Abstract
We retrospectively reviewed 68 hips in 62 patients with acetabular dysplasia who underwent curved periacetabular osteotomy. Among the 68 hips, 33 had acetabular retroversion (retroversion group) and 35 had anteversion (control group) preoperatively. All hips were evaluated according to the Harris hip score. Radiographic evaluations of acetabular retroversion and posterior wall deficiency were based on the cross-over sign and posterior wall sign, respectively. The clinical scores of the two groups at the final follow-up were similar. In the retroversion group, 12 hips had anteverted acetabulum postoperatively. The posterior wall sign disappeared in these hips, but remained in 21 hips with retroverted acetabulum postoperatively. Among the 21 hips with retroverted acetabulum, posterior osteoarthritis of the hip developed postoperatively in five hips. When performing corrective osteotomy for a dysplastic hip with acetabular retroversion, it is important to correct the acetabular retroversion to prevent posterior osteoarthritis of the hip due to posterior wall deficiency.
Résumé
Nous avons revu de façon rétrospective 68 hanches chez 62 patients présentant une dysplasie acétabulaire et ayant bénéficié d’une ostéotomie péri-acétabulaire. Parmi ces 68 hanches, 33 avaient en préopératoire une rétroversion acétabulaire (groupe rétroversion) et 35 une antéversion (groupe contrôle). Toutes les hanches ont été évaluées selon le score de Harris. L’évaluation radiographique de la rétroversion acétabulaire et du mur postérieur déficient ont été basées sur le signe du croisement et le signe du mur extérieur. Les scores cliniques des deux groupes au suivi final était semblable. Dans le groupe rétroversion, 12 hanches avaient antéversé leur acétabulum en post-opératoire le signe du mur postérieur disparaissant, mais celui-ci restant présent dans 21 hanches avec un acétabulum en rétroversion post-opératoire. Parmi les 21 hanches avec acétabulum rétroversé une coxarthrose postérieure s’est développée à 5 ans post-opératoire. Lorsque l’on réalise une correction par ostéotomie pour une hanche dysplasique avec un acétabulum rétroversé, il est important de corriger cette rétroversion de façon à prévenir une coxarthrose secondaire due à la déficience du mur postérieur.
Introduction
Developmental dysplasia of the hip is often associated with deficient anterior or global coverage of the femoral head [10] and is also associated with an increased prevalence of osteoarthritis [2, 17, 19]. It is generally thought that the responsible deficit is anterolateral and, therefore, any realignment procedures need to improve the anterior and lateral coverage.
Recently, acetabular retroversion, which can result from posterior wall deficiency or excessive anterior coverage, or both, has been described as a possible aetiological factor in osteoarthritis [1, 13, 16]. It has been reported that patients with acetabular dysplasia also exhibit a high frequency of acetabular retroversion. Specifically, one in six patients with acetabular dysplasia were reported to show acetabular retroversion, in which the superior one-third of the acetabulum faced posterolaterally [6].
The posterior aspect of the acetabulum is subjected to high loads during activities of daily living [12]. With acetabular retroversion, greater unit loads are theoretically imposed on the available posterior cartilage. Furthermore, a retroverted acetabulum can impinge between the anterior femoral neck and anterior edge of the acetabulum [1, 16]. Therefore, the recognition of acetabular retroversion is important when performing corrective osteotomy, such as periacetabular osteotomy. If this procedure for dysplastic hips with a retroverted acetabulum is carried out without recognition of the acetabular version and without correction of the retroversion, the postoperative clinical results may be affected.
The purposes of this study were to investigate the clinical and radiographic results in dysplastic hips with acetabular retroversion, and to compare the clinical outcomes between hips with acetabular anteversion and retroversion after periacetabular osteotomy.
Materials and methods
We retrospectively reviewed the radiographs of 256 hips in 220 consecutive patients with acetabular dysplasia who underwent curved periacetabular osteotomy [11] from August 1995 to March 2005. The surgical indications for curved periacetabular osteotomy included symptomatic acetabular dysplasia lasting longer than 5 months, a lateral centre-edge angle of Wiberg [19] (CE angle) of less than 16° on anteroposterior (AP) radiographs and the improvement of joint congruency on an AP radiograph in the abducted position. This type of osteotomy is not indicated for patients with aggravation of joint congruency in the abducted position. All surgical procedures were performed by the senior author (MN).
