Abstract
Range of motion (ROM) is an important outcome variable after total knee arthroplasty (TKA). This may be compounded by a pre-existing fixed flexion deformity (FFD). We therefore examined the long-term outcomes of patients with a flexion deformity undergoing TKA compared to those without a preoperative fixed flexion deformity. Participants who had undergone TKA at our centre between 1989 and 2002 were examined preoperatively, one, five and ten years after TKA (Kinemax PS; Howmedica, Rutherford, NJ, USA). Examining those with a preoperative FFD of greater than ten degrees with complete ten year follow-up data revealed 77 individuals. Seventy seven age, sex and body mass index matched patients were identified and the effect of TKA on indices of knee function (fixed flexion, maximum flexion, total ROM and Knee Society score (KSS) in both groups were analysed using repeated measures ANOVA. A significant difference between the groups with respect to fixed flexion (p < 0.001), total ROM (p = 0.001) and KSS (p < 0.001) was observed between baseline and year one suggesting that those with a preoperative FFD improved more than those without. A significant difference with regard to fixed flexion was also observed between years one to five (p = 0.001) and just failed to reach statistical significance between five to ten years (p = 0.052) between the groups. This study demonstrates that patients with a preoperative fixed flexion deformity show continued improvement in their fixed flexion up to ten years post arthroplasty and have similar outcomes to those with no preoperative fixed flexion.
Introduction
Fixed flexion deformities are a combination of ligamentous, capsular and bony deformity having an adverse effect on knee biomechanics, increasing the forces across the patellofemoral and tibiofemoral joints [1]. A range of 83–105 degrees flexion is required for normal daily activities and anything less severely affects a patient’s quality of life [2–5]. This makes simple everyday tasks such as walking or climbing stairs difficult and tiring. These deformities can, in most cases, be corrected by a total knee arthroplasty. Pain relief and range of motion remain important outcomes variables post TKA. Previous research has demonstrated that preoperative range of motion (ROM) was the strongest predictor of postoperative ROM [6]. The presence of fixed flexion deformities has been reported in up to 61% of knees undergoing primary TKA [7].
We present the results of our data for those patients with and without a FFD, with complete ten-year follow-up. Our aim was to ascertain if patients with a preoperative fixed flexion deformity performed as well as those without.
Patients and methods
During the period 1989 to 2002, 689 patients underwent a total knee arthroplasty in our centre, performed by one of five orthopaedic surgeons. Of these, 618 had a preoperative diagnosis of primary osteoarthritis (OA). Of the 618, 192 died before their ten-year follow up assessment, ten had revision surgery, 16 withdrew from the study, and contact was lost with a further 23. This left complete ten-year follow-up data for 377 patients. Patients with a preoperative fixed flexion deformity of greater than ten degrees with complete ten-year follow-up data were identified. This yielded 77 knee arthroplasties in 77 patients. Seventy seven knees in 77 age, sex and BMI matched subjects with no pre-existing FFD were then also examined.
All patients were assessed both clinically and radiographically preoperatively and at one, five and ten years post operatively by a dedicated research assistant who collected the data prospectively and entered it into a database. The database was then double-checked by a systems administrator. The maximum flexion and fixed flexion values were recorded by the research assistant using a goniometer with the patient in the supine position on the table. Knee Society scores [8] were calculated to give a functional evaluation for all patients at all four time points. Extension lag was not present in any of the patients in this study and thus has not been included in the data.
All patients in both groups received the Kinemax posterior cruciate sacrificing cemented prosthesis (Howmedica, Rutherford, NJ, USA). A standard midline incision with medial parapatellar approach and bony resection was undertaken, with the aim of the knee coming to full extension without pressure intra-operatively. The posterior cruciate ligament was excised and soft tissue balancing was performed in all cases. A tourniquet was used in all cases. Postoperatively a passive motion machine was used for 24 hours followed by intensive physiotherapy for all patients in this study.
Patients were then assessed clinically and radiologically at one, five and ten years. The research assistant was not aware of the preoperative diagnosis.
