Abstract
The aim of this study was to analyse the complication rates of six different shoulder arthroplasty concepts for different diagnoses in the short and midterm. The study included 485 primary shoulder arthroplasties. The mean follow-up of the cohort was 3.5 (1–10) years. Complications were classified into three categories: (1) without reoperation, (2) soft tissue revision and (3) implant revision. In total, 56 complications were recorded (11.6%): 34 (7%) were category 1 complications, 11 (2.3%) were category 2 and 11 (2.3%) were category 3. For the whole cohort the median follow-up was 1.6 years (1–10 years) and the survival rate without any complication was 90.5% (95% CI: 87.9–93.1). Patients rated the result of their surgery in 270 (55.7%) cases as very satisfied, in 148 (30.5%) as satisfied, in 43 (8.9%) as somewhat disappointed and in 24 (4.9%) as disappointed. A relatively low complication rate was found in this study. Long-term observations are necessary to confirm these results.
Introduction
The number of shoulder arthroplasties performed in cases of primary and secondary degenerative joint disease and fractures of the proximal humerus has continually increased in the past [4]. In the last decade surgical techniques, treatment options and implant design have been refined [14]. Moreover, the mean age of patients undergoing shoulder arthroplasty is lower than those receiving total hip and knee arthroplasty [31, 35]. Concern has been expressed about the elevated complication rate in hip, knee and shoulder arthroplasty in younger patients [15, 21, 31, 32]. The knowledge of possible complication and survival rates and outcomes of different implants and treatment options for a specific type of surgery is fundamental for orthopaedic surgeons when offering their advice to patients before major joint replacements. In the current literature different complication rates for multiple shoulder implant concepts have been described in single studies but have rarely been specifically addressed [4, 35]. Therefore, the aim of this single-centre study was to analyse the complication rates of primary shoulder arthroplasties treated with six different implant concepts and diagnoses using a prospective database.
Materials and methods
Between April 1997 and December 2006, 571 primary and revision shoulder arthroplasties were performed at our institution. All patients were included in a prospective database. Of these, 535 shoulders in 497 patients received a primary shoulder arthroplasty; 50 patients (9.4%) were lost to follow-up. Therefore, 485 shoulders were included in our study. Eleven patients (2%) died from causes unrelated to the surgery during the follow-up period, but a follow-up examination (minimum of one year after arthroplasty) was available in all cases. The study was reviewed by the local Ethics Committee and written consent was obtained from all patients before surgery. Inclusion criteria were: (1) all patients treated with a primary shoulder arthroplasty at our institution during the above-mentioned time period and (2) a minimum follow-up of one year. There were 352 women and 133 men. The dominant shoulder was involved in 325 cases. The mean age at the time of arthroplasty was 67 years (range: 20–96 years).
The mean follow-up of the whole cohort was 3.5 years (range: 1–10 years; median: 1.6 years); 212 shoulders were followed up for one to two years, 150 were followed for two to five years and 123 were followed for five to 11 years.
Six different types of implants were used. Table 1 shows the assignment of implants and diagnoses. There were 104 previous surgical procedures on the affected shoulders. Thirty-two shoulders had more than one procedure.
Table 1.
Assignment of diagnoses and implants used
| Diagnosis | Total shoulder (n) | Hemiarthroplasty (n) | Resurfacing arthroplasty (n) | Fracture implant (n) | Reversed implant (n) | Bipolar implant (n) | Total | % |
|---|---|---|---|---|---|---|---|---|
| OA | 148 | 23 | 38 | 0 | 0 | 1 | 210 | 43.3 |
| Fracture | 0 | 27 | 0 | 59 | 0 | 0 | 86 | 17.7 |
| PA | 12 | 29 | 18 | 11 | 6 | 2 | 78 | 16.1 |
| CTA | 0 | 12 | 9 | 0 | 39 | 8 | 68 | 14 |
| AVN | 10 | 8 | 8 | 0 | 0 | 0 | 26 | 5.4 |
| RA | 7 | 2 | 1 | 0 | 4 | 3 | 17 | 3.5 |
| Total | 177 | 101 | 74 | 70 | 49 | 14 | 485 | |
| % | 36.5 | 20.8 | 15.3 | 14.4 | 10.1 | 2.9 | 100 |
OA osteoarthritis, PA post-traumatic arthritis, CTA cuff tear arthropathy, AVN avascular necrosis, RA rheumatoid arthritis
The subjective result after surgery was rated in categories of “very satisfied”, “satisfied”, “somewhat disappointed” or “very disappointed”.
Operative technique and implants
In most cases a deltopectoral approach was used as described by Neer. For cases treated with a reversed implant, a superior approach was used.
For hemiarthroplasty and total shoulder arthroplasty a third-generation humeral component with a modular stem, eccentric heads and variable head inclination was used (Aequalis® Shoulder and Aequalis® Total Shoulder, Tornier, St. Ismier Cedex, France). In all but 11 cases the humeral component was cemented. All glenoid components (Aequalis® Total Shoulder) were cemented. In 137 cases a concave keeled glenoid and in 40 cases a flat-back glenoid was used.
