Abstract
The purpose of this study is to investigate the early clinical and radiographic findings related to acetabular orientation after a curved periacetabular osteotomy (CPO). 106 dysplastic hips of 88 patients underwent CPO were investigated retrospectively with an average follow-up of 3.6 years. Conventional anteroposterior radiographs were used to measure the radiographic findings and range of motion were used for clinical evaluations. A significant improvement was noted in radiographic measurements including lateral centre-edge angle, acetabular index, and acetabular angle of Sharp. However, a high rate of postoperative acetabular retroversion was observed (62% hips) and a marked decrease in free flexion was noted. The Tönnis scale revealed a one-grade progression in most retroversion hips. Acetabular retroversion is a high risk factor leading to degenerative osteoarthritis of hip. Therefore, special consideration must be taken in surgical planning and careful intraoperative confirmation is required whilst manoeuvring the acetabular fragment in CPO.
Introduction
Acetabular dysplasia is the most common cause of secondary osteoarthrosis [3, 18]. To improve the prognosis for dysplastic hips in young patients, various periacetabular osteotomies have been developed to reorient the hyaline cartilage of the acetabulum with an effort to improve the mechanical environment of dysplastic hips [9, 10, 14, 19, 20]. Among them, the Bernese periacetabular osteotomy provides a good coverage of the femoral head by redirecting the acetabulum, preserving the vascular supply of the transferred acetabulum and allowing medialisation of the hip [1]. Our first study reported a modified Bernese osteotomy, a curved periacetabular osteotomy (CPO), and its short-term clinical results demonstrated that it is also a good alternative as a joint-preserving procedure for the treatment of hip dysplasia [8, 15]. Recently, acetabular retroversion, which can result from such periacetabular osteotomies, has been recognised and described as a possible aetiological factor leading to osteoarthritis [2, 4, 13, 16]. The diagnosis of acetabular retroversion is made on the basis of computed tomograph findings of horizontal acetabular cross sections or on the basis of two distinct signs—the cross-over and posterior wall signs revealed by anteroposterior (AP) pelvic radiography [6, 7, 22]. Myers et al. were the first to report the case of acetabular retroversion after the Bernese periacetabular osteotomy in 1999. They found that this type of malorientation not only led to the progressive development of symptoms caused by an anterior impingement between the anterior acetabular rim and the anterior femoral head, but, when pronounced, also placed the patient at a higher risk of developing degenerative osteoarthritis [7]. A recent learning curve study reported 17 hips that were undercorrected to neutral wall relationships or acetabular retroversion; those were among the first 34 hips that underwent the Bernese osteotomy [11]. Therefore, it is necessary to evaluate the acetabular orientation, especially when a new periacetabular osteotomy was introduced to patients.
The purpose of this study was to investigate the early clinical and radiographic findings related to acetabular versions and to find out the potential reasons for the postoperative abnormality of acetabular versions while providing safer and more accurate surgical techniques for reconstructing anatomical acetabular versions during the CPO surgery.
Materials and methods
This retrospective study was approved by our institutional review board. Between 1998 and 2004, CPO was performed by one of our authors (M.N.) on 158 consecutive hips in 132 patients (ten males and 122 females). The diagnosis of acetabular dysplasia was established from lateral central angle (CE), which was less than 20 degrees on the AP radiography. Twenty-eight hips (25 patients) were excluded from this study due to excessive pelvic inclination and 19 patients (24 hips) were lost to follow-up. The final number of patients was 88 (106 hips). The average age of the patients at the time of surgery was 37.5 (range 15–52) years. The average follow-up period was 3.6 years (range 2–8).
Surgical procedure
The operation was carried out with patients in the supine position, through a direct anterior approach, with an incision of approximately 12 cm for surgical exposure. The osteotomy was performed in the same manner with a procedure described previously in detail [8]. An image intensifier was used after the acetabular fragment was redirected and fixed temporarily with Kirschner wires to ensure that three goals were achieved: the femoral head was covered adequately by the reorientated acetabular fragment, the weightbearing area of the reorientated acetabular fragment was in a horizontal position and that the hip was medialised. In this series, the flexion and internal rotation in flexion which should include passive forced flexion, adduction, and internal rotation of the hip with the patient in the supine position, was not tested intraoperatively. Two or three poly-L-lactic acid screws were used to finally fix the reorientated acetabular fragment.