Statistical analyses
Differences within the groups were analysed using a paired t-test. Differences between groups were analysed using general linear modelling (repeated measures analysis of variance) to analyse for statistically significant differences at each of the time points (preoperative, year one, year five and year ten). This was also used to look for statistically significant differences between the group with a pre-existing FFD and the group without. Age and body mass index were added as covariates. Categorical variables between the groups were analysed using a chi-squared test. A p value of less than or equal to 0.05 was considered to be significant. All analyses were performed using SPSS version 15.0 for Windows (SPSS Inc., Chicago, IL, USA).
Results
The results of the knee function scores for those with and without preoperative FFD from the preoperative period and one year postoperatively, between years one and five, and between years five and ten, are shown in Table 1. The results for all subjects were combined and analysed to ascertain whether one group was significantly better or worse than the other group.
Table 1.
Results of knee function tests between baseline (preoperative) and at one year post procedure, year one and year five, year five and year ten in those with and without the presence of a fixed flexion deformity
| Knee function tests | Preoperative FFD | No preoperative FFD | All subjects combined | Interaction | |||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Base-line | Year one | p | Base-line | Year one | p | Base-line | Year one | p | p | η2 | |
| FFD (°) | 16.88 (5.73) | 4.14 (6.00) | < 0.001 | 0.00 (0.00) | 1.13 (3.17) | 0.003 | 8.44 (9.39) | 2.64 (5.01) | < 0.001 | < 0.001 | .680 |
| Total ROM (°) | 84.02 (18.17) | 100.66 (17.02) | < 0.001 | 102.40 (13.92) | 108.16 (12.57) | 0.002 | 93.21 (18.54) | 104.41 (15.38) | < 0.001 | 0.001 | .010 |
| Maximum flexion (°) | 100.91 (15.99) | 104.80 (13.75) | 0.062 | 102.40 (13.92) | 109.29 (11.02) | < 0.001 | 101.66 (14.90) | 107.05 (12.62) | < 0.001 | 0.355 | .007 |
| KSS | 23.95 (13.82) | 90.23 (7.80) | < 0.001 | 42.58 (12.33) | 93.22 (6.12) | < 0.001 | 33.27 (16.06) | 91.72 (7.15) | < 0.001 | < 0.001 | .200 |
| Knee function tests | Preoperative FFD | No preoperative FFD | All subjects combined | Interaction | |||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Year one | Year five | p | Year one | Year five | p | Year one | Year five | p | p | η2 | |
| FFD (°) | 4.14 (6.00) | 2.58 (4.77) | 0.002 | 1.13 (3.17) | 0.77 (2.95) | 0.244 | 2.64 (5.01) | 1.68 (4.06) | 0.001 | 0.042 | .032 |
| Total ROM (°) | 100.66 (17.02) | 103.91 (15.37) | < 0.001 | 108.16 (12.57) | 111.70 (12.87) | < 0.001 | 104.41 (15.38) | 107.66 (14.66) | < 0.001 | 0.944 | .000 |
| Maximum flexion (°) | 104.80 (13.75) | 106.49 (12.82) | < 0.001 | 109.29 (11.02) | 112.47 (11.14) | < 0.001 | 107.05 (12.62) | 109.48 (12.34) | < 0.001 | 0.264 | .010 |
| KSS | 90.23 (7.80) | 90.33 (8.10) | 0.287 | 93.22 (6.12) | 92.42 (9.11) | 0.286 | 91.72 (7.15) | 91.38 (8.65) | 0.540 | 0.637 | .002 |
| Knee function tests | Preoperative FFD | No preoperative FFD | All subjects combined | Interaction | |||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Year five | Year ten | p | Year five | Year ten | p | Year five | Year ten | p | p | η2 | |
| FFD (°) | 2.58 (4.77) | 1.09 (3.09) | 0.005 | 0.77 (2.95) | 0.32 (1.87) | 0.096 | 1.68 (4.06) | 0.71 (2.57) | 0.001 | 0.058 | .028 |
| Total ROM (°) | 103.91 (15.37) | 105.31 (13.14) | 0.302 | 111.70 (12.87) | 109.42 (13.06) | 0.014 | 107.66 (14.66) | 107.36 (14.66) | 0.593 | 0.207 | .038 |
| Maximum flexion (°) | 106.49 (12.82) | 106.40 (12.01) | 0.932 | 112.47 (11.14) | 109.74 (11.92) | 0.001 | 109.48 (12.34) | 109.48 (12.34) | 0.039 | 0.052 | .008 |
| KSS | 90.33 (8.10) | 86.94 (16.34) | 0.046 | 92.42 (9.11) | 88.35 (13.42) | 0.004 | 91.38 (8.65) | 87.64 (14.99) | 0.001 | 0.349 | .007 |
FFD fixed flexion deformity, ROM range of movement, KSS Knee Society score
Values given as mean and (standard deviation)
The mean age for those with a preoperative FFD was 69.7 ± 7.0 compared to 70.4 ± 7.1 years in those without (p = 0.52). There was no significant difference in gender (p = 0.46) or body mass index (p = 0.14) between the groups. There was also no significant effect of age or body mass index observed in any of the general linear modelling (repeated measures) analyses.