Of the initial 256 hips in 220 patients, 42 hips in 35 patients were excluded due to excessive pelvic tilt or pelvic asymmetry, which can obscure accurate interpretation of the radiographs. We further excluded 34 hips in 30 patients with Legg-Calve-Perthes disease or altered anatomy through severe osteoarthritis. In the remaining 180 hips in 155 patients, we found 33 hips in 30 patients (5 men and 25 women) with a retroverted acetabulum on an AP radiograph preoperatively (retroversion group). Among the remaining 147 hips in 125 patients with an anteverted acetabulum preoperatively, 35 hips in 32 patients (5 men and 27 women) were selected as controls (control group). The patients were matched for gender, age and preoperative extent of osteoarthritis according to the Tönnis classification [18]. Finally, a total of 68 hips in 62 patients who underwent curved periacetabular osteotomy by a single surgeon were included in this study.
Clinical evaluations
Clinical evaluations were performed preoperatively and at the latest follow-up using the Harris hip score. All clinical evaluations were performed by two of the authors (KS and TS), who were blinded to the radiographic results.
Radiographic evaluations
AP radiographs of the pelvis were taken with the patients in the supine position. The tube-to-film distance was 120 cm and the tube was oriented perpendicularly to the table. The central beam was directed towards the mid-point between the upper border of the symphysis and a horizontal line connecting the anterior superior iliac spines. The extent of the pelvic inclination was judged according to a previously described method [15]. The distance between the pubic symphysis and sacrococcygeal joint was measured on each standard AP radiograph for comparison with the reported control values of 25–40 mm for men and 40–55 mm for women [15]. If the distance between the pubic symphysis and sacrococcygeal joint did not lie within the corresponding range of control values, the patients were considered to have excessive pelvic inclination and were excluded from the evaluation of acetabular retroversion. Pelvic symmetry was evaluated in terms of the comparative radiographic appearance of the obturator formation and the positions of the sacral midpoint and pubic symphysis.
AP pelvic and false-profile lateral radiographs were taken for all patients preoperatively and at the latest follow-up. Radiographic evaluations were performed by measuring the CE angle [19], acetabular roof obliquity [7], acetabular head index [3] and anterior CE angle [5]. The severity of the secondary osteoarthrosis before the osteotomy was graded using the Tönnis classification system [18]. Specifically, hips with subchondral sclerosis were classified as Grade 1, hips with subchondral cyst formation and partial cartilage space narrowing were classified as Grade 2 and hips with severe or complete but localised cartilage space narrowing were classified as Grade 3. All radiographic measurements were taken three times on different occasions by two authors (KS and TS), who were blinded to the clinical results, and the average values were calculated.
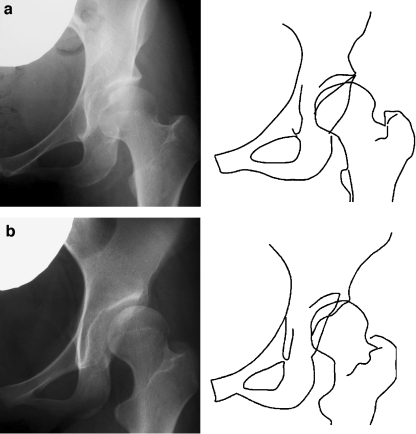
Acetabular version
In an anteverted acetabulum, a line can be drawn from the superolateral edge of the acetabulum that represents the anterior rim of the acetabulum, and is located medially and distally. A second line representing the posterior rim of the acetabulum can also be drawn, and is located more vertically (Fig. 1a). In a retroverted acetabulum, the superior part of the anterior line is actually lateral to the posterior line. As these lines progress medially and distally, the anterior line crosses the posterior line (Fig. 1b), and this finding is termed the cross-over sign [13]. The posterior line lies at or just lateral to the centre of the femoral head. If the line of the edge of the posterior wall is located medially to the centre of the femoral head, this finding is termed the posterior wall sign [13] and indicates relatively less posterior coverage [12].
Fig. 1.
a Anteroposterior (AP) radiograph of a patient with acetabular dysplasia and acetabular anteversion. The anterior line always runs medial to the posterior line. b AP radiograph of a patient with acetabular dysplasia and acetabular retroversion. The superior aspect of the anterior line is lateral to the posterior line, and the anterior and posterior lines cross each other at the proximal part of the acetabulum. The posterior line is medial to the centre of the femoral head, representing positive posterior wall sign
The Mann-Whitney U test was used to compare the corresponding clinical results and radiographic parameters between the retroversion and control groups, and the same parameters between hips with retroverted and anteverted acetabula after periacetabular osteotomy in the retroversion group. The Wilcoxon signed rank test was used to compare the changes in the clinical results and radiographic parameters in the retroversion group. The chi-square test was used to compare qualitative variables. Significance was defined as values of p<0.05.