Clinical and radiographic evaluations
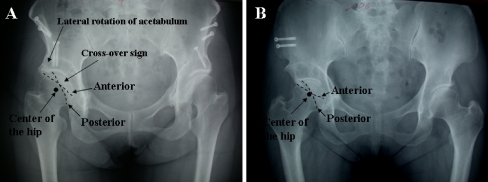
The range of motion of hip was measured for all patients preoperatively and postoperatively. Since acetabular dysplasia is frequently combined with femoral abnormalities such as a diminished antero-lateral head–neck offset which may produce a positive impingement test on internal rotation in flexion even after a correct acetabular version has been established [7], free flexion without internal rotation of hip was measured in this study. The patients were in the supine position and the angle of passive forced flexion of the hip was recorded when the pelvis was stabilised by one of the co-authors. A few hips may have had reduced flexion preoperatively due to pain, but when pain is subsiding postoperatively, flexion may increase. Therefore, the measurement was triplicated when patients were painfree and the average was considered as the final data. For the radiographic measurement, preoperative and postoperative AP radiographs of the pelvis were digitised into a personal computer, and lateral centre-edge angle, acetabular index and Sharp’s acetabular angle were measured using ImageJ software (version of 1.36; National Institutes of Health, USA). Regarding the assessment of acetabular version, if the posterior wall of the acetabulum extended more laterally than the shadow of the anterior wall in this projection, the hip was classified as showing anteversion, whereas the acetabulum was classified as showing retroversion on the basis of cross-over sign—when the anterior wall shadow projected more laterally to the posterior wall shadow [6]. On the other hand, a deficient coverage of the posterior wall was identified as the posterior wall sign when the outline of the posterior aspect of the rim was more medial than the centre of the femoral head (Fig. 1) [3]. To exclude the effect of pelvic inclination, we used the method described previously. The distance between the pubic symphysis and the sacrococcygeal joint was measured on each standard AP radiograph for comparison with the reported control values ranging from 25 to 40 mm for men and 40 to 55 mm for women. Pelvic symmetry was evaluated in terms of the comparative radiographic appearance of the obturator foramina and the positions of the sacral midpoint and the pubic symphysis [17]. The Tönnis classification was used to determine the presence of osteoarthritis in the hips [21].
Fig. 1.
Anteroposterior radiograph of a patient with acetabular retroversion after curved periacetabular osteotomy (CPO). The superior aspect of the anterior line is on lateral to the posterior line, resulting in a cross-over sign. Note that the posterior line is medial to the centre of the hip, which is the posterior wall sign (a). Acetabular retroversion with negative posterior wall sign (b)
Statistical analysis
Nonparametric statistical analysis was performed using Stat View 5.0 for Windows. We compared the clinical and radiographic data of preoperative hips with that of postoperative hips using the Mann-Whitney test. The significance level of these analyses was 5%.
Results
The physical examination revealed an increase in the range of free flexion for the hips with acetabular anteversion from 108 ± 14° preoperatively to 112 ± 17° postoperatively. Retroversion hips showed a significant decrease in the range of flexion from 122 ± 15° preoperatively to 102 ± 14° postoperatively (P < 0.05). No progression of osteoarthritis, as determined using the Tönnis scale, was found in 91 of the 106 hips. There was a one-grade progression in 14 hips. Among them, ten hips (71%) were identified as acetabular retroversion.
In radiographic measurements, there was a tendency toward a decrease in the acetabular index and an increase in the lateral centre-edge angle, regardless of the presence of acetabular anteversion or retroversion after CPO. The lateral centre-edge angle significantly increased from a preoperative 9 ± 8° to a postoperative 33 ± 7°, whereas the acetabular index decreased markedly from 23 ± 8° preoperatively to 4 ± 6° postoperatively in hips with acetabular anteversion. As for the hips with acetabular retroversion, the lateral centre-edge angle increased from 10 ± 7° preoperatively to 33 ± 10° postoperatively, and the acetabular index significantly decreased from 23 ± 7° to 5 ± 8° postoperatively (Table 1). AP radiographs taken at the time of the last follow-up did not reveal any signs of osteonecrosis of the femoral head in any patients.
Table 1.