Fixed flexion
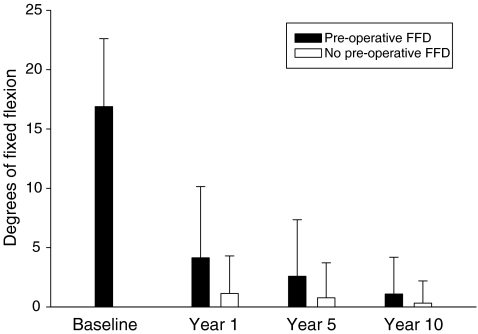
In those with a preoperative FFD a statistically significant decrease in the mean fixed flexion was demonstrated between preoperative and year one follow-up (16.9 ± 5.7 vs 4.1 ± 6.0, respectively; p < 0.001), years one and five (4.2 ± 6.0 vs 2.6 ± 4.8, respectively; p < 0.001) and between years five and ten (2.6 ± 4.8 vs 1.1 ± 3.1, respectively; p = 0.009) (Fig. 1). In those with no preoperative FFD the fixed flexion increased significantly at the end of the first year (0.0 ± 0.0 vs 1.1 ± 3.2, respectively; p = 0.003). No significant improvement was seen between years one and five (1.1 ± 3.2 vs 0.8 ± 3.0, respectively; p = 0.244), although there was a trend to improvement between years five and ten (0.8 ± 3.0 vs 0.3 ± 1.9; respectively; p = 0.096). The interaction between the two groups was significant between preoperative and year one (p < 0.001), years one to five (p = 0.04) and just failed to reach statistical significance between years five and ten (p = 0.058). These results would be expected due to the surgical correction of the fixed flexion deformity whereas those without a fixed flexion have no room for improvement.
Fig. 1.
Fixed flexion results (mean as bar with SD as error bars) at baseline, year one, year five and at year ten post total knee arthroplasty (TKA) in those with and without fixed flexion deformity. FFD fixed flexion deformity
Total range of movement
The total range of movement in both groups improved significantly up to five years post arthroplasty (from 84.02 to 103.91 degrees in those with a FFD and from 102.4 to 111.7 in those without). No significant change was observed between five and ten years (p = 0.302) in those with a preoperative FFD whilst those with no FFD had a significant decrease in ROM (p = 0.014) between these time points. The interaction between the groups was significant at year one only (p = 0.007), suggesting that the subjects with a preexisting FFD improved substantially more during this period reflecting the gain in extension from the operative correction of the FFD.
Maximum flexion
At the time point of preoperative to year one a significant increase in maximum flexion was observed in those with (p = 0.042) and without a preoperative FFD (p < 0.001). Similar improvements were observed between years one to five. Between five and ten years the maximum flexion remained static in those with a preoperative FFD (106.5 ± 12.8 vs 106.0 ± 12.0, respectively; p = 0.932) and decreased in those without a preoperative FFD (112.5 ± 11.1 vs 109.7 ± 11.9, respectively; p = 0.039). No significant interactions were observed at any time point between the groups.
