Abstract
We conducted a prospective randomised study comparing the clinical, functional and radiographic results of 46 patients treated for scaphoid nonunion using a vascularised bone graft from the dorsal and distal aspect of the radius (group I), relative to 40 patients treated by means of a conventional non-vascularised bone graft from the distal radius (group II). Surgical findings included 30 sclerotic, poorly-vascularised scaphoids in group I versus 20 in group II. Bone fusion was achieved in 89.1% of group I and 72.5% of group II patients (p = 0.024). Functional results were good to excellent in 72.0% of the patients in group I and 57.5% in group II. Considering only patients with sclerotic, poorly-vascularised scaphoids, the mean final outcome scores obtained were 7.5 and 6.0 for groups I and group II, respectively. We conclude that vascularised bone grafting yields superior results and is more efficient when there is a sclerotic, poorly-vascularised proximal pole in patients in scaphoid nonunion.
Introduction
Scaphoid nonunion is associated with biomechanical changes and serious functional impairment involving the wrist. Bone union, restoration of scaphoid architecture, relief of pain, and reestablishment of wrist function should be considered the primary goals of treatment. The usual treatment for scaphoid nonunion is conventional bone grafting, with or without bony fixation. Satisfactory bone union rates ranging from 80 to 90% have been reported by some authors [6]; but failure rates as high as 65% have been described by others [1, 9]. Most of these failures have been related to fractures of the proximal pole or avascular necrosis of the proximal fragment. Treating these challenging situations includes the use of vascularised bone grafts, as a more biological solution. Several types of grafting have been developed [10, 14, 23]; and, among these, local vascularised bone grafts near the wrist have gained the greatest popularity.
Since 1991, when Zaidemberg et al. [24] first described a retrograde branch of the radial artery that feeds the distal dorsoradial part of the radius, and in 1995, when Sheetz et al. [18] published detailed descriptions of the vascular anatomy of the radius, several studies using the inter-compartmental supraretinacular artery have demonstrated that satisfactory results can be achieved with this technique [5, 12]. However, other investigators [22] have questioned the efficacy of this approach, reporting low consolidation rates in patients with scaphoid nonunions with avascular necrosis of the proximal pole.
No prospective studies have been reported in which vascularised and non-vascularised grafting techniques, using grafts taken from the dorsal aspect of the distal radius, have been compared directly.
Consequently, the primary objective of our study was to directly compare the clinical and radiographic findings of scaphoid nonunion treated using a vascularised bone graft from the distal radius, as proposed by Zaidemberg et al. [24], versus a conventional non-vascularised bone graft derived from the same region. To do this, we adopted the architecture of a randomised clinical trial, so as to more definitively identify which procedure is best at achieving bone consolidation and re-establishing wrist function in patients with scaphoid nonunion.
Patients and methods
Patient recruitment and evaluation
For this study, we recruited 86 patients with scaphoid nonunion treated by the Hand Surgery Group of the Hospital Nossa Senhora do Pari, in São Paulo, Brazil. Prior to subject recruitment, the study protocol had been submitted to and approved by the hospital’s Committee for Ethics and Research. From July 1998 to December 2004, patients presenting to our service were randomised into one of two groups: group I consisted of 46 patients who underwent surgical repair involving a vascularised bone graft that was harvested from the distal radius, as described by Zaidemberg et al. [24], and group II consisted of 40 patients who received a conventional non-vascularised bone graft, similarly harvested from the distal radius. Informed signed consent was provided by all of the patients prior to their participation in the study. None of the patients had undergone any previous surgical procedure to treat their scaphoid nonunion; and patients otherwise were excluded if they had had either previous ipsilateral surgery or a previous contralateral wrist injury that prevented a valid treated-versus-normal clinical comparison between the two wrists. Randomisation was accomplished by means of sealed envelopes, each one containing the name of one of the procedures; for each patient, one of the envelopes was chosen, and the procedure noted within was adopted for use. All patients were treated by the same senior surgeon (S.R.). They were advised to stop smoking before surgery.
The time interval from the fracture to the surgical procedure to treat nonunion was a mean of 25.3 months in group I patients and 22.5 months in group II patients.
At the time of the first consultation, all patients underwent simple radiographic evaluation of their wrists, using four views (obtained in 90° shoulder abduction, 90° elbow flexion, neutral forearm rotation, and neutral wrist position). The views included posteroanterior with ulnar deviation, profile, lateral, and oblique and were taken four, eight, 12 weeks, six months, one and two years after the procedure. Two hand surgeons and two fellowship-trained, musculoskeletal radiologists evaluated radiographs independently to identify when union had occurred.
