Abstract
Ninety-eight pilon fractures associated with ipsilateral distal fibular fracture were included in this study. The pilon fractures were treated by open reduction and plating. The 98 fractures were divided into three groups based on the treatment method of fractured fibula. Group A was composed of 50 fibular fractures treated by open reduction and plate fixation. Group B was composed of 23 fibular fractures treated by open reduction and pin fixation. Group C was composed of 25 fibular fractures treated conservatively by closed reduction. The radiographs were reviewed for adequacy of fracture reduction and posttraumatic arthrosis. At the end of follow-up, the clinical outcomes were evaluated using a rating scale. The three groups were similar in respect to Ruedi type, open fracture grade, and demographics (all p values >0.25). Group A showed a decreasing trend of malunion and ankle arthrosis compared to group C (p = 0.091 and p = 0.099, respectively). Group A had a better clinical outcome than group C (p = 0.008). In addition, group A showed an increasing trend of satisfactory outcome compared to group B (p = 0.096). In conclusion, for pilon fractures associated with ipsilateral fibular fractures, stabilisation of the fractured fibula plays an important role in the decrease of distal tibial malunion and post-traumatic ankle arthrosis as well as improvement of clinical outcomes.
Résumé
98 fractures du pilon tibial avec fracture du péroné ont été inclus dans cette étude. Les fractures du pilon tibial ont été traitées par réduction sanglante et ostéosynthèse par plaque. Les 98 fractures ont été divisées en 3 groupes selon les méthodes de traitement du péroné fracturé. Le groupe A était composé de 50 fractures du péroné traitées par réduction sanglante et plaque, le groupe B de 23 fractures du péroné traitées par réduction sanglante et fixations par broches et le groupe C de 25 fractures du péroné qui ont été réduites sans fixation. Les radiographies ont été analysées afin d’évaluer la réduction de la fracture et l’évolution vers une arthrose post-traumatique. A la fin du suivi, les trois groupes étaient identiques sur le plan clinique le type de Ruedi, le stade d’ouverture et les données démographiques. Le groupe A montrait un nombre moins important de pseudarthrose et d’arthrose de la cheville comparé au groupe C (p = 0,091, p = 0,099 respectivement). Le groupe A avait un meilleur résultat clinique que le groupe C (p = 0,008). De plus, le groupe A montrait une amélioration plus satisfaisante sur le devenir clinique à long terme que le groupe B (p = 0,096). En conclusion, les fractures du pilon tibial présentant une fracture associée du péroné doivent être stabilisées au niveau du tibia et au niveau du péroné par une ostéosynthèse par plaques de façon à diminuer le nombre de cals vicieux postraumatiques et d’améliorer les résultats cliniques.
Introduction
The pilon fracture is usually caused by a high-energy force which commonly produces an ipsilateral distal fibular fracture [2, 19]. For an optimal outcome of the displaced pilon fracture, most authors agreed that there should be adequate management of soft tissue, anatomical reduction of the joint, restoration of distal tibial alignment, and stabilisation of the fracture to facilitate union [3, 4, 14, 17, 19]. Stabilisation of the fractured fibula in the pilon fractures may play an important role on the clinical outcomes. However, only a few studies have mentioned the results of the pilon fractures associated with the fibular fractures. This situation inspired us to retrospectively follow-up and determine the clinical outcome of the pilon fractures with ipsilateral fibular fractures. It is the purpose of our study to compare the clinical results of these fibular fractures that were treated with plate or pin fixation, or nonoperation.
