Abstract
A tip-apex distance (TAD) of greater than 25 mm has been shown to be an accurate predictor of lag screw cut-out when sliding hip screws (SHS) are used to treat peritrochanteric (PT) hip fractures. The purpose of this study was to determine which factors, including TAD, correlated with successful clinical outcomes of PT hip fractures surgically treated with intramedullary (IM) devices. A total of 192 patients were included in this retrospective study. The TAD values of this cohort were radiographically analysed at a mean follow-up of 13 months. This was correlated with limited functional status and the rate of revision for implant failure or inability to achieve fracture union. Only 82 patients had adequate follow-up to fracture union or definitive failure. There were 46 intertrochanteric (IT) hip fractures and 36 subtrochanteric (ST) fractures. Overall, seven patients (8.5%) went on to experience lag screw cut-out. The average TAD of the patients who did not cut-out was 18 mm, compared to 38 mm for those who did (p = 0.012). All patients who cut-out had IT fractures (p = 0.017). The percentage of cut-outs correlated directly to both the severity of IT fractures and the TAD. Using a cutoff of 25 mm there was a statistically significant difference in the incidence of lag screw cut-out (p < 0.001). As in sliding hip screws, surgeons should strive for a TAD less than 25 mm when using IM devices in the treatment of PT hip fractures to help avoid lag screw cut-out.
Introduction
The incidence of hip fractures continues to rise as the population ages to virtually epidemic proportions. Over 700,000 deaths are estimated annually worldwide due to hip fractures [1]. In the United States, the estimated six-month mortality rate is estimated to be between 17 and 20% [2–4]. At an expense of over $12 billion dollars in 2005, hip fractures were estimated to account for 72% of the total US costs associated with all fractures [5]. According to a 1997 report, it is expected that, by 2040, the number of hospital admissions and lifetime costs associated with hip fractures will double from 311,000 to 622,000 and $25 billion to $47 billion, respectively [4]. Successful treatment of these fractures during the first operative episode will be an essential component to returning these generally frail and debilitated patients back to maximal function.
Sliding hip screws (SHS) and intramedullary (IM) devices are commonly used in the treatment of unstable intertrochanteric (IT) and subtrochanteric (ST) fractures. While the use of a SHS combined with a derotation screw has been shown to effectively stabilise IT fractures [6], comparative studies between SHS and IM devices have shown that the use of IM devices is associated with a decrease in operative time, intraoperative blood loss, limb shortening, and lengthy hospital stays [7–9]. IM devices can also be inserted through multiple incisions smaller than those for SHS, which not only reduces operative blood loss, but also fluoroscopy time [10]. Moreover, the design aspects of IM devices, such as their intramedullary nature and the close proximity of the IM rod to the lag screw, facilitate load sharing and architectural stability not found in SHS. Although the biomechanical advantages of IM devices may lead to better overall patient outcomes [11], there has been an observed increased risk for certain types of failures, such as proximal femur shaft fractures [12] and lag screw cut-outs.
Tip-apex distance (TAD), which represents both the position and depth of a screw in the femoral neck and head, has been shown to be an accurate predictor of lag screw cut-out in SHS [7, 13, 14]. Although previous studies have stated that there is no statistical difference in cut-out between SHS fixed with either IM nails or side plates, no study has examined the relationship between the TAD and cut-out specifically for IM devices [13].
Therefore, the aim of the this study was to determine which factors, including TAD, correlated with successful clinical outcomes of IT and ST hip fractures surgically treated with IM devices. Our hypothesis was that, as with the use of SHS, a TAD of 25 mm would show improved clinical results and fewer hardware failures by lag screw cut-out.
Materials and methods
A retrospective review of all hip fracture patients treated with IM devices between 2000 and 2007 at the authors’ institution, a level two trauma centre and tertiary referral teaching facility, was performed. Patients with less than three months of follow-up or those who sustained pathological fractures of the femur were excluded from the study. There were no patients excluded based on age or other medical comorbidity.
Data collected included patients’ age at surgery, gender, fracture type, operative side, surgeon, type of implant, quality of reduction, TAD, and three-month postoperative ambulatory status. Fracture type, quality of reduction and TAD were determined using preoperative and postoperative anterior-posterior (AP) and lateral hip digital radiographs.
The IT fracture patterns were classified according to the system of Muller and Evans as modified by Kyle et al. [15], with types III and IV considered unstable. ST fracture patterns were classified according to the system of Seinsheimer [16], which is based on the number of fragments, with type V being the most severe with five or more fragments [16].
