Abstract
Twenty-five post-traumatic leg length discrepancies combined with axial deviation in 22 patients were treated with the Taylor spatial frame. We retrospectively analysed the accuracy of correction, the complication rate and the clinical outcome including the duration of treatment. The cases were divided into three sub-groups according to the level of the osteotomy. The mean age at operation was 22.7 years; the mean follow-up was 21.1 months. The patients presented uniplanar and multiplanar deformities in combination with leg length discrepancy. Twenty-one of 25 cases showed a frontal plane malalignment preoperatively. Only three of those 21 cases continued to show minimal malalignment postoperatively. The preoperative mechanical axis deviation present in 15 of 17 lower extremities was fully corrected in 13 extremities. The 25 lengthening and correction procedures were associated with a total of 61 difficulties, including 44 problems, seven obstacles and ten complications. In conclusion, the Taylor spatial frame allows accurate results in correction of complex post-traumatic deformities with minimal morbidity.
Introduction
The management of post-traumatic deformities of the lower limb, either occurring immediately after failed primary fracture treatment leading to malunion, or developing gradually caused by injury of the growth mechanism, is a continuing challenge facing the orthopaedic surgeon. In particular, leg length discrepancy or soft-tissue compromise limit the options for acute correction and internal fixation.
External fixation for the management of femoral and tibial post-traumatic deformities has become a standard procedure over recent decades. Better understanding of the reaction of bone and soft tissue to gradual distraction has resulted in a reduction of the historically high complication rate and improvement of functional outcome in correction of severe deformities with or without leg length discrepancy [2, 14].
The correction of deformities using the classic Ilizarov ring fixator has been reported in literature with good results even in the presence of soft-tissue compromise.
However, residual malalignment after correction of multiplanar deformities is a common problem [17], as complex modifications of the Ilizarov frame would be necessary for those corrections.
With the introduction of the Taylor spatial frame a new device for deformity correction and lengthening was made available. It allows simultaneous correction of deformities in all possible planes without frame modification.
The Taylor spatial frame is a modular circular external fixation system using the same methods of frame attachment and the same gradual correction principles known from the Ilizarov device. The main elements of this new fixator are two rings connected by six telescopic struts. By adjusting only the strut lengths, one ring can be repositioned with respect to the other in all dimensions of space.
A web-based software program is used to calculate a daily prescription schedule for strut adjustment. In cases of residual axial malalignment or planned staged correction of a deformity, a second program can easily be created.
The Taylor spatial frame was introduced to our department in 1999 and has been used for most external fixation cases since then. We have carried out a retrospective study of a consecutive case series of patients treated with the Taylor spatial frame for post-traumatic deformities of the lower limb.
The aim of the study was to analyse the accuracy of correction with regard to a three-dimensional approach, the complication rate and the clinical outcome including the duration of treatment. We postulated that the possibility of a three-dimensional correction would result in less residual deformities after correction.
Material and methods
Patients were extracted from our prospective patient database of cases treated with external fixation since 1990. Inclusion criteria were: (1) post-traumatic deformity, (2) treatment with the Taylor spatial frame (Smith & Nephew, Inc; Memphis, Tennessee), and (3) frame removal before June 2004. Exclusion criteria were defined as: (1) follow-up of less than one year, (2) TSF for segmental bone transport, and (3) missing long-standing radiographs of the lower extremity before and after operation or at the time of the last follow-up.
All operations were performed under general anaesthesia with the patient in supine position. The apparatus was assembled preoperatively to roughly mimic the deformity. For fixation of the rings to the bone, both wires and halfpins were used. After attachment of both rings and measurement of the mounting parameters, the struts were partially removed and the osteotomy was performed. In the femur and the tibia the drill-hole technique was applied, and for the fibula osteotomy an oscillating saw was used. Distraction was started five to seven days after the operation following the time schedule provided by the computer program.
