Abstract
We present our series of 72 patients with periprosthetic fractures. The Vancouver classification was used to evaluate the fractures; there was one type A, seven type B1, 42 type B2, 17 type B3 and five type C fractures. Demographics, pre and postoperative data using Charnley–D’Aubigne-Postel score for assessment of function were recorded. The mean follow-up for all patients was two years. The overall outcome of treatment was graded as excellent, good or poor. An excellent result indicated that the arthroplasty was stable with minimal deformity and no shortening. Stable subsidence of the prosthesis or when the fracture healed with moderate deformity or shortening was deemed as a good result. A loose prosthesis, nonunion, sepsis, severe deformity or shortening was considered poor. In our series 79% (n = 57) had good or excellent results following surgical intervention and 21% (n = 15) had complications; they all had undergone re-operation for various reasons such as nonunion, loosening, dislocation or infection. In B2 fractures the stem is unstable and hence revision of the prosthetic stem has been recommended with or without additional fixation. For B3 fractures an allograft prosthesis composite or tumour prosthesis is considered the treatment choice.
Introduction
The indications of joint replacements have increased considerably, and so have the revision arthroplasty rates [14]. The increasing incidence of periprosthetic fractures is attributed to an elderly population and the need for revision surgery [1, 14, 21]. The reported incidence of periprosthetic femoral fractures is 1% (238 of 23,980) for primary joint replacement and 7.8% (497 of 6349) for revision hip surgery [1]. The Mayo clinic reports an accumulated incidence of 0.6% in primary cemented total hip arthroplasty (THA) and 0.4% in primary uncemented THA performed between 1969 and 1990 [13]. The accumulated incidence was 0.4% for the primary group and 2.1% for the revised group from data published by Lindahl et al. [15].
Treatment of these fractures ranges from nonoperative intervention to complex, expensive revision procedures [16]. The morbidity is increased by pre-existing medical factors in the elderly population [16]. The surgical intervention most often poses a challenge to the surgeon as he not only has to solve the problems of aseptic loosening but also has to take into account the amount of bone loss, the fracture pattern and the integrity of the implant itself in a single procedure [18]. We used the Vancouver classification of postoperative periprosthetic fractures which has been developed and validated to address not just the fracture pattern but also takes into account the implant stability and the bone loss associated with it [2, 3, 5].
Materials and methods
We retrospectively reviewed periprosthetic femoral fractures over a ten-year period from 1995 to 2005 presenting to our institution and managed by a single surgeon. All cases were retrieved from a database of the operating surgeon. A total of 72 patients were identified; we were unable to classify entirely based on radiographs and hence descriptive data regarding fracture were obtained from operative notes. The Vancouver classification was used to evaluate the fractures. The Charnley prefixes A, B, and C were used to facilitate assessment of function of walking. All patients were followed-up for a minimum of two years. All data was entered at the time of each follow-up during the two-year period.
The data collected included time to radiological union. Plain radiographs were examined for evidence of nonunion, infection, loosening and subsidence. Fractures were considered to be united clinically when the patient could fully weight bear with no pain. The operative approach in cases of surgical fixation was noted. A modified Charnley–D’Aubigne Postel score was used. Complications with regards to fixation techniques were also recorded. The overall outcome of treatment was graded as excellent, good or poor. An excellent result indicates that the arthroplasty was stable with minimal deformity and no shortening. Stable subsidence of the prosthesis, or when the fracture healed with moderate deformity or shortening, was deemed as a good result. A loose prosthesis, nonunion, sepsis, severe deformity or shortening was considered poor. A survey of the patient satisfaction score was done at each follow-up.
Results
Of the 72 patients, 51 females and 21 males, who sustained a periprosthetic femoral fracture the average age was 74.2 (57.2–100.8) years. All fractures were sustained following a fall from a standing height. There were 41 right and 31 left hips in the study. Average time from index procedure was 6.7 years (1.4–27.7 years). The average time to union was four months. A total of 81% of periprosthetic fractures occurred in total hip arthroplasty (n = 58), and 19% of patients had uncemented hemiarthroplasties (n = 14). Of the periprosthetic fractures, 76% occurred in cemented prostheses, which included both primary (n = 40) and revision prostheses (n = 15). Twenty-four percent involved an uncemented prosthesis (n = 17) (Tables 1 and 2).
