Abstract
To evaluate proprioceptive potential in residual remnants, tissue harvested from ruptured ACLs in 63 consecutive patients was examined for evidence of residual proprioceptive fibres using H&E, and monoclonal antibodies to S-100 and NFP (neurofilament protein). Histological examination showed good subsynovial and intra-fascicular vascularity with free nerve endings in the majority. Morphologically normal mechanoreceptors (H&E) and proprioceptive fibres (positivity with monoclonal antibody for NFP) were found in 46% and 52.4% of stumps, respectively. A statistically significant correlation between injury duration and persistence of mechanoreceptors and proprioceptive fibres was noted. More fibres were seen where ACL remnant was adherent to PCL. Our study has shown that persistent residual proprioceptive fibres in injured ACLs (especially early cases with PCL adherence) are significant; not shaving ACL remnants may be of potential benefit during ACL reconstruction, as some re-innervation and recovery of proprioceptive potential may be possible, thus improving clinical outcomes.
Introduction
Injury to the anterior cruciate ligament (ACL) constitutes one of the most serious disabling injuries in sports [1], causing significant alteration of knee joint kinematics. Untreated patients often develop joint instability, meniscal lesions, cartilage damage and eventual secondary osteoarthritis [2].
The primary mechanical function of ACL is to prevent excessive anterior tibial translation in varying degrees of flexion. The knee joint, however, relies on mechanisms other than the mechanical properties of its ligaments to maintain joint stability during physical activities. This may be a form of 'functional stability' which is brought about by the muscle contractions (aided by ligaments) through the sensations transmitted by mechanoreceptors to the brain.
Borsa et al. [3] proposed that functional instability that occurs after ACL injury is due to the combined effects of excessive tibial translation and a lack of coordinated muscle activity to stabilise the knee; this is thought to be due to diminished or absent sensory feedback from the ruptured ACL to the neuromuscular system.
Histologically, it has been demonstrated that the human ACL contains mechanoreceptors that can detect changes in tension, speed, acceleration, direction of movement, and the position of the knee joint [3–9]. Altered neuromuscular function secondary to diminished somato-sensory information (proprioception and kinesthesia) from the injured ACL has been proposed as a key factor in functional instability after these injuries.
Arthroscopic ACL reconstruction using bone-patellar tendon-bone autograft and hamstring grafts is routinely performed [10–12], and very often ligament remnants are shaved off before graft insertion. The thinking is remnant ACL stump removal reduces chances of arthrofibrosis [13, 14] and 'cyclops' lesions. Shaving of the residual stump also facilitates visualisation and improves technical performance [15].
Recent studies have shown that knee proprioception, rather than clinically satisfactory mechanical restoration, may be more closely related to both the functional outcome and the patient's satisfaction following ACL reconstruction [16]. To avoid a complete sensory loss, it may seem reasonable to preserve residual ACL stumps; besides having inherent proprioceptive properties, these may be a source of re-innervation of the implanted ACL graft.
However, before emphasising that injured ACL stumps be preserved, it is important to document the viability of the residual proprioceptive fibres; more importantly, these fibres should be functionally relevant. Only three previous studies [4, 15, 17] have so far addressed these issues. Denti et al. [4] removed specimens from ruptured ACLs at arthroscopy but found mechanoreceptors only in the initial few months after injury. Ochi et al. [17] demonstrated reproducible cortical somatosensory evoked potentials induced by electrical stimulation in 15 of 32 ACL remnants and postulated that the original sensory neurons are preserved in ACL remnants to some extent. Georgoulis et al. [15] investigated the presence of mechanoreceptors in the ACL stump as a possible source of re-innervation of ACL graft.
Working on the same idea, we attempted to immuno-histologically evaluate the proprioceptive potential of residual ACL stumps, using monoclonal antibodies to neurofilament protein (NFP) to demonstrate the proprioceptive fibres. The efficacy of this procedure to pick up proprioceptive fibres in intact ACLs has been established in previous studies [18–21]. Our study was not just confined to finding mechanoreceptors or proprioceptive fibres on the ACL, but also an attempt to correlate their presence with various clinical and operative findings.