Patients and methods
Between 1990 and 2001, 198 consecutive tibial plafond (pilon) fractures were treated at an orthopaedic institution. Inclusion criteria for this study were (a) a displaced pilon fracture associated with an ipsilateral distal fibular fracture, (b) the pilon fracture treated by open reduction and plating, (c) fractured fibular treated with plate or pin fixation, or nonoperation, and (d) the ability to walk without assistance before injury. Exclusion criteria for this study were (a) bilateral pilon fractures, (b) patients with syndesmosis instability, (c) the requirement for intensive care or treatment in other departments, and (d) other fractures and operations on the same extremity. For example, a patient who had a concomitant tibial shaft fracture fixed by an intramedullary nail was excluded from this study. There were 119 patients who met the inclusion criteria. However, 21 patients could not be followed-up regularly due to death (two cases), amputation (two cases), or relocation (17 cases), and they were excluded. Therefore, 98 patients with an average age of 37.3 years were included in this study. All patients who were not able to participate in a personal examination were interviewed by telephone at an average follow-up period of six years (range two to ten years).
The 98 fractures were divided into three groups based on the treatment method of fractured fibula. Group A was composed of 50 fibular fractures treated by open reduction and plate fixation. The average age of these patients was 39.1 years. Thirty-six patients (72%) suffered from motor vehicle accidents. Group B was composed of 23 fibular fractures treated by open reduction and pin fixation. The average age of these patients was 36.5 years. Seventeen patients (73.9%) suffered from motor vehicle accidents. Group C was composed of 25 fibular fractures treated conservatively by closed reduction. The average age of these patients was 34.4 years. Nineteen patients (76%) suffered from motor vehicle accidents (Table 1).
Table 1.
The injury mechanism, Ruedi type, open fracture grade, and preoperative demographics in the three groups
| Group A | Group B | Group C | p value | |
|---|---|---|---|---|
| Gender (F/M) | 22/28 | 10/13 | 10/15 | >0.9 |
| Average age (years) | 39.1 | 36.5 | 34.4 | 0.45 |
| Vehicular trauma | 36 | 17 | 19 | >0.5 |
| Fall from a height | 10 | 4 | 3 | >0.5 |
| Other trauma | 4 | 2 | 3 | >0.6 |
| Ruedi I | 17 | 5 | 8 | >0.6 |
| Ruedi II | 23 | 14 | 11 | >0.6 |
| Ruedi III | 10 | 4 | 6 | >0.8 |
| Gustilo type I | 4 | 2 | 1 | >0.6 |
| Gustilo type II | 8 | 3 | 2 | >0.4 |
| Gustilo type III | 5 | 2 | 3 | >0.9 |
| Skin grafting | 1 | 0 | 1 | >0.9 |
| Local flap | 1 | 0 | 1 | >0.9 |
| Free flap | 2 | 1 | 1 | >0.9 |
| Bone graft | 5 | 2 | 2 | >0.9 |
| Preoperative undisplaced fibular fracture | 1 | 1 | 4 | p* |
| Marked displacement of fibular fracture | 45 | 19 | 19 | >0.16 |
| Average follow-up (months) | 69.4 | 73.5 | 76.2 | 0.252 |
* A vs. B, p = 0.53; B vs. C, p = 0.35; A vs. C, p = 0.04
A fibular fracture with >4 mm displacement on the preoperative radiographs was defined as a marked displacement. Less than 2 mm was defined as undisplaced. The pilon fractures were classified based on the Ruedi-Allgower classification [16]. Ruedi type I pilon fractures could be treated by internal fixation immediately. However, most Ruedi type II and III fractures were treated by delayed surgery after a period of one- to two-weeks traction until the swelling subsided. There were 68 closed (69.4%) and 30 open fractures (30.6%). Open fractures were categorised based on the Gustilo and Anderson classification. There were 17 open fractures in group A, seven in group B, and six in group C. An open fracture was treated by irrigation, thorough debridement, and appropriate intravenous antibiotics. The wound was approximated loosely or the exposed bone covered with a flap, according to the open type and condition of the soft tissue. Eight of 30 open fractures were classified as Gustilo grade IIIB (n = 6) or IIIC (n = 2) and were associated with severe soft tissue damage, which required skin grafting (n = 2), a local flap (n = 2), or a free flap (n = 4). In these fractures, a unilateral external fixator was temporarily used until the soft tissue was stabilised, as permitted by plating. Nine of 98 fractures (9.2%) were associated with extensive bone loss and required an autogenous bone graft (Table 1).
