Abstract
A live attenuated influenza A/Vietnam/1203/2004 (H5N1) vaccine virus (VN04 ca) has receptor binding specificity to α2,3-linked sialosides (α2,3SAL), and a single dose induces a minimal serum antibody response in mice and ferrets. In contrast, A/Hong Kong/213/2003 (H5N1) vaccine virus (HK03 ca) binds to both α2,6SAL and α2,3SAL and generates a stronger serum antibody response in animals. Among the 9 amino acids that differed between the two H5 HA1 proteins, several HK03-specific residues enabled the VN04 ca virus to bind to both α2,3SAL and α2,6SAL receptors, but only the removal of the 158N glycosylation, together with an S227N change, resulted in more-efficient viral replication in the upper respiratory tract of ferrets and an increased serum antibody response. However, the antibody response was HK03 strain specific and did not significantly cross-neutralize VN04 virus. A second approach was taken to adapt the H5N1 VN04 ca virus in MDCK cells to select HA variants with larger plaque morphology. Although a number of large-plaque-size HA variants with amino acid changes in the HA receptor binding region were identified, none of these mutations affected virus receptor binding preference and immunogenicity. In addition, the known receptor binding site changes, Q226L and G228S, were introduced into the HA protein of the VN04 ca virus. Only in conjunction with the removal of the 158N glycosylation did the virus replicate efficiently in the upper respiratory tract of ferrets and became more immunogenic, yet the response was also HK03 specific. Thus, the mask of the antigenic epitopes by 158N glycosylation at the HA globular head and its α2,3SAL binding preference of VN04 ca virus affect virus antigenicity and replication in the host, resulting in a lower antibody response.
Influenza A viruses have the potential to cause pandemics of various severities. The emergence of new influenza virus strains to which the general population has low or no immunity, such as the 2009 swine-origin influenza A H1N1 viruses, will continue to challenge public health authorities and the scientific community to develop quick and efficient mitigation responses (18). Highly pathogenic avian influenza A (HPAI) H5N1 viruses pose a serious pandemic threat due to their virulence and high mortality in humans, and their increasingly expanding host reservoir and significant ongoing evolution could enhance their human-to-human transmissibility (8). Currently, the case fatality rate of HPAI H5N1 viruses in humans is estimated to be approximately 60% (30).
Although HPAI H5N1 viruses are now endemic in several countries (2), direct transmission of influenza viruses from avian species to humans remains a relatively rare event. The hemagglutinin (HA) protein's affinity for cell surface sialic acid-containing molecules is one of the determinants of influenza A virus host range restriction. Human and avian influenza virus isolates differ in their recognition of host cell receptors; human strains mainly bind α2,3-linked sialosides (α2,6SAL), whereas the avian strains have a high affinity to α2,3SAL (15, 32). The influenza pandemics of the last century have been suggested to result from switching of HA receptor-binding specificity from α2,3SAL to α2,6SAL receptors (6, 26, 31).
The receptor-binding specificity of the HA protein can be influenced by several critical residues. For influenza H3 subtype viruses, substitutions of Q226L and G228S could completely reverse receptor-binding specificity from α2,3SAL to α2,6SAL (4, 21). For the H1 subtype viruses, the E190D and D225G residues switch virus receptor binding specificity from α2,3SAL to α2,6SAL for the 1918 pandemic H1N1 viruses (6, 25). However, based on glycan microarray analysis, the 190E and 225D residues cannot alter the HA binding preference from α2,3SAL to α2,6SAL for H5N1 viruses (26).
Vaccination is considered a preferred approach to prevent influenza-related illness in the community. A pandemic influenza vaccine should stimulate protective immunity in the target population using the smallest amount of antigen possible, thus enabling availability of maximal vaccine doses. The inactivated H5N1 VN04 vaccines have been found to be poorly immunogenic in humans, and adjuvants are needed to enhance vaccine immunogenicity (13). Live attenuated influenza vaccines (LAIV) have several desirable attributes: the stimulation of a durable mucosal and systemic immunity, broad efficacy against homologous and drifted strains, and efficient production (17).
Several H5N1 LAIV vaccines possessing a modified HA and neuraminidase (NA) of an H5N1 virus and the six internal protein gene segments (PB1, PB2, PA, NP, M, and NS) of the A/Ann Arbor/6/60 (H2N2) cold-adapted (AA ca) master donor virus were previously generated and evaluated for their immunogenicity and efficacy in mice and ferrets (29). A single dose of A/Vietnam/1203/2004 (VN04 ca) LAIV elicited very low levels of serum neutralizing antibodies against homologous and heterologous wild-type (wt) H5N1 viruses 4 weeks after administration to mice and ferrets. In contrast, a single dose of A/Hong Kong/213/2003 (H5N1) (HK03 ca) LAIV was more immunogenic (29). A specific amino acid residue at position 227 in the HK03 HA has been reported to be responsible for the greater immunogenicity of HK03 (9). VN04 and HK03 also differ in their receptor binding specificities. The VN04 HA mainly recognizes α2,3SAL, while the HK03 HA recognizes both α2,3SAL and α2,6SAL (7, 14, 22, 36). Sequence alignment of the two H5 HA proteins revealed nine amino acid differences in their HA1 region (9). The current analysis evaluates the impact of these amino acid differences on H5N1 VN ca vaccine strain replication and immunogenicity. In addition, adaptive mutations selected from MDCK passage of the H5N1 VN04 ca virus and introduction of known receptor binding sites were evaluated for their effect on antigenicity and immunogenicity of the H5N1 VN04 ca virus.
