Abstract
The aim of this study was to evaluate our treatment of distal tibial physeal injuries retrospectively and explain the relationship between the trauma mechanism, the radiographic injury pattern, the subsequent therapy and the functional outcome, as well as to further deduce and verify prognostic criteria. At the Department of Trauma Surgery, Vienna Medical University, 419 children and adolescent patients with physeal injuries of the distal tibia were treated from 1993 to 2007, of these 376 were included in our study and evaluated retrospectively. Seventy-seven displaced physeal fractures of the distal tibia were reconstructed anatomically by open or closed reduction and produced 95% excellent results. A perfect anatomical reduction, if necessary by open means, should be achieved to prevent a bone bridge with subsequent epiphysiodesis and post-traumatic deformities due to growth inhibition and/or retardation.
Introduction
Injuries to the physis of the distal tibia are the second most common growth plate injuries following those of the distal radius according to Peterson et al. [1]. A physeal growth arrest with consecutive bone bridge can occur occasionally after an injury of the distal tibial physis. Angular deformity or leg-length discrepancy can be the consequence. Permanent damage to the growth plate can be produced due to the trauma itself or by inadequate treatment [1]. Beaty et al. [2] described a contribution of 45% of the distal tibial physis to the longitudinal growth of the tibia, compared to 55% in the proximal physis. The distal physis contributes to about 5 mm/y during the years of most rapid growth in childhood. Fractures of the ankle joint represent only 6% of the total number of tibial fractures in children according to de Sanctis et al. [3]. These injuries include malleolar fractures, tibial and fibular physeal injuries. Fractures involving the medial or lateral malleolus are more common in older children and are similar to those in adults [3].
During paediatric ankle trauma, the force is transmitted directly to the metaphyseal tibial area, which is the most fragile region, due to the flexibility of the cortical bone from one side and the solidity and elasticity of the powerful ligamentous apparatus from the other side, as described by Melchior et al. [4]. These anatomical features of the adolescent ankle predispose a fracture and usually lead to a fracture displacement in the metaphyseal area.
Several hypotheses were described about the aetiology of growth plate damage after trauma, e.g. Carothers and Crenshaw [5], Aitken [6] or Salter and Harris [7]. The mechanism of trauma can be correlated with the type of lesion and the occurrence of post-traumatic damage to the growth plate [5, 8]. Further, post-traumatic growth plate damage is most frequently due to an injury with a crushing force [6].
The most severe complication following a physeal injury is growth plate arrest, which can be treated conservatively and operatively according to some reports, e.g. shoe lifts, excision of the bone bridge, leg lengthening, contra and ipsilateral epiphysiodesis, corrective osteotomies [9, 10].
This study compares the radiographic outcome with respect to the degree of displacement and separation by using the Carothers-Crenshaw classification [5], based on the initial trauma mechanism, with the Salter-Harris classification [7], based on radiographic criteria. We evaluated our methods of treatment retrospectively and present the relationship between the mechanism of trauma, the radiographic injury pattern, the subsequent therapy and the functional outcome, and verify the prognostic criteria for physeal ankle injuries of the distal tibia.
Patients and methods
At the Department of Trauma Surgery at the Vienna Medical University 419 children and adolescent patients with physeal injuries of the distal tibia were treated from 1993 to 2007. Forty-three patients were lost the follow-up. A group of 181 patients with a clinically diagnosed epiphyseal separation, having a negative X-ray (Salter Harries type I), was excluded from our results and statistical analysis. Thus, 195 patients were included in our study. Every patient’s clinical chart, and every X-ray and/or CT-scan was reviewed. Demographic data, the type of injury, the trauma mechanism, diagnostic and therapeutic procedures and the follow-up treatment were reviewed. The mean patient's age was 11.6 years, and 64% were male and 36% female.
The trauma mechanism was established by X-ray examination and classified according to the Carothers-Crenshaw Classification [5]: I, adduction; II, abduction; III, plantar flexion; IV, lateral rotation; and V, crush injury.
All fractures were classified according to the Salter-Harris Classification [7]: I, epiphyseal separation; II, epiphyseal separation and metaphyseal fracture; III, epiphyseal separation and epiphyseal fracture; IV, epi-metaphyseal fracture; and V, crush injury.