For humeral head resurfacing the Copeland Shoulder was used in 29 cases (Biomet Europe, Dordrecht, The Netherlands) and in 45 cases the Epoca RH® Cup (Argomedical, Cham, Switzerland) was used.
A third-generation fracture implant (Aequalis® Fracture Shoulder, Tornier, St. Ismier Cedex, France) was used. In all cases the stem was cemented and combined with eccentric heads.
The humeral stem of the reversed implant (Aequalis® Reversed Shoulder, Tornier, St. Ismier Cedex, France) was cemented in all cases. The glenoid component had a press-fit design and was fixed with four screws.
The stem of the Bipolar implant (Bio-Modular Shoulder, Biomet Europe, Dordrecht, The Netherlands) was cemented in all cases.
Classification of complications
All intra- and postoperative complications were recorded in the prospective database. The number and severity of complications were reviewed and classified using the following three categories:
Complications without reoperation/intraoperative complications
Temporary or permanent nerve palsy, intra- or postoperative fractures of the humerus or glenoid, rotator cuff tears, temporary dislocation of the glenohumeral joint, relevant intraoperative bleeding and implant instability
Complications with soft tissue revision
Recurrent dislocation of the glenohumeral joint, wound infection, painful biceps tendinitis and contracture of the shoulder joint
Complications with implant revision
Painful glenoid erosion, infection, malpositioning of the implant and implant loosening
Statistics
Estimates of implant survival were calculated by the Kaplan-Meier method for the whole cohort, different types of complications, diagnosis and implants.
Ethics
The study protocol was approved by the Ethics Committee of the local university (number S-305/2007) and informed consent was obtained from all patients included.
Results
In total, 56 complications in 485 shoulder arthroplasties were recorded (11.6%). Of these, 34 (7%) were category 1 complications, 11 (2.3%) were category 2 and 11 (2.3%) were category 3. The types and severity of the complications are shown in Table 2. The overall complication rates for each implant concept and each diagnosis are illustrated in Table 3.
Table 2.
Types and severity of complications: categories 1–3
| Total shoulder (n) | Hemiarthroplasty (n) | Resurfacing arthroplasty (n) | Fracture implant (n) | Reversed implant (n) | Bipolar implant (n) | Total | % | |
|---|---|---|---|---|---|---|---|---|
| Category 1 | ||||||||
| Temporary nerve palsy | 3 | 1 | 1 | 5 | 1.1 | |||
| Permanent nerve palsy | 2 | 2 | 2 | 6 | 1.3 | |||
| Dislocation | 1 | 1 | 2 | 1 | 1 | 6 | 1.3 | |
| Rotator cuff tear | 3 | 1 | 4 | 0.9 | ||||
| Humeral fracture, intraop. | 3 | 1 | 4 | 0.9 | ||||
| Humeral fracture, postop. | 3 | 1 | 4 | 0.9 | ||||
| Bleeding | 2 | 2 | 0.5 | |||||
| Implant malpositioning | 1 | 1 | 1 | 3 | 0.7 | |||
| Total | 15 | 9 | 3 | 3 | 3 | 1 | 34 | 7 |
| % | 8.5 | 8.9 | 4.1 | 4.3 | 6.1 | 7.1 | ||
| Category 2 | ||||||||
| Infection | 1 | 1 | 1 | 1 | 4 | 0.9 | ||
| Stabilisation after dislocation | 2 | 1 | 2 | 5 | 1.1 | |||
| Arthrolysis | 1 | 1 | 0.3 | |||||
| Tenotomy of biceps tendon | 1 | 1 | 0.3 | |||||
| Total | 4 | 1 | 3 | 1 | 2 | 11 | 2.3 | |
| % | 2.3 | 1 | 4.1 | 1.4 | 4.1 | |||
| Category 3 | ||||||||
| Glenoid erosion with pain | 1 | 4 | 5 | 1.1 | ||||
| Dislocation | 2 | 1 | 0.6 | |||||
| Infection | 1 | 1 | 0.3 | |||||
| Periprosthetic fracture | 1 | 1 | 0.3 | |||||
| Inadequate positioning | 2 | 2 | 0.5 | |||||
| Total | 3 | 4 | 2 | 2 | 11 | 2.3 | ||
| % | 3 | 5.4 | 2.9 | 4.1 |
Table 3.