Radiographic changes and range of motion in postoperative anteversion and retroversion hips
| Measurement | Preoperative | Latest follow-up | Correction |
|---|---|---|---|
| Lateral centre-edge angle | 9 ± 8/10 ± 7 | 33 ± 7/33 ± 10 | 24 ± 10*/22 ± 11* |
| Acetabular index | 23 ± 8/23 ± 7 | 4 ± 6/5 ± 8 | 19 ± 8*/18 ± 8* |
| Acetabular sharp angle | 48 ± 4/47 ± 5 | 39 ± 5/39 ± 6 | 9 ± 4*/9 ± 5* |
| Range of free flexion | 108 ± 14/122 ± 15 | 119 ± 17/102 ± 14 | 10 ± 9*/−21 ± 12* |
All data are shown as the mean ± SD in degrees for anteversion and retroversion hips (anteversion/retroversion)
*P < 0.05
Acetabular retroversion was found in 16 (15%) of 106 hips preoperatively (Table 2). The posterior wall deficiency of the acetabulum was observed in 46 (43%) hips with acetabular anteversion and 14 (13%) hips with retroversion. Postoperative evaluations showed 66 (62%) hips with acetabular retroversion. Among them, 16 (15%) hips were negative for the posterior wall sign (Fig. 1b), whereas 50 (47%) hips were positive for the posterior wall sign (Fig. 1a). The evaluation of acetabular version revealed that 56 hips with preoperative anteversion were overcorrected to retroversion. Ten hips with preoperative retroversion showed no change in the version. Six hips with preoperative retroversion were successfully corrected to anteversion.
Table 2.
Preoperative and postoperative number of hips with the cross-over sign and/or the posterior wall sign
| Posterior wall sign | Cross-over sign | |||
|---|---|---|---|---|
| Preoperative | Postoperative | |||
| − | + | − | + | |
| − | 44 (42%) | 2 (2%) | 32 (30%) | 16 (15%) |
| + | 46 (43%) | 14 (13%) | 8 (8%) | 50 (47%) |
| Sum | 90 (85%) | 16 (15%) | 40 (37%) | 66 (62%) |
All data are shown as the number with the percentage in parentheses
Discussion
Radiographic measurements preoperatively and postoperatively revealed significant improvements in acetabular index, CE angle, and Sharp’s acetabular angle, indicating the hip stability reconstructed by CPO. This is in good agreement with our previous study in which the stability of normal hips and instability of dysplastic hips strongly correlated with radiographic measurements such as CE angle and acetabular index [5]. Thus, one of the most important goals of periacetabular osteotomy is to restore joint stability by reorienting the acetabular fragment.
In this study, the prevalence of preoperative acetabular retroversion was 15% of 106 hips with developmental dysplasia, which is comparable to the values found in the literature ranging between 6% and 20% [21, 22]. The interesting finding is the preoperative number of anteversion hips with posterior wall sign, that is, 46 (43%) of 106 hips, suggesting a high prevalence of a global deficient coverage in both the anterior and posterior aspects among development dysplasia hips. On the other hand, irrespective of the presence of acetabular anteversion or retroversion postoperatively, the posterior wall sign was still found in 55% of dysplastic hips, indicating it would be a big challenge to obtain the proper medialisation of the femoral head and posterior coverage simultaneously in manoeuvring the acetabular fragment during the surgery. It is even more surprising that 62% of hips with postoperative retroversion have been observed. In the following physical examination, a significant decrease in flexion was noted in hips with retroversion, indicating the excessive anterior coverage of acetabulum. In addition, one-grade progressions were observed in most hips with retroversion (ten of 14 hips) using the Tönnis scale. Among 66 hips with retroversion, decreased flexion was found in 44 hips, while others were functioning well. We assume that, since the acetabular dysplasia usually has a global deficient coverage, that is, not only in the anterior aspect but also in the posterior aspect, anterior impingement will probably not occur unless the acetabulum is retroverted excessively to some extent. This is in agreement with a previous study in which the retroversion of the acetabulum was investigated clinically and radiologically using axial computed tomography (CT) scans. The significant symptoms were associated only with retroversion angles greater than 15°, which was defined as the angle between the acetabular roof line and the sagittal plane at a level distal to the roof [13]. This may be one of the reasons why a decrease in flexion was not observed in all hips with retroversion. Therefore, a quantitative analysis of retroversion should be incorporated in the design of a further study using more accurate methods such as CT scans.