MATERIALS AND METHODS
Cells, viruses, and antibodies.
Viral RNA was extracted from the influenza A H5N1 HK03 and VN04 wt viruses in a biosafety level 3-plus (BSL3+) laboratory. MDCK cells were obtained from the American Type Culture Collection (ATCC) and maintained in minimal essential medium (MEM) containing 5% fetal bovine serum (FBS) in a humidified atmosphere of 5% CO2. Polyclonal anti-influenza A/Ann Arbor/6/60 (H2N2) antiserum was produced in chickens. Rabbit anti-HA1 (H5N1) antiserum was obtained from Immune Technology Corp. (New York, NY).
Generation of recombinant viruses.
Recombinant cold-adapted (ca) HK03 and VN04 viruses that contain the cleavage site-modified HA were generated by reverse genetics as described previously (29). To introduce specific change in the HA protein, site-directed mutagenesis of the HK03 and VN04 HA plasmids was performed by using the QuikChange mutagenesis kit (Stratagene, La Jolla, CA). Mutagenized residues were confirmed by sequence analysis. Recombinant 6:2 vaccine viruses with specific changes in the HA gene, the unmodified NA from HK03 or VN04, and the six internal gene segments from the AA ca virus were rescued using the eight-plasmid transfection system (10, 11). Viruses were propagated in allantoic cavities of 10- to 11-day-old embryonated chicken eggs, and the viruses were harvested and stored at −80°C. The genetic sequence of each recombinant virus was confirmed by sequencing cDNA amplified from viral RNA (vRNA) by reverse transcription (RT)-PCR.
Selection of H5N1 VN04 ca variants from MDCK cell adaptation.
The VN04 ca virus was passaged six times in MDCK cells to select variants that exhibited large-plaque morphology. MDCK cells in six-well plates were infected with the VN04 ca virus at a multiplicity of infection (MOI) of 0.01 in triplicate in 3 ml of Opti-MEM I (Invitrogen, Carlsbad, CA) containing 1 μg/ml tosylsulfonyl phenylalanyl chloromethyl ketone (TPCK)-trypsin at 33°C in a CO2 incubator. When the cytopathic effect (CPE) reached 80 to 90% (2 to 4 days postinfection [p.i.]), the culture supernatant was collected, diluted 100- to 1,000-fold, and used to infect fresh MDCK cells. The VN04 ca virus used for the initial passage was referred to as VN04 ca virus P0, and the subsequently passaged viruses were referred to as VN04 ca viruses P1 to P6.
Plaque assay.
Plaque morphology of the passaged VN04 ca P0 to P6 viruses was examined in MDCK cells by plaque assay. MDCK cells in six-well plates were infected with 400 μl of 10-fold serially diluted virus and overlaid with 3 ml of L15/MEM containing 1% agarose and 1 μg/ml TPCK-trypsin. The infected cells were incubated at 33°C for 3 days. Plaques that were at least twice the size of the VN04 ca virus P0 were isolated for sequence analysis and further amplified in MDCK cells or eggs. The plates were then immunostained using polyclonal antiserum against AA ca, and the enumerated plaque images were captured using an AlphaImager system (Alpha Innotech, San Leandro, CA).
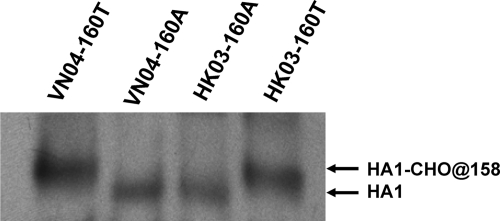
Examination of HA 158N glycosylation by Western blotting.
The VN04 HA has a putative glycosylation site at the N158 residue because of the T160 residue (9). To confirm whether a T-to-A substitution at residue 160 that is present in the HA protein of HK03 affected the 158N glycosylation status of VN04 HA, Western blotting was performed to examine the mobility change of the HA protein on a polyacrylamide gel. Each virus was concentrated by ultracentrifugation, and viral proteins were electrophoresed on a Novex 10% Tris-glycine gel (Invitrogen). The electrophoresed proteins on the gel were transferred to a nitrocellulose membrane, and the membranes were blocked in 5% fat-free milk before incubation with rabbit anti-HA1 (H5N1) antiserum (Immune Technology Corp., New York, NY), followed by incubation with horseradish peroxidase (HRP)-conjugated antirabbit antibodies (Dako, Carpinteria, CA). Protein bands were detected by a chemiluminescence detection kit (GE Healthcare Bio-Sciences, Piscataway, NJ) and developed on an X-ray film.
Receptor-binding assay.
The receptor-binding specificity of the recombinant viruses was determined by comparing the hemagglutination activities using enzymatically modified chicken red blood cells (cRBCs) that express either α2,3SAL or α2,6SAL, as previously described (3, 20). Briefly, 100 μl of 10% cRBCs was incubated with 50 mU Vibrio cholerae neuraminidase (Sigma, St. Louis, MO) at 37°C for 1 h to remove sialic acids from cRBCs. Subsequently, desialylated cRBCs were incubated with 2.5 mU of α2-3(N)-sialyltransferase (Calbiochem, La Jolla, CA) or 2 mU of α2-6(N)-sialyltransferase (Calbiochem, La Jolla, CA) and 1.5 mM cytidine-5′-monophospho-N-acetylneuramine acid (Sigma, St. Louis, MO) for 1.5 h at 37°C. The resialylated red blood cells (RBCs) were suspended (0.5% [vol/vol]) in phosphate-buffered saline (PBS) (pH 7.2 to 7.6) and incubated with 2-fold serially diluted virus at room temperature for 60 min. The viral HA titer was defined as the reciprocal of the highest dilution that displayed hemagglutination of the RBCs.