Plain films of all 98 patients were taken immediately postoperatively to evaluate reduction. A scale by McLennan and Ungersma [10] was used to grade the distal fibular reduction. Good reduction was defined as no fibula shortening, a posterior displacement less than 2 mm and less than a 1 mm increase in medial clear space. A fair reduction represented a fibula shortening of 2 mm, posterior displacement of 2–4 mm, and a 1–3 mm increase in the medial clear space. A poor reduction was defined as a fibula shortening in excess of 2 mm, posterior displacement of over 4 mm, and a greater than 3 mm increase in medial clear space. We evaluated the adequacy of pilon fracture reduction using a scale described by Conroy et al. [5]. According to their criteria, an excellent reduction was defined as <2 mm of joint incongruity and <5° of varus/valgus metaphyseal-diaphyseal angulation. A good reduction was regarded as 2–5 mm of joint incongruity or fracture plane separation and 5–10° of varus/valgus metaphyseal-diaphyseal angulation. A poor reduction evaluation was given for >5 mm of joint incongruity and >10° of varus/valgus metaphyseal-diaphyseal angulation. An adequate reduction included excellent and good reductions. We defined the distal tibial malunion as fractured healing with angulation of 10° or more in any plane, or internal rotation of 10° or more, external rotation of more than 15°, or tibial shortening of 2 cm or more. Nonunion was defined as no evidence of healing after six months. Ankle arthrosis was considered with >1/2 joint space narrowing and sclerotic change on the radiographs.
At the end of follow-up, we evaluated the results according to the rating scale of Teeny and Wiss [18]. In this system, the subjective and objective clinical data are evaluated, with the maximum score being 100 points, including pain, walking distance, supports or orthosis requirement, running ability, toe raising, hills up or down, stairs up or down, limping or not, plantar range of motion of the ankles, dorsal range of motion, and swelling. An overall score of 93–100 points was ranked as excellent, 87–92 points as good, 65–86 points as fair, and 0–64 as poor. We defined excellent and good results as a satisfactory outcome. Fair and poor results were considered an unsatisfactory outcome.
The chi-square test with Yates’ correction, Fisher’s exact test, and one-way ANOVA with post-hoc test were used to compare the three groups. SPSS 10.0 statistical software (SPSS Inc., Chicago, IL, USA) was used to analyse the data; p values below 0.05 were considered significant.
Results
The three groups were similar with respect to injury mechanisms, Ruedi type, open fracture grade, average follow-up period, and demographics (all p values >0.25). However, preoperatively, the rate of undisplaced fibular fracture in group C was higher than in group A (p = 0.04) (Table 1).
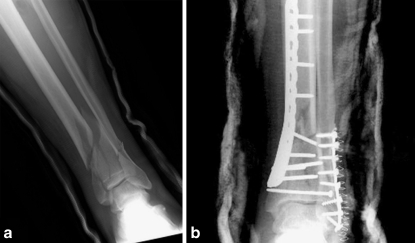
Evaluation of immediately postoperative roentgenograms revealed 84 of 98 (85.7%) patients with good reduction of the fibular fractures (Fig. 1). The good reduction rate of fibular fracture in group A was higher than group B or C (p < 0.05). Adequate reduction of the pilon fractures were seen in 89 of 98 (90.1%) patients. The adequate reduction rate of pilon fracture showed no significant difference among the three groups (92% vs. 91.3% vs. 88%, all p values >0.05). However, group A had an 88% (44 cases) satisfactory outcome, according to the rating scale of Teeny and Wiss. Group B had a 69.6% (16 cases) satisfactory outcome. Group C had a 60% (15 cases) satisfactory outcome. Operative fixation of the fractured fibula with a tubular plate (group A) resulted in a better outcome than nonoperative treatment (group C) (p = 0.008). In addition, group A showed a trend of increasing satisfactory outcome compared to group B, although this was not statistically significant (Fisher’s exact test, p = 0.096). At the end of follow-up, the post-traumatic arthrosis rate was 16% in group A (eight cases), 26.1% in group B (six cases), and 32% in group C (eight cases). Group A showed a trend of lower post-traumatic arthrosis rate compared to group C, although this was not significant (Fisher’s exact test, p = 0.099) (Table 2).