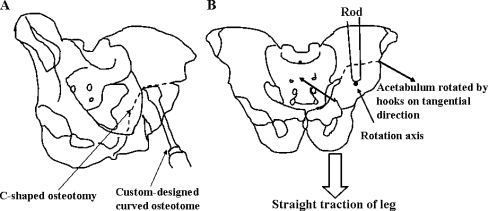
The proper positioning of the mobilised acetabulum is a very challenging stage of acetabular osteotomies. Our data indicate that CPO tends to produce acetabular retroversion. One possibility for difficulties with correction of the version may be the fact that the authors execute the correction of the lateral coverage first (indicated by the visible step in the lateral contour of the supraacetabular bone in Fig. 1). It may lead to easier jamming of the acetabular fragment compared with anterior rotation of the acetabulum as the first step of the correcting manoeuvre. Another reason is that only consideration of lateral coverage was taken due to the limited information regarding the acetabular orientation and femoral anterior impingement. Even though an image intensifier was used to confirm the correction of the acetabular fragment, the establishment of anatomical anteversion was not routinely carefully checked. On the basis of our surgical experience and the recognition of recent knowledge on acetabular wall relationship, we have modified our surgical technique to avoid retroversion. When all parts of acetabular fragment are freed from surrounding bone (Fig. 2a), the rotation is maneuvered using two bone hooks placed onto the anterior-superior and anterior-inferior ends of the fragment during straight traction of leg, while a rod was pressed on the point of the rotation axis to limit the extra anterior movement (Fig. 2b). Acetabular orientation was then carefully examined on an AP radiograph to ensure no retroversion before the final fixation. Finally, an inclusion of internal rotation in flexion of hip was tested when the correction was completed. In a very shallow acetabulum, more displacement of the acetabular fragment would be needed to acquire a sufficient acetabular coverage of the femoral head, thereby necessitating more rigid fixation than two screws. We have undertaken this procedure recently and obtained encouraging preliminary results.
Fig. 2.
A C-shaped osteotomy performed using a custom-designed curved osteotome. B Completely freed acetabular fragment rotated on the tangential direction of the C-shaped curve by two bone hooks placed on the anterior-superior and anterior-inferior ends of the fragment during straight traction of leg, while a rod was pressed on the point of the rotation axis to limit the extra anterior movement
In summary, CPO is a joint preservation procedure to correct acetabular coverage and to stabilise the hip joint. It achieves improvement of inadequate coverage of the femoral head and reduction of mediolateral displacement. However, a high rate of postoperative acetabular retroversion and decreased hip flexion was noted. Therefore, special consideration for acetabular version must be taken into consideration in the surgical plan and an accurate procedure of manoeuvring the acetabular fragment under the radiographic control is essential to prevent overcorrection of the anterior acetabulum during surgery.
References
- 1.Ganz R, Klaue K, Vinh TS, Mast J. A new periacetabular osteotomy for the treatment of hip dysplasias: technique and preliminary results. Clin Orthop Relat Res. 1988;232:26–36. [PubMed] [Google Scholar]
- 2.Ganz R, Parvizi J, Beck M, Leunig M, Notzli H, Siebenrock KA. Femoroacetabular impingement: a cause for osteoarthritis of the hip. Clin Orthop Relat Res. 2003;417:112–120. doi: 10.1097/01.blo.0000096804.78689.c2. [DOI] [PubMed] [Google Scholar]
- 3.Harris W. Etiology of osteoarthritis of the hip. Clin Orthop Relat Res. 1986;213:20–33. [PubMed] [Google Scholar]
- 4.Kiyama T, Naito M, Shiramizu K, Shinoda T (2007) Postoperative acetabular retroversion causes posterior osteoarthritis of the hip. Int Orthop. doi:10.1007/s00264-007-0507-6 [DOI] [PMC free article] [PubMed]
