Abstract
In order to prevent hip arthroplasty dislocations, information regarding the direction of the dislocation is important for accurate implant positioning and for optimising the postoperative regimens in relation to the surgical approach used. The aim of this study was to analyse the influence of the surgical approach on the direction of the dislocation in patients treated by a hemiarthroplasty (HA) or total hip arthroplasty (THA) after a femoral neck fracture. Fracture patients have a high risk for dislocations, and this issue has not been previously studied in a selected group of patients with a femoral neck fracture. We analysed the radiographs of the primary dislocation in 74 patients who had sustained a dislocation of their HA (n = 42) or THA (n = 32). In 42 patients an anterolateral (AL) surgical approach was used and in 32 a posterolateral (PL). The surgical approach significantly influenced the direction of dislocation in patients treated with HA (p < 0.001), while no such correlation was found after THA (p = 0.388). For THA patients there was a correlation between the mean angle of anteversion of the acetabular component and the direction of dislocation when comparing patients with anterior and posterior dislocations (p = 0.027). These results suggest that the surgical approach of a HA has an influence on the direction of dislocation, in contrast to THA where the position of the acetabular component seems to be of importance for the direction of dislocation in patients with femoral neck fractures.
Introduction
A dislocation of the prosthesis is a relatively common, severe and expensive complication after hip arthroplasty surgery [1–3]. While the overall dislocation rate for the various surgical approaches and diagnoses has been reported in a number of papers, less attention has been paid to the influence of the surgical approach on the direction of dislocation of the prosthesis [4–6]. In routine health care it is often assumed that patients operated upon using an anterior surgical approach are more likely to dislocate anteriorly, and vice versa for a posterior approach. Although information concerning this issue is valuable and has implications for selecting an accurate implant position and for optimising the postoperative rehabilitation regimens in relation to the surgical approach and thereby possibly preventing dislocations, studies regarding this specific issue are few.
In a paper from 1982, Woo and Morrey [4] reported that 77% of patients who had undergone a total hip arthroplasty (THA) using a posterior approach and subsequently sustaining a dislocation presented with a posterior dislocation, while patients operated upon through an anterior approach had an equal distribution between anterior and posterior dislocations at 46% each. The results for the anterolateral approach have been confirmed by Biedermann et al. [6] and those for the posterolateral approach by Pierchon et al. [5]. However, the majority of the patients in these studies were treated for degenerative joint disease.
Patients undergoing an arthroplasty after a fracture of the femoral neck, either primarily or secondarily after a failed internal fixation, run a substantially higher risk of dislocation [1, 4, 7] compared to those operated on for osteoarthritis (OA) or rheumatoid arthritis (RA) [8]. In fracture patients the incidence of dislocation ranges between 2% and 16% for hemiarthroplasty (HA) [9–11] and between 2% and 22% for THA [12–15].
The principal modern surgical approaches for hip arthroplasty are the anterolateral [16] and the posterolateral [17] approaches. The optimal technique remains controversial for patients with OA and RA; increasing evidence suggests that the anterolateral approach, as compared to the posterolateral, provides significantly better stability after both HA and THA in patients with a femoral neck fracture [9–11, 15, 18, 19]. In fracture patients, the influence of the surgical approach on the direction of dislocation of the arthroplasty has not been studied previously, after HA nor after THA.
The aim of this study was to analyse the influence of the surgical approach on the direction of dislocation of the hip arthroplasty in patients undergoing HA or THA after a femoral neck fracture.
The study was conducted in conformity with the Helsinki Declaration and was approved by the Regional Ethics Committee in Stockholm (reference no. 2008/63–31/3).
Patients and methods
Between January 1996 and September 2008 a total of 1,741 HAs and 970 THAs were performed due to a femoral neck fracture at our department at the Stockholm Söder Hospital. We searched this cohort to find all patients with a primary dislocation of their arthroplasty within one year after prosthesis surgery and who had radiographs of diagnostic quality available. We identified and included 74 (63 females) patients with a HA (n = 42) or a THA (n = 32), treated by a primary arthroplasty (n = 40) for a displaced femoral neck fracture (Garden III and IV) [20] or a secondary arthroplasty (n = 34) after failure of internal fixation of a femoral neck fracture. An anterolateral [16] surgical approach was used in 42 patients and a posterolateral [17] in 32. On every occasion, the selection of the surgical approach was determined by the individual surgeon’s preference. An additional 36 patients were identified from whom radiographs of diagnostic quality were lacking, giving a total dislocation rate of 4.1% within the first year after surgery. There were no differences in patient characteristics when comparing the patients included in the study and those lacking radiographs allowing interpretation (data not shown).