Knee Society scores
The Knee Society scores increased markedly during the first year in both groups (p < 0.001). No statistically significant change was observed in either group in Knee Society scores between years one and five. A statistically significant decrease was observed in those with pre-existing FFD (90.3 ± 8.1 vs 86.9 ± 16.3, respectively; p = 0.046) and those without (92.4 (± 9.1 vs 88.4 ± 13.4, respectively; p = 0.004) between the five- and ten-year time points. The interaction between the groups was significant at preoperative to year one only (p < 0.001), suggesting that the subjects with a preexisting FFD gained more during this period, but the final outcome in both groups were similar.
Discussion
This study demonstrates a continued and sustained improvement in fixed flexion deformity up to ten years after knee arthroplasty. In those without a preoperative FFD, an initial increase in fixed flexion was observed in the first year which is consistent with previously published research [8]; however, there was a trend to improvement at ten years. A significant interaction between the groups was observed for fixed flexion, total range of movement and Knee Society scores at the one year. This suggests that those with a preexisting FFD demonstrated a greater improvement in the first year, which could be explained by the fact that this group started off worse and improved significantly due to the correction of their fixed flexion deformity. A significant interaction with regard to fixed flexion was also observed at five years and just failed to reach significance at ten years, demonstrating a continued and sustained improvement throughout this period. Our results also show that the final total ROM at ten years was better in the group with no FFD than in those with (103.51 versus 109.42, respectively). As far as we are aware, this study is the first to compare the effects of TKA in both those with and those without FFD and apply statistical methodology to ascertain differences between the groups.
Similar studies have shown a continued improvement in fixed flexion deformity. Lizaur et al. prospectively followed-up 83 arthroplasties (in 74 patients with a diagnosis of OA) up to a 12-month postoperative period [7]. Significant reduction in flexion contractures and increases in flexion were demonstrated at this stage. Similar results were observed by Tanzer et al. who prospectively studied 33 patients for a mean duration of 55 weeks and again demonstrated that flexion contractures can improve after total knee arthroplasty (TKA) [9]. Two-year follow-up data from McPherson et al. reported that in 29 patients a continued improvement in the degree of flexion contracture was observed up to two years [10]. In contrast, Tew et al. studied 697 TKAs and followed them up from 1–16 years [6]. They found no postoperative improvement or deterioration in flexion deformity but the data included both osteoarthritis and rheumatoid arthritis as well as subjects who had undergone revision surgery. A total of 11 different knee prostheses were used with fixed flexion angles assessed by three surgeons which may have introduced a degree of inter-individual variability. Ritter et al. reviewed 5,622 TKAs in patients with OA, RA and osteonecrosis, using 22 different knee prostheses performed by five surgeons. He demonstrated that the greater the postoperative FFD the higher the likelihood of a poor outcome [11]. By comparison our study has a homogenous cohort (OA attending for primary surgery with the same implant) assessed by a dedicated research assistant. Our study however does have some limitations. Due to the long follow-up period a significant proportion of participants (39%) were ineligible for follow-up due to death, withdrawal from the study and requisite for revision surgery. This therefore may have affected the results obtained. The use of a homogenous cohort of participants from a single centre who all received one type of implant (Kinemax PS) may also therefore limit the widespread application of these results.
While the functional range of movement after TKA remains the primary outcome variable for studies, numerous differing methods exist to analyse this, namely, goniometry, electrogoniometry, gait analysis and radiographic examination. Simple goniometry was chosen for this study for its ease given the large number of subjects studied (n = 618) and cost-effectiveness, unlike the other methods which are time consuming, expensive and, in the case of the radiographic methods, raise ethical issues regarding exposure to X-rays for research purposes. Previous research has demonstrated that range of motion, flexion contracture, and extension lag in knee examinations have shown a high intra-observer correlation using a simple goniometer [12–15].
In summary, our study demonstrates that patients with a preoperative fixed flexion deformity show continued improvement in their fixed flexion up to ten years after arthroplasty and have similar outcomes to those with no preoperative fixed flexion.