Table 1.
Types of the primary prostheses
| Type of prosthesis | Number of patients |
|---|---|
| Hemiarthroplasty (uncemented) | 14 |
| THA (cemented) | 40 |
| THA (uncemented) | 3 |
| Revision THA (cemented) | 15 |
| Total | 72 |
THA total hip arthroplasty
Table 2.
Treatment and outcome
| Fracture type | Treatment method | Outcome | ||
|---|---|---|---|---|
| Excellent | Good | Poor | ||
| A (N = 1) | Conservative | 1 | - | - |
| B1 (N = 7) | DCP (3) | 1 | 1 | 1 non-union |
| Long stem revision (4) | 2 | - | 1 dislocation, 1 infected nonunion | |
| B2 (N = 42) | Long stem revision alone (19) | 14 | 5 | - |
| Long stem revision with DCP (8) | 5 | 3 | - | |
| Distal locking long stem revision (15) | 6 | 3 | 2 dislocation, 3 stem subsidence, 1 nonunion | |
| B3 (N = 17) | Distal locking long stem revision (8) | 3 | 2 | 3 stem subsidence |
| Long stem revision alone (9) | 4 | 2 | 3 infection | |
| C (N = 5) | ORIF (4) | 3 | 1 | - |
| Distal locking long stem revision (1) | - | 1 | - | |
| Total | 39 (54%) | 18 (25%) | 15 (21%) | |
DCP dynamic compression plate, ORIF open reduction internal fixation
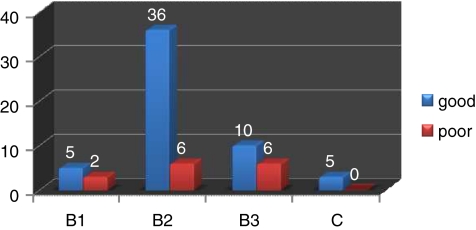
There were seven B1 fractures, 42 B2, 17 B3 and five C fractures; there was only one type A fracture, which was treated nonoperatively. Three out of seven B1 fractures were treated with dynamic compression plating (DCP); one had a nonunion. Four out of seven were treated with long-stemmed prosthesis; of these one had dislocation and the others had infected nonunion. Twenty-seven patients with B2 fractures were treated with long stem revisions; eight of 27 had additional fixation (DCP). Fracture union was achieved in all. Fifteen of 42 had distal locking long stem revision prosthesis among which there were two cases of infections, two dislocations, three stem subsidences and one nonunion which required further revision. Eight out of 17 B3 fractures were treated with distal locking long stem revision prosthesis; one had a wound infection and three had an unstable stem with subsidence that required revision. Nine had a long stem revision alone; of these there were three cases of wound infection; two treated with two-staged revisions and one with excision arthroplasty. In type C, one had distal locking revision prosthesis and the remaining four were treated with open reduction internal fixation (ORIF); all of these fractures united successfully (Table 3).
Table 3.
Fracture versus outcome
In our series 79% (n = 57) had good or excellent results following surgical intervention and 21% (n = 15) had complications; they all had undergone re-operation for various reasons such as nonunion, loosening, dislocation or infection. Twenty-one percent (n = 15) of the periprosthetic femoral fractures were augmented with bone graft Figs. 1, 2, 3, 4.
Fig. 1.

B3 periprosthetic femoral fracture
Fig. 2.

Implant subsidence seen in B3 fracture treated with long stem revision
Fig. 3.

B3 fracture treated with long stem revision
Fig. 4.