For the analyses, the patients were divided into four groups depending on the type of arthroplasty, HA or THA, and the surgical approach, anterolateral (AL) or posterolateral (PL). Baseline data, with reference to the type of arthroplasty and surgical approach, for all patients are displayed in Table 1. As expected, the patients in the THA group were younger and the HAs were performed more often as a primary procedure.
Table 1.
Baseline data for all patients included in relation to the type of prosthesis and surgical approach (n = 74)
| Description | HA/AL n = 28 |
HA/PL n = 14 |
THA/AL n = 14 |
THA/PL n = 18 |
|
|---|---|---|---|---|---|
| Age (years); mean (SD, range) | 83.0 (8.6, 58–96) | 81.0 (5.3, 66–87) | 70.3 (9.8, 53–87) | 76.7 (10.0, 57–90) | |
| Gender, n (%) | Male (n = 11) | 4 (15) | 2 (14) | 3 (21) | 2 (11) |
| Female (n = 63) | 24 (85) | 12 (86) | 11 (79) | 16 (89) | |
| Indication, n (%) | Primary (n = 40) | 19 (68) | 8 (57) | 4 (29) | 9 (50) |
| Secondary (n = 34) | 9 (32) | 6 (43) | 10 (71) | 9 (50) | |
HA hemiarthroplasty, THA total hip arthroplasty, AL anterolateral surgical approach, PL posterolateral surgical approach
Radiological analysis
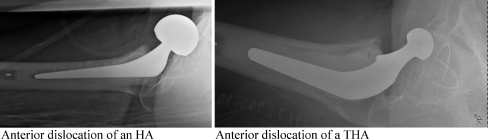
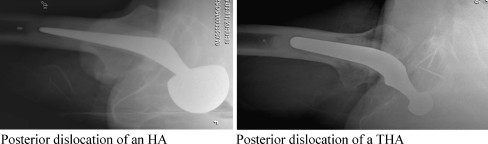
The radiological analysis was performed by an independent radiologist who was blinded to the surgical approach. The lateral radiograph from the time of the primary dislocation was analysed and the position of the head of the dislocated prosthesis was classified as anterior, posterior or superior in relation to the acetabulum (HA) or the acetabular component (THA). This position was assumed to be the route and direction of the dislocation of the prosthesis [4, 21] (Figs. 1 and 2). Angles of inclination and anteversion of the acetabular component were measured with regard to the patients with THA on the anteroposterior and the lateral radiographs, respectively, using the method previously described by Woo and Morrey [4].
Fig. 1.
Anterior dislocation of a hemiarthroplasty (HA). Anterior dislocation of a total hip arthroplasty (THA)
Fig. 2.
Posterior dislocation of a hemiarthroplasty (HA). Posterior dislocation of a total hip arthroplasty (THA)
Statistics
Scale variables were tested using one-way ANOVA and a post hoc analysis was performed when comparing groups using a t-test with Bonferroni correction adjusted for three groups. The normality assumption within each group was tested with the Shapiro-Wilks test and homogeneity of the variances was tested with Levene’s test. Nominal variables were tested two-sided by the Fisher’s exact test. The results were considered significant at p < 0.05. All analyses were performed using SPSS version 16.0 (SPSS, Inc., Chicago, IL).
Results
The mean (SD; range) time from surgery to the primary dislocation was 32 (41; 0–242) days.
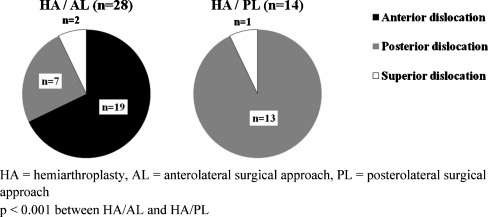
The direction of dislocation in relation to the surgical approach for the HA group is displayed in Fig. 3. In the HA/AL group the dislocations were categorised as anterior in 19 patients (68%), posterior in seven (25%) and superior in two (7%). No patient in the HA/PL group had an anterior dislocation, 13 patients (93%) had a posterior dislocation and one patient (7%) had a superior dislocation. This difference in the direction of the dislocation between the HA/AL and the HA/PL groups was significant (p < 0.001).
