3 | 3.4 | 30 |
| 22 | M | 42 | L4-5 | 5 | + | 7.9 | 4.1 | 3.2 | 3 | 2.9 | 3.1 | 3.3 | 32 |
| 23 | M | 20 | L5-S1 | 3 | + | 8.2 | 3.6 | 2.9 | 2.9 | 3.1 | 3.3 | 3.5 | 34 |
| 24 | F | 45 | L5-S1 | 11 | + | 8.6 | 3.5 | 2.8 | 2.8 | 2.9 | 3.3 | 3.4 | 35 |
| 25 | M | 42 | L4-5 | 12 | + | 8.1 | 3.7 | 2.8 | 2.7 | 2.9 | 3.4 | 3.6 | 31 |
| 26 | M | 24 | L4-5 | 8 | + | 8.2 | 4.2 | 3.1 | 3 | 3.2 | 3.3 | 3.7 | 24 |
| 27 | M | 24 | L4-5 | 7 | + | 7.8 | 4.4 | 3.2 | 3.1 | 3.3 | 3.4 | 3.6 | 25 |
| 28 | M | 27 | L5-S1 | 6 | + | 7.5 | 4.3 | 3 | 3 | 3.1 | 3.3 | 3.6 | 34 |
SLR straight leg raising test, Duration duration of symptoms in weeks before operation, Pre-op VAS preoperative visual analogue scale, PO 2W VAS postoperative visual analogue scale at 2 weeks, PO 1M VAS postoperative visual analogue scale at 1 month, PO 3M VAS postoperative visual analogue scale at 3 months, PO 6M VAS postoperative visual analogue scale at 6 months, PO 1Y VAS postoperative visual analogue scale at 1 year
Table 3.
Distribution, involvement of levels, and pre- and postoperative visual analogue scales with preoperative symptom duration and follow-up duration of each patient in the steroid group
| No | Sex | Age (years) | Level | Duration (weeks) | SLR | Pre-op VAS | PO 2W VAS | PO 1M VAS | PO 3M VAS | PO 6M VAS | PO 1Y VAS | Final VAS | Follow-up (months) |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | M | 24 | L4-5 | 2 | + | 7.9 | 2.6 | 2.1 | 2.3 | 2.7 | 3.3 | 3.4 | 28 |
| 2 | M | 25 | L4-5 | 5 | + | 7.7 | 3.1 | 2.5 | 2.6 | 2.8 | 3.2 | 3.1 | 31 |
| 3 | M | 44 | L4-5 | 7 | + | 8.2 | 3.2 | 2.6 | 2.8 | 2.7 | 3.4 | 3.6 | 34 |
| 4 | M | 19 | L4-5 | 8 | + | 8.3 | 2.9 | 2.7 | 2.7 | 2.6 | 3.3 | 3.5 | 35 |
| 5 | M | 43 | L4-5 | 9 | + | 8.5 | 3.1 | 2.6 | 2.8 | 2.9 | 3.2 | 3.6 | 29 |
| 6 | M | 34 | L4-5 | 5 | + | 8.6 | 3.3 | 2.5 | 2.9 | 2.9 | 3.1 | 3.4 | 33 |
| 7 | F | 33 | L4-5 | 4 | + | 7.6 | 3.2 | 2.7 | 3 | 3.1 | 3.4 | 3.7 | 28 |
| 8 | M | 32 | L4-5 | 2 | + | 6.9 | 2.9 | 2.4 | 2.6 | 2.7 | 3.1 | 3.6 | 29 |