We used the Russe classification system [16] to determine the level of nonunion, which also was classified as being in the distal, middle or proximal aspect of the scaphoid. In group I, there were 25 patients (54.3%) with nonunion involving the middle third of their scaphoid and 21 patients (45.7%) with nonunion of the proximal pole. Among group II patients, there were 22 cases (55%) of nonunion involving the middle third, two cases (5%) involving the distal pole, and 16 cases (40%) involving the proximal pole.
To assess any associated carpal instability, we measured the scaphoid-lunate angle. Preoperative measurements of this angle revealed a range from 34° to 80° (mean = 58.3°) among the group I patients and from 40° to 82° (mean = 60.9°) in group II.
Patients were assessed clinically considering the parameters of pain, grip strength and joint mobility. Pain was the main complaint for all 86 patients (100%).
Grip strength was measured in both the affected and unaffected extremities using a Jamar dynamometer (J.P. Marsh, Skokie, IL), before and after treatment. In addition, grip strength on the affected side was expressed as a percentage of grip strength in the contralateral upper limb.
Active range of flexion, extension, radial deviation and ulnar deviation of both the affected and unaffected contralateral wrists were measured, both pre- and postoperatively. All patients were also asked to provide their own global assessment of perceived function, using criteria suggested by Robbins et al. [15] and modified by Steinmann et al. [19]. The sum of these evaluations was a global outcome score, which incorporated the following parameters: pain, functional state (time to return to work), range of motion, and patient global satisfaction. A final score was tabulated as the sum of the scores in the four categories, and this final score was further categorised either as excellent, good, moderate or poor, depending upon the total (see Table 1).
Table 1.
Scaphoid outcome scores
| Description | Score |
|---|---|
| Pain | |
| No pain | 3 |
| Occasional pain, no change in activity, mild discomfort with strenuous use | 2 |
| Moderate pain, tolerable but some limitation in activities | 2 |
| Severe pain, serious limitations in activities | 0 |
| Function | |
| Back to usual work | 3 |
| Back to usual work/sports with mild limitations | 2 |
| Can perform most activities of daily living, but cannot perform high-demand wrist activities | 1 |
| Chronic pain limitation/discomfort | 0 |
| Motiona | |
| Equal to opposite side | 3 |
| Not equal to opposite side, but enough to perform usual activities | 2 |
| Enough motion for daily use, but some limitations in usual activities | 1 |
| Stiff, not enough motion for daily use | 0 |
| Overall satisfaction | |
| Very satisfied with surgical results | 2 |
| Moderately satisfied with surgical results | 1 |
| Not satisfied with surgical results | 0 |
| Maximum score | 11 |
| Results | |
| Excellent | 10 or 11 |
| Good | 9 or 8 |
| Fair | 7 or 6 |
| Poor | ≤ 5 |
a Patient’s perception of motion
Surgical techniques
To access the scaphoid, a curvilinear dorsoradial approach was used, centred over the space between the first and second extensor tunnels. After identifying the focus of the nonunion, the condition of the scaphoid fragments was assessed. The amount of bleeding in the proximal fragment was used to determine the vascular state of the bone, e.g. absence of bleeding was considered to be evidence of a hypovascular segment.
The surgical technique used to harvest a vascularised cortical-cancellous graft from the distal radius (group I) entailed careful dissection and release of the 1–2 supraretinacular inter-compartmental vascular pedicle from its proximal to distal aspect, extending as far as the styloid process of the radius, where the rotation point is located.
The technique used to harvest the conventional non-vascularised graft (group II) was similar, except that the bone graft did not have vascular perfusion. Three converging percutaneous Kirschner wires were used to achieve bone fixation of the scaphoid and graft.
Postoperative evaluation
All patients were immobilised in a plaster cast including the wrist and thumb for four weeks (wrists then were splinted after removal of the plaster cast, at which time patients were encouraged to mobilise their wrists), and all Kirschner wires were removed within ten weeks of operation.
Nonunions were considered healed after radiographic evidence of bone consolidation (bridge trabeculae on both sides of the graft, with attenuation of the continuity solution lines in the scaphoid). When such parameters were not observed, residual nonunion of the scaphoid was considered present.