Materials and methods
From July 2007 to December 2008, 90 patients admitted for arthroscopic ACL reconstruction in PGIMER, Chandigarh, India were evaluated. Exclusion criteria included previous knee surgery, age above 50 years, inflammatory arthritis, history of other significant knee injury/fracture, and presence of associated posterior cruciate ligament (PCL) or collateral ligament injury.
Clinical assessment included evaluation of age, sex, side, duration of injury, clinical examination findings, and associated injury to other soft tissue knee stabilisers. Intra-operative assessment included evaluation of the site of the residual stump (tibial or femoral), stump length, notch type, presence of infrapatellar plica, meniscal evaluation, PCL and collateral integrity, presence of synovitis and presence of cyclops lesion. Special note was made to see if the stump was adherent to PCL.
Out of 90 cases, six were excluded on the basis of the exclusion criteria. Of the remaining 84, 21 had an atrophied ACL stump too small to be biopsied. Thus, a total of 63 ACL stumps were biopsied and evaluated.
Intra-operatively, residual ACL tissue was harvested by cutting stumps from as near to the attachment site as possible using arthroscopic scissors. In cases where the residual stump was adherent to the PCL, the attachment was carefully dissected out before the remainder of the ACL was cut from its insertion site. If present, both the femoral and the tibial stumps were separately harvested. The specimens were preserved in 10% buffered formaldehyde solution. The harvested samples were serially sectioned on a standard rotatory microtome and examined by conventional light microscope after staining using: (1) haemotoxylin and eosin (H&E), (2) monoclonal antibody against NFP (neurofilament protein) and (3) monoclonal antibody against S-100 protein.
Adequate controls were used to confirm the staining of these monoclonal antibodies before these were evaluated. The monoclonal antibody against NFP stained the axons cylinders carrying proprioception. The monoclonal antibodies against S-100 stained free nerve endings and Schwann cells. H&E was used for detailed histological evaluation of synovial lining, subsynovial vascularity, intra-fasicular morphologically normal mechanoreceptors, degenerative changes, and inflammation.
Statistical analysis was carried out with the chi-square test and calculation of odds ratios.
Results
The mean duration between injury and surgery was 14.95 months (range 2–60 months). The length of residual stump harvested ranged from 0.5 cm to 4.5 cm (mean 2.26 cm). A single full length stump measuring 4.5 cm in length was harvested; this probably represented an incomplete tear and functionally incompetent ACL.
The femoral stump could be harvested in only six patients; in 56 a tibial remnant was harvested, and both tibial and femoral stumps were harvested in one. The ACL remnant was adherent to the PCL in 29 cases. Other findings noted were an infrapatellar plica in 36 knees, 24 narrow notches requiring notchplasty, 19 lateral meniscus tears, 35 medial meniscus tears, and six knees with synovial hyperaemia.
H&E examination confirmed ACL ligamentous tissue in all specimens. Abundant synovium, good subsynovial and intrafasicular vascularity with free nerve endings were seen in most specimens. A few specimens had extensive degeneration, but some ligamentous tissues were always identifiable in these specimens. Inflammatory changes were seen in only two cases, with areas of lymphocytic infiltration.
