Abstract
The aim of this study was to evaluate the clinical and radiological results in a group of patients who underwent aseptic revision hip arthroplasty using the cement within cement (CWC) technique. Between 1999 and 2005, 37 aseptic revision hip operations were performed. There were 30 women and five men, with an average age of 68 years. The reasons for revision were femoral stem fracture, cup failure, acetabular protrusion after hemi-arthroplasty and recurrent dislocation. At an average follow-up of 46 months, none of the patients required further femoral revision. The average post-operative Merle D’Aubigne score was 16.6 points (p<0.05). No evidence of radiological stem failure was observed and no femoral component was considered to be at risk for loosening. In this series of patients, the CWC technique provided consistent with high functional outcomes. This valid and effective alternative should be considered in carefully selected aseptic cases.
Résumé
Le but de cette étude est d’évaluer les résultats cliniques et radiologiques d’un groupe de patients ayant bénéficié de révisions pour descellement aseptique d’une prothèse totale de hanche en utilisant une technique cimentée ou non cimentée. Méthode: entre 1999 et 2005, 37 révisions aseptiques ont été réalisées chez 30 femmes et 5 hommes avec un âge moyen de 68 ans. L’origine de cette révision était fémorale (fracture de la pièce fémorale), faillite de la cupule, protusion acétabulaire après arthroplastie, luxations récidivantes. Résultats : après un suivi moyen de 46 mois aucun patient n’a nécessité une révision fémorale itérative. Le score post-opératoire de Merle d’Aubigné a été de 16,6 points (p<0.05). Il n’y avait pas de signe de faillite radiologique au niveau de la pièce fémorale, aucun composant fémoral n’était considéré comme étant à risques. En conclusion: dans cette série de patients la technique de cimentage permet de bénéficier d’un bon niveau fonctionnel. Il s’agit d’une alternative valable et effective qui doit être utilisée dans certains cas parfaitement sélectionnés.
Introduction
Total hip arthroplasty (THA) revision surgery is more demanding, takes a longer operative time and is associated with higher rates of complications in comparison with primary THA [25].
Complete removal of the old cement mantle, which, in some cases, remains intact, is technically difficult. This surgical step is often associated with a high incidence of complications, such as bone perforations, femur fractures and a decrease in the quantity and the quality of the cancellous bone, which is essential for the correct interdigitation of cement [5, 6, 9, 14]. We have previously reported a 20% incidence of intraoperative periprosthetic fractures during revision hip surgery, which was mainly associated with cement removal rather than with the reconstructive technique [10].
Eftekhar described the “in-cement” technique in 1978 for the revision of the femoral component, which is based on the preparation of the existing cement mantle prior to recementing a new femoral component [8]. From a biomechanical viewpoint, this technique was validated by studies reported by Greenwald et al. [12]. Although the method is about to turn 20 years old, the results of the cement within cement (CWC) technique have been described in the literature by few authors [17, 18, 20, 22].
The aim of our study was to evaluate the clinical and radiological results in a group of carefully selected patients who underwent aseptic revision hip arthroplasty, in which the CWC technique was used.
Patients and methods
We retrospectively reviewed a consecutive series of 38 patients with 40 aseptic revision hip operations that were done from April 1999 to May 2005 using the CWC technique. The study was approved by our institutional review board and the procedures followed were in accordance with the ethical standards of the responsible committee on human experimentation and with the Helsinki Declaration of 1975, as revised in 2000. During the study period, 428 revision operation using other techniques were performed by the authors. Three patients of the series in this study were lost to follow-up. Therefore, 37 revisions in 35 patients—30 women and five men—were evaluated. The mean age at revision surgery was 68 (range 29 to 68). Thirteen revisions were left-sided and 24 were right-sided. The mean pre-operative Merle D’Aubigne and Postel score [21] was 3.5 points (1 to 4) for pain, 2.3 (1 to 4) for mobility and 2.1 (1 to 3) for gait. The average time from the first operation to the revision surgery was 12 years.