Fig. 3.
The direction of dislocation in relation to the surgical approach in the hemiarthroplasty (HA) group (n = 42)
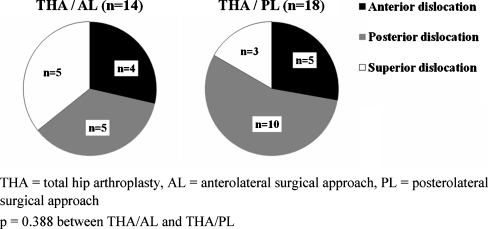
The direction of dislocation in relation to the surgical approach for the THA group is shown in Fig. 4. In the THA/AL group the dislocations were categorised as anterior in four patients (29%), posterior in five (36%) and superior in five (36%). In the THA/PL group five patients (28%) had an anterior dislocation, ten (56%) a posterior dislocation and three (17%) a superior dislocation. There was no significant (p = 0.388) difference between the THA/AL and THA/PL groups regarding the direction of the dislocation.
Fig. 4.
The direction of dislocation in relation to the surgical approach in the total hip arthroplasty (THA) group (n = 32)
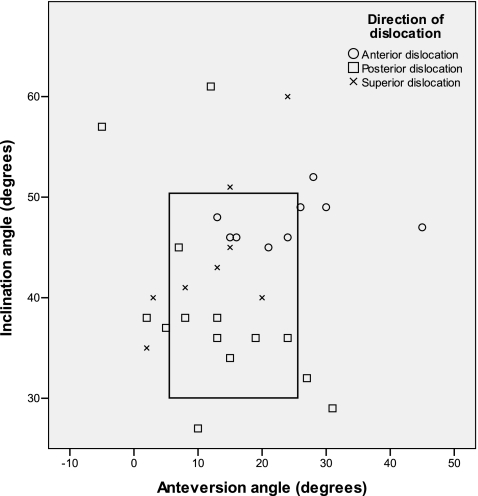
The inclination and anteversion angles of the acetabular component in relation to the direction of dislocation in patients with a THA are displayed in Table 2 and Fig. 5. The mean angle of inclination was 48° in patients with an anterior dislocation, 39° in patients with a posterior dislocation and 44° in patients with a superior dislocation. Only the difference between the anterior and posterior dislocation groups was significant (p = 0.045). The mean angle of anteversion was 24° in patients with an anterior dislocation and 13° in patients with posterior and superior dislocations, respectively. The differences between the anterior and posterior and between the anterior and superior dislocation groups were significant (p = 0.027 and p = 0.048, respectively).
Table 2.
The inclination and anteversion of the acetabular component in relation to the direction of dislocation in patients with total hip arthroplasty (THA) (n = 32)
| Angles | Anterior (n = 9) | Posterior (n = 15) | Superior (n = 8) | p |
|---|---|---|---|---|
| Inclinationa | 48° (2.2; 45–52) | 39° (9.6; 27–61)c | 44° (7.8; 35–60) | 0.037 |
| Anteversionb | 24° (9.8; 13–45) | 13° (9.6;–5–31) | 13° (7.8; 2–24) | 0.012 |
Values given as mean (SD, range)
a p-values between groups after Bonferroni correction: anterior versus posterior 0.045, anterior versus superior 0.777 and posterior versus superior 0.546
b p-values between groups after Bonferroni correction were: anterior versus posterior 0.027, anterior versus superior 0.048 and posterior versus superior 1.0
c One missing value
Fig. 5.