| 9 | M | 20 | L4-5 | 3 | + | 7.6 | 2.8 | 2.3 | 2.7 | 2.8 | 3.2 | 3.6 | 34 |
| 10 | M | 36 | L5-S1 | 6 | + | 7.5 | 3.1 | 2.6 | 2.9 | 3.1 | 3.3 | 3.5 | 35 |
| 11 | M | 20 | L4-5 | 5 | + | 7.8 | 3.4 | 2.9 | 3 | 3.2 | 3.4 | 3.7 | 31 |
| 12 | M | 24 | L4-5 | 7 | + | 7.7 | 3.6 | 2.7 | 2.9 | 3.2 | 3.5 | 3.6 | 30 |
| 13 | M | 26 | L5-S1 | 6 | + | 7.6 | 3.2 | 2.8 | 2.9 | 3.4 | 3.4 | 3.4 | 29 |
| 14 | F | 26 | L5-S1 | 10 | + | 8.1 | 3.3 | 2.5 | 2.9 | 3.1 | 3.2 | 3.6 | 28 |
| 15 | F | 28 | L4-5 | 6 | + | 7.8 | 3.4 | 2.6 | 3.3 | 3.5 | 3.3 | 3.1 | 27 |
| 16 | M | 37 | L4-5 | 4 | + | 7.5 | 3.1 | 2.7 | 3.2 | 3.3 | 3.4 | 3.1 | 33 |
| 17 | F | 25 | L4-5 | 3 | + | 8.2 | 3.2 | 2.8 | 3.1 | 3.2 | 3.3 | 3.2 | 25 |
| 18 | M | 32 | L4-5 | 4 | + | 8.1 | 2.5 | 2.4 | 3.6 | 3.4 | 3.6 | 3.3 | 28 |
| 19 | M | 33 | L5-S1 | 2 | + | 8.2 | 1.9 | 2.4 | 3.2 | 3.1 | 3.1 | 3.4 | 29 |
| 20 | M | 34 | L4-5 | 3 | + | 7.8 | 2.4 | 2.6 | 3.3 | 3.6 | 3.5 | 3.3 | 34 |
| 21 | M | 27 | L5-S1 | 8 | + | 7.6 | 2.7 | 2.4 | 3.5 | 3.4 | 3.6 | 3.4 | 33 |
| 22 | M | 40 | L4-5 | 6 | + | 7.6 | 2.5 | 2.3 | 2.7 | 3.4 | 3.4 | 3.1 | 39 |
| 23 | M | 22 | L5-S1 | 7 | + | 7.9 | 3.3 | 3 | 2.9 | 3.3 | 3.7 | 37 | |
| 24 | F | 41 | L5-S1 | 10 | + | 7.6 | 3.1 | 2.7 | 2.9 | 3.6 | 3.4 | 3.5 | 33 |
| 25 | M | 38 | L4-5 | 11 | + | 7.8 | 3.2 | 2.6 | 3.1 | 3.3 | 3.6 | 3.6 | 32 |
| 26 | M | 25 | L4-5 | 9 | + | 8.1 | 3.2 | 2.4 | 2.6 | 3.2 | 3.5 | 34 | 31 |
| 27 | M | 26 | L4-5 | 8 | + | 7.6 | 2.6 | 2.3 | 2.7 | 3.2 | 3.4 | 3.2 | 31 |
| 28 | M | 28 | L5-S1 | 5 | + | 7.8 | 2.7 | 2.5 | 2.6 | 3.1 | 3.6 | 3.1 | 30 |
| 29 | M | 23 | L4-5 | 6 | + | 7.5 | 2.4 | 2.2 | 2.5 | 2.8 | 3.4 | 3.3 | 29 |
SLR straight leg raising test, Duration duration of symptoms in weeks before operation, Pre-op VAS preoperative visual analogue scale, PO 2W VAS postoperative visual analogue scale at 2 weeks, PO 1M VAS postoperative visual analogue scale at 1 month, PO 3M VAS postoperative visual analogue scale at 3 months, PO 6M VAS postoperative visual analogue scale at 6 months, PO 1Y VAS postoperative visual analogue scale at 1 year
Fig. 3.