Statistical analysis
Inter-group mean differences were identified using two-tailed Mann-Whitney U tests for continuous variables and Pearson chi-square analysis for nominal variables, with p = 0.05 used as the threshold for statistical significance.
Results
A statistically greater percentage of patients who received a vascularised graft achieved bony consolidation than did those who received a non-vascularised graft (89.1% versus 72.5%; χ2 = 3.91; p = 0.024). Moreover, they did so over a shorter time interval, i.e. 9.7 versus 12.0 weeks (p < 0.0001) (see Table 2).
Table 2.
Postoperative results
| Group | Consolidation achieved | Mean time to consolidation (weeks) | Scaphoid-lunate angle | Good to excellent functional result | Follow-up (months) |
|---|---|---|---|---|---|
| Group I | 41 (89.1%) | 9.7 | 54.9° | 33 (71.7%) | 24.4 |
| Group II | 29 (72.5%) | 12.0 | 58.9º | 23 (57.5%) | 21.7 |
Outcome based on the patient’s perception of function was measured by the scaphoid score (Table 1). Overall results were excellent in six, good in 27, fair in nine, and poor in four (group I). For group II, results were excellent in seven, good in 16, fair in eight, and poor in nine. A slightly greater percentage of the former versus the latter group achieved a good to excellent result, though this failed to achieve statistical significance (71.7 vs. 57.5% (χ2 = 1.91; p = 0.17).
Considering only patients with scaphoid nonunions and proximal pole fragment, there was bone healing in 19 of 21 (90.5%) patients in group I, but in only 11 of 16 (68.9%) patients in group II (χ2 = 2.79; p = 0.09).
The two groups did not differ significantly in terms of the percentage with a perfused versus a sclerotic/non-perfused proximal scaphoid pole, the percentages being 34.8% and 65.2% in group I, respectively, and both 50% in group 2 (χ2 = 2.02; p = 0.16) (Table 3).
Table 3.
Percentage of patients with a vascularised versus non-vascularised proximal pole
| Group | Bleeding scaphoid | Non-vascularized |
|---|---|---|
| Group I | 16 (34.8%) | 30 (65.2%) |
| Group II | 20 (50%) | 20 (50%) |
Ten of 46 patients in group I were smokers. Six of these patients stopped smoking before surgery and did not resume smoking for the duration of follow-up. Of the four remainders, two achieved union. Eight of 40 in group II were smokers, among whom three stopped smoking. Four failures in this group occurred in smokers who had not quit preoperatively.
Functional results with the two surgical techniques were evaluated, comparing patients in the two groups who had scaphoid nonunions with sclerotic versus well-vascularised fragments (Table 4). The mean functional scores were not statistically different when comparing subjects in the two groups (groups I and II) with scaphoid nonunions and well-vascularised bone fragments (p = 0.98); however, a statistically significant difference was identified between subjects in groups I and II with scaphoid nonunions and non-vascularised proximal pole bone fragments (p = 0.007).
Table 4.
Mean functional scores categorised according to bleeding versus sclerotic scaphoid
| Group | Bleeding scaphoid | Sclerotic scaphoid |
|---|---|---|
| Group I | 7.9 | 7.5 |
| Group II | 8.5 | 6.0 |
Figures 1, 2 and 3 depict the radiographic results obtained in a representative group I patient.
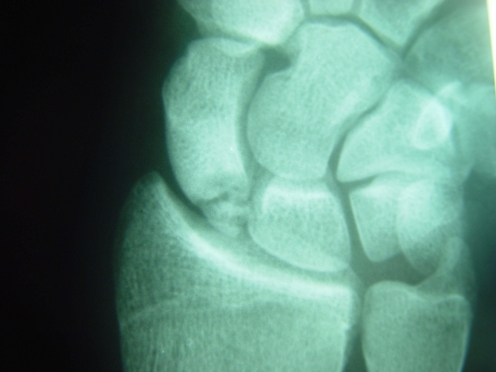
Fig. 1.
Radiography prior to surgery in a patient from group I showing nonunion in an extremely small proximal pole
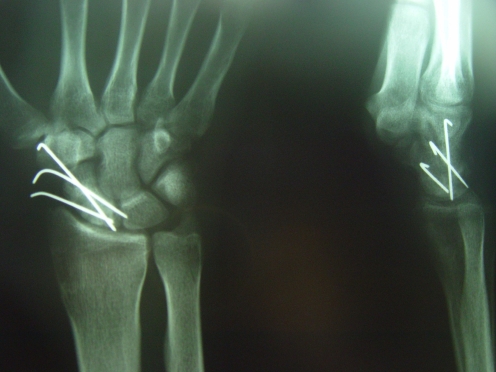
Fig. 2.