Results
The preoperative and postoperative clinical scores in the two groups are presented in Table 1. The average Harris hip scores improved from 75.5 points (range, 60–93 points) preoperatively to 93.6 points (range, 80–100 points) at the latest follow-up in the retroversion group and from 74.2 points (range, 72–100 points) preoperatively to 94.1 points (range, 82–100 points) at the latest follow-up in the control group. The clinical scores of the two groups did not differ significantly (p=0.68). The radiographic measurements of the two groups are presented in Table 2. Postoperatively, the CE angle, acetabular roof obliquity, acetabular head index and anterior CE angle all showed improvement (p<0.0001, p<0.0001, p<0.0001 and p<0.0001, respectively) compared to their preoperative values in both groups. None of the radiographic parameters differed significantly between the two groups, with the exception of the preoperative anterior CE angle. The preoperative mean anterior CE angle in the retroversion group was significantly larger than that in the control group (p=0.015).
Table 1.
Patient data and clinical scores in the retroversion and control groups
| Retroversion group (33 hips) | Control group (35 hips) | Significance | |
|---|---|---|---|
| Gender (males: females) | 5:25 | 5:27 | NS |
| Age at surgery* (years) | 39.6±12.0 | 39.7±9.3 | NS |
| Duration of follow-up* (years) | 4.5±1.9 | 4.4±1.5 | NS |
| Tönnis classification (grade 1:2) | 14:19 | 14:21 | NS |
| Preoperative scores* | |||
| Overall | 75.5±11.6 | 74.2±10.3 | NS |
| Pain | 24.2±8.6 | 25.0±9.4 | NS |
| Function | 40.3±2.3 | 39.8±4.2 | NS |
| Follow-up scores* | |||
| Overall | 93.6±5.8 | 94.1±7.0 | NS |
| Pain | 40.6±4.7 | 40.9±4.4 | NS |
| Function | 44.1±8.2 | 46.9±9.3 | NS |
*Values are mean±standard deviation
Table 2.
Radiographic evaluation in the retroversion and control groups
| Parameters | Retroversion group (33 hips) | Control group (35 hips) | Significance |
|---|---|---|---|
| Preoperative evaluation* | |||
| Centre-edge angle (°) | 5.9±8.4 | 7.7±6.4 | NS |
| Acetabular roof obliquity (°) | 24.9±7.8 | 22.7±5.9 | NS |
| Acetabular head index (%) | 59.5±9.8 | 61.9±9.5 | NS |
| Anterior centre-edge angle (°) | 14.6±12.6 | 5.5±12.4 | p=0.015 |
| Latest follow-up evaluation* | |||
| Centre-edge angle (°) | 28.1±7.1 | 28.8±7.6 | NS |
| Acetabular roof obliquity (°) | 4.9±6.2 | 3.7±5.3 | NS |
| Acetabular head index (%) | 87.7±8.4 | 85.5±17.2 | NS |
| Anterior centre-edge angle (°) | 27.3±9.2 | 29.7±7.3 | NS |
| Postoperative acetabular version | |||
| Anteversion (no. of hips) | 12 | 11 | |
| Retroversion (no. of hips) | 21 | 24 | |
*Values are mean±standard deviation
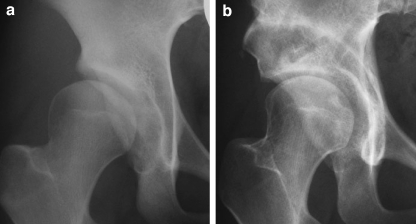
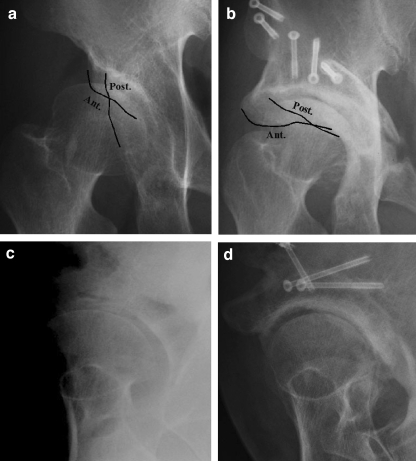
Preoperatively, the posterior wall sign was recognised in all hips in the retroversion group. In contrast, 17 of 35 hips (48%) in the control group had a negative posterior wall sign. Postoperatively, 12 of 33 hips (36%) in the retroversion group had an anteverted acetabulum and the remaining 21 hips had a retroverted acetabulum. The posterior wall sign disappeared in all 12 hips with an anteverted acetabulum (Fig. 2), but remained in all 21 hips with a retroverted acetabulum (Fig. 3). The average Harris hip score at the latest follow-up was higher (p=0.051) in the hips with an anteverted acetabulum than in those with a retroverted acetabulum (Table 3). In the control group, 11 of 35 hips (31%) had a retroverted acetabulum and the remaining 24 hips had an anteverted acetabulum postoperatively. The average Harris hip scores at the latest follow-up in the control group were similar between hips with an anteverted acetabulum and those with a retroverted acetabulum postoperatively (anteverted acetabulum: mean, 95.2 points, range, 82–100 points; retroverted acetabulum: mean, 93.5 points, range, 84–99 points; p=0.65).