Overall complication rates
| Implant concepts | |||||||
| Categories 1, 2 and 3 | Total shoulder | Hemiarthroplasty | Resurfacing arthroplasty | Fracture implant | Reversed implant | Bipolar implant | Overall |
| n | 19 | 13 | 10 | 6 | 7 | 1 | 56 |
| % | 10.7 | 11.2 | 13.5 | 8.6 | 14.3 | 7.1 | 11.6 |
| Diagnosis | |||||||
| Categories 1, 2 and 3 | Humeral head fracture | Post-traumatic arthritis | Rheumatoid arthritis | Osteoarthritis | Cuff tear arthropathy | Osteonecrosis | Overall |
| n | 10 | 12 | 4 | 20 | 8 | 2 | 56 |
| % | 11.6 | 15.4 | 23.5 | 9.5 | 11.8 | 7.7 | 11.6 |
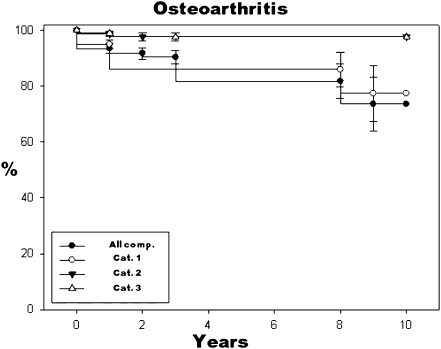
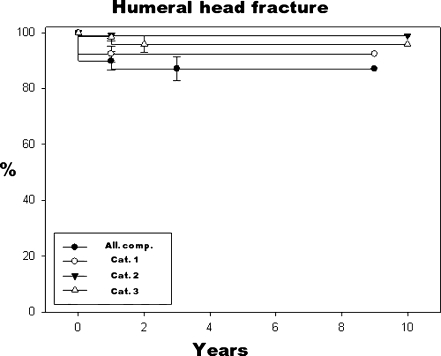
Survival rates of the whole cohort and for each diagnosis (n = 485) are shown in Table 4. The highest survival rate of 92.7% with a median follow-up of 1.75 years (range: 1–10 years) was found for the osteoarthritis cohort. The lowest survival rate of 79.2% with a median follow-up of 1.1 years (range: 1–10 years) was found for the rheumatoid arthritis cohort. Kaplan-Meier survival curves are shown for patients with osteoarthritis and for the humeral head fractures (Figs. 1 and 2)
Table 4.
Survival rates for the different diagnoses
| Diagnosis | Complications (category) | Median (years) | Survival with CI (%) | Confidence interval (%) |
|---|---|---|---|---|
| Humeral head fracture | All | 1.3 | 89.9 (83.4–96.4) | ± 6.5 |
| 1 | 1.4 | 92.4 (86.8–98) | ± 5.6 | |
| 2 | 1.7 | 99 (97–100) | ± 2 | |
| 3 | 1.7 | 98.5 (95.5–100) | ± 3 | |
| Post-traumatic arthritis | All | 1.2 | 84.6 (67.6–100) | ± 17 |
| 1 | 1.5 | 93 (87.5–98.5) | ± 5.5 | |
| 2 | 1.5 | 96.2 (91.9–100) | ± 4.3 | |
| 3 | 1.6 | 95.4 (91.2–99.6) | ± 4.2 | |
| Rheumatoid arthritis | All | 1.1 | 79.2 (60.6–97.8) | ± 18.6 |
| 1 | 1.2 | 89.7 (75.9–100) | ± 13.8 | |
| 2 | 1.2 | 89.7 (75.9–100) | ± 13.8 | |
| 3 | 1.3 | 100 | ± 0 | |
| Osteoarthritis | All | 1.8 | 92.7 (74.1−100) | ± 18.6 |
| 1 | 1.8 | 95 (92–98) | ± 3 | |
| 2 | 2 | 98.7 (96.9–100) | ± 1.8 | |
| 3 | 2 | 99 (97.6–100) | ± 1.4 | |
| Cuff tear arthropathy | All | 2.1 | 88.9 (80.9–96.9) | ± 8 |
| 1 | 2.2 | 94 (88.2–99.8) | ± 5.8 | |
| 2 | 2.2 | 98.6 (95.8–100) | ± 2.8 | |
| 3 | 2.2 | 96.2 (101.6–90.8) | ± 5.4 | |
| Osteonecrosis | All | 2.3 | 92.6 (82.6–100) | ± 10 |
| 1 | 2.5 | 96.3 (89.1–100) | ± 7.2 | |
| 2 | 2.5 | 96.3 (89.1–100) | ± 7.2 | |
| 3 | 3.3 | 100 | ± 0 | |
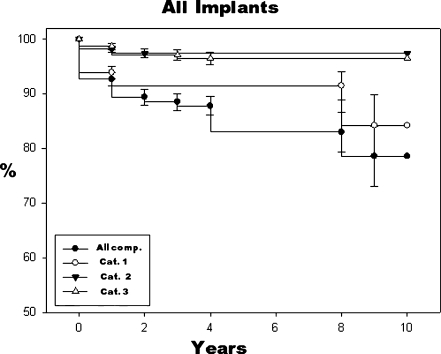
| All | All | 1.6 | 90.5 (87.9–93.1) | ± 2.6 |
| 1 | 1.8 | 93.9 (91.9–95.9) | ± 2 | |
| 2 | 1.9 | 97.9 (84.1–100) | ± 13.8 | |
| 3 | 1.9 | 98.1 (84.3–100) | ± 13.8 |
Fig. 1.