The angles of inclination and anteversion for the acetabular component for total hip arthroplasty (THA) patients in relation to the direction of dislocation. The “safe zone” according to Lewinnek et al. [22] (inclination 40 ± 10°, anteversion 15 ± 10°) is marked in the figure
Discussion
In this study on patients who had undergone a primary or secondary hip arthroplasty after a femoral neck fracture, we found that an HA inserted through a posterolateral approach dislocated significantly more often posteriorly (93%), while an HA inserted through an anterolateral approach more often dislocated anteriorly (68%). However, after a THA in fracture patients, we did not find any significant correlation between the surgical approach and the direction of dislocation, suggesting that the surgical approach is only one of several factors affecting the direction of dislocation after a THA. Our results imply that the position of the acetabular component might be one important factor.
Our finding that the direction of dislocation of an HA in patients with a femoral neck fracture is highly dependent on the surgical approach has not been reported previously. In the absence of an acetabular component, the direction of dislocation is influenced by the position of the femoral component and/or the surgical approach. The position of the femoral stem may differ slightly between the different approaches but, on the other hand, the condition for an optimal implant position is an important characteristic of the surgical approach. Therefore, the surgical approach is likely to be the most important factor determining the direction of dislocation. It is reasonable to assume that the femoral head is prone to dislocate in a direction in which the soft tissues have been weakened by surgery. A posterior dislocation in the hip results from a flexion/internal rotation, a much more common position in the daily life of an elderly patient compared to extension/external rotation, the position which may result in an anterior dislocation. This may be one important reason why dislocations are so frequent after the posterolateral approach in elderly patients with femoral neck fractures, and also why some patients (25%) operated upon via an anterolateral approach had a posterior dislocation.
We recently reported factors influencing the stability of HA and THA in patients with femoral neck fracture with special reference to the surgical approach within the context of two large prospective cohort trials [11, 15]. After both HA and THA the anterolateral approach was associated with a significantly lower risk for dislocation than the posterolateral approach with or without posterior repair: for HA 3.0%, 8.5%, and 13.0%, respectively (p < 0.001), and for THA 1.9%, 11.8% and 13.6%, respectively (p < 0.001).
One previous study, by Woo and Morrey [4], assessed the influence of various surgical approaches on the direction of dislocation after THA. In their retrospective study including 43 patients with a dislocated THA, the majority (77%) of the patients operated on via a posterior approach had a posterior dislocation, but patients operated on via an anterior approach had an equal distribution between anterior (46%) and posterior (46%) dislocations. Biederman et al. [6] reported similar results in 83 patients who had had a primary THA via an anterolateral approach: 46% anterior dislocations and 45% posterior dislocations. Finally, Pierchon et al. [5] reported 95% posterior and 5% anterior dislocations in a study on 38 patients with a primary or a secondary THA performed via a posterolateral surgical approach. However, although not clearly stated in the papers, the majority of the patients in these three studies were treated for degenerative joint disease and it is not clear whether any fracture patients were included. In our study, including only patients with femoral neck fracture, we found no significant difference in the direction of dislocation between THA patients operated upon via anterolateral and posterolateral approaches. There was a tendency towards posterior (56%), as compared to anterior (28%), dislocations among patients operated on using a posterolateral approach and a more equal distribution between posterior (29%) and anterior (36%) dislocations among patients operated on via an anterolateral approach. The interpretation of these results is, however, difficult as 25% of the THA patients had a superior dislocation. The superior dislocations are most likely a result of an anterior or a posterior dislocation in which the abductor muscles have pulled the dislocated femur in a cranial direction, leaving the femoral head in a position superior to the socket. A true superior dislocation may occur in excessive adduction in combination with a vertically placed acetabular component [4, 22, 23]. This seems to be a less likely explanation in our study as none of our patients had an inclination angle exceeding 61°. However, the surrounding soft tissues may contribute to the stability of the joint and the possibility that some of our patients had compromised soft tissues, resulting in a true superior dislocation cannot be ruled out.
The association between the position of the acetabular component and the risk for dislocation has been discussed in several studies. The socket is usually recommended to be inserted with an inclination angle of 30° to 50° and an anteversion angle of 5° to 25° [6, 24–26]. In our study the angle of anteversion was greater for patients with anterior dislocations than for those with posterior dislocations. This is in line with the results of Biederman et al. [6] and Masaoka et al. [27] who reported an increased risk for anterior dislocation as anteversion of the acetabular component increased and vice versa for posterior dislocation. However, other authors have not been able to demonstrate any correlation between socket anteversion and the risk for dislocations [5, 28, 29]. The influence of the angle of inclination on the direction of the dislocation is even more unclear. Our results, as well as those of others do not support the view that this is a factor of major importance [5, 6, 28, 29].