Radiography ten weeks after the operation, before removing the wires. a Front view. b Lateral view
Fig. 3.
Radiography 24 months after the surgery
Discussion
Treatment of scaphoid nonunion is still a challenge for hand surgeons, particularly when there is a very small and sclerotic proximal fragment. Success treating scaphoid nonunion is measured in terms of achieving consolidation (bone healing), reestablishing the shape of the scaphoid, making the patient pain free, recovering wrist range of motion, and re-establishing normal biomechanical capabilities of the wrist [17]. When consolidation of the nonunion is not achieved, the results are generally poor, associated with persistent pain, progressive stiffness and degenerative changes.
Among the various surgical options for treatment, we point out the use of bone morphogenetic proteins (BMPs) or osteogenic proteins (OPs) applied to both scaphoid fragments and subsequent autogenous or allogenic bone implants. In one clinical study, Bilic et al. [2] demonstrated that recombinant human OP-1 (BMP-7) results in the radiological and clinical repair of avascular scaphoid and necrotic proximal pole nonunions via increased bone vascularisation and the replacement of pre-existing, proximal pole, sclerotic bone. Vascularised bone grafts initially were developed in an attempt to improve consolidation rates obtained during surgical treatment of scaphoid nonunions. Better consolidation rates and earlier consolidation have since been achieved [24]. On the other hand, many of these studies involved small groups of patients, and no clear information was provided about the vascular status of the scaphoid fragments. A non-vascularised proximal pole should be considered a predictor of poor prognosis. Boyer et al. [3] achieved a consolidation rate of 60% in ten patients with avascular necrosis. In a recent study, Waitayawinyu et al. [22] treated 30 consecutive patients with scaphoid nonunion and proximal pole AVN. The results of this investigation support the use of a vascularised bone graft for the treatment of scaphoid nonunions with avascular necrosis of the proximal pole. Meanwhile, Straw et al. [20] achieved a mere 27% consolidation rate in 16 patients with poles that were considered avascular.
The results of one meta-analysis [13] suggest that vascularised bone grafts are superior to conventional grafts. However, this review analysed and compared patients with different clinical characteristics, including differences in the vascular pattern of fragments, the types and location of scaphoid nonunion, the surgical technique used (access, graft, bone fixation, etc.), and the form and duration of follow-up and rehabilitation.
In this study, we prospectively compared subjects randomly assigned to receive either a vascularised or non-vascularised graft, with all subjects undergoing a surgical procedure that entailed the same surgical access, bone graft and bone fixation technique, and all patients receiving the same follow-up and rehabilitation procedures. Even after randomisation, the patients in our two groups were clinically very similar, the only real difference between them being the type of bone graft used. Our clinical outcomes of interest included a summation score that incorporated pain, functional state, range of motion, and patient global satisfaction. Using this same scoring system, Steinmann et al. [19] achieved a good to excellent functional result in 64% of their patients. Using the same criteria, we achieved a good to excellent functional result in 72% of our patients who had received a vascularised bone graft, but only in 57.4% of those who received a non-vascularised graft.
Tobacco use may be an important determinant of union rates [11]. Dinah and Vickers [7] concluded that smoking is significantly associated with operative treatment failure in patients with established nonunion of the scaphoid bone. Our results suggest an important and potentially avoidable risk factor, but further studies would be required to determine if vascularised grafting is superior. Vascularised bone grafting is a technique that increases the proportion of consolidation in the most severe cases. There is more efficient and faster bone healing in patients with sclerotic scaphoid nonunions who are treated with vascularised bone grafts [21]. In our study, patients who received vascularised grafts achieved bony consolidation within a mean of 9.7 weeks versus 12 weeks with conventional grafting, and 89.1% in the former group achieved consolidation versus 72.5% in the latter, a statistically and clinically significant difference.
Considering only patients with scaphoid nonunions and proximal pole fragment, there was bone healing in 19 of 21 patients in group I (90.5%), but in just 11 of 16 patients in group II (68.9%). We believe that the decisive factor in this very significant difference in the consolidation rates was the association of avascular necrosis with the proximal fragments.