Further classification followed according to the anatomical fracture type: 118 patients (60.5%) sustained a physeal separation of the distal tibia without displacement and 77 patients (39.5%) had a displaced physeal injury. Bimalleolar fractures occurred in 37 patients (18.3%). All non-displaced fractures were treated by plaster cast immobilisation. Displaced fractures, regardless the degree of displacement, were treated by open or closed reduction, with or without internal fixation, to achieve an absolutely anatomical reduction. A plaster cast immobilisation followed in each case, unless an external fixator was used.
The time of plaster cast immobilisation varied, depending on the patient’s age, from three to six weeks in all groups. The decision for weight bearing or non-weight bearing mobilisation in the plaster cast was based on following facts: fracture location (extra/intraarticular), fragment size, stable/unstable fracture, comminution, stability of osteosynthesis, patient age and compliance. We prefer plaster cast treatment to obviate compliance problems and secure good results, although a stable osteosynthesis would not require additional external fixation.
The mean overall follow-up time was 12.1 weeks (range, 3 weeks to 2.5 years). This major disparity of follow-up time results from to the variable healing time, depending on the patients age and the type of lesion. The mean follow-up time of operatively treated displaced fractures was 1.2 years.
SPSS 15.0 (Statistical Program for the Social Sciences; SPSS Inc., Chicago, IL, USA) was used to compare the results of each classification, with the type of treatment and clinical and radiographic outcome with each other in cross-tables.
Results
One hundred twenty-five (64.1%) patients were treated conservatively, while 70 (35.9%) patients underwent a surgical procedure.
Screw fixation or K-wires were used following an open reduction and an external fixator only in special cases. Twenty-four fractures were treated by open means (six pinning, 11 screws, seven screws and pins), and 40 were treated closed (seven pinning, 25 screws, eight screws and pinning), either by pinning or/and screw fixation. Six fractures were treated by an external fixator in addition to an open fracture reduction, either to achieve greater stability or in an unstable soft tissue situation. A full and immediate recovery without any complications was seen in 91.8% of patients, with no angular deformities or limb length discrepancies. Only 8.1% of our patients had average or poor results, caused by persisting pain, joint stiffness or leg-length discrepancy during the follow-up period.
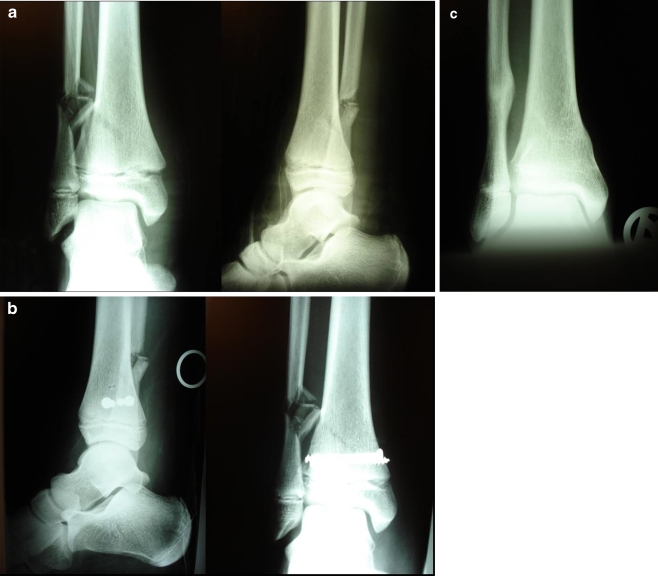
One patient developed a limb-length discrepancy of 1 cm after 1.5 years caused by a premature closure of the medial part of the distal tibial physis (Fig. 1a–c). No patient developed a clinically significant angular deformity; one patient with an open distal tibial fracture and severe dislocation had a major loss of joint function.
Fig. 1.
a X-ray injury. b X-ray postoperative. c X-ray follow-up with partial epiphysiodesis
The average age pattern (male and female), according to the Salter-Harries classification, was 11 years for type II injuries, 12.4 years for type III injuries and 13.3 years for type IV injuries. The Salter-Harris type II injury, mostly caused by an adduction mechanism, had the highest rate of fracture dislocation (35.4%), which required an operative intervention in all 40 patients, but produced 95% good results (Tables 1, 2, 3).
Table 1.