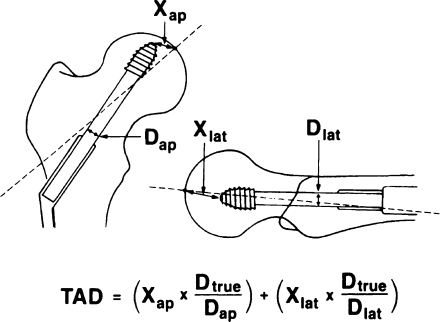
The quality of reduction was modified from the system of Baumgaertner et al. based on immediate postoperative AP and lateral radiographs [13, 14]. For both fracture types, reductions were evaluated on the basis of displacement and angulation, and categorised as good, acceptable, or poor. A reduction met the displacement criteria if there was less than 4 mm of displacement on either the AP or lateral X-ray. The angulation criteria were met if the neck shaft angulation was normal or slightly valgus (130–150°) and there was less than 20 degrees of angulation on the lateral X-ray. A reduction was categorised as good if it met both criteria, acceptable if it met one criterion and poor if it met neither criterion. All radiographs were analysed as previously described in the literature regarding IM nails in the treatment of PT hip fractures [17] using GE Pacs Centricity software (General Electric Medical Systems). Radiographs were adjusted for magnification by multiplying the measured distances on both AP and lateral radiographs by the ratio of the true to measured lag screw diameter (Fig. 1).
Fig. 1.
Illustration of tip-apex distance (TAD) with its corresponding equation for correcting radiographic magnification. Xap and Xlat refer to the measured distance as illustrated on the anteroposterior and lateral X-rays, respectively. Dtrue refers to the actual diameter of the lag screw; whereas, Dap and Dlat refer to the measured diameter of the lag screw as illustrated on the anteroposterior and lateral X-rays. (Used with permission from Baumgaertner et al. [7])
TAD was determined by measuring the distance from the tip of the lag screw to the apex of the femoral head on both AP and lateral radiographs (Fig. 1).
Statistical methods
The final endpoint of the study was lag screw cut-out or fracture union respectively. Interval and dichotomous data were analysed using Student’s t test and Fisher’s test, respectively.
Results
There were a total of 192 patients treated with IM devices during the study period. Of these, only 82 patients met inclusion criteria. There were a total of 13 males and 69 females with an average age of 78 ± 12 years included in this study. There were 46 IT fractures and 36 ST fractures, of which 41% (n = 19) were considered unstable. Surgical hip fracture repair was performed by one of eight senior surgeons based on the on-call responsibilities. Good (32%) or acceptable (55%) reduction criteria were met for 71 out of 82 patients (87%).
The IM devices used were the Stryker (Mahwah, NJ) second and third generation gamma nail and the Synthes (Paoli, PA) long trochanteric fixation nail (TFN). The second generation gamma nail is further classified as trochanteric or long. All versions of the gamma nail had an angle of 130 degrees, while the TFNs had an angle of 125 degrees. The second and third generation gamma nails had lag screw diameter of 12 mm and 10.5 mm, respectively. The TFNs had a lag screw diameter of 11 mm. The choice of implant was based entirely on the surgeons’ preference.
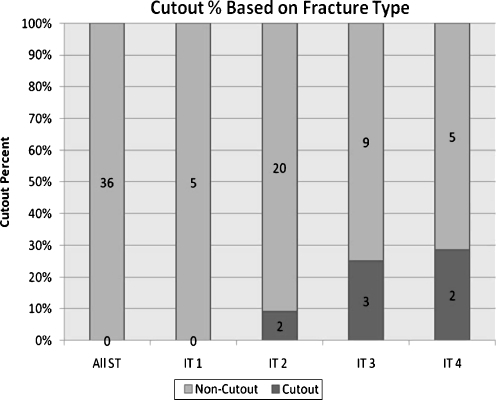
At a mean of 13 months follow-up, all ST and IT1 fractures were fully healed while IT2, IT3, and IT4 fractures had non-union rates of 9.1% (n = 2), 25% (n = 3), and 29% (n = 2), respectively. All patients who cut-out had non-union, intertrochanteric fractures (n = 7), while there were no cut-outs in the subtrochanteric group (p = 0.017). Unlike intertrochanteric fractures, the severity of subtrochanteric fractures was not associated with cut-out. A direct correlation between the severity of IT fracture and the percentage of cut-outs is illustrated in Fig. 2.
Fig. 2.