Fig. 2.
a Preoperative AP radiograph of a 25-year-old woman showing acetabular dysplasia with acetabular retroversion and positive posterior wall sign. b AP radiograph taken 73 months postoperatively shows that the acetabular retroversion has been corrected. The posterior wall sign has disappeared in this hip. The patient had a Harris hip score of 99 points
Fig. 3.
a Preoperative AP radiograph of a 45-year-old man showing acetabular dysplasia with acetabular retroversion and positive posterior wall sign. b An AP radiograph taken 3 years postoperatively shows that the acetabular retroversion has not been corrected and the posterior wall sign is still present. c A preoperative false-profile view of the same hip shows no osteoarthritis of the posterior part. d A false-profile view taken 3 years postoperatively shows posterior wall deficiency and progressive osteoarthritis of the posterior part of the hip with cartilage space narrowing. The patient has a Harris hip score of 87 points
Table 3.
Comparison of the `results of hips with retroverted and hips with anteverted acetabulum
| Factor | Hips with retroverted acetabulum (12 hips) | Hips with anteverted acetabulum (21 hips) | Significance |
|---|---|---|---|
| Gender (males: females) | 2:10 | 3:15 | NS |
| Age at surgery* (years) | 39.2±14.6 | 41.7±9.7 | NS |
| Duration of follow-up* (years) | 4.7±2.0 | 4.4±1.9 | NS |
| Clinical results | |||
| Preoperative scores* | 75.1±12.3 | 75.8±11.4 | NS |
| Follow-up scores* | 91.2±5.8 | 95.1±2.4 | p=0.051 |
| Radiographic evaluation | |||
| Tönnis classification | |||
| Grade 1 (n=19) | 7 | 12 | NS |
| Grade 2 (n=14) | 5 | 9 | |
| Centre-edge angle | |||
| Preoperative* (°) | 6.3±7.3 | 5.4±9.2 | NS |
| Postoperative* (°) | 28.8±5.7 | 27.1±8.5 | NS |
| Anterior centre-edge angle | |||
| Preoperative* (°) | 14.2±13.3 | 15.3±12.7 | NS |
| Postoperative* (°) | 14.2±13.4 | 30.4±10.0 | p=0.043 |
*Values are mean±standard deviation
In 5 of 21 hips with a retroverted acetabulum after periacetabular osteotomy in the retroversion group, false-profile view radiographs revealed that osteoarthritis of the posterior part of the hip developed postoperatively (Fig. 3). This finding was also recognised in 2 of 11 hips with a retroverted acetabulum in the control group.
Discussion
Periacetabular osteotomy is currently established as an effective treatment for delaying and possibly preventing osteoarthritis of the dysplastic hip [4, 14]. Many factors that may affect the clinical outcomes can be identified preoperatively and postoperatively. Important factors include the degree of secondary osteoarthritis, severity of the acetabular dysplasia, severity of any associated femoral head deformity and sphericity of the joint surfaces [9]. The acetabular version may be another important factor affecting the clinical outcomes, since postoperative retroversion may cause anterior femoroacetabular impingement or posterior wall deficiency.
The recognition of retroversion is important when performing periacetabular osteotomy to correct dysplasia of the acetabulum. In most cases of acetabular dysplasia, the deficit is anterolateral and the surgeon, therefore, rotates the acetabular fragment forward and laterally. If this procedure were to be carried out indiscriminately for patients with developmental dysplasia and acetabular retroversion, the surgeon would make the retroversion larger. Therefore, in order to assess whether preoperative or postoperative acetabular retroversion influenced the clinical results, we compared the clinical outcomes between hips with retroverted and anteverted acetabula preoperatively, as well as the clinical outcomes between hips with retroverted and anteverted acetabula postoperatively after periacetabular osteotomy.