One strength of our study is that the patients were included from a cohort treated at one hospital during a defined period of time where the selection of the surgical approach was determined by the individual surgeon’s preference. Moreover, the patient cohort was well defined and included only patients with a femoral neck fracture. Another strength is that the radiological analysis was performed by an independent radiologist who was blinded to the surgical approach.
The method we used to assess the direction of dislocation, i.e. from radiographs, may be criticised, although the same method has been used in previous studies [4, 21]. We have discussed the difficulties in the interpretation of the superior dislocations. An alternative method for assessing the direction of dislocation could be to test the stability and direction of the dislocation of the prosthesis at the time of the reduction manoeuvre. However, this may be difficult to achieve in routine health care since many of the reductions are performed by junior surgeons outside office hours who may be reluctant to redislocate the hip after having successfully reduced it. Furthermore, our method for assessing the position of the acetabular component has limitations even though it has been used by several previous authors [4, 21, 22, 28–30]. Measuring the anteversion of the socket may be especially difficult since no true reference line is available in the pelvis. However, the method gives a fair estimate of the position of the socket and gross malpositioning can be appreciated. Another weakness of this study is the lack of assessments of the femoral stem anteversion. A malpositioned femoral component is a well-known risk factor for prosthetic dislocation and may also influence the direction of the dislocation [22]. As previously stated, the prerequisites for an optimal stem position are an important feature of the surgical approach. However, McCollum and Gray [31] stated that the orientation of the femoral component is assumed to be less critical than that of the acetabular component, and the most common cause of failure is the orientation of the acetabular, rather than the femoral, component [22, 32]. A more detailed analysis of the position of the acetabular component and the femoral stem anteversion requires assessment with CT [5, 23]. Furthermore, as only patients with primary radiographs allowing interpretation were of interest to this study, theoretically, there could have been selection with regard to surgical approach and/or direction of dislocation. However, in summary, we believe that the weaknesses of our study, as stated above, should not jeopardise the validity of our main conclusions.
The treatment of displaced femoral neck fractures with HA or THA has a good and predictable outcome regarding the need for revision surgery, hip function and health-related quality of life [14, 19, 33, 34]. However, dislocation of the prosthesis remains a significant problem, especially after the posterolateral approach [9–11, 15, 18]. In this study we have shown that the surgical approach influences the direction of dislocation in HA patients, but the approach does not seem to have the same influence in THA patients in whom the position of the acetabular component seems to play an important role. The implications of our results are that the postoperative mobilisation in patients with HA should be dependent on the surgical approach used. For THA patients the mobilisation regimen should include strategies aiming to reduce the risk of both anterior and posterior dislocation regardless of the surgical approach used. Moreover, when performing THA in patients with a femoral neck fracture, special attention should be paid to optimal positioning of the acetabular component.