In cases of tibial lengthening of more than 3 cm, the frame was extended distally, including the foot, in order to avoid development of equinus deformity in the ankle. To improve range of motion in the ankle joint, this foot ring was removed in an additional elective operation two to three months after frame attachment, when the soft tissues had already gained sufficient length, to enable range of motion exercises in the ankle. In cases of distal tibial osteotomies with short distal fragments the frame was extended across the ankle to avoid the development of equinus contracture and to achieve more stability during angular correction.
Daily physiotherapy to maintain and enhance the range of motion in the hip, knee and ankle was started one or two days postoperatively. Furthermore, the patients were advised to perform range-of-motion exercises for the individual joints at home. During the postoperative period the patients were instructed in pin-site care and strut adjustment.
The demographic data of all patients and all mean values including the standard deviations are reported.
Main outcome measures were the alignment of the lower limb after frame removal and at the time of final follow-up assessed using the malalignment test [23, 24]. This included the mechanical axis deviation (MAD), the mechanical lateral distal femoral angle (mLDFA), the posterior distal femoral angle (PDFA), the medial proximal tibial angle (MPTA), the posterior proximal tibial angle (PPTA), the lateral distal tibial angle (LDTA) and the anterior distal tibial angle (ADTA).
Secondary outcome measures were the functional outcome, the duration of treatment and the complication rate. The range of motion of the knee and ankle joint were assessed to describe the functional outcome. To analyse the duration of treatment, the healing index was calculated.
Complications were graded according to Paley et al. into problems, obstacles and complications [22]. Problems are defined as difficulties that arise during treatment and can be fully resolved by nonoperative intervention before the end of treatment, whereas obstacles are difficulties that arise during treatment and can be fully resolved by operative intervention before the end of treatment. According to Paley et al., all intraoperative neural and vascular injuries and all problems during lengthening that are not resolved before the end of treatment are considered true complications. True complications are further subdivided into minor and major complications, according to their clinical importance.
Additionally, the cases were divided into three subgroups according to the affected bone and the osteotomy level with group 1 including corrections at the distal femur, group 2 at the proximal tibia and group 3 at the distal tibia.
Results
Twenty-two patients were included in the study. There were 11 female and 11 male patients with a mean age at the time of trauma of 14.3 years (range, 2–46 years). The mean age at the time of correction was 22.7 years (range, 12–48 years) while the mean period between occurrence of trauma and deformity correction was 8.2 years (range, 6 months to 27 years). The mean duration of follow-up was 21.1 months (range, 12–43 months).
The most common mechanisms of injury were motor vehicle accidents, sports accidents, bicycle accidents or falls. In 18 patients the limb length discrepancy and deformity resulted from an injury of a growth plate. Four patients sustained trauma after physeal closure of the individual limb segment which resulted in a malunion.
A total of 24 limb segments (9 femurs, 15 tibias) in 22 patients were treated.
One female patient consecutively underwent bilateral correction of both tibias. In one limb concomitant correction of the femur and the tibia was performed by the use of a separate frame for each limb segment. Another male patient underwent a two-level lengthening of the tibia, using a three ring frame (Fig. 1). The two-level tibia lengthening was split in two separated cases. A total of 25 lengthening and correction procedures were analysed.
Fig. 1.
This patient presented a posttraumatic mid-diaphyseal varus deformity of 8 degrees, a recurvatum deformity of 10 degrees, an internal rotation deformity of 15 degrees and a shortening of 32 mm (a, b). A bi-level Taylor spatial frame was used for simultaneous deformity correction in the mid-diaphyseal area and lengthening at the proximal metaphysis (c–f). A full correction of the mechanical axis and the joint orientation angles with a good clinical and cosmetic result was achieved (g–j)
Axial deformities (valgus, varus, procurvatum, recurvatum) were present in 21 of 25 cases: 16 cases had pure frontal plane angulations, five cases had oblique plane angulation (combined frontal plane and sagittal plane angulation), and three cases showed rotation malalignment. In three patients only lengthening was performed. Twelve deformities had a mean valgus angulation of 6.9 ± 5.5 degrees (range, 2–23 degrees), and nine cases had a mean varus angulation of 13.2 ± 8.65 degrees (range, 3–30 degrees). Four cases had a mean recurvatum deformity of 13.8 ± 4.1 degrees (range, 10–20 degrees), and one case had a 10-degree procurvatum deformity. Three cases had a mean rotational deformity of 12.7 ± 5.6 degrees (range, 5–18 degrees).