Our data indicate that preoperative acetabular retroversion did not influence the clinical results of periacetabular osteotomy when the acetabular retroversion was corrected to a neutral or anteverted acetabulum postoperatively. Furthermore, the postoperative acetabular version in the control group did not affect the clinical outcomes. However, among hips with preoperative acetabular retroversion, the mean clinical score of hips with a retroverted acetabulum postoperatively tended to be inferior to that of hips with an anteverted acetabulum postoperatively.
The posterior wall sign indicates relatively less posterior coverage. In our study, all hips with acetabular retroversion preoperatively had positive posterior wall sign, compared to 18 of 35 hips (51%) with acetabular anteversion. These results suggest that the posterior wall coverage of dysplastic hips with acetabular retroversion tends to be lower than that of dysplastic hips with acetabular anteversion. One of the reasons why the mean postoperative clinical score of hips with a retroverted acetabulum was inferior to those with an anteverted acetabulum in the retroversion group is considered to be that the posterior wall deficiency was not improved or deteriorated in these hips.
In a review of the literature, acetabular retroversion was reported to be present in 40 of 232 hips (17.2%) with developmental dysplasia [6], and this prevalence is almost the same as our findings (18.3%). In contrast, a separate study reported that acetabular retroversion was present in 87 of 235 hips (37%) with developmental dysplasia [8]. The latter study used different criteria to evaluate the pelvic tilt. Briefly, that study excluded patients in whom the tip of the coccyx was >2 cm from the superior border of the pubic symphysis, whereas we used the pelvic tilt evaluation criteria of Siebenrock et al. [7, 12]. Acetabular retroversion can be easily influenced by the inclination of the pelvis. Therefore, the prevalence of acetabular retroversion may be affected by differences in the methods used to evaluate the pelvic inclination.
A false-profile view may be useful for evaluating not only the anterior coverage of the femoral head, but also the posterior wall deficiency or articular surface of the posterior part of the hip after periacetabular osteotomy. In our study, the false-profile view revealed that osteoarthritis of the posterior part of the hip due to posterior wall deficiency developed postoperatively in seven hips with a retroverted acetabulum.
We note several limitations to our study. First, it involved only a small number of hips (68) and an even smaller number of hips with acetabular retroversion (33). Furthermore, the subgroups within the retroversion group contained yet smaller numbers, i.e. the subgroups showing anteverted and retroverted acetabula postoperatively consisted of 12 and 21 hips, respectively. Second, we could not evaluate the hips using computed tomography (CT) to determine the pre-postoperative acetabular version. Finally, the posterior wall sign is an easy and useful method for evaluating the posterior coverage of the acetabulum. However, when the femoral head migrates superolaterally due to acetabular dysplasia, this sign can more easily appear as a positive sign compared to hips without migration of the femoral head. Therefore, patients who had a false-positive posterior wall sign may be included in our study. In future studies, a method for the quantitative evaluation of the posterior coverage of the acetabulum is required.
In conclusion, retroversion of the acetabulum associated with acetabular dysplasia is more common than previously thought. The posterior wall coverage of dysplastic hips with acetabular retroversion tends to be lower than that of dysplastic hips with an anteverted acetabulum. Therefore, when corrective osteotomy is performed in patients with developmental dysplasia and a retroverted acetabulum, surgeons should transfer the osteotomised acetabulum in a posterolateral direction while simultaneously moving the femoral head medially to prevent osteoarthritis of the posterior part of the hip due to posterior wall deficiency.
Conflict of interest statement
Each author certifies that he or she has no commercial associations (e.g. consultancies, stock ownership, equity interest, patient/licensing arrangements etc.) that might pose a conflict of interest in connection with the submitted article.
Footnotes
Ethical review board statement Each author certifies that his or her institution has approved or waived approval for the human protocol for this investigation and that all investigations were conducted in conformity with ethical principles of research.