Ferret studies.
Seven- to ten-week-old ferrets from Simonsen (Gilroy, CA) or Triple F farm (Sayre, PA), testing seronegative for antibodies to influenza A H1N1, H3N2, and H5N1 viruses, were used to examine viral replication in the upper and lower respiratory tract of ferrets and to compare levels of serum antibodies induced by the recombinant viruses. Groups of 3 ferrets were inoculated intranasally with 7.0 log10 PFU of the VN04 ca, HK03 ca, or VN04 ca HA variants in a volume of 0.2 ml (0.1 ml per nostril). Replication of the H5 variants in the upper and lower respiratory tract of ferrets was determined by 50% egg infectious titer and expressed as log10 egg infective dose (EID)/g tissue. H5-specific antibody responses were examined by hemagglutination inhibition (HAI) and microneutralization (Nt) assays using sera collected at day 28 p.i. after a single dose or 14 days after the second dose (42 days p.i.).
Microneutralization assay.
Serum antibody levels of postimmunization ferret sera against the homologous and heterologous viruses were determined by an Nt assay. Sera were treated overnight with receptor-destroying enzyme (RDE) (Denka-Seiken, Tokyo, Japan) at 37°C for 18 h and heat inactivated at 56°C for 45 min. Serial 2-fold dilutions of ferret serum starting from 1:10 dilution were incubated with an equal volume of the indicated viruses at a concentration of 100 50% tissue culture infectious dose (TCID50)/ml in a 96-well U-bottom plate for 60 min at 33°C. The virus-serum mixture was transferred to monolayers of MDCK cells and incubated at 33°C for 6 days. The neutralizing antibody titers were defined as the reciprocal of the highest serum dilution that completely neutralized the appropriate virus as defined by the absence of CPE on day 6 p.i.
RESULTS
Adaptation of the VN04 ca virus in MDCK cell cultures.
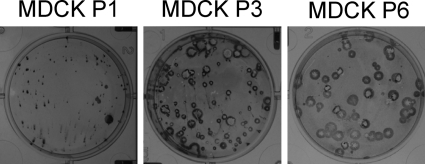
The VN04 strain, which was isolated from an infected person, originated with an avian host and has receptor binding specificity to α2,3SAL. Passage of the VN04 ca virus in MDCK cells selected viruses with large-plaque morphology (Fig. 1). There was a progressive increase in the proportion of plaques that exhibited large-plaque morphology on MDCK cells in later passages, indicating that these viruses with large-plaque phenotype may have acquired an amino acid change(s). Eighteen larger plaques from each passage were selected for sequence analysis to identify amino acid substitutions in the HA and NA genes. As shown in Table 1, the most frequently isolated large-plaque isolates contained sequence changes at or near the HA receptor binding site; no mutations in the NA were detected in any of these virus isolates. Some of the changes occurred as early as passage 1. Several substitution mutations, E190D, T219N, K222E, G225E, and S227N (H3 numbering) (27, 34), were detected in H5 HA at a much higher frequency. The 190D or 225E mutation has been reported to affect receptor specificities of H1 viruses (6, 15, 19, 25). The 227N residue is also present in HA of HK03 and was found to allow the virus to bind α2,6SAL (1, 9, 24). The other changes in HA1 at residues H130N, A138T, Y201C, S203F, K222Q, and N240D were detected at a much lower frequency. In addition to the changes in the HA1 region, two mutations at residues 64 and 82 (H5 numbering) in the HA2 region were also detected. The sequences of the six internal protein gene segments of the VN04 HA variants with mutations at residues 190D, 219N, 222E, 225E, and 227N were also examined. Random mutations with one or two amino acid changes were detected in the PB1, PB2, PA, or NP gene segment. To eliminate any possible effects of the mutations in the internal protein gene segments on virus phenotypes, mutations at positions 190, 219, 222, 225, and 227 were introduced into the VN04 HA plasmid, and recombinant viruses possessing these substitutions were generated and characterized.
FIG. 1.
Plaque morphology of the H5N1 VN04 ca virus passaged in MDCK cells. MDCK cells were infected with the VN04 ca virus at a MOI of 0.01, and virus supernatants collected at passages 1, 3, and 6 were examined by plaque assay in MDCK cells. The viruses in the later passages exhibited large-plaque morphology compared to the viruses in the earlier passage.
TABLE 1.