There is controversy regarding the possibility that avascular scaphoids might consolidate regardless of the type of surgery used. Schuind et al. [17] did not observe any significant difference between scaphoid nonunion patients with or without an avascular proximal pole in relation to bone healing. However, their results were based only upon preoperative radiographs. Filan and Herbert [8] found a low correlation between preoperative radiographic findings and intraoperative surgical findings. Magnetic resonance may better indicate the state and pattern of bone vascularisation of the fragments, but it is not infallible [4]. According to Green [9], radiography is not an accurate indicator of the state of scaphoid vascularisation, which is better diagnosed during surgery. During surgical procedures, it is possible to analyse the vascular condition of the fragments. We observed that 30 scaphoids in group I (65.2%) and 20 scaphoids in group II (50%) did not present with bleeding and were sclerotic.
The use of vascularised bone grafting promoted bone healing and a consolidation rate of 83.3% in those scaphoids that did not bleed (sclerotic) and a rate of 100% in those that did bleed. Conversely, the use of a conventional non-vascularised bone graft yielded consolidation rates of 55% in sclerotic scaphoids and 90% in bleeding scaphoids. Radiographic and functional results allow us to conclude that the vascularised graft is superior to the conventional non-vascularised graft. On the other hand, no differences are apparent in patients with scaphoid nonunions and well-vascularised fragments. In these patients, we were unable to conclude that either technique is superior to the other.
In conclusion, we suggest that vascularised bone grafting is mandatory whenever there is a non-vascularised sclerotic fragment. On the other hand, in patients with well-vascularised fragments, either the vascularised or conventional technique can be used, depending upon the surgeon’s experience and preference.
References
- 1.Barton NJ. Experience with scaphoid grafting. J Hand Surg [Br] 1997;22:153–160. doi: 10.1016/s0266-7681(97)80051-4. [DOI] [PubMed] [Google Scholar]
- 2.Bilic R, Simic P, Jelic M, Stern-Padovan R, Dodig D, Meerdervoort HP, Martinovic S, Ivankovic D, Pecina M, Vukicevic S. Osteogenic protein-1 (BMP-7) accelerates healing of scaphoid non-union with proximal pole sclerosis. Int Orthop. 2006;30(2):128–134. doi: 10.1007/s00264-005-0045-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Boyer MI, Schroeder HP, Axelrod TS. Scaphoid nonunion with avascular necrosis of the proximal pole. J Hand Surg [Br] 1998;23:686–690. doi: 10.1016/s0266-7681(98)80029-6. [DOI] [PubMed] [Google Scholar]
- 4.Cerezal L, Abascal F, Canga A, Garcia-Valtuille R, Pinal F. Usefulness of gadolinium-enhanced MR imaging in the evaluation of the vascularity of scaphoid nonunions. Am J Roentgenol. 2000;174:141–149. doi: 10.2214/ajr.174.1.1740141. [DOI] [PubMed] [Google Scholar]
- 5.Chen ACY, Chao EK, Tu YK, Ueng SW. Scaphoid nonunion treated with vascular bone grafts pedicled on the dorsal supra-retinacular artery of the distal radius. J Trauma. 2006;61:1192–1197. doi: 10.1097/01.ta.0000234723.78487.52. [DOI] [PubMed] [Google Scholar]
- 6.Cooney WP, Dobyns JH, Linscheid RL. Nonunion of the scaphoid: analysis of the results from bone grafting. J Hand Surg [Am] 1980;5:343–354. doi: 10.1016/s0363-5023(80)80173-0. [DOI] [PubMed] [Google Scholar]
- 7.Dinah AF, Vickers RH. Smoking increases failure rate of operation for established non-union of the scaphoid bone. Int Orthop. 2007;31(4):503–505. doi: 10.1007/s00264-006-0231-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Filan SL, Herbert TJ. Herbert screw fixation of fixation of scaphoid fractures. J Bone Joint Surg [Br] 1996;78:519–529. [PubMed] [Google Scholar]