References
- 1.Meek RM, Allan DB, McPhillips G, Kerr L, Howie CR. Epidemiology of dislocation after total hip arthroplasty. Clin Orthop Relat Res. 2006;447:9–18. doi: 10.1097/01.blo.0000218754.12311.4a. [DOI] [PubMed] [Google Scholar]
- 2.Sanchez-Sotelo J, Haidukewych GJ, Boberg CJ. Hospital cost of dislocation after primary total hip arthroplasty. J Bone Jt Surg Am. 2006;88:290–294. doi: 10.2106/JBJS.D.02799. [DOI] [PubMed] [Google Scholar]
- 3.Bosker BH, Ettema HB, Verheyen CC, Castelein RM. Acetabular augmentation ring for recurrent dislocation of total hip arthroplasty: 60% stability rate after an average follow-up of 74 months. Int Orthop. 2009;33:49–52. doi: 10.1007/s00264-007-0456-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Woo RY, Morrey BF. Dislocations after total hip arthroplasty. J Bone Jt Surg Am. 1982;64:1295–1306. [PubMed] [Google Scholar]
- 5.Pierchon F, Pasquier G, Cotten A, Fontaine C, Clarisse J, Duquennoy A. Causes of dislocation of total hip arthroplasty. CT study of component alignment. J Bone Jt Surg Br. 1994;76:45–48. [PubMed] [Google Scholar]
- 6.Biedermann R, Tonin A, Krismer M, Rachbauer F, Eibl G, Stockl B. Reducing the risk of dislocation after total hip arthroplasty: the effect of orientation of the acetabular component. J Bone Jt Surg Br. 2005;87:762–769. doi: 10.1302/0301-620X.87B6.14745. [DOI] [PubMed] [Google Scholar]
- 7.Berry DJ, Knoch M, Schleck CD, Harmsen WS. The cumulative long-term risk of dislocation after primary Charnley total hip arthroplasty. J Bone Jt Surg Am. 2004;86-A:9–14. doi: 10.2106/00004623-200401000-00003. [DOI] [PubMed] [Google Scholar]
- 8.Philippot R, Camilleri JP, Boyer B, Adam P, Farizon F. The use of a dual-articulation acetabular cup system to prevent dislocation after primary total hip arthroplasty: analysis of 384 cases at a mean follow-up of 15 years. Int Orthop. 2009;33:927–932. doi: 10.1007/s00264-008-0589-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Pajarinen J, Savolainen V, Tulikoura I, Lindahl J, Hirvensalo E. Factors predisposing to dislocation of the Thompson hemiarthroplasty: 22 dislocations in 338 patients. Acta Orthop Scand. 2003;74:45–48. doi: 10.1080/00016470310013644. [DOI] [PubMed] [Google Scholar]
- 10.Varley J, Parker MJ. Stability of hip hemiarthroplasties. Int Orthop. 2004;28:274–277. doi: 10.1007/s00264-004-0572-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Enocson A, Tidermark J, Törnkvist H, Lapidus LJ. Dislocation of hemiarthroplasty after femoral neck fracture: better outcome after the anterolateral approach in a prospective cohort study on 739 consecutive hips. Acta Orthop. 2008;79:211–217. doi: 10.1080/17453670710014996. [DOI] [PubMed] [Google Scholar]
- 12.Lu-Yao GL, Keller RB, Littenberg B, Wennberg JE. Outcomes after displaced fractures of the femoral neck. A meta-analysis of one hundred and six published reports. J Bone Jt Surg Am. 1994;76:15–25. doi: 10.2106/00004623-199401000-00003. [DOI] [PubMed] [Google Scholar]
- 13.Johansson T, Jacobsson SA, Ivarsson I, Knutsson A, Wahlström O. Internal fixation versus total hip arthroplasty in the treatment of displaced femoral neck fractures: a prospective randomized study of 100 hips. Acta Orthop Scand. 2000;71:597–602. doi: 10.1080/000164700317362235. [DOI] [PubMed] [Google Scholar]
- 14.Tidermark J, Ponzer S, Svensson O, Söderqvist A, Törnkvist H. Internal fixation compared with total hip replacement for displaced femoral neck fractures in the elderly. A randomised, controlled trial. J Bone Jt Surg Br. 2003;85:380–388. doi: 10.1302/0301-620X.85B3.13609. [DOI] [PubMed] [Google Scholar]
- 15.Enocson A, Hedbeck C-J, Tidermark J, Pettersson H, Ponzer S, Lapidus LJ. Dislocation of total hip replacement in patients with fractures of the femoral neck. A prospective cohort study on 713 consecutive hips. Acta Orthop. 2009;80:184–189. doi: 10.3109/17453670902930024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Hardinge K. The direct lateral approach to the hip. J Bone Jt Surg Br. 1982;64:17–19. doi: 10.1302/0301-620X.64B1.7068713. [DOI] [PubMed] [Google Scholar]