Kaplan-Meier curve for the diagnosis of osteoarthritis
Fig. 2.
Kaplan-Meier curve for the diagnosis of humeral head fracture
In the following the survival rates of the whole cohort (n = 485) and for each implant concept are shown.
Whole cohort
For the whole cohort the median follow-up was 1.6 (range: 1–10) years and the survival rate without any complication was 90.5% (CI: 87.9–93.1%). Survival without category 1 complication was 93.9% (median follow-up = 1.8 years, range: 1–10 years, CI: = 91.8–96%), survival without category 2 complication was 97.9% (median follow-up = 1.9 years, range: 1–10 years, CI: 84.1–111.7%) and for category 3 complication 98.1% (median follow-up = 1.9 years, range: 1–10 years, CI: 84.3–111.9%). Figure 3 shows the Kaplan-Meier survival curve for all implant concepts.
Fig. 3.
Kaplan-Meier curve for all implant concepts
Patients rated the result of their surgery in 270 (55.7%) cases as very satisfied, in 148 (30.5%) as satisfied, in 43 (8.9%) as somewhat disappointed and in 24 (4.9%) as very disappointed.
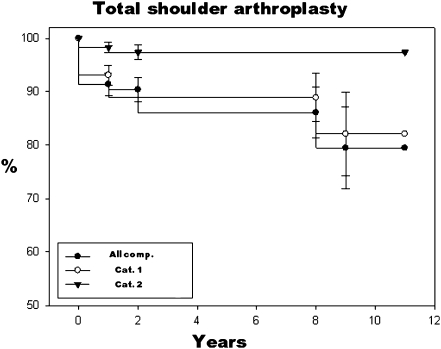
Total shoulder arthroplasty
For total shoulder arthroplasty the median follow-up was 2.2 years and the survival rate for all complications was 91.4% (range = 1–10 years, CI: 87.2–95.6%). Survival without category 1 complication was 93.1% (median follow-up = 2.2 years, range: 1–10 years, CI: 89.5–96.7%), survival without category 2 complication was 97.4% (median follow-up = 1.6 years, range: 1–10 years, CI: 94.8–100%) and survival without category 3 complication was 100% (median follow-up = 2.7 years, range: 1–10 years). Figure 4 shows the Kaplan-Meier survival curve for this implant concept.
Fig. 4.
Kaplan-Meier curve for total shoulder arthroplasty
In 129 (72.9%) cases a very satisfying result, in 36 (20.4%) a satisfying result, in eight (4.5%) a somewhat disappointing result and in four (2.3%) a very disappointing result was reported.
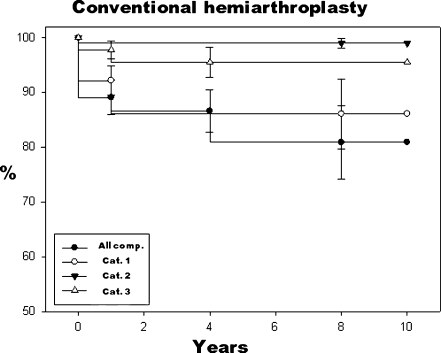
Hemiarthroplasty
For hemiarthroplasty the median follow-up was 1.8 years and the survival rate for all complications was 89.1% (range = 1–10 years, CI: 82.9–95.3%). Survival without category 1 complication was 92.2% (median follow-up = 1.9 years, range: 1–10 years, CI: 87–97.4%), survival without category 2 complication was 99% (median follow-up = 2.2 years, range: 1–10 years, CI: 80–118%) and survival without category 3 complication was 97.8% (median follow-up = 2.2 years, range: 1–10 years, CI: 94.6–101%). Figure 5 shows the Kaplan-Meier survival curve for this implant concept.
Fig. 5.
Kaplan-Meier curve for conventional hemiarthroplasty
In 46 (45.5%) cases a very satisfying result, in 32 (31.7%) a satisfying result, in 14 (13.9%) a somewhat disappointing result and in nine (8.9%) a very disappointing result was stated.
Resurfacing arthroplasty
For resurfacing arthroplasty the median follow-up was 1.7 years and the survival rate for all complications was 84.3% (range = 1–7 years, CI: 74.9–93.7.4%). Survival without category 1 complication ´was 96.1% (median follow-up = 1.7 years, range: 1–7 years, CI: 91.7–100.5%), survival without category 2 complication was 94.9% (median follow-up = 1.7 years, range: 1–7 years, CI: 88.9–100.9%) and survival without category 3 complication was 93% (median follow-up = 1.8 years, range: 1–7 years, CI: 86–100%).