The overall mean preoperative leg length discrepancy was 27.6 ± 14.7 mm (range, 3–61 mm). The mean amount of lengthening was 27.0 ± 14.8 mm (range, 3–62 mm).
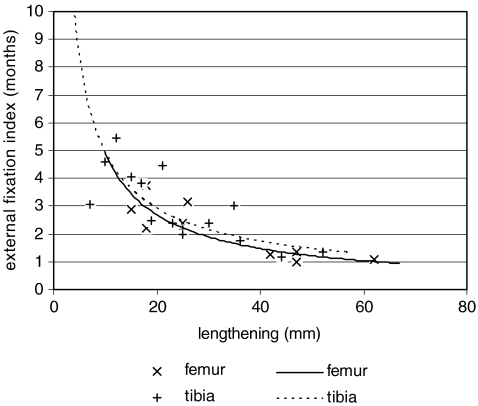
The mean duration of external fixation, beginning with the application of the Taylor spatial frame and ending with frame removal, was 6.0 ± 1.7 months (range, 2.1–10.6 months). The mean external fixation index, calculated as the number of months of external fixation per centimetre of lengthening, of all corrections was 3.2 ± 2.9 months per centimetre (range, 1.0–16 months per centimetre). Figure 2 shows the external fixation index of all femoral and tibial lengthenings relative to the amount of lengthening.
Fig. 2.
External fixation index relative to amount of lengthening of all femoral and tibial corrections
For lengthenings smaller than 30 mm the mean external fixation index was higher and the variation of the index was larger than the index and the variation for lengthenings of 30 mm and more. The mean external fixation index for femoral corrections was lower than the index for proximal tibial and distal tibial corrections. The index for proximal tibial corrections was lower than the index for distal tibial corrections (Table 1).
Table 1.
Mean external fixation index of all groups
| Description | Total | Group 1 | Group 2 | Group 3 |
|---|---|---|---|---|
| Number of cases | 25 | 9 | 9 | 7 |
| Mean external fixation index (months) | 3.2 | 2.1 | 2.8 | 4.7 |
| Mean amount of lengthening (mm) | 27.0 | 33.3 | 24.2 | 22.3 |
Twenty-one of 25 cases showed a frontal plane malalignment preoperatively. Three of those 21 cases still showed malalignment postoperatively with a residual deviation of less then 2 degrees outside of the normal range.
Seven of the twelve deformities in the sagittal plane were not addressed by treatment intentionally, as the adjacent joint range of motion was normal. In the remaining five cases, restoration of normal joint orientation was performed without a residual deformity.
The preoperative mechanical axis deviation present in 15 of 17 lower extremities was fully corrected in 13 extremities. Two lower extremities showed a residual MAD of 16 and 17 mm lateral, respectively.
The radiographs obtained immediately after frame removal were compared to follow-up radiographs to identify postoperative changes. Only one case showed a significant change of the axial alignment (more then 2 degrees joint orientation angle or 3 mm MAD) and presented a late bowing, resulting in a decreased MPTA.
The 25 lengthening and correction procedures were associated with a total of 61 difficulties, including 44 problems, seven obstacles and ten complications (Table 2).
Table 2.