Cross-table comparison of the frequency of distal tibial physeal injuries with the Salter-Harris classification (radiographic) versus the Carothers-Crenshaw classification (trauma mechanism)
| Carothers Crenshaw | Salter-Harris | Σ | ||||
|---|---|---|---|---|---|---|
| SH 1 | SH 2 | SH 3 | SH 4 | SH 5 | SH | |
| Adduction | 158 | 67 | 43 | 9 | 0 | 277 |
| Suppination | 13 | 18 | 10 | 0 | 0 | 41 |
| Abduction plantar flexion | 2 | 19 | 2 | 1 | 0 | 24 |
| External rotation | 8 | 9 | 11 | 6 | 0 | 34 |
| Crush-injury | 0 | 0 | 0 | 0 | 0 | 0 |
| Σ | 181 | 113 | 66 | 16 | 0 | 376 |
Table 2.
Cross-table comparison of the frequency of distal tibial physeal injuries with the Salter-Harris classification (radiographic) versus the frequency of fracture dislocation
| Salter-Harris | Displacement | Σ | |
|---|---|---|---|
| Positive | Negative | ||
| SH 1 | 0 | 181 | 181 |
| SH 2 | 40 | 73 | 113 |
| SH 3 | 26 | 40 | 66 |
| SH 4 | 11 | 5 | 16 |
| Σ | 77 | 294 | 376 |
Table 3.
Cross-table comparison of the frequency of distal tibial physeal injuries with the Salter-Harris classification (radiographic) versus patient outcome
| Salter-Harris | Outcome | Σ | |
|---|---|---|---|
| Good | Poor | ||
| SH 1 | 180 | 1 | 181 |
| SH 2 | 107 | 6 | 113 |
| SH 3 | 58 | 8 | 66 |
| SH 4 | 15 | 1 | 16 |
| Σ | 360 | 16 | 376 |
The most common injuries to the distal tibial physis are caused by an adduction trauma of the ankle in 60.9%, followed by abduction in 14.6%, external rotation in 13%, and plantar flexion in 11.5%. A crush injury was not seen (Table 1). Correlation of the frequency of distal tibial physeal fractures with the Salter-Harris classification confirms that the most common radiographic injury patterns, without respect to type I injuries, were type II injuries in 113 patients (58%), followed by type III fractures in 66 patients (33.8%) and type IV fractures in 16 patients (8.2%) (Table 1).
Patients with Salter-Harris type II injuries had a mean immobilisation time of 4.1 weeks, while type III injuries needed 4.7 weeks and type IV injuries 5.6 weeks. Injuries followed by surgery in type II occurred in 35.4%, in type III in 34.8% and in type IV in 60%, analysing each group separately.
Patients presenting a Salter-Harris type I injury had good results in nearly every case (99.7%) and had a short period of immobilisation and recovery with a mean time of 1.4 weeks.
Discussion
In 1922, Ashhurst and Bromer published a literature review describing a classification of ankle fractures based on the trauma mechanism [11], and Carothers and Crenshaw published 54 physeal ankle fractures in 1955, based on this classification system [5]. They stated that the Salter-Harris type V physeal injury is difficult, if not impossible, to diagnose acutely. The only radiographic indication may be decrease in the normal width of the radiolucent physis. These fractures are usually diagnosed in retrospect, sometime after the injury. The absence of Harris arrest lines indicates that growth of the entire physis has completely stopped. The development of a bony bar, within some months following the initial injury, is associated with a complete arrest of growth of only a portion of the entire physis. This eventually produces a joint surface deformity, an angular deformity and/or a length discrepancy of the damaged extremity. According to Sferopoulos, a Salter-Harris type V injury is usually considered radiographically occult. To him, these injuries may have no obvious fracture line extending to the physis, but the persistence of significant pain at the level of the physeal plate for over a week, and the radiographic appearance of impaction or diminution of the width of the growth plate could be absolute indications to perform an MRI. He also stated that the appearance of bone contusions across the physis in the setting of acute injury could be a strong indication of a Salter-Harris type V injury [12].
The correct treatment of ankle fractures in children depends on the fracture location, degree of displacement and the child’s age. In accordance with Kling et al. [13], we state that epiphyseal injuries should be anatomically reduced by open means. We do not believe that physeal fractures in older children, in whom growth is nearly complete, or in younger children whose fractures are associated with little risk for disturbance in growth, will do well with a closed treatment. We believe that every fracture displacement must be corrected anatomically at any patient age to achieve excellent results.