References
- 1.Ganz R, Parvizi J, Beck M, Leunig M, Nötzli H, Siebenrock KA. Femoroacetabular impingement: a cause for osteoarthritis of the hip. Clin Orthop Relat Res. 2003;417:112–120. doi: 10.1097/01.blo.0000096804.78689.c2. [DOI] [PubMed] [Google Scholar]
- 2.Harris WH. Etiology of osteoarthritis of the hip. Clin Orthop Relat Res. 1986;213:20–33. [PubMed] [Google Scholar]
- 3.Heyman CH, Herndon CH. Legg-Perthes disease: a method for the measurement of the roentgenographic result. J Bone Joint Surg Am. 1950;32:767–778. [PubMed] [Google Scholar]
- 4.Kleuver M, Kooijman MAP, Pavlov PW, Veth RPH. Triple osteotomy of the pelvis for acetabular dysplasia: results at 8 to 15 years. J Bone Joint Surg Br. 1997;79:225–229. doi: 10.1302/0301-620X.79B2.7167. [DOI] [PubMed] [Google Scholar]
- 5.Lequesne M, Seze S.La faux profil du basin: nouvelle incidence radiographique pour letude de la hanche Rev Rhum 196128643–652.14464207 [Google Scholar]
- 6.Li PL, Ganz R. Morphologic features of congenital acetabular dysplasia: one in six is retroverted. Clin Orthop Relat Res. 2003;416:245–253. doi: 10.1097/01.blo.0000081934.75404.36. [DOI] [PubMed] [Google Scholar]
- 7.Massie WK, Howorth MB. Congenital dislocation of the hip. Part 1. Method of grading results. J Bone Join Surg Am. 1950;32:519–531. [PubMed] [Google Scholar]
- 8.Mast JW, Brunner RL, Zebrack J. Recognizing acetabular version in the radiographic presentation of hip dysplasia. Clin Orthop Relat Res. 2004;418:48–53. doi: 10.1097/00003086-200401000-00009. [DOI] [PubMed] [Google Scholar]
- 9.Murphy SB, Deshmukh R. Periacetabular osteotomy: preoperative radiographic predictors of outcome. Clin Orthop Relat Res. 2002;405:168–174. doi: 10.1097/00003086-200212000-00021. [DOI] [PubMed] [Google Scholar]
- 10.Murphy SB, Kijewski PK, Millis MB, Harless A. Acetabular dysplasia in the adolescent and young adult. Clin Orthop Relat Res. 1990;261:214–223. [PubMed] [Google Scholar]
- 11.Naito M, Shiramizu K, Akiyoshi Y, Ezoe M, Nakamura Y. Curved periacetabular osteotomy for treatment of dysplastic hip. Clin Orthop Relat Res. 2005;433:129–135. doi: 10.1097/01.blo.0000153281.75265.1d. [DOI] [PubMed] [Google Scholar]
- 12.Pedersen DR, Brand RA, Davy DT. Pelvic muscle and acetabular contact forces during gait. J Biomech. 1997;30:959–965. doi: 10.1016/S0021-9290(97)00041-9. [DOI] [PubMed] [Google Scholar]
- 13.Reynolds D, Lucas J, Klaue K. Retroversion of the acetabulum. A cause of hip pain. J Bone Joint Surg Br. 1999;81:281–288. doi: 10.1302/0301-620X.81B2.8291. [DOI] [PubMed] [Google Scholar]
- 14.Schramm M, Pitto RP, Rohm E, Hohmann D. Long-term results of spherical acetabular osteotomy. J Bone Joint Surg Br. 1999;81:60–66. doi: 10.1302/0301-620X.81B1.8679. [DOI] [PubMed] [Google Scholar]
- 15.Siebenrock KA, Kalbermatten DF, Ganz R. Effect of pelvic tilt on acetabular retroversion: a study of pelves from cadavers. Clin Orthop Relat Res. 2003;407:241–248. doi: 10.1097/00003086-200302000-00033. [DOI] [PubMed] [Google Scholar]
- 16.Siebenrock KA, Schoeniger R, Ganz R. Anterior femoro-acetabular impingement due to acetabular retroversion. Treatment with periacetabular osteotomy. J Bone Joint Surg Am. 2003;85:278–286. doi: 10.2106/00004623-200302000-00015. [DOI] [PubMed] [Google Scholar]
- 17.Solomon L. Patterns of osteoarthritis of the hip. J Bone Joint Surg Br. 1976;58:176–183. doi: 10.1302/0301-620X.58B2.932079. [DOI] [PubMed] [Google Scholar]
- 18.Tönnis D. Congenital dysplasia and dislocation of the hip in children and adults. Berlin Heidelberg New York: Springer; 1987. [Google Scholar]
- 19.Wiberg G (1939) Studies on dysplastic acetabula and congenital subluxation of the hip joint. With special reference to the complication of osteoarthritis. Acta Chir Scand 83(Suppl 58)