Problems, obstacles and complications for all three groups
| Difficulties | Total | Group 1 | Group 2 | Group 3 |
|---|---|---|---|---|
| Problems | 44 | 19 | 11 | 14 |
| Pin infection | 32 | 15 | 8 | 9 |
| Delayed ossification | 6 | 2 | 0 | 4 |
| Obstacles | 7 | 1 | 3 | 3 |
| Pin removal | 6 | 1 | 3 | 2 |
| Pin renewal | 1 | 0 | 0 | 1 |
| Complications | 10 | 2 | 5 | 3 |
| Limited range of motion | 3 | 1 | 0 | 2 |
| Late bowing | 1 | 0 | 1 | 0 |
| Nerve injury | 3 | 0 | 3 | 0 |
| Axial deviation | 3 | 1 | 1 | 1 |
Pin infections were treated successfully by oral antibiotics in 32 cases. In six cases the pins had to be removed, and a new pin was inserted in one case. A delayed consolidation was seen in six cases, with four in the distal tibia, which all healed without any intervention. The late bowing occurred during the first two months after apparatus removal and produced a change in the MPTA from 88 degrees to 85 degrees. Three patients that had normal range of motion preoperatively developed a limited range of motion in the knee (ROM 0-0-120) or in the ankle joint (ROM 5-0-40, ROM 0-0-40) at the last follow-up. Intraoperative nerve injuries (N. peroneus profundus) occurred in three cases. These patients were treated with physiotherapy and electro-stimulation. Although the nerve function completely recovered in all cases without any surgical intervention, they were considered as true complications with respect to classification. Additionally, the three cases that developed axial deviations at the last follow-up were considered as complications.
In group 1 the mean preoperative lateral distal femoral angle (LDFA) was 84.4 ± 9.8 degrees (range, 64–100 degrees). The mean postoperative LDFA was 88.3 ± 1.5 degrees (range, 85–90 degrees). The mean preoperative MAD (absolute value) was 36.8 ± 18.3 mm (range, 10–80 mm). After lengthening and correction, two cases still had an abnormal mechanical axis deviation (MAD). One case showed a postoperative LDFA of 85 degrees with a MAD of 16 mm lateral, and another case with a LDFA of 89 showed a MAD of 17 mm lateral due to an inaccurate correction in the proximal tibia (postoperative MPTA 92 degrees). The mean postoperative MAD (absolute value) was 7.1 ± 5.2 mm (range, 2–17 mm). The mean lengthening was 33.3 ± 15.6 mm (range, 15–62 mm).
In group 2 a preoperative leg length discrepancy was seen in all nine cases (23.4 ± 13.3 mm, range 3–48 mm), with two cases requiring simultaneous valgus correction of the tibia. In three cases, in addition to lengthening, correction of tibial recurvatum and valgus was performed. One case had simultaneous lengthening and correction of an external rotational deformity of 15 degrees.
Preoperatively, the medial proximal tibial angle (MPTA) was outside of the normal range (85–90 degrees) in five cases with a mean MPTA of 92.4 ± 1.5 degrees (range, 91–95 degrees). One of the five cases still had an abnormal MPTA of 92 degrees after lengthening and correction, caused by undercorrection. Postoperatively, the mean MPTA of all cases was 88.6 ± 1.5 degrees (range, 87–92 degrees). The mean preoperative MAD (absolute value) of this group was 14.7 ± 13.3 mm (range 1–38 mm). Postoperatively, the mean MAD (absolute value) of all cases of this group was 6.0 ± 4.4 mm (range, 0–17 mm).
Three cases presented recurvatum with a mean PPTA of 96.7 ± 5.3 degrees (range, 90–103 degrees) that resulted in an abnormal range of motion. The recurvatum deformity was fully corrected with a postoperative mean PPTA of 82 ± 0.8 degrees (range, 81–83 degrees).
Lengthening was performed in all nine cases (mean lengthening 2.4 ± 1.2 cm, range 0.7–5.2 cm). All patients in this group regained preoperative knee flexion within six months after frame removal.
In group 3 all cases required lengthening and simultaneous correction of either distal tibial varus or valgus angulation. Six deformities with a mean varus of 14.8 degrees (range, 6–30 degrees) and one ten-degree valgus deformity were treated. One case with varus showed an additional internal rotation of five degrees. In another case of diaphyseal varus a ten-degree extension deformity was corrected simultaneously.
The mean magnitude of the preoperative leg length discrepancy was 25.8 ± 14.4 mm (range, 8–49 mm). The level of osteotomy was metaphyseal in five tibias and diaphyseal in two. The mean preoperative LDTA was 101 ± 13.1 degrees (range, 80–120 degrees). The LDTA was corrected in all but one case, which showed a postoperative LDTA of 93 degrees. The mean postoperative LDTA of group 3 was 90.3 ± 2.9 degrees (range, 84–93 degrees). The mean amount of lengthening was 22.3 ± 13.1 cm (range, 3–44 mm), and the limb length was equalised in all cases within 1 cm.