Our results show that physeal injuries of the distal tibia requiring surgery occur at an average age of 12.4 years. Direct and indirect forces acting on the ankle, the ligamentous anatomy of the ankle and the effects of trauma on the epiphysis before and during the time of epiphyseal fusion are responsible for the fracture mechanism. Pro- or supination and/or external rotation injuries are the most common trauma mechanisms in our group (Table 1). In concurrence with de Sanctis et al. [3], our results underline that an adduction supination injury frequently causes Salter-Harris injuries type II (n = 67, 24,.%), type III (n = 43, 15.5%) and type IV (n = 9, 3.5%) with permanent damage to the physis (Table 1). The combination of a traumatic mechanism with compression and adduction forces may cause a type III or IV fracture with an additive physeal crush. In contrast, injuries caused by abduction, lateral rotation and plantar flexion determining fracture types I and II have a low incidence of complications. The predominance of distraction and translation explains this finding.
The most commonly injured area of the growth plate is the proliferative layer of cells. This location of damage to the physis after fracture displacement is the cause of complications. Although the growth plate is interrupted at the level of the degenerative layer of cells, the lesions remain with low risk of disturbance in types I and II. Type III and IV lesions of the growth plate, caused by compressive trauma or a fracture passing through the physis, may severely damage the proliferative layer of cells with a high risk of growth disturbance [3].
A further major fact influencing the functional outcome is the degree of displacement. Salter and Harris [7] showed that fractures passing through the physis are replaced by bony tissue, followed by a bone bridge.
Lalandle et al. [14] insisted on bar excision if a partial physeal arrest involving <50% of the physis arises and is detected before a deformity is apparent. They proceeded with an ipsilateral epiphysiodesis of the tibia and fibula if the patient was near the end of his or her growth. They also stated that if a child still has any great degree of growth to attain and the leg-length discrepancy is predicted to exceed 5 cm, leg lengthening with an external fixator or an intramedullary device must be considered. Finally, if the angular deformity is clinically significant, supramalleolar osteotomy can be performed for angular correction. According to Langenskiöld's original article, Sailhan stated that at least a year of growth should remain if resection of a bony bar is attempted. Optimal correction results when two years of expected longitudinal growth remains and when the physeal bridge involves less than 50% of the growth plate area [15].
For de Sanctis et al., growth disturbance can be caused by the use of inadequate surgical fixation. For them the risks with a Kirschner wire are minor compared with the insertion of a screw near a proliferative layer of cells, which may cause growth arrest [3]. Cottalorda believes that reduction, especially compression, is better with screws than Kirschner wires. To achieve anatomical reduction his team uses an epiphyseal lag screw for cancellous bone to achieve better compression of the fracture line. They showed in their study that this risk is very low if the surgery is done under the control of the intensifier screen. Their results demonstrate that anatomical open reduction with realignment of the physis can result in continued longitudinal growth without deformity. The lack of complications after surgery at their longest follow-up suggests that open reduction is a safe procedure. The consequence is that the larger the fracture gap, the bigger the bone bridge. Therefore, displaced type III and IV Salter-Harris fractures require an early anatomical reduction by closed or open means [16].
In contrast to Spiegel et al. [17], we require an anatomical reduction in every displaced epiphyseal fracture, not only in cases with ≥2 mm fragment displacement. Our results underline that only an absolute anatomical fracture reduction can prevent a bone bridge and a consecutive epiphysiodesis with axial malalignement and limb length discrepancy. The open reduction is a safe procedure in children with a low rate of complications, and a subsequent partial or total epiphysiodesis with bony bar bridging rarely occurs. A weak point of our study is the relatively short follow-up of the nonoperatively treated patients with undisplaced fractures (12.1 weeks). The group of patients with operatively treated displaced fractures could be better studied, but the optimal follow-up time could not be achieved, as mentioned in the conclusion.
Conclusion
The understanding of common paediatric ankle fracture patterns will assist the surgeon in the management of these injuries. To determine prognostic factors for physeal injuries, the X-ray must be interpreted in order to understand the trauma mechanism and of evaluate the grade of damage to the physeal plate correctly. The young patient must be carefully assessed, and the fracture displacement must be assessed by X-ray or, if necessary, by CT-scan. Our operative results underline the requirement to achieve an absolute anatomical reduction in all planes in every patient by closed or open procedures. This decreases the rate of post-traumatic epiphysiodesis with the subsequent problems, including leg-length discrepancy and/or angular deformities. No fracture displacement can be tolerated. We recommend that a two-year follow-up period is necessary to safely detect severe complications and avoid major growth disturbance.