Fig. 1.
A 34-year-old man sustained a left pilon fracture with ipsilateral distal fibular fracture. The distal tibial and fibular fractures that were treated with plate fixation achieved adequate reduction. a Preoperative anteroposterior view shows the Ruedi type II pilon fracture with displaced distal fibular fracture. b Immediately postoperative X-ray shows excellent reduction of the pilon fracture and good reduction of the fibular fracture
Table 2.
Reduction rate, clinical results, and complications in the three groups
| A | B | C | p | |
|---|---|---|---|---|
| Good fibular reduction | 49 (98%) | 19 (82.6%) | 16 (64%) | p* |
| Adequate reduction of pilon fractures | 46 (92%) | 21 (91.3%) | 22 (88%) | >0.9 |
| Satisfactory outcome | 44 (88%) | 16 (69.6%) | 15 (60%) | p** |
| Posttraumatic arthrosis | 8 (16%) | 6 (26.1%) | 8 (32%) | p*** |
| Superficial infection | 2 (4%) | 1 (4.3%) | 1 (4%) | >0.9 |
| Deep infection | 2 (4%) | 1 (4.3%) | 0 | >0.9 |
| Nonunion | 2 (4%) | 1 (4.3%) | 1 (4%) | >0.9 |
| Skin slough | 6 (12%) | 2 (8.7%) | 3 (12%) | >0.9 |
| Malunion | 2 (4%) | 3 (13%) | 4 (16%) | p**** |
* A vs. B, p = 0.032; B vs. C, p = 0.2; A vs. C, p < 0.001
** A vs. B, p = 0.096; B vs. C, p = 0.56; A vs. C, p = 0.008
*** A vs. B, p = 0.24; B vs. C, p = 0.76; A vs. C, p = 0.099
**** A vs. B, p = 0.317; B vs. C, p = 1.0; A vs. C, p = 0.091
There were 31 (31.6%) complications in our series, including four (4.1%) superficial infections, three (3.1%) deep infections, four (4.1%) nonunions, 11 (11.2%) skin sloughs, and nine (9.2%) distal tibial malunions. The three groups were similar with respect to superficial infections, deep infections, nonunions, and skin sloughs. However, group C (n = 4, 16%) showed a trend of higher rate of distal tibial malunion than group A (n = 2, 4%) (p = 0.091) (Table 2). Concerning infection management, superficial infections were treated with oral antibiotics and deep infections were treated with repeated debridement and an intravenous administration of antibiotics (four to six weeks). Eventually, two cases (2%) developed osteomyelitis that was treated by implant removal, repeated debridement, and intravenous administration of antibiotics. After one- to two-years treatment, there was no evidence of infective signs at the last follow-up. With respect to nonunion, although all fractures achieved bone healing after undergoing secondary surgery with an autogenous bone graft, only one patient (25%) had satisfactory clinical outcome. Most of them had ankle stiffness and incapacitating pain during their daily activities.
Discussion
Fractures of the distal tibial plafond pose a treatment challenge for the orthopaedic surgeon [1, 7, 9, 12, 17]. In 1969, Ruedi and Allgower [15] reported 74% excellent or good results when they reviewed 84 pilon fractures treated with ORIF. Previous studies have demonstrated significant differences in outcomes based on the clinical characteristics of the fracture types [9, 18]. In our study, 75 of 98 (76.5%) pilon fractures associated with ipsilateral fibular fractures achieved satisfactory clinical outcome. However, different clinical outcomes were based on the treatment methods of the fractured fibula. Group A had a better outcome than group C (88% vs. 60%). Group B showed a trend of decreasing satisfactory outcome compared to group A (69.6% vs. 88%).