Five of the seven had regained more than 85% of the preoperative range of motion by six months after frame removal. At the latest follow-up visit no difference to the preoperative range of motion was found in these five cases.
Two cases had a normal range of motion of the ankle preoperatively, but limitation of dorsiflexion at the last follow-up caused by distinct osteoarthritis that developed during and after lengthening and correction. Initial signs of osteoarthritis were found in both ankles in preoperative radiographs. Radiographs obtained after frame removal showed aggravation of osteoarthritis. Maximal dorsiflexion in these two cases was zero degrees and five degrees, respectively.
Discussion
Our study showed that the Taylor spatial frame allows for accurate correction of post-traumatic deformities in all planes. Three patients had leg length discrepancy only. Sixteen patients had a frontal (varus/valgus) malalignment, five patients a combination of a frontal and sagittal deformity and an additional rotational deformity was present in three of these cases. All sagittal and rotational deformities were fully corrected. Only two cases showed a residual mechanical axis deviation at the last follow-up. One case showed a MAD of 16 mm lateral due to a LDFA of 85 degrees, and another patient showed a MAD of 17 mm lateral as the result of a MPTA of 92 degrees. The only additional malorientation of a joint angle was seen in a distal tibia with an LDTA of 93 degrees, which presented a normal MAD of 5 mm medial. Thus, only 8% showed a residual MAD over 10 mm.
Tetsworth et al. was one of the first who reported on the correction of complex lower-limb deformities with the Ilizarov fixator [25]. Deformity correction involved 36 limb segments in 28 limbs. In six of 28 limbs (21%) the residual MAD was greater than 10 mm. In eight of 14 cases with distal femoral malalignment the femoral joint orientation was restored to within three degrees of the normal value (57%). In 17 of 22 cases (77%) proximal tibial joint orientation was restored to within three degrees of the normal value. We achieved a higher accuracy of correction in our case series. However, their article reports on a very heterogenic group of patients including many hereditary diseases.
The accuracy of the TSF versus the Ilizarov ring fixator (IRF) was evaluated in a study by Manner et al. who compared the final result after frame removal with the initial aim of deformity correction and lengthening [17]. A total of 278 consecutive lower-limb deformity corrections treated either with the TSF or IRF were evaluated. Of the 79 cases treated with the IRF, there was no residual deformity in 44 cases (55.7%). Of the 129 cases treated with TSF, there was no residual deformity in 117 cases (90.7%). In both groups, one essential finding was obvious. With rising dimensions of axial corrections, an increasing percentage of residual deformities could be seen. The goal of treatment in one-dimensional corrections was achieved in 79.3% of the IRF cases and in 100% of the TSF cases; similarly, in two-dimensional corrections, the goal of treatment was achieved in 48.6% of the IRF cases and in 91.8% of the TSF cases, while in three-dimensional corrections it occurred in 28.6% of the IRF cases and 91.1% of the TSF cases. And lastly, in four-dimensional corrections the goal was not achieved in the IRF case but in 66.7% of the TSF cases. In conclusion, their study showed clear advantages of the TSF compared to the Ilizarov ring fixator in complex multiplanar deformities. In our case series nine patients had a multi-dimensional deformity, which was corrected simultaneously. No frame modification or hinge modifications were necessary in our cases of multidimensional corrections using the TSF as the virtual hinge was placed or changed by programming the mounting parameters in the software. In our series we treated deformities up to 30 degrees in the frontal plane. Theoretically there are limitations in the amount of correction due to ring size and strut length; we saw no limits in adolescent and adult cases.
Most reports on deformity correction using the Taylor spatial frame describe rather small, nonconsecutive case series or series with heterogenic patient populations with only one to 14 post-traumatic cases [4, 5, 9, 18–21, 24, 26]. However, almost all of them reported that the TSF compares favourably with standard external ring fixators, especially with regard to accuracy and patient comfort. We found that patients prefer the easy handling of the graduated colour-coded struts and the distraction schedule.