Amino acid substitutions detected in the HA protein of the VN04 ca variantsa
| aa position no. for H3, H5 | aa substitution |
No. of isolates | Isolated in passage(s): | |
|---|---|---|---|---|
| VN04 | Variant | |||
| 190, 186 | E | D | 6 | 2, 3, 6 |
| 219, 215 | T | N | 4 | 1, 2, 3 |
| 222, 218 | K | E | 5 | 3, 6 |
| 225, 221 | G | E | 5 | 1, 2, 3 |
| 227, 223 | S | N | 4 | 2, 3, 6 |
| 130, 125 | H | N | 1 | 3 |
| 138, 134 | A | T | 1 | 2 |
| 201, 197 | Y | C | 1 | 1 |
| 203, 199 | S | F | 1 | 1 |
| 222, 218 | K | Q | 1 | 2 |
| 240, 236 | N | D | 1 | 2 |
| NA, HA2-64 | E | K | 3 | 2, 3, 6 |
| NA, HA2-82 | K | N | 1 | 2 |
Amino acid (aa) substitutions are indicated by a single-letter amino acid residue at each position, and their positions in H5 numbering and H3 numbering are presented. NA, not applicable.
Generation of the H5N1 VN04 and HK03 ca variants by reverse genetics.
Alignment of the H5 HA protein sequences of HK03 and VN04 revealed 9 amino acid differences in their HA1 region (NCBI accession number BAE07201 or AAT39065 for HK03 HA and AAT73274 or ABP51977 for VN04 HA). Analysis of the three-dimensional (3D) protein structure of the H5 HA protein indicated that 6 amino acid residues (125, 159, 160, 193, 216, and 227, H3 numbering) (27, 34) are located at the antigenic sites of the HA globular domain, and these residues were chosen for further evaluation. The HK03 HA-specific amino acids were introduced individually or in combination into the VN04 HA protein (Table 2). Viruses possessing the introduced mutations in HA of the VN04 ca virus were rescued by reverse genetics. In addition, the Q226L and/or G228S mutation, with or without the T160A change, was also introduced into HA of the VN04 ca virus. None of these amino acid changes (with the HK03 residue, adaptive mutations, or introduced mutations) in the HA protein of VN04 ca virus affected viral growth, since all the viruses replicated well in eggs with titers of ∼8 log10 PFU/ml (Table 2).
TABLE 2.
Comparisons of H5N1 VN04 ca, HK03 ca, and VN04 ca HA variants for their replication in eggs and antigenicity
| Category of VN04 HA mutation | Virus | Titer of virusa (log10 PFU/ml) | Nt titerb |
HAI titerb |
||||
|---|---|---|---|---|---|---|---|---|
| HK03 |
VN04 |
HK03 |
VN04 |
|||||
| 1 dose | 1 dose | 1 dose | 2 dose | 1 dose | 2 dose | |||
| None | HK03 ca | 7.8 | 1280 | 80 | 64 | 256 | <4 | 64 |
| VN04 ca | 8.1 | 40 | 80 | <4 | 16 | <4 | 16 | |
| With HK residue | VN-S125N | 8.0 | 80 | 80 | <4 | 8 | <4 | 16 |
| VN-S159N | 8.1 | 80 | 80 | <4 | 8 | <4 | 16 | |
| VN-T160A | 7.8 | 640 | 80 | 32 | 64 | <4 | 64 | |
| VN-K193R | 8.0 | 160 | 80 | <4 | 8 | <4 | 16 | |
| VN-R216K | 8.1 | 40 | 80 | <4 | 4 | <4 | 16 | |
| VN-S227N | 8.3 | 40 | 80 | 8 | 16 | <4 | 64 | |
| VN-S159N/T160A | 7.3 | 320 | 80 | 16 | 32 | <4 | 32 | |
| VN-T160A/S227N | 8.1 | 640 | 80 | 32 | 64 | <4 | 32 | |
| Adaptive mutations | VN-E190D | 8.2 | 80 | 80 | <4 | 16 | <4 | 64 |
| VN-T219N | 8.3 | 80 | 80 | <4 | 16 | <4 | 32 | |
| VN-K222E | 8.0 | 80 | 80 | <4 | 16 | <4 | 64 | |
| VN-G225E | 8.0 | 80 | 80 | <4 | 16 | <4 | 32 | |
| Introduced mutations | VN-Q226L | 7.7 | 80 | 80 | 32 | 64 | <4 | 128 |
| VN-G228S | 8.1 | 80 | 80 | 8 | 64 | <4 | 128 | |
| VN-Q226L/G228S | 8.4 | 80 | 80 | 16 | 32 | <4 | 128 | |
| VN-Q226L/T160A | 7.7 | 640 | 80 | 64 | 128 | <4 | 128 | |
| VN-Q226L/G228S/T160A | 8.1 | 640 | 80 | 128 | 256 | <4 | 128 | |
Titer of virus was measured by plaque assay on MDCK cells and expressed as mean log10 PFU/ml from two experiments.
Ferrets were immunized with the HK03 ca or VN04 ca virus, serum was collected 4 weeks after a single dose or 2 weeks after the second dose, and sera from three ferrets were pooled for the Nt assay and HAI assay using turkey RBCs. The values represent the highest serum dilution that neutralized the indicated viruses.
Evaluation of antigenicity of VN04 ca variants.