Preoperative, postoperative 2 weeks, 1 month, 3 months, 6 months, 1 year, and final follow-up Visual Analog Scale (VAS) score in both groups
No patient from either group received any steroid to relieve the postoperative symptoms either in the form of oral or systemic application. None of the patients in the entire study group received any muscle relaxant or morphine derivatives for postoperative back or leg pain. Postoperative pain was controlled by anti-inflammatory analgesic medicines only to maintain the uniformity of the study. None of the patients showed VAS score more than 5 during the entire postoperative follow-up period. However, we observed increased frequency of anti-inflammatory analgesic consumption during the first postoperative month in patients from the control group. No obvious complications were noted postoperatively in either group in the form of infection, re-herniation of the disc, secondary operations, or neurological deficits. There were no dural tears or CSF leaks intraoperatively. Only a few patients from both groups had mild gastritis or nausea due to anti-inflammatory analgesics which were controlled with appropriate antacids.
Discussion
It is well known that back and leg pain following lumbar disc herniation is due to both compression and inflammatory oedema of the nerve root. Therefore if the stimulus is applied to an inflamed oedematous nerve root with fibrosis and demyelination, significant pain can result [17]. This indicates that a patient can not be completely relieved of back or leg pain even after successful removal of the herniated disc because discectomy can not reduce oedema and inflammation immediately after operation. There are various preoperative, perioperative, or postoperative ways to reduce inflammation and oedema of the affected nerve. Butterman [4] reported preoperative effects of epidural steroid injection in 169 patients with large disc herniation and compared the results with discectomy. He found that epidural injections were successful in relieving symptoms in a few patients or delaying the timing of surgery; however, it was not as effective as discectomy with regard to reducing symptoms and disability associated with a large disc herniation. We did not inject epidural steroid preoperatively in our study group; instead we considered discectomy if conservative treatment did not relieve the symptoms. Pre-emptive analgesia is also intended to inhibit the sensitisation of the central nervous system with a stimulus by applying analgesia before the pain stimulus starts. Mullen and Cook [15] reported that use of intramuscular bupivacaine during the lumbar discectomy reduces postoperative back pain. Cherian et al. [5] reported that wound infiltration with bupivacaine before the incision resulted in significance between groups in the time to first postoperative use of narcotic analgesic. In our study we did not infiltrate skin with any anaesthetic or analgesic agents before the incision.
Various substances that produce pain and are released by the herniated disc have been identified in the literature [18]. Autoimmune response initiated by the nucleus pulposus was also proposed as a possible cause for this inflammation and edema [10]. Literature shows that improvement in clinical symptoms is best correlated with a decrease in inflammation and swelling on the affected nerve root [2]. King [11] reported decreased need of narcotic analgesia in patients who received intravenous dexamethasone during surgery followed by intramuscular dexamethasone postoperatively for three days. Glasser et al. [8] divided their study into three groups. Group 1 received 160 mg intramuscular Depo-Medrol and 250 mg intravenous Solu-Medrol at the start of operation. A macerated fat graft soaked in 80 mg Depo-Medrol was placed over the affected nerve root after the discectomy. In addition, 30 ml of 0.25% bupivacaine was injected into the paraspinal muscles at the time of incision and also during closure. Group 2 also received the same systemic steroid injections and infiltration with 30 ml bupivacaine into the paraspinal muscles at both time points. However, in this group, a saline soaked fat graft was placed over the affected nerve root. Group 3 received neither corticosteroid nor bupivacaine and acted as a control group. They attained immediate and sustained benefits for one week after the operation by using intravascular and intramuscular steroids. Ersayli et al. [7] compared their study group, which was divided in four subgroups, with a control group. They infiltrated the operative site with 30 ml 0.25% bupivacaine and 40 mg of methylprednisolone or 30 ml 0.25% bupivacaine alone before the wound closure or before the incision. The control group was infiltrated with 30 ml of 0.9% NaCl before the wound closure. They showed significantly better results than the control group with bupivacaine alone or bupivacaine-methylprednisolone in study groups. However we should not forget that use of various combinations of different drugs at various stages of operation reduces the reliability of effect of agents and increases the chances of postoperative infections. Aminmansour et al. [1] showed that intraoperative injections of 40 mg dexamethasone could effectively reduce postoperative radicular leg pain and narcotics usage in patients with single-level herniated lumbar disc. They found that a higher dose of steroids is not more effective; however, intravenous administration of steroids was not effective in reducing back pain. All these articles clearly indicate that high dose of steroids is effective in reducing the inflammation and oedema of the affected nerve root. However, in our study, we have achieved significant relief in leg pain as well as back pain with local application of low dose methylprednisolone.