In 34 (45.9%) cases a very satisfying result, in 29 (39.2%) a satisfying result, in four (5.4%) a somewhat disappointing result and in seven (9.5%) a very disappointing result was reported.
Reversed implant
For the reversed implant the median follow-up was 1.3 years and the survival rate for all complications was 88.6% (range = 1–7.5 years, CI: 79.8–97.4%). Survival without category 1 complication was 94.1% (median follow-up = 1.5 years, range: 1–7.5 years, CI: 87.5–100.7%), survival without category 2 complication was 96.3% (median follow-up = 1.3 years, range: 1–7.5 years, CI: 91.1–101.5%) and survival without category 3 complication was 98.1% (median follow-up = 1.5 years, range: 1–7.5 years, CI: 94.5–101.7%).
In 31 (63.3%) cases a very satisfying result, in 14 (28.6%) a satisfying result, in three (6.1%) a somewhat disappointing result and in one (2%) a very disappointing result was stated.
Bipolar implant
For the bipolar implant the median follow-up was 1.3 years and the survival rate for all complications was 93.8% (range = 1–4.5 years, CI: 81.8–105.8%). Survival without category 1 complication was 93.8% (median follow-up = 1.3 years, range: 1–4.5 years, CI: 81.8–105.8%), survival without category 2 complication was 100% (median follow-up = 1.3 years, range: 1–4.5 years) and survival without category 3 complication was 100% (median follow-up = 1.2 years, range: 1–4.5 years).
In five (35.7%) cases a very satisfying result, in seven (50%) a satisfying result and in two (14.3%) a somewhat disappointing result was reported.
Fracture implant
For the fracture implant the median follow-up was one year and the survival rate for all complications was 94.2% (range = 1–8.5 years, CI: 88.4–100%). Survival without category 1 complication was 95.6% (median follow-up = one year, range: 1–8.5 years, CI: 90.4–100.8%), survival without category 2 complication was 98.5% (median follow-up = 1.1 years, range: 1–8.5 years, CI: 95.5–101.5%) and survival without category 3 complication was 97.7% (median follow-up = 1.1 years, range: 1–8.5 years, CI: 93.2–102.3%).
In 24 (34.3%) cases a very satisfying result, in 30 (42.9%) a satisfying result, in 12 (17.1%) a somewhat disappointing result and in four (5.7%) a very disappointing result was reported.
Discussion
Complication and survival rates following shoulder arthroplasty were described in some studies but have rarely been addressed specifically. Moreover, there is a lack of standardised methodology for classification of types and severity of complications in shoulder arthroplasty [35]. The different complication rates described in the literature can relate to different initial diagnoses, surgical techniques, surgeons’ experience, implants and classification systems. Therefore, we introduced a system of three complication categories that can easily be applied to other cohorts and can be used as a standardised routine for the presentation of complications in shoulder arthroplasty.
The overall complication rate in this study was 11.6%. These results seem to be comparable to other reported complication rates after shoulder arthroplasty [4, 9].
However, all events were rated as a complication. Most complications were intraoperative findings or events that were treated during the index surgery or did not require revision (7%; category 1). Revision for a complication was required in 4.6%, with all soft tissue and implant revisions included (category 2–3).
With regard to the diagnoses included, the best survival rates were found for the osteoarthritis and osteonecrosis cohort (Table 4). These results seem to be difficult to interpret as for each diagnosis different implant concepts were used (Table 1). However, these data may be used as a basis for decision making by orthopaedic surgeons in shoulder replacement surgery.
For total shoulder arthroplasty (TSA), the number of reported complications has decreased tremendously in recent decades [9]. In a meta-analysis of Bohsali et al. the most common complication in TSA was component loosening [4]. In 2,540 shoulders a percentage of glenoid component loosening of 5.3% and humeral component loosening of 1.1% at 5.3 years was stated. The second most common complication was instability of the glenohumeral joint (4.9%) followed by periprosthetic fractures (1.8%; intraoperative 1.1%, postoperative 0.7%), rotator cuff tears (1.3%), neural injuries (0.8%) and infections (0.7%). Surprisingly, for TSA no revision for component loosening was found in our cohort. One reason for these results may be the short mean follow-up. The most common complications in our TSA group (n = 197) were humeral fractures (3%; intra- and postoperative 1.5%, respectively) followed by nerve palsy (2.6%), dislocation and rotator cuff tears (1.5%, respectively), infections and contracted soft tissues (0.5%, respectively; Table 2). These results seem to be comparable to the literature. The total number of complications in our TSA cohort was 10.4% and only category 1 and 2 complications were found without necessity for implant revision.