The antigenicity of the VN04 ca variants was compared to those of the VN04 ca and HK03 ca viruses by using postinfection ferret serum collected after intranasal inoculation with a single dose or two doses of 7.0 log10 PFU of either the VN04 ca or HK03 ca virus. Since the VN04 and HK03 ca viruses have different receptor binding preference, which may affect the sensitivity of the HAI assay, an Nt assay was also performed to assess the antigenicity of the H5N1 ca viruses. All of the preimmunized sera had Nt antibody titers of <10. As shown in Table 2, the HK03 ca virus-immunized ferret serum had an Nt titer of 1,280, but it neutralized the VN04 ca virus at a much lower titer of 40; its reactivity with VN04 was reduced by 32-fold. These data are consistent with the previous reported finding that HK03-specific antibody has very narrow reactivity to other H5N1 viruses (29). Although VN04 ca postimmunization ferret serum had a low Nt antibody titer (80) against the homologous virus, it had a similar titer against the HK03 ca virus, confirming that VN04 ca vaccine-induced antibody had broader reactivity than the HK03 ca virus-induced antiserum. The VN04 ca variants reacted similarly to the VN04 ca virus-specific sera. However, their reactivity to the HK03 ca vaccine-induced serum varied. The VN04 ca variants with the 160A residue (VN-T160A, VN-S159N/T160A, VN-T160A/S227N, VN-Q226L/T160A, and VN-Q226L/G228S/T160A) reacted with the HK03 ferret serum much better than the VN04 ca virus and other VN04 ca variants, suggesting that the 160 residue determined strain-specific reactivity. The VN04 ca variants selected from the MDCK cells (adaptive mutations) and the viruses with the introduced Q226L and/or G228S mutation had antigenicity similar to that of the VN04 ca virus as determined by the Nt assay.
Similar to the Nt assay, the HAI assay also showed that the one- and two-dose HK03 ca virus postimmunization ferret sera reacted with the variants that had the T160A mutation better than the VN04 ca virus (Table 2). The HK03 ca virus post-dose-1 and -dose-2 serum had HAI titers of 64 and 256 against the homologous HK03 ca virus and <4 and 16 against the heterologous VN04 ca virus, respectively. However, HAI titers of 16 to 128 (post-dose-1 serum) or 32 to 256 (post-dose-2 serum) were detected for the VN-T160A, VN-S159N/T160A, VN-T160A/S227N, VN-Q226L/T160A, and VN-Q226L/G228S/T160A variants. Similar to the case with the VN04 ca virus, the adaptation mutations did not react with the HK03 1-dose serum and had an HAI titer of 16 with the HK03 ca 2-dose serum. The introduced Q226L and G228S mutations had greater reactivity to the HK03 ca serum in the HAI assay. VN04 ca 1-dose serum had an antibody titer too low to be detected by the HAI assay using turkey RBCs, while the VN04 ca 2-dose serum reacted to the HK03 ca virus at a titer 4-fold higher than that of the homologous VN04 ca virus (64 versus 16) due to the difference in the receptor binding property. The VN04 ca 2-dose serum also reacted with some of the variants better than the VN04 ca virus. The highest titers were detected for the introduced Q226L and/or G228S mutation with or without the T160A mutation. The data obtained by the HAI assay indicated that some of the mutations in the HA molecule may have affected virus receptor binding preference or avidity such that the variants had better binding to the turkey RBCs, resulting in increased sensitivity of the HAI assay.
Receptor-binding preference of the VN04 ca variants.
The VN04 ca variants bearing substitutions in the HA protein, reflecting either the HK03-specific amino acids, adaptive mutations selected from MDCK cells, or the introduced Q226L and G228S changes, were analyzed for their receptor-binding specificities by hemagglutination of the variants with cRBCs resialylated with either α2,3SAL or α2,6SAL. The HA titer of 64 was used for the analyses of the VN04 ca variants. As expected, the HK03 ca virus had binding affinity for both α2,3SAL and α2,6SAL, and the VN04 ca virus displayed a strong binding preference for α2,3SAL (Table 3). The introduction of single amino acids from HK03 HA, S125N, S159N, T160A, K193R, and the double S159N/T160A and T160A/S227N mutations resulted in increased binding to α2,6SAL without a loss of binding to α-2,3SAL. The virus with the single R216K or S227N change did not bind to α2,6SAL. Surprisingly, the VN04 ca variants that had the MDCK adaptive mutations (E190D, T219N, K222E, G225E, and S227N) remained unable to bind to α2,6SAL at the virus concentration tested (Table 3). The Q226L mutation reduced the receptor binding affinity for α2,3SAL without detectable binding to α2,6SAL being shown. However, the G228S mutation allowed the virus to bind to α2,6SAL better, and the double Q226L/228S mutant bound to α2,6SAL and α2,3SAL equally but at a low level (both had a titer of 8). Introduction of the T160A mutation into the Q226L and Q226L/G228S mutants improved virus binding affinity for α2,6SAL. Thus, the mutations introduced into HA of the VN04 ca virus had various impacts on virus receptor binding preferences.
TABLE 3.
Receptor binding specificities of VN04 ca variants
| Virus | Titer of HA using cRBCs with indicated treatmenta |
||
|---|---|---|---|
| Untreated | α2,3SAL | α2,6SAL | |
| HK03 ca | 64 | 64 | 32 |
| VN04 ca | 64 | 64 | 2 |
| VN-S125N | 64 | 64 | 16 |
| VN-S159N | 64 | 128 | 32 |
| VN-T160A | 64 | 64 | 64 |
| VN-K193R | 64 | 64 | 64 |
| VN-R216K | 64 | 64 | 2 |
| VN-S227N | 64 | 64 | <2 |
| VN-S159N/T160A | 64 | 64 | 64 |
| VN-T160A/S227N | 64 | 64 | 32 |
| VN-E190D | 64 | 32 | <2 |
| VN-T219N | 64 | 64 | <2 |
| VN-K222E | 64 | 64 | <2 |
| VN-G225E | 64 | 64 | <2 |
| VN-Q226L | 64 | 8 | <2 |
| VN-G228S | 64 | 64 | 16 |
| VN-Q226L/G228S | 64 | 8 | 8 |
| VN-Q226L/T160A | 64 | 4 | 64 |
| VN-Q226L/G228S/T160A | 64 | 64 | 64 |
Virus that didn't hemagglutinate RBCs was assigned a value of <2.