Preoperatively, the rate of undisplaced fibular fracture in group C was higher than in group A. This might be a selection bias because some surgeons thought that undisplaced fibular fracture could be treated conservatively. Postoperatively, the good reduction rate of fibular fracture in group A was higher than in groups B and C (p < 0.05). Nonoperative treatment resulted in the lowest good reduction rate due to difficult restoration of the fibular alignment though a closed reduction. In addition, we determined that a plate used in a fibular fracture could achieve stable fixation in contrast to a pin fixation which runs the risk of poor control of fragment rotation. Furthermore, stable fixation of the fractured fibula in the pilon fracture might help the maintenance of distal tibial alignment. This might explain why group A showed a trend of lower rate of distal tibial malunion than group C (p = 0.091).
In previous studies, most authors agree that the distal fibula plays the key role in the stability of the ankles because 1 mm lateral displacement of the talus decreases the tibiotalar contact surface by 42% [8, 13]. As we know, ankle instability increases the risk of tibiotalar arthrosis. In our study, group A showed a trend of lower post-traumatic arthrosis rate compared to group C (p = 0.099). We concluded that rigid fixation of the fractured fibula in the pilon fracture provided strong ankle stability and should decrease the ankle arthrosis.
In our study, the infection rate showed no difference among the three groups. The total deep infection and osteomyelitis rates were low, at 3.1% and 2.0%, respectively. Other authors have reported various infection rates. Sirkin et al. [17] published an infection rate of 5.3%. Ovadia and Beals [11] reported a rate of osteomyelitis of 7%. All of the above series included both open and closed pilon fractures. The low infection rate in our series was due to multiple factors, including adequate debridement, early skeletal stabilisation, and subsequent obliteration of the dead space by a healthy, well-vascularised flap. Poor soft tissue healing with skin slough was common, ranging from 11% to 27% [11, 18]. As a result, surgeons began searching for a solution to the soft tissue problem. Helfet et al. [6] were able to decrease wound complications in patients treated with ORIF by delaying surgery until the soft tissue stabilised. In our study, although most pilon fractures were treated by delayed surgery, the skin slough rate was up to 11.2%. This problem might be attributed to the pilon fractures treated with medial plating that can increase skin tension. However, the treatment method of the fractured fibula (lateral plating, pinning, or nonoperation) did not affect the skin slough rate (p > 0.05).
Our study had various limitations. First, it was a retrospective study and could produce a selection bias. Second, several important factors affected the results of pilon fractures such as fracture patterns, quality of articular reduction, and severity of soft tissue injury. Our study could not control all of these variations well. Third, this study was performed in a teaching institution where the resident was the operating surgeon and the surgeons’ level of experience could influence the outcomes. And fourth, the study was not a large series and when we calculated the power of this study, most were only 80–90%. If the null hypothesis (no difference between the groups) was accepted in our study, the false-negative rate was up to 10–20%.
In conclusion, for pilon fractures associated with ipsilateral fibular fractures, operative fixation of the fractured fibula with a plate had a better outcome than nonoperative treatment. Stabilisation of the fractured fibula seemed to play an important role in the decrease of distal tibial malunion and post-traumatic ankle arthrosis, and improvement of clinical outcomes.