The results of hemiarthroplasty are inferior compared to TSA with regard to pain relief, motion and activity [11, 12, 23, 26]. However, many surgeons are concerned about using glenoid components especially in cases of preoperative irreparable rotator cuff tears, glenoid wear or young patients with respect to the survival of the component [8, 15, 31]. In a long-term study of Rispoli et al. significant pain relief and joint mobility were found, but also a high number of revisions was reported [27]. Of 60 patients, ten (17%) underwent revision surgery, 90% of these for postoperative glenoid wear [27]. In our cohort implant revision of a hemiarthroplasty was necessary in three cases. Only one shoulder was revised for postoperative glenoid wear (Table 2). The most common complications were nerve palsies (2.9%) followed by acute intraoperative bleeding and revision for technical error (1.9%, respectively; Table 2).
Cementless humeral head resurfacing is a bone-preserving treatment option for different diseases of the shoulder joint and later conversion to a conventional hemiarthroplasty or TSA is possible [17, 18, 24, 25]. Short surgery time as well as minimal bone and blood loss are the main advantages [22]. In the study of Bailie et al. a complication rate of 16.7% was reported using resurfacing arthroplasty [2]. The rates in other studies seem to be comparable and vary between 3% and 20% without resurfacing the glenoid [17–19, 24]. In contrast to the above-mentioned studies, we found a relatively high number of postoperative glenoid erosions (5.2%) and total number of complications (13%). The number of implant revisions was higher than in the cohort treated with a reversed implant (5.2 vs 3.7%). One reason for these findings might be the high number of post-traumatic osteoarthritis and cuff tear arthropathies in our series (Table 1).
The numbers of complications stated for fracture hemiarthroplasty vary between 5% and 64% [5, 13, 28, 30]. Non-homogenous inclusion criteria of tuberosity-related problems such as non-union may explain these divergent results. Tuberosity non-union was not categorised as a complication in this study. This may explain the relatively low complication rate for this implant concept used for humeral head fractures in this study (8.6%).
The main indications for reversed implants are rotator cuff tear arthropathies, revision arthroplasties without an intact rotator cuff tear, fractures and other less common pathological conditions. Reoperation rates for reverse arthroplasty in cases of cuff tear arthropathies are described in up to 18% of cases [16, 33, 34]. In cases of revisions and fractures, high reoperation rates were reported [6, 33, 34].
Dislocation and implant loosening are often described in the literature [20, 33]. In our cohort, implant dislocation leading to revision surgery was the most common complication (n = 4; 8.2%). The rate of satisfaction with reverse shoulder arthroplasty was highest (>90%) in our cohort.
There is little information available about the outcome and complication rates in bipolar shoulder arthroplasty. End-stage rheumatoid arthritis and cuff tear arthropathy are the most common indications for the bipolar implant [3, 7, 10]. However, satisfying results have been described by Sarris et al. in patients with cuff tear arthropathy [29]. We used bipolar implants in cases of insufficient glenoid bone stock as a second line of defence implant. The complication rates described in the literature vary between 0 and 23% [1, 10, 36].
In conclusion, shoulder arthroplasty is a very successful operation with an acceptable rate of complications in the short and midterm.
Acknowledgements
This study was supported by the “Deutsche Arthrose-Hilfe e.V.”
Footnotes
Shared first authorship: the second author equally contributed to the study.
References
- 1.Arredondo J, Worland RL. Bipolar shoulder arthroplasty in patients with osteoarthritis: short-term clinical results and evaluation of birotational head motion. J Shoulder Elbow Surg. 1999;8:425–429. doi: 10.1016/S1058-2746(99)90071-X. [DOI] [PubMed] [Google Scholar]
- 2.Bailie DS, Llinas PJ, Ellenbecker TS. Cementless humeral resurfacing arthroplasty in active patients less than fifty-five years of age. J Bone Joint Surg Am. 2008;90:110–117. doi: 10.2106/JBJS.F.01552. [DOI] [PubMed] [Google Scholar]