The 158N residue in the HA protein of the VN04 ca virus is glycosylated.
Posttranslational N-linked glycosylation of the HA protein can influence the virulence and pathogenicity of influenza virus by masking the antigenic epitopes of the HA protein (23), resulting in altered virus receptor binding (16) and modulation of the cleavability of the HA precursor protein (5). The 158N residue was present in both VN04 and HK03 HA, but VN04 has residue 160T, which could make the 158N glycosylated (N-S-T). HK03 has 160A, and its 158N residue thus could not be glycosylated. To confirm that this 158N glycosylation site in the VN04 H5 HA protein was indeed utilized, the H5 HA proteins of the VN04, VN04-160A, HK03 and HK03-160T ca viruses were analyzed by Western blotting using an H5 HA-specific antibody (Fig. 2). As expected, the H5 HA protein of the VN04 ca virus with the 158N-159S-160T sequence in HA1 migrated slower than the VN04 virus with 160A. Similarly, the HA protein of the HK03 ca virus migrated faster than HK03-160T. These data confirmed that the T160A change resulted in the loss of the glycosylation site and the 158N residue in the H5 HA of the VN04 ca virus was indeed glycosylated.
FIG. 2.
Examination of glycosylation of the H5N1 HA proteins by Western blotting. Viruses were amplified in eggs, concentrated by centrifugation, and electrophoresed on 10% polyacrylamide gel containing 0.1% SDS. The HA1 proteins were detected by using polyclonal anti-VN04 antibody. The 158N glycosylated (CHO-HA1) with 160T and nonglycosylated HA1 (HA1) with 160A proteins are indicated.
Replication of the VN04 ca variants in ferrets.
To determine whether the VN04 ca variants with a receptor binding preference for α2,6SAL could replicate more efficiently in vivo, the VN04 ca mutants were evaluated for their replication in the upper and lower respiratory tract of ferrets (Table 4). All of the VN04 ca variants remained attenuated, with no virus replication detected in the lungs of ferrets. The VN04 ca virus replicated in the nasal turbinates (NT) at a very low level (titer of 2.2 log10 50% EID (EID50)/g of tissue), which was about 100-fold lower than replication of the HK03 ca virus. To determine if the NA contributed to virus replication in the respiratory tract, chimeric viruses with the HK03 HA and VN04 NA (HK-HA+VN-NA) or VN04 HA and HK03 NA (VN-HA+HK-NA) were produced. This chimeric HK-HA+VN-NA virus replicated at a mean titer of 3.4 log10 EID50/g, yet its level of replication in the NT varied significantly among the three ferrets, with a standard error (SE) value (0.9) much greater than those of the VN04 (0.1) or HK03 (0.1) ca viruses. The chimeric VN-HA+HK-NA virus replicated similarly to the VN04 virus. These data indicate that HA plays a greater role than NA in determining virus replication in vivo. Most of the VN04 ca variants replicated poorly in the NT. However, VN-T160A/S227N exhibited better replication in the NT, at a titer of 3.4 log10 EID50/g, which was similar to that of the chimeric virus containing the HA from HK03 and NA from VN04 (3.4 log10 EID50/g). Conversely, adding the glycosylation site and making the N227S change in the HA protein of the HK03 ca virus reduced replication of the HK03 ca virus (HK-A160T/N227S) in the NT (2.5 log10 EID50/g). The VN-Q226L/T160A and Q226L/G228S/T160A variants replicated most efficiently in the NT of the ferrets (5.2 and 4.9 log10 EID50/g). Thus, the combination of the removal of the 158N glycosylation (because of the T160A mutation) and an additional receptor binding site mutation enabled the VN04 ca virus to replicate more efficiently in the upper respiratory tract of ferrets.
TABLE 4.
Replication of VN04 ca variants in ferrets
| Virus | Titer of virusa (log10 EID50/g tissue ± SE) |
|
|---|---|---|
| NT | Lung | |
| VN04 ca | 2.2 ± 0.1 | <1.5 |
| HK03 ca | 4.6 ± 0.1 | <1.5 |
| HK-HA+VN-NA | 3.4 ± 0.9 | <1.5 |
| VN-HA+HK-NA | 2.7 ± 0.2 | <1.5 |
| HK-A160T/N227S | 2.5 ± 0.5 | <1.5 |
| VN-T160A | 2.5 ± 0.0 | <1.5 |
| VN-S227N | 2.2 ± 0.2 | <1.5 |
| VN-K193R | 2.2 ± 0.3 | <1.5 |
| VN-T160A/S227N | 3.4 ± 0.6 | <1.5 |
| VN-E190D | 2.0 ± 0.3 | <1.5 |
| VN-T219N | 2.1 ± 0.5 | <1.5 |
| VN-K222E | 2.2 ± 0.1 | <1.5 |
| VN-G225E | 2.0 ± 0.3 | <1.5 |
| VN-Q226L | 2.1 ± 0.1 | <1.5 |
| VN-G228S | 2.2 ± 0.2 | <1.5 |
| VN-Q226L/G228S | 2.1 ± 0.1 | <1.5 |
| VN-Q226L/T160A | 5.2 ± 0.6 | <1.5 |
| VN-Q226L/G228S/T160A | 4.9 ± 0.3 | <1.5 |
Ferrets in groups of three were inoculated intranasally with indicated virus at a dose of 7.0 log10 PFU. Three days postinfection, the virus titer in the NT and lung tissues was determined by measuring the 50% egg infectious titer (log10 EID50/g tissue ± SE).