Indications for the CWC technique only included cases presenting an intact femoral cement mantle. The reasons for revision are listed in Table 1. Patients with septic failures, damage to the femoral cement mantle or femoral radiolucencies, and femoral osteolysis were considered as contraindications for this technique.
Table 1.
Indications for the cement within cement (CWC) technique
| Indications | Number of cases |
|---|---|
| Femoral stem fracture | 2 |
| Cup failure | 20 |
| Hemiarthroplasty failure | 2 |
| Recurrent dislocation | 13 |
Surgical technique
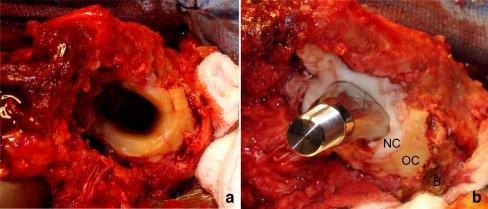
The operations were performed by three of the authors (M.B., F.C. and F.P.) in an operating room with laminar flow. The surgeons wore body-exhaust suits and all operations were performed using epidural hypotensive anaesthesia. A posterolateral approach without trochanteric osteotomy was used in 24 cases and a transtrochanteric approach in 13. Once the femoral component was removed, the cement mantle was examined in detail, confirming an intact cement–bone interface (Fig. 1).
Fig. 1.
A Cement mantle quality previous to re-cementing a new femoral component. B Intraoperative view depicting the implanted femoral component and the limits between calcar femoralis bone (B), the old (OC) and the new cement mantle (NC)
The superficial layer of the fixed and intact cement mantle was reamed with intermediate-speed blunt burrs of progressive diameters, creating a rough cavity within the old cement mantle, which was washed with a pulsatile spray to ensure a clean and dry surface.
One dose of CMW1 cement (DePuy®, Blackpool, England) was used in 31 cases and one dose of Simplex cement (Stryker Howmedica Osteonics®, Rutherford, NJ, USA) in six cases. A cement gun with a thin nozzle was used to inject the new cement in a state of low viscosity (liquid phase) to allow the insertion of the new femoral stem.
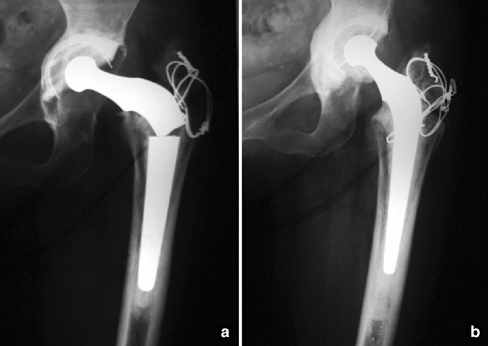
A Charnley stem (DePuy®, Leeds, England) was implanted in three cases, an Exeter femoral component (Stryker Howmedica Osteonics®, Rutherford, NJ, USA) in six cases and a C Stem femoral component (DePuy®, Warsaw, IN, USA) in 28 cases (Fig. 2).
Fig. 2.
A Anteroposterior radiograph of the right hip showing a Charnley femoral stem fracture with an undamaged cement mantle and an acetabular aseptic loosening. B Anteroposterior radiograph at 8 years follow-up of acetabular revision using impacted cancellous bone allografts and a CWC femoral technique
The rehabilitation protocol depended on the reason for revision, and included early mobilisation and walking with two crutches or a walker and partial weight-bearing on the involved side for 45 days. After that, and in the absence of pain, full weight-bearing was commenced.
Patients were evaluated clinically and radiographically by the authors using the Merle D’Aubigne and Postel functional score [21] at 15, 45 and 90 days postoperative, and then yearly thereafter. The last clinical and radiographic follow-up evaluation was performed by one of the authors.
Femoral radiolucencies and periprosthetic osteolysis, defined as bone loss in an area >5 mm2, were assessed in the zones described by Gruen et al. [13]. Radiographic evidence of femoral loosening was determined according to Harris and McGann’s criteria [15]. The orientation of the femoral component was determined by measuring the angle between a line that goes through the medullary axis of the femur and the axial axis of the femoral stem. Angles between 0° and 3° were considered as neutral, smaller than 0° as varus and greater than 3° as valgus. Subsidence was determined according to Loudon and Charnley [19].