Percentage of cut-outs and non-cut-outs for all subtrochanteric (ST) and intertrochanteric (IT) fracture pattern subtypes. The IT fracture patterns were classified according to the system of Muller and Evans as modified by Kyle et al. [13], with types III and IV considered unstable
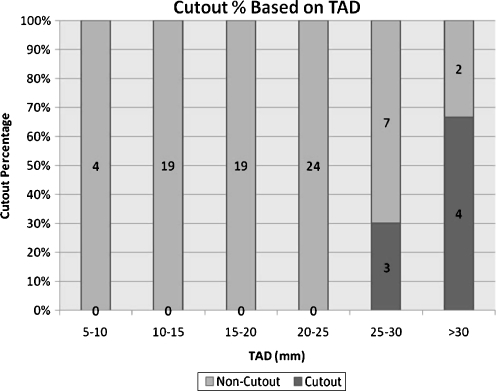
Overall, there was an average TAD of 20 mm ± 9 mm with an 8.5% cut-out rate (n = 7 patients). The mean TAD of the patients who did cut-out compared to those who did not was 38 mm and 18 mm, respectively (p = 0.012). Since no patients with a TAD below 25 mm cut-out and 44% of patients with a TAD above 25 mm cut-out, there was a strong statistical difference in the incidence of lag screw cut-out (p < 0.001) between patients with TAD values above and below 25 mm. Figure 3 illustrates the direct correlation between TAD and cut-out for TAD values greater than 25 mm.
Fig. 3.
Percentage of cut-outs and non-cut-outs withing each respective tip-apex distance (TAD) (mm) range
There was no statistically significant correlation (p < 0.05) between cut-out and age, sex, side of fracture, reduction quality, implant type, or operating surgeon.
Discussion
With the rise in an aging population and a limited amount of healthcare resources in the foreseeable future, it will be increasingly important to find ways to avoid complications when treating hip fractures. This cohort of patients is exceedingly fragile as evidenced by the occurrence of the fracture itself. Most of these patients will be unable to endure a second operation, let alone tolerate prolonged physical therapy. They will probably be placed into another rehabilitation institution for an extended period of time and face the problems associated with being placed out of the home environment after a secondary reconstructive procedure [4, 5, 18]. Even after one operation, the one-year mortality rate after a hip fracture is alarmingly high at 25% [19].
Baumgartner et al., in his initial landmark report documenting the ideal position of the lag screw in the centre-centre position, showed a small cohort of patients who were treated using a cephalomedullary implant. Other studies have compared the IM devices versus traditional SHSs [12, 13]. However, our literature review found no studies that specifically evaluated the lag screw cut-out rate using cephalomedullary implants. The advantages of our study include a satisfactory number of patients with adequate follow-up in this cohort of patients with typically poor follow-up. It seems commonplace that a large majority of these patients fail to return for follow-up due to a multitude of factors when they are transferred to a skilled nursing facility after hospital discharged. Additionally, the mortality rate is likely to be higher than has been reported.
The major disadvantages of this study are the retrospective nature and the difficulty we experienced trying to increase the follow-up data pool of patients. The investigation does, however, provide valuable analysis of this extremely common and likely increasingly needed surgical procedure.
In conclusion, the high incidence (44%) of cut-outs in IT fractures surgically fixed with TAD >25 mm in this study is a dramatic statistic. It stresses the importance of accurate surgical technique in the prevention of extremely unfortunate situations where revision fixation may be needed. As noted, it is probably exacerbated by the poor bone quality in the region surrounding the lag screw postoperatively and patients who have significantly comminuted intertrochanteric fractures may be more prone to IM device cut-out. If revision surgery becomes necessary, it may portend a high possibility of mortality or at the very least a high rate of in-hospital morbidity and cost.
As shown in other studies focusing on sliding hip screws, IM devices are susceptible to cut-out at TAD values greater than 25 mm. Hence, surgeons should strive for a TAD less than 25 mm when using IM devices, especially in the treatment of comminuted intertrochanteric hip fractures to help avoid lag screw cut-out. Additionally, this study reconfirms that cephalomedullary devices are appropriate for ST fractures and that unstable IT fractures can be more vexing than was classically considered.