- 3.Berth A, Pap G. Hemi- versus bipolar shoulder arthroplasty for chronic rotator cuff arthropathy. Int Orthop. 2007;32:735–740. doi: 10.1007/s00264-007-0394-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Bohsali KI, Wirth MA, Rockwood CA., Jr Complications of total shoulder arthroplasty. J Bone Joint Surg Am. 2006;88:2279–2292. doi: 10.2106/JBJS.F.00125. [DOI] [PubMed] [Google Scholar]
- 5.Boileau P, Krishnan SG, Tinsi L, Walch G, Coste JS, Molé D. Tuberosity malposition and migration: reasons for poor outcomes after hemiarthroplasty for displaced fractures of the proximal humerus. J Shoulder Elbow Surg. 2002;11:401–412. doi: 10.1067/mse.2002.124527. [DOI] [PubMed] [Google Scholar]
- 6.Boileau P, Watkinson D, Hatzidakis AM, Hovorka I. Neer Award 2005: The Grammont reverse shoulder prosthesis: results in cuff tear arthritis, fracture sequelae, and revision arthroplasty. J Shoulder Elbow Surg. 2006;15:527–540. doi: 10.1016/j.jse.2006.01.003. [DOI] [PubMed] [Google Scholar]
- 7.Boyer P, Huten D, Alnot JY. Bipolar shoulder prosthesis for rheumatoid arthritis with irreparable rotator cuff tear: results after 5 years’ follow-up (in French) Rev Chir Orthop Reparatrice Appar Mot. 2006;92:556–566. doi: 10.1016/s0035-1040(06)75913-x. [DOI] [PubMed] [Google Scholar]
- 8.Burroughs PL, Gearen PF, Petty WR, Wright TW. Shoulder arthroplasty in the young patient. J Arthroplasty. 2003;18:792–798. doi: 10.1016/S0883-5403(03)00253-5. [DOI] [PubMed] [Google Scholar]
- 9.Chin PY, Sperling JW, Cofield RH, Schleck C. Complications of total shoulder arthroplasty: are they fewer or different? J Shoulder Elbow Surg. 2006;15:19–22. doi: 10.1016/j.jse.2005.05.005. [DOI] [PubMed] [Google Scholar]
- 10.Diaz-Borjon E, Yamakado K, Pinilla R, Keith P, Worland RL. Shoulder replacement in end-stage rotator cuff tear arthropathy: 5- to 11-year follow-up analysis of the bi-polar shoulder prosthesis. J Surg Orthop Adv. 2007;16:123–130. [PubMed] [Google Scholar]
- 11.Edwards TB, Kadakia NR, Boulahia A, Kempf JF, Boileau P, Némoz C, Walch G. A comparison of hemiarthroplasty and total shoulder arthroplasty in the treatment of primary glenohumeral osteoarthritis: results of a multicenter study. J Shoulder Elbow Surg. 2003;12:207–213. doi: 10.1016/S1058-2746(02)86804-5. [DOI] [PubMed] [Google Scholar]
- 12.Gartsman GM, Roddey TS, Hammerman SM. Shoulder arthroplasty with or without resurfacing of the glenoid in patients who have osteoarthritis. J Bone Joint Surg Am. 2000;82:26–34. doi: 10.2106/00004623-200001000-00004. [DOI] [PubMed] [Google Scholar]
- 13.Gronhagen CM, Abbaszadegan H, Revay SA, Adolphson PY. Medium-term results after primary hemiarthroplasty for comminute proximal humerus fractures: a study of 46 patients followed up for an average of 4.4 years. J Shoulder Elbow Surg. 2007;16:766–773. doi: 10.1016/j.jse.2007.03.017. [DOI] [PubMed] [Google Scholar]
- 14.Haines JF, Trail IA, Nuttall D, Birch A, Barrow A. The results of arthroplasty in osteoarthritis of the shoulder. J Bone Joint Surg Br. 2006;88:496–501. doi: 10.1302/0301-620X.88B4.16604. [DOI] [PubMed] [Google Scholar]
- 15.Hayes PR, Flatow EL. Total shoulder arthroplasty in the young patient. Instr Course Lect. 2001;50:73–88. [PubMed] [Google Scholar]
- 16.John M, Pap G, Angst F, Flury MP, Lieske S, Schwyzer HK, Simmen BR (2009) Short-term results after reversed shoulder arthroplasty (Delta III) in patients with rheumatoid arthritis and irreparable rotator cuff tear. Int Orthop [DOI] [PMC free article] [PubMed]
- 17.Levy O, Copeland SA. Cementless surface replacement arthroplasty of the shoulder. 5- to 10-year results with the Copeland mark-2 prosthesis. J Bone Joint Surg Br. 2001;83:213–221. doi: 10.1302/0301-620X.83B2.11238. [DOI] [PubMed] [Google Scholar]
- 18.Levy O, Copeland SA. Cementless surface replacement arthroplasty (Copeland CSRA) for osteoarthritis of the shoulder. J Shoulder Elbow Surg. 2004;13:266–271. doi: 10.1016/j.jse.2004.01.005. [DOI] [PubMed] [Google Scholar]
- 19.Levy O, Funk L, Sforza G, Copeland SA. Copeland surface replacement arthroplasty of the shoulder in rheumatoid arthritis. J Bone Joint Surg Am. 2004;86-A:512–518. doi: 10.2106/00004623-200403000-00008. [DOI] [PubMed] [Google Scholar]