References
- 1.Swanson SAV. Biomechanics. In: Aubriot H, Freeman MAR, editors. Arthritis of the knee: clinical features and surgical management. Berlin: Springer-Verlag; 1980. pp. 1–30. [Google Scholar]
- 2.Laubenthal KN, Smidt GL, Kettelkamp DB. A quantitative analysis of knee motion during activities of daily living. Phys Ther. 1972;52:34–43. doi: 10.1093/ptj/52.1.34. [DOI] [PubMed] [Google Scholar]
- 3.Ritter MA, Campbell ED. Effect of range of motion on the success of a total knee arthroplasty. J Arthroplasty. 1987;2:95–97. doi: 10.1016/S0883-5403(87)80015-3. [DOI] [PubMed] [Google Scholar]
- 4.Callahan CM, Drake BG, Heck DA, Dittus RS. Patient outcomes following tricompartmental total knee replacement. A meta-analysis. JAMA. 1994;271:1349–1357. doi: 10.1001/jama.271.17.1349. [DOI] [PubMed] [Google Scholar]
- 5.Dennis DA, Komistek RD, Stiehl JB, Walker SA, Dennis KN. Range of motion after total knee arthroplasty: the effect of implant design and weight-bearing conditions. J Arthroplasty. 1998;13:748–752. doi: 10.1016/S0883-5403(98)90025-0. [DOI] [PubMed] [Google Scholar]
- 6.Ritter MA, Harty LD, Davis KE, Meding JB, Berend ME. Predicting range of motion after total knee arthroplasty. Clustering, log-linear regression, and regression tree analysis. J Bone Joint Surg Am. 2003;85-A:1278–1285. doi: 10.2106/00004623-200307000-00014. [DOI] [PubMed] [Google Scholar]
- 7.Tew M, Forster IW. Effect of knee replacement on flexion deformity. J Bone Joint Surg Br. 1987;69:395–399. doi: 10.1302/0301-620X.69B3.3584192. [DOI] [PubMed] [Google Scholar]
- 8.Insall JN, Dorr LD, Scott RD, Scott WN (1989) Rationale of the Knee Society clinical rating system. Clin Orthop Relat Res (248):13–14 [PubMed]
- 9.Lizaur A, Marco L, Cebrian R. Preoperative factors influencing the range of movement after total knee arthroplasty for severe osteoarthritis. J Bone Joint Surg Br. 1997;79:626–629. doi: 10.1302/0301-620X.79B4.7242. [DOI] [PubMed] [Google Scholar]
- 10.Tanzer M, Miller J (1989) The natural history of flexion contracture in total knee arthroplasty. A prospective study. Clin Orthop Relat Res (248):129–134 [PubMed]
- 11.Ritter MA, Lutgring JD, Davis KE, Berend ME, Pierson JL, Meneghini RM. The role of flexion contracture on outcomes in primary total knee arthroplasty. J Arthroplasty. 2007;22:1092–1096. doi: 10.1016/j.arth.2006.11.009. [DOI] [PubMed] [Google Scholar]
- 12.Myles CM, Rowe PJ, Walker CR, Nutton RW. Knee joint functional range of movement prior to and following total knee arthroplasty measured using flexible electrogoniometry. Gait Posture. 2002;16:46–54. doi: 10.1016/S0966-6362(01)00198-9. [DOI] [PubMed] [Google Scholar]
- 13.Brosseau L, Tousignant M, Budd J, Chartier N, Duciaume L, Plamondon S, O'Sullivan JP, O'Donoghue S, Balmer S. Intratester and intertester reliability and criterion validity of the parallelogram and universal goniometers for active knee flexion in healthy subjects. Physiother Res Int. 1997;2:150–166. doi: 10.1002/pri.97. [DOI] [PubMed] [Google Scholar]
- 14.Mayerson NH, Milano RA. Goniometric measurement reliability in physical medicine. Arch Phys Med Rehab. 1984;65:92–94. [PubMed] [Google Scholar]
- 15.Rothstein JM, Miller PJ, Roettger RF. Goniometric reliability in a clinical setting. Elbow and knee measurements. Phys Ther. 1983;63:1611–1615. doi: 10.1093/ptj/63.10.1611. [DOI] [PubMed] [Google Scholar]