Immunogenicities of VN04 ca variants in ferrets.
To evaluate whether the specific amino acid changes in HA of the VN04 ca virus would affect the ability of the VN04 ca virus to induce serum antibody responses, groups of three ferrets were vaccinated intranasally with 107 PFU of different VN04 ca variants, and serum neutralizing and HAI antibody titers against the HK03 ca, VN04 ca, and VN04 ca variants were determined (Table 5). There was a relatively good correlation in the Nt and HAI antibody titers. The geometric mean Nt antibody titer of the VN04 ca virus postimmunization serum was much lower than that of the HK03 ca postimmunization serum. All the VN04 ca variants with the MDCK adaptation mutations and the introduced Q226L and/or G228S mutation had antibody responses similar to that for the VN04 ca virus (data not shown). As shown in Table 5, only the VN04 ca variants with the 160A mutation in combination with the S227N, Q226L, or Q226L/G228S changes, VN-T160A/S227N, VN-Q226L/T160A, and VN-Q226L/G228S/T160A, were associated with higher antibody titers against the homologous virus than the VN04 ca virus. Thus, the antibody titers correlated well with the viral replication level in the upper respiratory tract of ferrets. Although the homologous Nt antibody titers of VN-T160A/S227N (508), VN-Q226L/T160A (806), and VN-Q226L/G228S/T160A (1,016) were approaching that of the HK03 ca virus (1,280) and reacted well with the HA variants, they did not react well with the VN04 ca virus. Thus, the enhanced immunogenicity imparted by the T160A mutation in combination with the S227N, Q226L, or Q226L/G228S mutations to the VN04 ca virus was HK03 strain specific and did not extend to cross-reaction with the VN04 ca virus.
TABLE 5.
Immunogenicity of VN04 ca variants in ferrets
| Virus | GMT of serum Nt (HAI) antibody of ferrets immunized with indicated virusa |
|||||
|---|---|---|---|---|---|---|
| HK03 | VN04 | VN-T160A | VN-Q160A/S227N | VN-Q226L/T160A | VN-Q226L/G228S/T160A | |
| HK03 ca | 1280 (256) | 63 (6) | 63 (8) | 254 (25) | 320 (40) | 640 (102) |
| VN04 ca | 32 (<4) | 63 (<4) | 50 (<4) | 101 (<4) | 40 (<4) | 50 (5) |
| VN-T160A | 640 (64) | 63 (<4) | 80 (<4) | 320 (10) | 254 (40) | 508 (64) |
| VN-T160A/S227N | 640 (64) | 160 (13) | 127 (13) | 508 (25) | 254 (40) | 806 (81) |
| VN-Q226L/T160A | 806 (102) | 50 (10) | 127 (10) | 202 (32) | 806 (40) | 806 (128) |
| VN-Q226L/G228S/T160A | 806 (256) | 50 (25) | 50 (20) | 160 (51) | 640 (64) | 1016 (256) |
Ferrets were immunized with the indicated virus, and serum was collected 21 days later for microneutralization assay on MDCK cells and HAI assay using turkey RBCs. Values represent reciprocal geometric mean antibody titers (GMT) from three animals. The homologous titers are boldfaced and underlined.
DISCUSSION
In order to understand and improve the immunogenicity of the H5N1 VN04 ca vaccine, several approaches were explored in this study: identification of the adaptive mutations in the VN04 HA protein after serial passages in MDCK cells, evaluation of amino acid substitutions from the naturally immunogenic HK03 virus strain introduced into the VN04 HA protein, and introduction of the Q226L and/or G228S mutation identified in influenza A H2/H3 viruses (4, 21). Although a number of adaptive mutations were identified in the HA protein of the VN04 ca virus, none of these mutations affected the virus receptor binding preference or improved virus replication in ferrets. The introduction of the HK03 HA-specific mutations into the HA protein of the VN04 ca virus produced variants that had enhanced immunogenicity; however, the antibody response was HK03 strain specific. Introduction of the Q226L and G228S mutations resulted in better binding to α2,6SAL but had no impact on virus replication in the host and virus immunogenicity unless 158N was not glycosylated. Our data strongly suggest that the low antibody response to the VN04 ca virus in ferrets is due to its poor replication in the upper respiratory tract because of 158N glycosylation that masks antigenic epitopes and the virus receptor binding specificity to the α2,3SAL receptor that restricts virus replication.