- 20.McFarland EG, Sanguanjit P, Tasaki A, Keyurapan E, Fishman EK, Fayad LM. The reverse shoulder prosthesis: a review of imaging features and complications. Skeletal Radiol. 2006;35:488–496. doi: 10.1007/s00256-006-0109-1. [DOI] [PubMed] [Google Scholar]
- 21.Mont MA, Maar DC, Krackow KA, Jacobs MA, Jones LC, Hungerford DS. Total hip replacement without cement for non-inflammatory osteoarthrosis in patients who are less than forty-five years old. J Bone Joint Surg Am. 1993;75:740–751. doi: 10.2106/00004623-199305000-00015. [DOI] [PubMed] [Google Scholar]
- 22.Mullett H, Levy O, Raj D, Even T, Abraham R, Copeland SA. Copeland surface replacement of the shoulder. Results of an hydroxyapatite-coated cementless implant in patients over 80 years of age. J Bone Joint Surg Br. 2007;89:1466–1469. doi: 10.1302/0301-620X.89B11.18850. [DOI] [PubMed] [Google Scholar]
- 23.Radnay CS, Setter KJ, Chambers L, Levine WN, Bigliani LU, Ahmad CS. Total shoulder replacement compared with humeral head replacement for the treatment of primary glenohumeral osteoarthritis: a systematic review. J Shoulder Elbow Surg. 2007;16:396–402. doi: 10.1016/j.jse.2006.10.017. [DOI] [PubMed] [Google Scholar]
- 24.Raiss P, Aldinger PR, Kasten P, Rickert M, Loew M. Humeral head resurfacing for fixed anterior glenohumeral dislocation. Int Orthop. 2007;33:451–456. doi: 10.1007/s00264-007-0487-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Raiss P, Kasten P, Baumann F, Moser M, Rickert M, Loew M. Treatment of osteonecrosis of the humeral head with cementless surface replacement arthroplasty. J Bone Joint Surg Am. 2009;91:340–349. doi: 10.2106/JBJS.H.00560. [DOI] [PubMed] [Google Scholar]
- 26.Rickert M, Loew M. Hemiarthroplasty or total shoulder replacement in glenohumeral osteoarthritis (in German)? Orthopade. 2007;36:1013–1016. doi: 10.1007/s00132-007-1149-5. [DOI] [PubMed] [Google Scholar]
- 27.Rispoli DM, Sperling JW, Athwal GS, Schleck CD, Cofield RH. Humeral head replacement for the treatment of osteoarthritis. J Bone Joint Surg Am. 2006;88:2637–2644. doi: 10.2106/JBJS.E.01383. [DOI] [PubMed] [Google Scholar]
- 28.Robinson CM, Page RS, Hill RM, Sanders DL, Court-Brown CM, Wakefield AE. Primary hemiarthroplasty for treatment of proximal humeral fractures. J Bone Joint Surg Am. 2003;85-A:1215–1223. doi: 10.2106/00004623-200307000-00006. [DOI] [PubMed] [Google Scholar]
- 29.Sarris IK, Papadimitriou NG, Sotereanos DG. Bipolar hemiarthroplasty for chronic rotator cuff tear arthropathy. J Arthroplasty. 2003;18:169–173. doi: 10.1054/arth.2003.50041. [DOI] [PubMed] [Google Scholar]
- 30.Smith AM, Mardones RM, Sperling JW, Cofield RH. Early complications of operatively treated proximal humeral fractures. J Shoulder Elbow Surg. 2007;16:14–24. doi: 10.1016/j.jse.2006.05.008. [DOI] [PubMed] [Google Scholar]
- 31.Sperling JW, Cofield RH, Rowland CM. Minimum fifteen-year follow-up of Neer hemiarthroplasty and total shoulder arthroplasty in patients aged fifty years or younger. J Shoulder Elbow Surg. 2004;13:604–613. doi: 10.1016/j.jse.2004.03.013. [DOI] [PubMed] [Google Scholar]
- 32.Stern SH, Bowen MK, Insall JN, Scuderi GR. Cemented total knee arthroplasty for gonarthrosis in patients 55 years old or younger. Clin Orthop Relat Res. 1990;260:124–129. [PubMed] [Google Scholar]
- 33.Wall B, Nové-Josserand L, O’Connor DP, Edwards TB, Walch G. Reverse total shoulder arthroplasty: a review of results according to etiology. J Bone Joint Surg Am. 2007;89:1476–1485. doi: 10.2106/JBJS.F.00666. [DOI] [PubMed] [Google Scholar]
- 34.Werner CM, Steinmann PA, Gilbart M, Gerber C. Treatment of painful pseudoparesis due to irreparable rotator cuff dysfunction with the Delta III reverse-ball-and-socket total shoulder prosthesis. J Bone Joint Surg Am. 2005;87:1476–1486. doi: 10.2106/JBJS.D.02342. [DOI] [PubMed] [Google Scholar]
- 35.Wirth MA, Rockwood CA., Jr Complications of total shoulder-replacement arthroplasty. J Bone Joint Surg Am. 1996;78:603–616. doi: 10.2106/00004623-199604000-00018. [DOI] [PubMed] [Google Scholar]
- 36.Worland RL, Jessup DE, Arredondo J, Warburton KJ. Bipolar shoulder arthroplasty for rotator cuff arthropathy. J Shoulder Elbow Surg. 1997;6:512–515. doi: 10.1016/S1058-2746(97)90083-5. [DOI] [PubMed] [Google Scholar]