- 9.Green DP. The effect of avascular necrosis on Russe bone grafting for scaphoid nonunion. J Hand Surg [Am] 1985;10:597–605. doi: 10.1016/s0363-5023(85)80191-x. [DOI] [PubMed] [Google Scholar]
- 10.Kuhlmann JN, Mimoun M, Boabighi A, Baux S. Vascularized bone graft pedicled on the volar carpal artery for non-union of the scaphoid. J Hand Surg [Br] 1987;12:203–210. doi: 10.1016/0266-7681_87_90014-3. [DOI] [PubMed] [Google Scholar]
- 11.Little CP, Burston BJ, Hopkinson-Woolley J, Burge P. Failure of surgery for scaphoid non-union is associated with smoking. J Bone Joint Surg [Br] 2006;31:252–255. doi: 10.1016/j.jhsb.2005.12.010. [DOI] [PubMed] [Google Scholar]
- 12.Malizos KN, Dailiana ZH, Kirou M, Vragalas V, Xenakis TA, Soucacos PN. Longstanding nonunions of scaphoid fractures with bone loss: successful reconstruction with vascularized bone grafts. J Hand Surg [Br] 2001;26:330–334. doi: 10.1054/jhsb.2001.0570. [DOI] [PubMed] [Google Scholar]
- 13.Merrel GA, Wolfe S, Slade JF. Treatment of scaphoid nonunions: quantitative meta-analysis of the literature. J Hand Surg [Am] 2003;27:685–691. doi: 10.1053/jhsu.2002.34372. [DOI] [PubMed] [Google Scholar]
- 14.Rath S, Leung PC. Vascular anatomy of the pronator quadratus muscle-bone flap. A justification for its use with a distally based blood supply. J Hand Surg [Am] 1990;15:630–636. doi: 10.1016/S0363-5023(09)90027-2. [DOI] [PubMed] [Google Scholar]
- 15.Robbins RR, Ridge O, Carter PR. Iliac crest bone grafting and Herbert screw fixation of nonunions of the scaphoid with avascular proximal poles. J Hand Surg [Am] 1995;20:818–831. doi: 10.1016/S0363-5023(05)80438-1. [DOI] [PubMed] [Google Scholar]
- 16.Russe O. Fracture of the carpal navicular. J Bone Joint Surg Am. 1960;42:759–768. [PubMed] [Google Scholar]
- 17.Schuind F, Haentijens P, Innis FV, Maren CV, Elias MG, Sennwald G. Prognostic factors in the treatment of carpal scaphoid nonunions. J Hand Surg [Am] 1999;24:761–776. doi: 10.1053/jhsu.1999.0761. [DOI] [PubMed] [Google Scholar]
- 18.Sheetz KK, Bishop AT, Berger RA. The arterial blood supply of the distal radius and ulna and its potential use in vascularized pedicled bone grafts. J Hand Surg [Am] 1995;20:902–914. doi: 10.1016/S0363-5023(05)80136-4. [DOI] [PubMed] [Google Scholar]
- 19.Steinmann SP, Bishop AT, Berger RA. Use of the 1,2 intercompartmental supraretinacular artery as a vascularized pedicle bone graft for difficult scaphoid nonunion. J Hand Surg [Am] 2002;27:391–401. doi: 10.1053/jhsu.2002.32077. [DOI] [PubMed] [Google Scholar]
- 20.Straw RG, Davis TRC, Dias JJ. Scaphoid nonunion: treatment with a pedicled vascularized bone graft based on the 1, 2 inter-compartmental supraretinacular branch of the radial artery. J Hand Surg [Br] 2002;27:413–416. doi: 10.1054/jhsb.2002.0808. [DOI] [PubMed] [Google Scholar]
- 21.Sunagawa T, Bishop AT, Muramatsu K. Role of conventional and vascular bone grafts in scaphoid nonunion with avascular necrosis: a canine experimental study. J Hand Surg [Am] 2000;25:849–859. doi: 10.1053/jhsu.2000.8639. [DOI] [PubMed] [Google Scholar]
- 22.Waitayawinyu T, McCallister WV, Katolik LI, Schlenker JD, Trumble TE. Outcome after vascularized bone grafting of scaphoid nonunions with avascular necrosis. J Hand Surg [Am] 2009;34:387–394. doi: 10.1016/j.jhsa.2008.11.023. [DOI] [PubMed] [Google Scholar]
- 23.Yuceturk A, Isiklar ZU, Tuncay C, Tandogan R. Treatment of scaphoid nonunions with a vascularized bone graft based on the first dorsal metacarpal artery. J Hand Surg [Br] 1997;22:425–427. doi: 10.1016/s0266-7681(97)80420-2. [DOI] [PubMed] [Google Scholar]
- 24.Zaidemberg C, Siebert JW, Angrigiani C. A new vascularized bone graft for scaphoid nonunion. J Hand Surg [Am] 1991;16:474–478. doi: 10.1016/0363-5023(91)90017-6. [DOI] [PubMed] [Google Scholar]