References
- 1.Johnell O, Kanis JA. An estimate of the worldwide prevalence, mortality and disability associated with hip fracture. Osteoporos Int. 2004;15(11):897–902. doi: 10.1007/s00198-004-1627-0. [DOI] [PubMed] [Google Scholar]
- 2.Hannan EL, Magaziner J, Wang JJ, Eastwood EA, Silberzweig SB, Gillbert M, Morrison RS, McLaughlin MA, Orosz GM, Siu AL. Mortality and locomotion 6 months after hospitalization for hip fracture: risk factors and risk-adjusted hospital outcomes. JAMA. 2001;285(21):2736–2742. doi: 10.1001/jama.285.21.2736. [DOI] [PubMed] [Google Scholar]
- 3.van Balen, R, Steyerberg EW, Polder JJ, Ribbers TL, Habbema JD, Cools HG (2001) Hip fracture in elderly patients: outcomes for function, quality of life, and type of residence. Clin Orthop Relat Res (390):232–243 [PubMed]
- 4.Braithwaite RS, Col NF, Wong JB. Estimating hip fracture morbidity, mortality and costs. J Am Geriatr Soc. 2003;51(3):364–370. doi: 10.1046/j.1532-5415.2003.51110.x. [DOI] [PubMed] [Google Scholar]
- 5.Burge R, Dawson-Hughes B, Solomon DH, Wong JB, King A, Tosteson A. Incidence and economic burden of osteoporosis-related fractures in the United States, 2005–2025. J Bone Miner Res. 2007;22(3):465–475. doi: 10.1359/jbmr.061113. [DOI] [PubMed] [Google Scholar]
- 6.Massoud EIE (2009) Fixation of basicervical and related fractures. Int Orthop. doi:10.1007/s00264-009-0814-1 [DOI] [PMC free article] [PubMed]
- 7.Baumgaertner MR, Curtin SL, Lindskog DM (1998) Intramedullary versus extramedullary fixation for the treatment of intertrochanteric hip fractures. Clin Orthop Relat Res (348):87–94 [PubMed]
- 8.Sadowski C, Lübbeke A, Saudan M, Riand N, Stern R, Hoffmeyer P. Treatment of reverse oblique and transverse intertrochanteric fractures with use of an intramedullary nail or a 95 degrees screw-plate: a prospective, randomized study. J Bone Joint Surg Am. 2002;84-A(3):372–381. [PubMed] [Google Scholar]
- 9.Park SR, Kang JS, Kim HS, Lee WH, Kim YH. Treatment of intertrochanteric fracture with the gamma AP locking nail or by a compression hip screw-a randomised prospective trial. Int Orthop. 1998;22(3):157–160. doi: 10.1007/s002640050231. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Utrilla AL, Reig JS, Muñoz FM, Tufanisco CB. Trochanteric gamma nail and compression hip screw for trochanteric fractures: a randomized, prospective, comparative study in 210 elderly patients with a new design of the gamma nail. J Orthop Trauma. 2005;19(4):229–233. doi: 10.1097/01.bot.0000151819.95075.ad. [DOI] [PubMed] [Google Scholar]
- 11.Mahomed N, Harrington I, Kellam J, Maistrelli G, Hearn T, Vroemen J (1994) Biomechanical analysis of the gamma nail and sliding hip screw. Clin Orthop Relat Res (304):280–288 [PubMed]
- 12.Liu M, Yang Z, Pei F, Huang F, Chen S, Xiang Z (2009) A meta-analysis of gamma nail and dynamic hip screw in treating peritrochanteric fractures. Int Orthop. doi:10.1007/s00264-009-0783-4 [DOI] [PMC free article] [PubMed]
- 13.Baumgaertner MR, Curtin SL, Lindskog DM, Keggi JM. The value of the tip-apex distance in predicting failure of fixation of peritrochanteric fractures of the hip. J Bone Joint Surg Am. 1995;77(7):1058–1064. doi: 10.2106/00004623-199507000-00012. [DOI] [PubMed] [Google Scholar]
- 14.Baumgaertner MR, Solberg BD. Awareness of tip-apex distance reduces failure of fixation of trochanteric fractures of the hip. J Bone Joint Surg Br. 1997;79(6):969–971. doi: 10.1302/0301-620X.79B6.7949. [DOI] [PubMed] [Google Scholar]
- 15.Kyle RF, Gustilo RB, Premer RF. Analysis of six hundred and twenty-two intertrochanteric hip fractures. J Bone Joint Surg Am. 1979;61(2):216–221. [PubMed] [Google Scholar]
- 16.Seinsheimer F. Subtrochanteric fractures of the femur. J Bone Joint Surg Am. 1978;60(3):300–306. [PubMed] [Google Scholar]
- 17.Shyam Kumar AJ, Parmar V, Bankart J, William C, Harper WM. Comparison of accuracy of lag screw placement in cephalocondylic nails and sliding hip screw plate fixation for extracapsular fractures of the neck of femur. Int Orthop. 2006;30(5):320–324. doi: 10.1007/s00264-006-0092-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Cummings SR, Rubin SM, Black D (1990) The future of hip fractures in the United States. Numbers, costs, and potential effects of postmenopausal estrogen. Clin Orthop Relat Res (252):163–166 [PubMed]
- 19.US Congress (1994) Hip fracture outcomes in people age 50 and over. Background paper. Government Printing Office, Washington, DC, USA