Kristiansen et al. reported on a series of 20 cases treated with a TSF including 12 post-traumatic deformities [15]. However, they mainly described the complication rate and the lengthening index and compared the results to a series of patients treated with the Ilizarov ring fixator. The complication rate or lengthening index is not reported for the post-traumatic cases separately.
Feldmann et al. reported on 18 patients treated for tibial malunion and non-union using the TSF [10]. Unlike our patients, the patients in their series, with a mean age of 29.6 years (range, 10–64), underwent additional surgery such as bone grafting, flap coverage, and debridement after infection. The postoperative mean angulation deformity was 1.8 degrees (range, 0–3.6 degrees).
We found comparable results in our series with one patient with a postoperative angulation deformity of five degrees (MPTA of 92), while all other patients were corrected within three degrees of the mean population average value. The range of motion improved in their series from the preoperative status to the last follow-up. This might be the result of the high number of non-unions (7 of 18) and the presumably short duration between the fracture or initial stabilisation and the reoperation with the TSF. They report one failed union after frame removal with a consecutive varus deformity. As we did not include non-unions we cannot directly compare the complication rate.
Fractures after frame removal are a common complication of external fixation. In our series one case (4%) sustained refracture of the distal femur eight months after frame removal and adequate trauma. In another case, late bowing occurred in the proximal tibia. A literature review [6] of 571 cases cited three incidences, but the aetiology and the amount of lengthening were not discussed. Danzinger et al. reported nine (50%) fractures in a series of 18 femoral lengthenings [3]. Two of the fractures were seen in the group of post-traumatic deformities which included five cases (40%).
In a series of 62 tibial lengthenings using the Ilizarov fixator, Stanitski et al. reported deformation of the regenerate bone after frame removal in six cases (10%) [27].
In our study late bowing of the regenerate bone was observed in one quite heavy male patient (weight 92 kg), who continued hard physical work soon after frame removal and did not comply with the recommended partial weight bearing.
Limitations in the range of motion of the joints immediately proximal and distal to the bone segment being lengthened have been reported by other authors [12, 16].
Herzenberg et al. studied the effect of femoral lengthening with the Ilizarov fixator on the range of motion in the knee joint [12]. The overall average follow-up range of motion was 94% of preoperative flexion. The mean worst flexion during lengthening was 29% of the preoperative value.
Maffulli et al. investigated the effect of femoral and tibial lengthening on knee flexion in 46 patients [16]. The mean femoral lengthening gained was 6.6 cm (17 patients); the mean tibia lengthening was 5.8 cm (29 patients). After a mean follow-up of 41 months the mean knee flexion was 94% of the preoperative value. Femoral lengthening resulted in a significantly greater loss of range of motion than tibial lengthening.
In our study only 86% (19 of 22) of patients had regained their preoperative range of motion in the knee and ankle joint at the latest follow-up visit. One of nine patients (11%) with correction in the distal femur had a preoperative patella subluxation and had lost more than 15% of preoperative flexion at the latest follow-up visit.
Two of seven patients (28%) who had correction in the distal tibia suffered from lack of dorsiflexion in the ankle in combination with radiological signs of osteoarthritis in the ankle joint at the latest follow-up visit. Both patients had correction of a post-traumatic distal tibial varus angulation in combination with loss of length. The amount of lengthening (3.6 cm/4.4 cm) performed in these two cases, was the largest of their entire group. Another important aspect is that these two patients had the longest period of time (27.5 years/14 years) between the incidence of trauma and the deformity correction. Initial signs of osteoarthrosis, presumably caused by the long period of unphysiological stress on the ankle joint cartilage, were seen in both cases on preoperatively obtained radiographs.
In our series the foot was rigidly attached to the frame, resulting in a complete immobilisation of the ankle joint. In the past, orthopaedic research has demonstrated that both joint immobilisation in combination with continuous joint compression have deleterious effects on joint morphology and histological configuration [1, 7, 8, 13]. Since 2004 we split up the correction process, performing lengthening in the proximal tibia and angular correction in the distal tibia as this minimises the contact pressure on the ankle joint cartilage.