- 17.Moore AT. The self-locking metal hip prosthesis. J Bone Jt Surg Am. 1957;39-A:811–827. [PubMed] [Google Scholar]
- 18.Keene GS, Parker MJ. Hemiarthroplasty of the hip-the anterior or posterior approach? A comparison of surgical approaches. Injury. 1993;24:611–613. doi: 10.1016/0020-1383(93)90125-P. [DOI] [PubMed] [Google Scholar]
- 19.Keating JF, Grant A, Masson M, Scott NW, Forbes JF. Randomized comparison of reduction and fixation, bipolar hemiarthroplasty, and total hip arthroplasty. Treatment of displaced intracapsular hip fractures in healthy older patients. J Bone Jt Surg Am. 2006;88:249–260. doi: 10.2106/JBJS.E.00215. [DOI] [PubMed] [Google Scholar]
- 20.Garden RS. Low-angle fixation in fractures of the femoral neck. J Bone Jt Surg. 1961;43-B:647–663. [Google Scholar]
- 21.Cobb TK, Morrey BF, Ilstrup DM. The elevated-rim acetabular liner in total hip arthroplasty: relationship to postoperative dislocation. J Bone Jt Surg Am. 1996;78:80–86. doi: 10.2106/00004623-199601000-00011. [DOI] [PubMed] [Google Scholar]
- 22.Daly PJ, Morrey BF. Operative correction of an unstable total hip arthroplasty. J Bone Jt Surg Am. 1992;74:1334–1343. [PubMed] [Google Scholar]
- 23.Mian SW, Truchly G, Pflum FA (1992) Computed tomography measurement of acetabular cup anteversion and retroversion in total hip arthroplasty. Clin Orthop Relat Res 206–209 [PubMed]
- 24.Lewinnek GE, Lewis JL, Tarr R, Compere CL, Zimmerman JR. Dislocations after total hip-replacement arthroplasties. J Bone Jt Surg Am. 1978;60:217–220. [PubMed] [Google Scholar]
- 25.Ali Khan MA, Brakenbury PH, Reynolds IS. Dislocation following total hip replacement. J Bone Jt Surg Br. 1981;63-B:214–218. doi: 10.1302/0301-620X.63B2.7217144. [DOI] [PubMed] [Google Scholar]
- 26.Dorr LD, Wan Z (1998) Causes of and treatment protocol for instability of total hip replacement. Clin Orthop Relat Res 144–151 [DOI] [PubMed]
- 27.Masaoka T, Yamamoto K, Shishido T, Katori Y, Mizoue T, Shirasu H, Nunoda D. Study of hip joint dislocation after total hip arthroplasty. Int Orthop. 2006;30:26–30. doi: 10.1007/s00264-005-0032-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Pollard JA, Daum WJ, Uchida T. Can simple radiographs be predictive of total hip dislocation? J Arthroplast. 1995;10:800–804. doi: 10.1016/S0883-5403(05)80078-6. [DOI] [PubMed] [Google Scholar]
- 29.Paterno SA, Lachiewicz PF, Kelley SS. The influence of patient-related factors and the position of the acetabular component on the rate of dislocation after total hip replacement. J Bone Jt Surg Am. 1997;79:1202–1210. doi: 10.2106/00004623-199708000-00013. [DOI] [PubMed] [Google Scholar]
- 30.Zwartele RE, Brand R, Doets HC. Increased risk of dislocation after primary total hip arthroplasty in inflammatory arthritis: a prospective observational study of 410 hips. Acta Orthop Scand. 2004;75:684–690. doi: 10.1080/00016470410004049. [DOI] [PubMed] [Google Scholar]
- 31.McCollum DE, Gray WJ (1990) Dislocation after total hip arthroplasty. Causes and prevention. Clin Orthop Relat Res 159–170 [PubMed]
- 32.Morrey BF (1997) Difficult complications after hip joint replacement. Dislocation. Clin Orthop Relat Res 179–187 [PubMed]
- 33.Blomfeldt R, Törnkvist H, Eriksson K, Söderqvist A, Ponzer S, Tidermark J. A randomised controlled trial comparing bipolar hemiarthroplasty with total hip replacement for displaced intracapsular fractures of the femoral neck in elderly patients. J Bone Jt Surg Br. 2007;89:160–165. doi: 10.1302/0301-620X.89B2.18576. [DOI] [PubMed] [Google Scholar]
- 34.Frihagen F, Grotle M, Madsen JE, Wyller TB, Mowinckel P, Nordsletten L. Outcome after femoral neck fractures: a comparison of Harris hip score, Eq-5d and Barthel index. Injury. 2008;39:1147–1156. doi: 10.1016/j.injury.2008.03.027. [DOI] [PubMed] [Google Scholar]