Results
At a mean follow-up of 46 months (range 24 to 144), none of the patients required further femoral revision surgery. Following the D’Aubigne and Postel score [21], the post-operative average was 5.7 points for pain, 5.5 for mobility and 5.4 for gait (p<0.05).
There was no evidence of femoral radiolucencies, femoral loosening or periprosthetic osteolysis in any of the patients, according to the criteria described by Gruen et al. [13] and Harris and McGann [15], respectively.
None of the femoral stems showed more than 3 mm subsidence.
In relation to the femoral stem orientation, 59% of the components were observed in varus, 24% were inserted in valgus and 17% presented neutral angles.
Two patients developed an acetabular failure and required further acetabular surgery, for which the femoral CWC technique was used again. At final follow-up, they did not develop any other complications.
One patient developed a superficial infection of the wound. He was treated with surgical debridement with THA retention and intravenous antibiotic therapy, without evidence of infection or radiographic signs of loosening at the last follow-up.
Isolated dislocation occurred in two patients. One of these cases required an acetabular liner and femoral head revision, due to cup malposition and a damaged ceramic femoral head. The second patient was braced for two months and continued to be stable up to the last follow-up.
Discussion
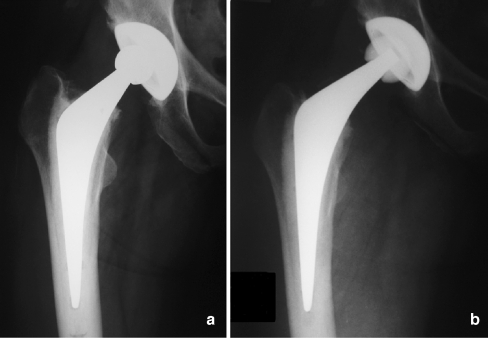
In this series of patients, the femoral CWC technique was used to treat several situations in revision hip surgery, thus, avoiding the removal of the previous cement mantle with favourable short- and medium-term results. This method may be recommended in a variety of situations, such as broken prosthetic components (Fig. 2a, b), acetabular failures in which the surgery is easier if the femoral component is taken out, conversion from a cemented hemiarthroplasty to a THA and recurrent dislocation (Fig. 3a, b) [17, 18, 20, 22].
Fig. 3.
A Anteroposterior radiograph of the right hip in a patient with recurrent dislocation and an intact femoral cement mantle. B Anteroposterior radiograph at 25 months follow-up after liner exchange from 22 to 28 mm and femoral revision to a higher offset using the CWC femoral technique
Although modern instruments, ultrasonic tools and techniques have been described to remove a stable polymethylmethacrylate mantle [11], complications and costs could be diminished by using the CWC technique.
It is important to note that the CWC technique was only used in patients presenting an intact distal femoral mantle without damage to the cement–bone interface verified in the pre-operative anteroposterior and lateral radiographs, and with meticulous intra-operative confirmation. This technique is contraindicated if patients present femoral osteolysis or radiolucencies in the cement–bone interface in the zones described by Gruen et al. [13].
The cement technique is a key factor in this method. In all the cases, a cement gun was used. It is necessary to use the cement in a liquid phase in order to help the new stem to be introduced properly and to obtain a correct filling of the distal femoral canal, with a suitable pressurisation of the polymethylmethacrylate.
We consider another important factor related to the success of this technique—use of polished stems. Although in three of these cases a matte Charnley stem was used, we have been using polished designs since 2001, and there is recent data acquired that is related to cement–bone interface protection with this surface finish [16]. Furthermore, in the eventual situation that further revision surgery is required, the absence of bonding between these stems and the polymethylmethacrylate could protect the cement mantle especially if stem removal is required. This was the situation in two patients that developed an acetabular failure and required further acetabular surgery.
Some authors have used this method for the treatment of septic failures. Quinlan et al. [22] have recently published a series of patients using the femoral CWC technique, including cases with prosthetic infection, reporting no clinical or radiographic failures. No cases of infection were included in our series, due to the fact that we consider retaining cement in septic cases could be related to persistent infection [2].