In our study the femoral correction had a lower external fixation index than corrections in the proximal or distal tibia. The corrections in the proximal tibia had a lower external fixation index than those in the distal tibia. Similar results have been reported by Fischgrund et al. who found that metaphyseal lengthening healed faster than diaphyseal lengthening, especially for distraction gaps less than 7 cm [11]. Furthermore, femoral lengthening had a significantly faster healing than lengthening performed in the tibia. This data might suggest that the variables affecting time for bone healing in corrections using the Taylor spatial frame are similar to those identified using the Ilizarov frame.
A further important finding of Fischgrund et al. was that the distraction–consolidation index, calculated as the distraction consolidation time divided by the amount of lengthening, produces a hyperbolic curve when plotted against lengthening [11]. The index rises exponentially as the amount of lengthening approaches zero, whereas it tends to reach a plateau as the amount of lengthening increases. A similar effect was observed in our series.
The results of this study may be interpreted as an encouragement to use this external fixation device for correction of post-traumatic deformities. Despite the potentially difficult group of patients, the results were good, with minimal morbidity. The Taylor spatial frame offers the experienced surgeon an accurate and reproducible method for simultaneous six-axes correction.
References
- 1.Akeson WH, Amiel D, Abel MF, Garfin SR, Woo SL. Effects of immobilization on joints. Clin Orthop Rel Res. 1987;219:28–37. [PubMed] [Google Scholar]
- 2.Aronson J. Current concepts review—Limb lengthening, skeletal reconstruction and bone transport with the Ilizarov method. J Bone Joint Surg Am. 1997;79(8):1243–1258. doi: 10.2106/00004623-199708000-00019. [DOI] [PubMed] [Google Scholar]
- 3.Danzinger MB, Kumar A, DeWeese J. Fractures after femoral lengthening using the ilizarov method. J Pediatr Orthop. 1995;15:220–223. [PubMed] [Google Scholar]
- 4.Docquier PL, Rodriguez D, Mousny M. Three-dimensional correction of complex leg deformities using a software assisted external fixator. Acta Orthop Belg. 2008;74(6):816–822. [PubMed] [Google Scholar]
- 5.Eidelman M, Bialik V, Katzman A. Correction of deformities in children using the Taylor spatial frame. J Pediatr Orthop B. 2006;15(6):387–395. doi: 10.1097/01.bpb.0000228380.27239.8a. [DOI] [PubMed] [Google Scholar]
- 6.Eldridge JC, Bell DF. Problems with substantial limb lengthening. Orthop Clin North Am. 1991;22:625–631. [PubMed] [Google Scholar]
- 7.Enneking WF, Horowitz M. The intra-articular effects of immobilization on the human knee. J Bone Joint Surg Am. 1972;54(5):973–985. [PubMed] [Google Scholar]
- 8.Evans EB, Eggers GWN, Butler JK, Blumel J. Experimental immobilization and remobilization of rat knee joints. J Bone Joint Surg Am. 1960;42-A:737–758. [Google Scholar]
- 9.Fadel M, Hosny G. The Taylor spatial frame for deformity correction in the lower limbs. Int Orthop. 2005;29:125–129. doi: 10.1007/s00264-004-0611-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Feldman DS, Shin SS, Madan S, Koval KJ. Correction of tibial malunion and nonunion with six-axis analysis deformity correction using the Taylor spatial frame. J Orthop Trauma. 2003;17(8):549–554. doi: 10.1097/00005131-200309000-00002. [DOI] [PubMed] [Google Scholar]
- 11.Fischgrund J, Paley D, Suter C. Variables affecting time to bone healing during limb lengthening. Clin Orthop Relat Res. 1994;301:31–37. [PubMed] [Google Scholar]