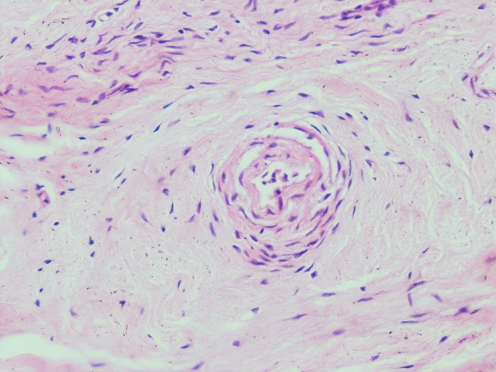
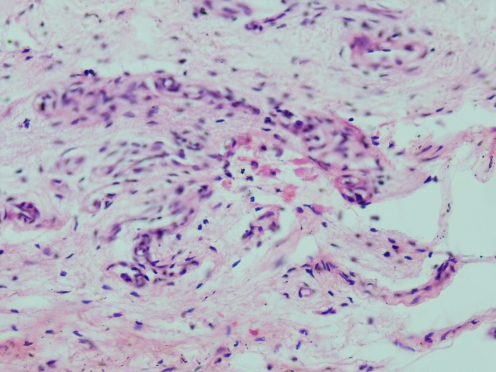
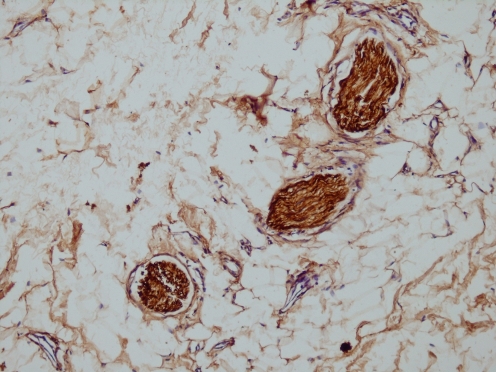
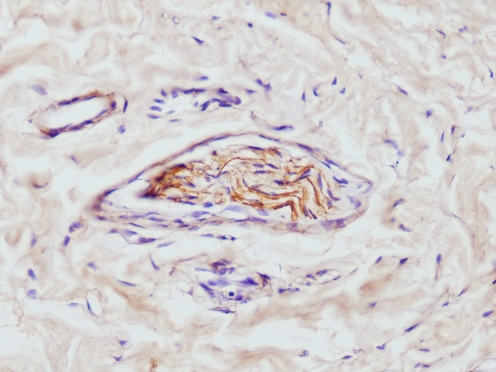
Monoclonal antibodies to S-100 used to stain Schwann cells and nerve tissue showed positive results in 82.5% of specimens (52 patients); morphologically normal mechanoreceptors were identified in 46% of these (29 patients) (mostly Paccinian or Ruffini type). Fusiform mechanoreceptors (Golgi tendon organ type) were also seen in three specimens (Figs. 1, 2, 3 and 4). Specimens where mechanoreceptors were identified had on average one to two mechanoreceptors seen under the light microscope, mostly located subsynovially. Less frequently they were seen intra-fasicularly (in connective tissue between parallel running fascicles). The monoclonal antibody to NFP which specifically stained the nerve fibres carrying proprioception was positive in 52.4% of specimens (33 patients).
Fig. 1.
Intraligamentous Paccinian-like mechanoreceptors (H&E, high power ×40)
Fig. 2.
Intraligamentous fusiform mechanoreceptors (H&E, high power ×40)
Fig. 3.
Nerve endings S-100 positive (high power ×40)
Fig. 4.
Neurofilament protein (NFP) positive slender axons (high power ×40)
The age, sex and side involved did not have any statistically significant correlation with any of the outcomes. Injury duration and residual stump length had no statistically significant relationship with presence of synovial lining, subsynovial and intra-fasicular vascularity or free nerve endings. However, morphologically normal mechanoreceptors (MR) and immune-reactivity to NFP were more significantly and more frequently seen with lesser duration of injury (p-values 0.045 and 0.22, respectively).
Remnant stump length also had a statistically significant relationship with presence of morphologically normal mechanoreceptors and immunoreactivity of NFP (p-values 0.096 and 0.004, respectively).
No statistically significant difference was seen in the outcomes with respect to site of stump harvest (tibial or femoral), presence or absence of infrapatellar plica, type of notch and presence of cyclops lesion. However, an infrapatellar plica was seen more frequently in cases of wide notch and there was a trend towards significance in this difference (p-value 0.052).