The use of ultrasound for the preparation of the cement mantle suggested by McCallum and Hozack [20] has been associated with the advantage of avoiding complications, such as bone perforations and femoral fractures. Nevertheless, the short period of treatment of their series does not allow us to make a suitable evaluation of the possible consequences of the ultrasound over the mechanical properties of the cement. In our series, no femoral perforations or intraoperative fractures were observed due to the fact that blunt instruments of progressive diameters with intermediate speed were used.
A high incidence of varus positioning of the femoral stem is one of our current concerns. In previous THA studies [3, 4, 7, 23], the varus orientation of the femoral stem has been related to poor results due to a thin cement mantle in the calcar region [24] or to an inadequate cement support in the distal portion of the implant [1]. We do not consider this fact to be a problem because we carefully selected patients presenting an intact cement mantle. The contact between the end of the stem and the cortical bone would not be possible.
Limitations of this study include a small number of patients, short-term follow-up and a lack of a control group of patients in whom revision surgery was performed with other methods.
In this series of patients, the CWC technique provided consistent and high-functional outcomes without revisions. This valid and effective alternative should be considered in carefully selected aseptic cases presenting a stable cement–bone interface. This technique was useful in many situations, including enhancing exposure when performing an acetabular revision and the revision of a stable nonmodular stem to improve offset and stability.
References
- 1.Bocco F, Langan P, Charnley J. Changes in the calcar femoris in relation to cement technology in total hip replacement. Clin Orthop Relat Res. 1977;128:287–295. [PubMed] [Google Scholar]
- 2.Buttaro M, Valentini R, Piccaluga F. Persistent infection associated with residual cement after resection arthroplasty of the hip. Acta Orthop Scand. 2004;75(4):427–429. [PubMed] [Google Scholar]
- 3.Callaghan JJ, Salvati EA, Pellicci PM, Wilson PD, Jr, Ranawat CS. Results of revision for mechanical failure after cemented total hip replacement, 1979 to 1982. A two to five-year follow-up. J Bone Joint Surg Am. 1985;67:1074–1085. [PubMed] [Google Scholar]
- 4.Coudane H, Fery A, Sommelet J, Lacoste J, Leduc P, Gaucher A. Aseptic loosening of cemented total arthroplasties of the hip in relation to positioning of the prosthesis. New utilization of the Tschuprow-Cramer statistical test. Acta Orthop Scand. 1981;52:201–205. doi: 10.3109/17453678108991782. [DOI] [PubMed] [Google Scholar]
- 5.Dennis DA, Dingman CA, Meglan DA, O’Leary JF, Mallory TH, Berme N. Femoral cement removal in revision total hip arthroplasty. A biomechanical analysis. Clin Orthop Relat Res. 1987;220:142–147. [PubMed] [Google Scholar]
- 6.Dohmae Y, Bechtold JE, Sherman RE, Puno RM, Gustilo RB. Reduction in cement–bone interface shear strength between primary and revision arthroplasty. Clin Orthop Relat Res. 1988;236:214–220. [PubMed] [Google Scholar]
- 7.Ebramzadeh E, Sarmiento A, McKellop HA, Llinas A, William G. The cement mantle in total hip arthroplasty. Analysis of long-term radiographic results. J Bone Joint Surg Am. 1994;76(1):77–87. doi: 10.2106/00004623-199401000-00010. [DOI] [PubMed] [Google Scholar]
- 8.Eftekhar NS. Principles of total hip arthroplasty. St. Louis: CV Mosby; 1978. [Google Scholar]