Debi et al. [6] put 80 mg of methylprednisolone-soaked collagen absorbable sponge in a study group and 2 ml saline-soaked collagen absorbable sponge in a control group over the affected nerve root after discectomy. They reported significant improvement in immediate postoperative back pain as well as leg pain. In this study we showed similar improvement in back pain as well as radicular leg pain with 40 mg of Depo-Medrol soaked absorbable Gelfoam for one month postoperatively. The difference was insignificant after one month. The second difference in our study was that we did not put Gelfoam or saline in the control group. Several other reports also suggested the efficacy of local or systemic steroids in the immediate postoperative period. In various studies [6, 9, 13, 14], saline or saline-soaked fat graft or absorbable gel was used in the control group and the effects were recorded. However in clinical practice we never inject saline or saline-soaked fat graft or Gelfoam if we do not intend to apply a local steroid or other agents. Therefore we decided to maintain our control group without any kind of injection or material. We believe this is the major difference in our study from most of the reported literature.
Lowell et al. [12] noted in their case report that use of epidural steroid after discectomy may predispose to infection. They hypothesised that the local immunosuppressive effect of methylprednisolone could be responsible for the infection. However, we did not observe any infection in either group. We believe that low doses of methylprednisolone can not produce infection if strict aseptic precautions, meticulous dissection, and prophylactic use of antibiotics are undertaken. Moreover, one report [9] suggested that presence of blood in the epidural space may interfere with the drug action and presence of a vacuum tube drain might lead to inadequate retention of the drug. We used a mini drain after the discectomy in all cases, but we do not think that it can decrease the amount of drug soaked by Gelfoam; instead it will drain the blood from the epidural space and reduce the chance of infection.
In conclusion we can say that local application of low dose Depo-Medrol reduces immediate postoperative back and leg pain effectively without any risk of infection. However, long-term effects were not observed to be more beneficial than in the control group. The immediate relief in symptoms helps patients with early mobilisation and resuming jobs early as well as shortening the hospital stay.
References
- 1.Aminmansour B, Khalili HA, Ahmadi J, Nourian M. Effect of high-dose intravenous dexamethasone on postlumbar discectomy pain. Spine. 2006;31(21):2415–2417. doi: 10.1097/01.brs.0000238668.49035.19. [DOI] [PubMed] [Google Scholar]
- 2.Berg A. Clinical and myelographic studies of conservatively treated cases of lumbar intervertebral disc protrusion. Acta Chir Scand. 1952;104(2–3):124–129. [PubMed] [Google Scholar]
- 3.Boutrand LS, Tadie M. Use of collagen based sealant to prevent in vivo epidural adhesions in an adult rat laminectomy model. J Neurosurg. 2001;94:61–67. doi: 10.3171/jns.2001.94.1.0061. [DOI] [PubMed] [Google Scholar]
- 4.Buttermann GR. Treatment of lumbar disc herniation: epidural steroid injection compared with discectomy. A prospective, randomized study. J Bone Joint Surg Am. 2004;86A(4):670–679. [PubMed] [Google Scholar]