When PCL adherence was taken into consideration, no statistically significant difference was noted concerning the presence of synovium, or subsynovial and intra-fasicular vascularity in cases with ACL stumps adherent or not to the PCL. We could not find any significant difference with regard to presence of free nerve endings (both subsynovial and intra-fasicular) or immune-reactivity to S-100P in adherent or non adherent stumps. However, both mechanoreceptors and immune-reactivity to NFP was found to be more frequent in specimens adherent to PCL, and this difference was found to be statistically significant (p-values 0.004 and 0.015, respectively).
Residual stump adherence to PCL also had a statistically significant relationship with the length of the stump (p-value 0.002), with longer stumps adhering to PCL more often. However, there was no relation between PCL adherence and age of the patient or duration of injury.
Histologically, degeneration was significantly more common (p-value 0.033) in stumps harvested from patients presenting late for surgery. No other independent variable showed a significant relationship with degenerative changes in ACL stumps.
Meniscal tears did not have any significant relationship with any of the outcomes.
Discussion
With proprioception being accepted as a major contributing factor to knee stability, thought processes are now focussing on evaluating if this sensation can return after surgical ACL reconstruction. Studies have demonstrated that gait and kinematic patterns have a tendency to return to normal 6–12 months post ACL reconstruction. Ochi et al. [17] emphasised that restoration of knee function was not only important in terms of the anatomical ACL reconstruction as a mechanical restraint, but also in sensory re-innervation of the graft which could potentially improve overall outcomes. The evidence of re-innervation was presented anatomically by Denti et al. [4]; they found re-innervation of autologous bone-patellar tendon bone graft in animals three to six months postoperatively. The occurrence of this in patients means that the ACL remnant may be an important source for graft neuralisation.
To identify the various fibres or receptors that could be present in residual stumps, we used indirect methods; we employed monoclonal antibody to NFP and were able to see proprioceptive fibres in residual tissues. A few previous studies had used monoclonal antibody to NFP as a standard method to demonstrate proprioceptive fibres in normal ACLs [18, 20]; we went a step further and used it for the first time in injured ACLs. Its positivity was easy to pick up by direct evaluation under the light microscope. We were also able to demonstrate mechanoreceptors in some injured stumps using H&E staining, establishing the fact that potential for regeneration from these stump tissues exists.
We found a statistically significant relationship between lesser duration of injury and higher proprioceptive potential of injured ACL stumps. Our result was somewhat similar to those of Denti et al. [4]; however, they could not demonstrate any mechanoreceptors in stumps after one year of injury, whereas we found some mechanoreceptors even as late as 42 months after injury in one patient. The larger sample size used in our study may partly account for this difference in results. This fact assumes importance in certain areas of the world where delays in presentation to specialised centres for arthroscopic ACL reconstruction is frequent. From our analysis we predict that there is some hope for residual proprioceptive fibres being present even in these delayed cases.
We also found the stump length to be a strong predictor of a higher proprioceptive potential. This sounds logical because a longer stump is more likely to have a larger number of mechanoreceptors and proprioceptive fibres because of its larger volume. These results, however, can also be explained by the fact that most of the longer stumps were adherent to the PCL, and PCL adherence in itself was found to be a strong predictor of high proprioceptive potential of the injured stumps.
The presence of synovium, subsynovial vascularity, intra-fasicular vascularity and free nerve endings was not significantly affected statistically by any of our predictors. We found these to be present in a large majority of the residual stumps. Thus, we noted that vascularity and free nerve endings are maintained in most of the injured ACL stumps. This was supported by staining with monoclonal antibody to S-100 which was found to be positive in 82.5% of the stumps. However, it is difficult to conclude if these free nerve endings are of any significance with regard to proprioception.
A statistically significant difference in proprioceptive potential was found between the remnants which were adherent to PCL as compared to those which were not. This increased proprioceptive potential with PCL adherence was also noted by Georgoulis et al. [15]; however, our sample size (63) was significantly larger than that in the previous study. The re-adaptation of the ACL remnant as it becomes adherent to the PCL may contribute to some degree of functional stability of the knee. The PCL adherent stumps were also found to be longer; this can probably be explained by the fact that an increased length allows an ACL stump to fall onto the PCL, and subsequent adhesions develop with time.