- 9.Eftekhar NS, Smith DM, Henry JH, Stinchfield FE. Revision arthroplasty using Charnley low friction arthroplasty technic. With reference to specifics of technic and comparison of results with primary low friction arthroplasty. Clin Orthop Relat Res. 1973;95:48–59. [PubMed] [Google Scholar]
- 10.Farfalli G, Buttaro M, Piccaluga F. Femoral fractures in revision hip surgeries with impacted bone allograft. Clin Orthop Relat Res. 2007;462:130–136. doi: 10.1097/BLO.0b013e318137968c. [DOI] [PubMed] [Google Scholar]
- 11.Gardiner R, Hozack WJ, Nelson C, Keating EM. Revision total hip arthroplasty using ultrasonically driven tools. A clinical evaluation. J Arthroplasty. 1993;8(5):517–521. doi: 10.1016/S0883-5403(06)80023-9. [DOI] [PubMed] [Google Scholar]
- 12.Greenwald AS, Narten NC, Wilde AH. Points in the technique of recementing in the revision of an implant arthroplasty. J Bone Joint Surg Br. 1978;60:107–110. doi: 10.1302/0301-620X.60B1.627570. [DOI] [PubMed] [Google Scholar]
- 13.Gruen TA, McNeice GM, Amstutz HC. “Modes of failure” of cemented stem-type femoral components: a radiographic analysis of loosening. Clin Orthop Relat Res. 1979;141:17–27. [PubMed] [Google Scholar]
- 14.Harris WH. Revision surgery for failed, nonseptic total hip arthroplasty: the femoral side. Clin Orthop Relat Res. 1982;170:8–20. [PubMed] [Google Scholar]
- 15.Harris WH, McGann WA. Loosening of the femoral component after use of the medullary-plug cementing technique. Follow-up note with a minimum five-year follow-up. J Bone Joint Surg Am. 1986;68:1064–1066. [PubMed] [Google Scholar]
- 16.Jewett BAJ, Collis DK. Radiographic failure patterns of polished cemented stems. Clin Orthop Relat Res. 2006;453:132–136. doi: 10.1097/01.blo.0000246540.64821.73. [DOI] [PubMed] [Google Scholar]
- 17.Li PL, Ingle PJ, Dowel JK. Cement-within-cement revision hip arthroplasty; should it be done? J Bone Joint Surg Br. 1996;78:809–811. [PubMed] [Google Scholar]
- 18.Lieberman JR, Moeckel BH, Evans BG, Salvati EA, Ranawat CS. Cement-within-cement revision hip arthroplasty. J Bone Joint Surg Br. 1993;75:869–871. doi: 10.1302/0301-620X.75B6.8245073. [DOI] [PubMed] [Google Scholar]
- 19.Loudon JR, Charnley J. Subsidence of the femoral prosthesis in total hip replacement in relation to the design of the stem. J Bone Joint Surg Br. 1980;62:450–453. doi: 10.1302/0301-620X.62B4.7430222. [DOI] [PubMed] [Google Scholar]
- 20.McCallum JD, 3rd, Hozack WJ. Recementing a femoral component into a stable cement mantle using ultrasonic tools. Clin Orthop Relat Res. 1995;319:232–237. [PubMed] [Google Scholar]
- 21.Merle D’Aubigne RM, Postel M. Functional results of hip arthroplasty with acrylic prosthesis. J Bone Joint Surg Am. 1954;36:451–475. [PubMed] [Google Scholar]
- 22.Quinlan JF, O’Shea K, Doyle F, Brady OH. In-cement technique for revision hip arthroplasty. J Bone Joint Surg Br. 2006;88:730–733. doi: 10.1302/0301-620X.88B6.17037. [DOI] [PubMed] [Google Scholar]
- 23.Søballe K, Christensen F. Calcar resorption after total hip arthroplasty. J Arthroplast. 1988;3:103–107. doi: 10.1016/S0883-5403(88)80074-3. [DOI] [PubMed] [Google Scholar]
- 24.Wejkner B, Wiege M. Correlation between radiologic and clinical findings in Charnley total hip replacement. A 10-year follow-up study. Acta Radiol. 1987;28:607–613. doi: 10.3109/02841858709177410. [DOI] [PubMed] [Google Scholar]
- 25.Zhan C, Kaczmarek R, Loyo-Berrios N, Sangl J, Bright RA. Incidence and short-term outcomes of primary and revision hip replacement in the United States. J Bone Joint Surg Am. 2007;89(3):526–533. doi: 10.2106/JBJS.F.00952. [DOI] [PubMed] [Google Scholar]