- 5.Cherian MN, Mathews MP, Chandy MJ. Local wound infiltration with bupivacaine in lumbar laminectomy. Surg Neurol. 1997;47(2):120–122. doi: 10.1016/S0090-3019(96)00255-8. [DOI] [PubMed] [Google Scholar]
- 6.Debi R, Halperin N, Mirovsky Y. Local application of steroids following lumbar discectomy. J Spinal Disord Tech. 2002;15(4):273–276. doi: 10.1097/00024720-200208000-00002. [DOI] [PubMed] [Google Scholar]
- 7.Ersayli DT, Gurbet A, Bekar A, Uckunkaya N, Bilgin H. Effects of perioperatively administered bupivacaine and bupivacaine-methylprednisolone on pain after lumbar discectomy. Spine. 2006;31(19):2221–2226. doi: 10.1097/01.brs.0000232801.19965.a0. [DOI] [PubMed] [Google Scholar]
- 8.Glasser RS, Knego RS, Delashaw JB, Fessler RG. The perioperative use of corticosteroids and bupivacaine in the management of lumbar disc disease. J Neurosurg. 1993;78(3):383–387. doi: 10.3171/jns.1993.78.3.0383. [DOI] [PubMed] [Google Scholar]
- 9.Jirarattanaphochai K, Jung S, Thienthong S, Krisanaprakornkit W, Sumananont C. Peridural methylprednisolone and wound infiltration with bupivacaine for postoperative pain control after posterior lumbar spine surgery: a randomized double-blinded placebo-controlled trial. Spine 15. 2007;32(6):609–616. doi: 10.1097/01.brs.0000257541.91728.a1. [DOI] [PubMed] [Google Scholar]
- 10.Kawakami M, Tamaki T, Weinstein JN, Hashizume H, Nishi H, Meller ST. Pathomechanism of pain-related behavior produced by allografts of intervertebral disc in the rat. Spine. 1996;21(18):2101–2107. doi: 10.1097/00007632-199609150-00009. [DOI] [PubMed] [Google Scholar]
- 11.King JS. Dexamethasone–a helpful adjunct in management after lumbar discectomy. Neurosurgery. 1984;14(6):697–700. doi: 10.1097/00006123-198406000-00009. [DOI] [PubMed] [Google Scholar]
- 12.Lowell TD, Errico TJ, Eskenazi MS. Use of epidural steroids after discectomy may predispose to infection. Spine. 2000;25(4):516–519. doi: 10.1097/00007632-200002150-00020. [DOI] [PubMed] [Google Scholar]
- 13.Lundin A, Magnuson A, Axelsson K, Kogler H, Samuelsson L. The effect of perioperative corticosteroids on the outcome of microscopic lumbar disc surgery. Eur Spine J. 2003;12(6):625–630. doi: 10.1007/s00586-003-0554-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Mirzai H, Tekin I, Alincak H. Perioperative use of corticosteroid and bupivacaine combination in lumbar disc surgery: a randomized controlled trial. Spine. 2002;27(4):343–346. doi: 10.1097/00007632-200202150-00003. [DOI] [PubMed] [Google Scholar]
- 15.Mullen JB, Cook WA., Jr. Reduction of postoperative lumbar hemilaminectomy pain with Marcaine. Technical note. J Neurosurg. 1979;51(1):126–127. doi: 10.3171/jns.1979.51.1.0126. [DOI] [PubMed] [Google Scholar]
- 16.Murphy RW. Nerve roots and spinal nerves in degenerative disc disease. Clin Orthop. 1977;129:46–60. doi: 10.1097/00003086-197711000-00005. [DOI] [PubMed] [Google Scholar]
- 17.Nachemson A. Intradiscal measurements of pH in patients with lumbar rhinopathies. Acta Orthop Scand. 1969;40:23–42. doi: 10.3109/17453676908989482. [DOI] [PubMed] [Google Scholar]
- 18.Saal JS, Franson RC, Dobrow R, Saal JA, White AH, Goldthwaite N. High levels of inflammatory phospholipase A2 activity in lumbar disc herniations. Spine. 1990;15(7):674–678. doi: 10.1097/00007632-199007000-00011. [DOI] [PubMed] [Google Scholar]