Treatment delays are a significant issue in countries of the Asian and African continents. It is presumed that degeneration of tissues and neural elements would be more in cases seen with delay as compared to those with a shorter duration of injury. This was shown to be true from our observations, and this difference was statistically significant. With degenerative changes the proprioceptive potential of the injured stump decreased more, further substantiating the fact that delays in treatment negatively affect the mechanoreceptor and propriceptive fibres in the stump. We postulate that in ACL deficient knees of long duration, repeated episodes of giving way and re-injury due to instability may render the stump prone to degeneration.
Our study has shown that residual proprioceptive fibres and mechanoreceptors persist in almost half the ACL stumps (52.40% and 46%, respectively). Even Ochi et al. [17] noted somatosensory evoked potentials in about 50% of the investigated ACL remnants as confirmation that original sensory neurons are preserved to some extent in the ACL remnant. This assumes importance as many surgeons feel the need to shave off the ACL remnant to facilitate surgical visualisation and technical performance of the surgery. Shaving probably reduces the chances of notch impingement and arthrofibrosis; however, we would recommend a change in the routine attitude to indiscriminate soft tissue removal at surgery. Since we have noted mechanoreceptors and proprioceptive fibres in almost half the residual stumps, especially those with PCL adherence, we recommend that only selective cases should have the ACL stumps shaved off. Ingrowth of neural and vascular elements from these stumps into the implanted grafts could add to the stability of the reconstruction; even if limited proprioception returns, the benefit may be tremendous.
To conclude, our study has shown that residual propioceptive fibres exist in soft tissues of ACL deficient knees. Negative factors are treatment delays, stumps of small size and those not adherent to PCL. We predict that restoration of proprioception after ACL reconstruction may be aided if only selective shaving is done on these tissues, as ACL remnants are a potential source for nerve fibres which could help in the reinnervation of implanted grafts.
References
- 1.Bonci CM. Assessment and evaluation of predisposing factors to anterior cruciate ligament injury. J Athl Train. 1999;34(2):155–164. [PMC free article] [PubMed] [Google Scholar]
- 2.McDaniel WJ, Jr, Dameron TB., Jr The untreated anterior cruciate ligament rupture. Clin Orthop Relat Res. 1983;172:158–163. [PubMed] [Google Scholar]
- 3.Borsa PA, Lephart SM, Irrgang JJ, Safran MR, Fu FH. The effects of joint position and direction of joint motion on proprioceptive sensibility in anterior cruciate ligament-deficient athletes. Am J Sports Med. 1997;25(3):336–340. doi: 10.1177/036354659702500311. [DOI] [PubMed] [Google Scholar]
- 4.Denti M, Monteleone M, Berardi A, Panni AS. Anterior cruciate ligament mechanoreceptors. Clin Orthop Relat Res. 1994;308:29–32. [PubMed] [Google Scholar]
- 5.Johansson H, Sjolander P, Sojka P. Receptors in knee joint and their role in biomechanics of joint. Crit Rev Biomed Eng. 1991;18(5):341–368. [PubMed] [Google Scholar]
- 6.Johansson H, Sjolander P, Sojka P. A sensory role for the cruciate ligaments. Clin Orthop Relat Res. 1991;268:161–178. [PubMed] [Google Scholar]