Distal locking prosthesis with screw breakage
Discussion
Periprosthetic fractures are difficult to manage [7]. There is an increasing incidence of late postoperative periprosthetic femoral fractures that is attributable to many factors including an increasing number of elderly patients at risk for falls, increasing numbers of young patients with total hip replacements at risk for high-energy trauma events, and the increasing numbers of revision procedures using cementless press-fit fixation or bone impaction allograft techniques [1, 9]. Periprosthetic femoral fractures usually occur with low energy events, either after falls or spontaneously during activities of daily living [17]. Despite different classification systems and treatment methods, the ideal solution for this entity has always been a dilemma [7]. In recent years great advances in prosthetic designs such as distal locking modular revision prosthesis, fixed angle locking plates, and usage of cortical onlay grafts have improved the outcomes of these fractures [6, 11, 18, 19]. Our study examined the demography, patterns of fracture, treatment modalities and rate of failure in patients having operative treatment for postoperative periprosthetic fracture of femur. In the B1 group failure may be attributed to the misinterpretation of radiographs based on Vancouver classification as can be seen from our small series where four of the B1 fractures had stem revisions intraoperatively due to prosthetic stems being loose [15, 17]. In our series of B2 fractures in both cemented and uncemented revisions, union was achieved in all except one.
Failure rates were high in this series for B3 fractures. The failures in B3 can be attributed to deficiency in restoration of bone stock and failure in addressing cortical deficiency. Ideally in these cases the main modality of treatment should be proximal femoral replacement using tumour prosthesis or allograft prosthesis composite [12, 20]. Type C fractures ORIF is an effective method of treatment and is comparable to other studies [4, 8, 10]. Therefore it is of prime importance to tailor treatment to each individual patient based on the fracture personality.
Conclusion
Surgical decision making in this complex group is influenced by various factors such as the patient’s age, gender, comorbidity, mobility prior to surgical intervention, femoral anatomy, bone stock quality, type and size of the prosthesis, surgical approaches and techniques. A systematic approach is necessary which is provided by the Vancouver classification to achieve the best outcome. By identifying the high risk groups (recurrent dislocation, loosening, subsidence and osteolysis) and persistent surveillance of clinical and radiological follow-up failures can be avoided.
References
- 1.Berry DJ. Epidemiology: hip and knee. Orthop Clin North Am. 1999;30(2):183–190. doi: 10.1016/S0030-5898(05)70073-0. [DOI] [PubMed] [Google Scholar]
- 2.Brady OH, Garbuz DS, Masri BA, Duncan CP. Classification of the hip. Orthop Clin North Am. 1999;30(2):215–220. doi: 10.1016/S0030-5898(05)70076-6. [DOI] [PubMed] [Google Scholar]
- 3.Brady OH, Garbuz DS, Masri BA, Duncan CP. The reliability and validity of the Vancouver classification of femoral fractures after hip replacement. J Arthroplasty. 2000;15(1):59–62. doi: 10.1016/S0883-5403(00)91181-1. [DOI] [PubMed] [Google Scholar]
- 4.Chakravarthy J, Bansal R, Cooper J. Locking plate osteosynthesis for Vancouver type B1 and type C periprosthetic fractures of femur: a report on 12 patients. Injury. 2007;38(6):725–733. doi: 10.1016/j.injury.2007.02.038. [DOI] [PubMed] [Google Scholar]
- 5.Duncan CP, Masri BA. Fractures of the femur after hip replacement. Instr Course Lect. 1995;44:293–304. [PubMed] [Google Scholar]