References
- 1.Peterson CA, Peterson HA. Analysis of the incidence of injuries to the epiphyseal growth plate. J Trauma. 1972;12:275–281. doi: 10.1097/00005373-197204000-00002. [DOI] [PubMed] [Google Scholar]
- 2.Rathjen K, Birch J. Physeal injuries and growth disturbances. In: Rockwood and Wilkins fractures in children. 6. Philadelphia: Lippincott Williams & Wilkins; 2006. pp. 102–104. [Google Scholar]
- 3.Sanctis N, Della Corte S, Pempinello C. Distal tibial and fibular epiphyseal fractures in children: Prognostic criteria and long term results in 158 patients. J Pediatr Orthop Part B. 2000;9:40–44. doi: 10.1097/01202412-200001000-00008. [DOI] [PubMed] [Google Scholar]
- 4.Melchior B, Badelon P, Peraldi P, Bensahel H. Les fractures decollementes epiphysaires de l’extremite inferieure du tibia. Chir Pediatr. 1990;31:113–118. [PubMed] [Google Scholar]
- 5.Carothers CO, Crenshaw AH. Clinical significance of a classification of epiphyseal injuries of the ankle. Am J Surg. 1953;89:879–889. doi: 10.1016/0002-9610(55)90158-6. [DOI] [PubMed] [Google Scholar]
- 6.Aitken AP. The end results of the fractured distal tibial epiphysis. J Bone Joint Surg. 1936;18:685–691. [Google Scholar]
- 7.Salter RB, Harris WR. Injuries involving the epiphyseal plate. J Bone Joint Surg Am. 1963;45:587–622. [Google Scholar]
- 8.Hajdu S, Kaltenecker G, Schwendenwein E, Vécsei V. Apophyseal injuries of the proximal tibial tubercle. Int Orthop. 2000;24:279–281. doi: 10.1007/s002640000162. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Berson L, Davidson RS, Dormans JP, Drummond DS, Gregg JR. Growth disturbance after distal physeal fractures. Foot Ankle Int. 2000;21:54–58. doi: 10.1177/107110070002100110. [DOI] [PubMed] [Google Scholar]
- 10.Williamson RV, Staehli LT. Partial physeal growth arrest: treatment by bridge resection and fat interposition. J Pediatr Orthop. 1990;10:769–776. [PubMed] [Google Scholar]
- 11.Ashhurst APC, Bromer RS. Classification and mechanism of fractures of the leg bones involving the ankle. Arch Surg. 1922;4:51–129. [Google Scholar]
- 12.Sferopoulos NK. Type V physeal injury. J Trauma. 2007;63:121–123. doi: 10.1097/TA.0b013e3180686548. [DOI] [PubMed] [Google Scholar]
- 13.Kling TF, Bright RW, Hensinger RN. Distal tibial physeal fractures in children that might require an open reduction. J Bone Joint Surg Am. 1984;66:647–657. [PubMed] [Google Scholar]
- 14.Lalandle K, Letts M. Traumatic growth arrest of the distal tibia: a clinical and radiographic review. Can J Surg. 2005;2:143–147. [PMC free article] [PubMed] [Google Scholar]
- 15.Sailhan F, Chotel F, Guibal AL, Gollogly S, Adam P, Bérard J, Guibaud L. Three dimensional MR imaging in the assessment of physeal growth arrest. Eur Radiol. 2004;14:1600–1608. doi: 10.1007/s00330-004-2319-z. [DOI] [PubMed] [Google Scholar]
- 16.Cottalorda J, Béranger V, Louahem D, Camilleri JP, Launay F, Diméglio A, Bourelle S, Jouve JL, Bollini G. Salter-Harris type III and IV medial malleolar fractures: growth arrest is it a fate? J Pediatr Orthop. 2008;28:652–655. doi: 10.1097/BPO.0b013e318182f74c. [DOI] [PubMed] [Google Scholar]
- 17.Spiegel P, Cooperman D, Laros G. Epiphyseal fractures of the distal ends of the tibia and fibula. J Bone Joint Surg Am. 1978;60:1046–1059. [PubMed] [Google Scholar]