- 12.Herzenberg JE, Scheufele LL, Paley D, Bechtel R, Tepper S. Knee range of motion in isolated femoral lengthening. Clin Orthop Relat Res. 1994;301:49–54. [PubMed] [Google Scholar]
- 13.Hong SP, Henderson CN. Articular cartilage surface changes following immobilization of the rat knee joint. A semiquantitative scanning electron-microscopic study. Acta Anat (Basel) 1996;157(1):27–40. doi: 10.1159/000147864. [DOI] [PubMed] [Google Scholar]
- 14.Ilizarov GA. Clinical application of the tension-stress effect for limb lengthening. Clin Orthop Relat Res. 1990;250:8–26. [PubMed] [Google Scholar]
- 15.Kristiansen LP, Steen H, Reikerås O. No difference in tibial lengthening index by use of Taylor spatial frame or Ilizarov external fixator. Acta Orthop. 2006;77(5):772–777. doi: 10.1080/17453670610012971. [DOI] [PubMed] [Google Scholar]
- 16.Maffulli N, Nele U, Matarazzo L. Changes in knee motion following femoral and tibial lengthening using the Ilizarov apparatus: a cohort study. J Orthop Sci. 2001;6(4):333–338. doi: 10.1007/s007760100028. [DOI] [PubMed] [Google Scholar]
- 17.Manner HM, Huebl M, Radler C, Ganger R, Petje G, Grill F. Accuracy of complex lower-limb deformity correction with external fixation: a comparison of the Taylor spatial frame with the Ilizarov ring fixator. J Child Orthop. 2007;1(1):55–61. doi: 10.1007/s11832-006-0005-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Marangoz S, Feldman DS, Sala DA, Hyman JE, Vitale MG. Femoral deformity correction in children and young adults using Taylor spatial frame. Clin Orthop Relat Res. 2008;466(12):3018–3024. doi: 10.1007/s11999-008-0490-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Matsubara H, Tsuchiya H, Sakurakichi K, Watanabe K, Tomita K. Deformity correction and lengthening of lower legs with an external fixator. Int Orthop. 2006;30:550–554. doi: 10.1007/s00264-006-0133-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Nakase T, Kitano M, Kawai H, Ueda T, Higuchi C, Hamada M, Yoshikawa H (2008) Distraction osteogenesis for correction of three-dimensional deformities with shortening of lower limbs by Taylor spatial frame. Arch Orthop Trauma Surg Sep 11. [Epub ahead of print] [DOI] [PubMed]
- 21.Naqui SZ, Thiryayi W, Foster A, Tselentakis G, Evans M, Day JB. Correction of simple and complex pediatric deformities using the Taylor-Spatial Frame. J Pediatr Orthop. 2008;28(6):640–647. doi: 10.1097/BPO.0b013e3181831e99. [DOI] [PubMed] [Google Scholar]
- 22.Paley D. Problems, obstacles, and complications of limb lengthening by the Ilizarov technique. Clin Orthop Relat Res. 1990;250:81–104. [PubMed] [Google Scholar]
- 23.Paley D, Tetsworth K. Mechanical axis deviation of the lower limbs. Preoperative planning of multiapical frontal plane angular and bowing deformities of the femur and tibia. Clin Orthop Relat Res. 1992;280:65–71. [PubMed] [Google Scholar]
- 24.Paley D, Tetsworth K. Mechanical axis deviation of the lower limbs. Preoperative planning of uniapical angular deformities of the tibia or femur. Clin Orthop Relat Res. 1992;280:48–64. [PubMed] [Google Scholar]
- 25.Tetsworth KD, Paley D. Accuracy of correction of complex lower-extremity deformities by the Ilizarov method. Clin Orthop Relat Res. 1994;301:102–110. [PubMed] [Google Scholar]
- 26.Sluga M, Pfeiffer M, Kotz R, Nehrer S. Lower limb deformities in children: two-stage correction using the Taylor spatial frame. J Pediatr Orthop B. 2003;12(2):123–128. doi: 10.1097/00009957-200303000-00009. [DOI] [PubMed] [Google Scholar]
- 27.Stanitski DF, Shahcheraghi H, Nicker DA, Armstrong PF. Results of tibial lengthening with the Ilizarov technique. J Pediatr Orthop. 1996;16(2):168–172. doi: 10.1097/00004694-199603000-00006. [DOI] [PubMed] [Google Scholar]