- 6.Eingartner C, Volkmann R, Putz M, Weller S. Uncemented revision stem for biological osteosynthesis in periprosthetic femoral fractures. Int Orthop. 1997;21(1):25–29. doi: 10.1007/s002640050112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Franklin J, Malchau H. Risk factors for periprosthetic femoral fracture. Injury. 2007;38(6):655–660. doi: 10.1016/j.injury.2007.02.049. [DOI] [PubMed] [Google Scholar]
- 8.Fulkerson E, Tejwani N, Stuchin S, Egol K. Management of periprosthetic femur fractures with a first generation locking plate. Injury. 2007;38(8):965–972. doi: 10.1016/j.injury.2007.02.026. [DOI] [PubMed] [Google Scholar]
- 9.Garbuz DS, Masri BA, Duncan CP. Periprosthetic fractures of the femur: principles of prevention and management. Instr Course Lect. 1998;47:237–242. [PubMed] [Google Scholar]
- 10.Giannoudis PV, Kanakaris NK, Tsiridis E. Principles of internal fixation and selection of implants for periprosthetic femoral fractures. Injury. 2007;38(6):669–687. doi: 10.1016/j.injury.2007.02.050. [DOI] [PubMed] [Google Scholar]
- 11.Haddad FS, Duncan CP, Berry DJ, Lewallen DG, Gross AE, Chandler HP. Periprosthetic femoral fractures around well-fixed implants: use of cortical onlay allografts with or without a plate. J Bone Joint Surg Am. 2002;84-A(6):945–950. [PubMed] [Google Scholar]
- 12.Kellett CF, Boscainos PJ, Maury AC, Pressman A, Cayen B, Zalzal P, Backstein D, Gross A. Proximal femoral allograft treatment of Vancouver type-B3 periprosthetic femoral fractures after total hip arthroplasty. Surgical technique. J Bone Joint Surg Am. 2007;89(Suppl 2 Pt.1):68–79. doi: 10.2106/JBJS.F.01047. [DOI] [PubMed] [Google Scholar]
- 13.Lewallen DG, Berry DJ. Periprosthetic fracture of the femur after total hip arthroplasty: treatment and results to date. Instr Course Lect. 1998;47:243–249. [PubMed] [Google Scholar]
- 14.Lindahl H. Epidemiology of periprosthetic femur fracture around a total hip arthroplasty. Injury. 2007;38(6):651–654. doi: 10.1016/j.injury.2007.02.048. [DOI] [PubMed] [Google Scholar]
- 15.Lindahl H, Malchau H, Herberts P, Garellick G. Periprosthetic femoral fractures classification and demographics of 1049 periprosthetic femoral fractures from the Swedish National Hip Arthroplasty Register. J Arthroplasty. 2005;20(7):857–865. doi: 10.1016/j.arth.2005.02.001. [DOI] [PubMed] [Google Scholar]
- 16.Lindahl H, Oden A, Garellick G. The excess mortality due to periprosthetic femur fracture. A study from the Swedish national hip arthroplasty register. Bone. 2007;40(5):1294–1298. doi: 10.1016/j.bone.2007.01.003. [DOI] [PubMed] [Google Scholar]
- 17.Masri BA, Meek RM. Periprosthetic fractures evaluation and treatment. Clin Orthop Relat Res. 2004;420:80–95. doi: 10.1097/00003086-200403000-00012. [DOI] [PubMed] [Google Scholar]
- 18.O'Shea K, Quinlan JF, Kutty S, Mulcahy D. The use of uncemented extensively porous-coated femoral components in the management of Vancouver B2 and B3 periprosthetic femoral fractures. J Bone Joint Surg Br. 2005;12:1617–1621. doi: 10.1302/0301-620X.87B12.16338. [DOI] [PubMed] [Google Scholar]
- 19.Tsiridis E, Narvani AA, Timperley JA, Gie GA. Dynamic compression plates for Vancouver type B periprosthetic femoral fractures: a 3-year follow-up of 18 cases. Acta Orthop. 2005;76(4):531–537. doi: 10.1080/17453670510041529. [DOI] [PubMed] [Google Scholar]
- 20.Tsiridis E, Spence G, Gamie Z, El Masry MA, Giannoudis PV. Grafting for periprosthetic femoral fractures: strut, impaction or femoral replacement. Injury. 2007;38(6):688–697. doi: 10.1016/j.injury.2007.02.046. [DOI] [PubMed] [Google Scholar]
- 21.Wal BC, Vischjager M, Grimm B, Heyligers IC, Tonino AJ. Periprosthetic fractures around cementless hydroxyapatite-coated femoral stems. Int Orthop. 2005;29(4):235–240. doi: 10.1007/s00264-005-0657-3. [DOI] [PMC free article] [PubMed] [Google Scholar]