References
- 1.Ayeni JP. Pilon fractures of the tibia: a study based on 19 cases. Injury. 1988;19:109–114. doi: 10.1016/0020-1383(88)90085-X. [DOI] [PubMed] [Google Scholar]
- 2.Barei DP, Nork SE, Bellabarba C, et al. Is the absence of an ipsilateral fibular fracture predictive of increased radiographic tibial pilon fracture severity? J Orthop Trauma. 2006;20(1):6–10. doi: 10.1097/01.bot.0000189589.94524.ff. [DOI] [PubMed] [Google Scholar]
- 3.Bourne RB. Pilon fractures of the distal tibia. Clin Orthop. 1989;240:42–46. [PubMed] [Google Scholar]
- 4.Chen SH, Wu PH, Lee YS. Long-term results of pilon fractures. Arch Orthop Trauma Surg. 2007;127(1):55–60. doi: 10.1007/s00402-006-0225-3. [DOI] [PubMed] [Google Scholar]
- 5.Conroy J, Agarwal M, Giannoudis PV, et al. Early internal fixation and soft tissue cover of severe open tibial pilon fractures. Int Orthop. 2003;27:343–347. doi: 10.1007/s00264-003-0486-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Helfet DL, Koval K, Pappas J, et al. Intra-articular “pilon” fracture of the tibia. Clin Orthop. 1994;298:221–228. [PubMed] [Google Scholar]
- 7.Leonard M, Magill P, Khayyat G (2008) Minimally-invasive treatment of high velocity intra-articular fractures of the distal tibia. Int Orthop Jul 25. [Epub ahead of print] [DOI] [PMC free article] [PubMed]
- 8.Lee YS, Huang HL, Lo TY, et al. Lateral fixation of AO type-B2 ankle fractures in the elderly: the Knowles pin versus the plate. Int Orthop. 2007;31:817–821. doi: 10.1007/s00264-006-0260-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Leung F, Kwok HY, Pun TS, et al. Limited open reduction and Ilizarov external fixation in the treatment of distal tibial fractures. Injury. 2004;35:278–283. doi: 10.1016/S0020-1383(03)00172-4. [DOI] [PubMed] [Google Scholar]
- 10.Mclennan JG, Ungersma JA. A new approach to the treatment of ankle fractures. Clin Orthop. 1986;213:125–136. [PubMed] [Google Scholar]
- 11.Ovadia DN, Beals RK. Fractures of the tibial plafond. J Bone Joint Surg Am. 1986;68:543–551. [PubMed] [Google Scholar]
- 12.Patterson MJ, Cole JD. Two-staged delayed open reduction and internal fixation of severe pilon fractures. J Orthop Trauma. 1999;13:85–91. doi: 10.1097/00005131-199902000-00003. [DOI] [PubMed] [Google Scholar]
- 13.Phillips WA, Schwartz HS, Keller CS, et al. A prospective randomized study of the management of severe ankle fractures. J Bone Joint Surg Am. 1985;67:67–78. [PubMed] [Google Scholar]
- 14.Pollak AN, McCarthy ML, Bess RS, et al. Outcomes after treatment of high-energy tibial plafond fractures. J Bone Joint Surg Am. 2003;85:1893–1900. doi: 10.2106/00004623-200310000-00005. [DOI] [PubMed] [Google Scholar]
- 15.Ruedi TP, Allgower M. Fractures of the lower end of the tibia into the ankle joint. Injury. 1969;1:92–99. doi: 10.1016/S0020-1383(69)80066-5. [DOI] [Google Scholar]
- 16.Ruedi TP, Allgower M. The operative treatment of intra-articular fractures of the lower end of the tibia. Clin Orthop. 1979;138:105–110. [PubMed] [Google Scholar]
- 17.Sirkin M, Sanders R, DiPasquale T, et al. A staged protocol for soft tissue management in the treatment of complex pilon fractures. J Orthop Trauma. 2004;18(8 suppl):S32–S38. doi: 10.1097/00005131-200409001-00005. [DOI] [PubMed] [Google Scholar]
- 18.Teeny SM, Wiss DA. Open reduction and internal fixation of tibial plafond fractures. Clin Orthop. 1993;292:108–117. [PubMed] [Google Scholar]
- 19.Topliss CJ, Jackson M, Atkins RM. Anatomy of pilon fractures of the distal tibia. J Bone Joint Surg Br. 2005;87:692–697. doi: 10.1302/0301-620X.87B5.15982. [DOI] [PubMed] [Google Scholar]