- 7.Zimny ML, Schutte M, Dabezies E. Mechanoreceptors in the human anterior cruciate ligament. Anat Rec. 1986;214(2):204–209. doi: 10.1002/ar.1092140216. [DOI] [PubMed] [Google Scholar]
- 8.Schultz RA, Miller DC, Kerr CS, Micheli L. Mechanoreceptors in human cruciate ligaments. A histological study. J Bone Joint Surg Am. 1994;66(7):1072–1076. [PubMed] [Google Scholar]
- 9.Schutte MJ, Dabezies EJ, Zimny ML, Happel LT. Neural anatomy of the human anterior cruciate ligament. J Bone Joint Surg Am. 1987;69(2):243–247. [PubMed] [Google Scholar]
- 10.Paterson FWN, Trickey EL. Anterior cruciate ligament reconstruction using patellar tendon as a graft. J Bone Joint Surg Br. 1986;68(B):453–457. doi: 10.1302/0301-620X.68B3.3733814. [DOI] [PubMed] [Google Scholar]
- 11.Noyes FR, Butler DL, Paulos LE, Grood ES. Intraarticular cruciate reconstruction. I: Perspective on graft strength, vascularisation and immediate motion after placement. Clin Orthop Relat Res. 1983;172:71–77. [PubMed] [Google Scholar]
- 12.Arnoczky SP, Tarvin GB, Marshall JL. Anterior cruciate ligament replacement using patellar tendon. An evaluation of graft revascularization in the dog. J Bone Joint Surg Am. 1982;64(2):217–224. [PubMed] [Google Scholar]
- 13.Mayr HO, Weig TG, Plitz W. Arthrofibrosis following ACL reconstruction–reasons and outcome. Arch Orthop Trauma Surg. 2004;124(8):518–522. doi: 10.1007/s00402-004-0718-x. [DOI] [PubMed] [Google Scholar]
- 14.Recht MP, Piraino DW, Cohen MA, Parker RD, Bergfeld JA. Localized anterior arthrofibrosis (cyclops lesion) after reconstruction of the anterior cruciate ligament: MR imaging findings. AJR Am J Roentgenol. 1995;165(2):383–385. doi: 10.2214/ajr.165.2.7618562. [DOI] [PubMed] [Google Scholar]
- 15.Georgoulis AD, Pappa L, Moebius U, et al. The presence of proprioceptive mechanoreceptors in the remnants of ruptured ACL as possible source of reinnervation of ACL autograft. Knee Surg Sports Traumatol Arthrosc. 2001;9(6):364–368. doi: 10.1007/s001670100240. [DOI] [PubMed] [Google Scholar]
- 16.Barrett DS. Proprioception and function after anterior cruciate ligament reconstruction. J Bone Joint Surg Br. 1991;73(5):833–837. doi: 10.1302/0301-620X.73B5.1894677. [DOI] [PubMed] [Google Scholar]
- 17.Ochi M, Iwasa J, Uchio Y, et al. The regeneration of sensory neurons in the reconstruction of the anterior cruciate ligament. J Bone Joint Surg Br. 1999;81(5):902–906. doi: 10.1302/0301-620X.81B5.9202. [DOI] [PubMed] [Google Scholar]
- 18.Fromm B, Kummer W. Nerve supply of anterior cruciate ligaments and of cryopreserved anterior cruciate ligament allografts: a new method for the differentiation of the nervous tissues. Knee Surg Sports Traumatol Arthrosc. 1994;2(2):118–122. doi: 10.1007/BF01476484. [DOI] [PubMed] [Google Scholar]
- 19.Parsch D, Fromm B, Kummer W. Projections and fiber characteristics of sensory afferents of the anterior cruciate ligament in an animal experiment. Unfallchirurgie. 1996;22(5):193–201. doi: 10.1007/BF02641220. [DOI] [PubMed] [Google Scholar]
- 20.Krauspe R, Schmitz F, Zöller G, Drenckhahn D. Distribution of neurofilament-positive nerve fibres and sensory endings in the human anterior cruciate ligament. Arch Orthop Trauma Surg. 1995;114(4):194–198. doi: 10.1007/BF00444261. [DOI] [PubMed] [Google Scholar]
- 21.Valle ME, Harwin SF, Maestro A, et al. Immunohistochemical analysis of mechanoreceptors in the human posterior cruciate ligament: a demonstration of its proprioceptive role and clinical relevance. J Arthroplasty. 1998;13(8):916–922. doi: 10.1016/S0883-5403(98)90199-1. [DOI] [PubMed] [Google Scholar]