- 5.Maeyama A, Naito M, Moriyama S, Yoshimura I. Evaluation of dynamic instability of dysplastic hip with use of triaxial accelerometry. J Bone Joint Surg Am. 2008;90:85–92. doi: 10.2106/JBJS.G.00029. [DOI] [PubMed] [Google Scholar]
- 6.Mast JW, Brunner RL, Zebrack J. Recognizing acetabular version in the radiographic presentation of hip dysplasia. Clin Orthop Relat Res. 2004;418:48–53. doi: 10.1097/00003086-200401000-00009. [DOI] [PubMed] [Google Scholar]
- 7.Myers SR, Eijer H, Ganz R. Anterior femoroacetabular impingement after periacetabular osteotomy. Clin Orthop Relat Res. 1999;363:93–99. doi: 10.1097/00003086-199906000-00012. [DOI] [PubMed] [Google Scholar]
- 8.Naito M, Shiramizu K, Akiyoshi Y, Ezoe M, Nakamura Y. Curved periacetabular osteotomy for treatment of dysplastic hip. Clin Orthop Relat Res. 2005;433:129–135. doi: 10.1097/01.blo.0000153281.75265.1d. [DOI] [PubMed] [Google Scholar]
- 9.Ninomiya S. Rotational acetabular osteotomy for the severely dysplastic hip in the adolescent and young adult. Clin Orthop Relat Res. 1989;247:127–137. [PubMed] [Google Scholar]
- 10.Nozawa M, Maezawa K, Matsuda K, Kim S, Shitoto K, Kurosawa H (2008) Rotational acetabular osteotomy for advanced osteoarthritis of the hip joint with acetabular dysplasia. Int Orthop. doi:10.1007/s00264-008-0657-1 [DOI] [PMC free article] [PubMed]
- 11.Peters CL, Erickson JA, Hines JL. Early results of the Bernese periacetabular osteotomy: the learning curve at an academic medical center. J Bone Joint Surg Am. 2006;88:1920–1926. doi: 10.2106/JBJS.E.00515. [DOI] [PubMed] [Google Scholar]
- 12.Petersen DR, Brand RA, Davy DT. Pelvic muscle and acetabular contact forces during gait. J Biomech. 1997;30:959–965. doi: 10.1016/S0021-9290(97)00041-9. [DOI] [PubMed] [Google Scholar]
- 13.Reynolds D, Lucas J, Klaue K. Retroversion of the acetabulum. A cause of hip pain. J Bone Joint Surg Br. 1999;81:281–288. doi: 10.1302/0301-620X.81B2.8291. [DOI] [PubMed] [Google Scholar]
- 14.Salter RB. Innominate osteotomy in the treatment of congenital dislocation and subluxation of the hip. J Bone Joint Surg Am. 1961;43B:518–539. [PubMed] [Google Scholar]
- 15.Shinoda T, Naito M, Nakamura Y, Kiyama T (2007) Periacetabular osteotomy for the treatment of dysplastic hip with Perthes-like deformities. Int Orthop. doi:10.1007/s00264-007-0476-9 [DOI] [PMC free article] [PubMed]
- 16.Siebenrock KA, Schoeniger R, Ganz R. Anterior femoro-acetabular impingement due to acetabular retroversion. Treatment with periacetabular osteotomy. J Bone Joint Surg Am. 2003;85:278–286. doi: 10.2106/00004623-200302000-00015. [DOI] [PubMed] [Google Scholar]
- 17.Siebenrock KA, Kalbermatten DF, Ganz R. Effect of pelvic tilt on acetabular retroversion: a study of pelvis from cadavers. Clin Orthop Relat Res. 2003;407:241–248. doi: 10.1097/00003086-200302000-00033. [DOI] [PubMed] [Google Scholar]
- 18.Solomon L. Patterns of osteoarthritis of the hip. J Bone Joint Surg Br. 1976;58:176–183. doi: 10.1302/0301-620X.58B2.932079. [DOI] [PubMed] [Google Scholar]
- 19.Steel HH. Triple osteotomy of the innominate bone. J Bone Joint Surg Am. 1973;55A:343–350. [PubMed] [Google Scholar]
- 20.Tönnis D, Arning A, Bloch M, et al. Triple pelvic osteotomy. J Pediatr Orthop. 1994;3:54–67. [Google Scholar]
- 21.Tönnis D, Heinecke A. Acetabular and femoral anteversion: relationship with osteoarthritis of the hip. J Bone Joint Surg Am. 1999;81:1747–1770. doi: 10.2106/00004623-199912000-00014. [DOI] [PubMed] [Google Scholar]
- 22.Visser JD, Jonkers A, Hillen B. Hip joint measurements with computerized tomography. J Pediatr Orthop. 1982;2:143–146. doi: 10.1097/01241398-198202020-00005. [DOI] [PubMed] [Google Scholar]