The amino acid differences in the HA protein between the VN04 and HK03 ca viruses determined virus antigenicity and immunogenicity. Among the 9 amino acids that differed between these two H5N1 viruses, four amino acid changes, at residues 125, 159, 160, and 193, individually resulted in increased binding to α2,6SAL. Recent avian H5N1 viruses (in clade 2.2) that are characterized by the loss of the glycosylation at residue 158N and the acquisition of the 193R residue exhibit an increased propensity for acquiring human receptor specificity (24, 33). These features are also found in the HK03 strain, conferring binding to both types of receptor. Our studies showed that the removal of 158N glycosylation through the T160A mutation or the K193R change in the H5 HA of the VN04 ca virus allowed the virus to bind to α2,6SAL receptors. The T160A or K193R change alone was not sufficient to improve virus replication in vivo; introduction of the S227N change was needed to increase VN04-T160A virus replication in the upper respiratory tract of ferrets. Although the VN04 ca virus with the T160A and S227N changes replicated at a level approximately 10-fold lower than that of the HK03 ca virus, this level of replication was similar to that of the chimeric virus with the HA protein from HK03 and the NA protein from VN04. The NA protein of VN04 has a 20-amino-acid deletion in the stalk region, which may also contribute to virus replication in vivo. Thus, the VN04 HA protein with the T160A and S227N changes is very similar to the HA protein of HK03 in its dual receptor binding specificity and the ability to replicate in ferrets and to induce immune responses. The removal of 158N glycosylation and the S227N change in the HA protein of the VN04 wt virus were previously reported to correlate with reduced pathogenicity in mice (35). Interestingly, the removal of 158N glycosylation from the HA protein with the Q226L or Q226L/G228S mutations enabled the virus to replicate as efficiently as the HK03 ca virus in the upper respiratory tract of ferrets, resulting in a higher level of serum antibody titer. It is not entirely unexpected that the increased antibody titers conferred by the T160A, T160A/S227N, Q226L, or Q226L/G228S mutations to the VN04 ca vaccine virus remained highly strain specific, because these residues are located at the receptor binding and antigenic site of the HA protein (27). Our data indicate that it might be difficult to find a single H5N1 vaccine virus that could offer broad protection against antigenically diverse H5N1 strains in different clades.
Our receptor binding data with use of sialic acid-specific RBCs to hemagglutinate influenza viruses are consistent with previous glycan microarray and cell binding assay results (1, 3, 25, 27). Although a number of mutations introduced into the HA protein of VN04 did not improve virus binding to α2,6SAL, these mutations are associated with a greater sensitivity in detecting serum HAI antibodies by adjusting receptor binding avidity, as was also reported for the S227N mutation (9). In addition to the S227N change, the T160A, MDCK adaptation changes (E190D, T219N, K222E, and G225E) and the introduced Q226L and G228S mutations were associated with increased sensitivity in the HAI assay using sera from ferrets that had received 2 doses of VN04 ca. Surprisingly, with the exception of S227N, which is also present in the HA protein of HK03, the adaptive mutations selected from MDCK cells did not change the receptor binding specificity of the VN04 ca virus. Residues 190 and 225 have been found to affect virus receptor binding specificity for the H1N1 viruses, including the 1918 and 2009 H1N1 pandemic viruses (3, 6, 27). We also tried to evaluate effects of the 190D and 225E double mutations on virus phenotype. However, the recombinant virus with the introduced 190D and 225E readily mutated at either of the residues. Thus, the impact of the 190 and 225 residues on the H5N1 virus is different from that for the H1N1 viruses. Using the glycan microarray method, Stevens et al. also showed that the recombinant HA protein of VN04 with the 190D and 225D residues retained its binding specificity to α2,3-SAL (27). The fact that the VN04 ca virus had a high tendency to mutate at residues 190, 219, 222, 225, and 227 during replication in MDCK cells indicates that these changes may affect HA receptor binding affinity or the interaction/balance between the HA and NA proteins. These changes are beneficial for the virus to enter or be released from the infected cells and allow the VN04 ca virus to replicate more efficiently. The changes may have impacted the HA protein binding avidity for the cell surface receptor, since Hensley et al. (8a) recently demonstrated that single amino acid substitutions in the globular head of the HA protein significantly affected receptor binding avidity for cell surface glycans.
Recent phase I clinical trials of the H5N1 VN04 and HK03 ca vaccines revealed that these vaccines were highly restricted in replication and induced low serum antibody responses in healthy adult vaccine recipients (12). Thus, even the HK03 ca virus with binding to the human-like receptor did not appear to replicate productively in humans, suggesting that other factors play a role in restricting the replication of the H5N1 virus in the upper respiratory tract of humans. This finding is also supported by the fact that HK03 is not adapted for human-to-human transmission. Modification of the H5 HA protein in the H5N1 VN04 ca virus by the removal of the multibasic cleavage site has been shown to restrict viral replication and contribute significantly to the reduced immunogenicity and efficacy of the vaccine virus in mice (28), suggesting that the multibasic amino acids in the HA1-HA2 cleavage site are favorable for vaccine virus replication. The precise immunologic mechanisms by which LAIV induces protective immunity are not well understood; however, responses include mucosal antibody and cellular responses in addition to systemic antibody responses. We have noted previously that even in the absence of detectable serum neutralizing antibodies, the VN04 ca virus-immunized mice were protected from lethal challenge with homologous and heterologous H5N1 wt viruses, indicating that the neutralizing antibody titer may not be a good predictor of protection and that other immune mechanisms may be involved in mediating protective immunity. The antibody titer induced by the VN04 ca virus in ferrets in this study appeared to be higher than that in our previous study (29). Although the antibody titer induced by one dose of the VN04 ca virus could not be detected by HAI, two doses of the VN04 ca virus vaccination induced an antibody titer that was detectable by HAI and a significantly higher Nt antibody titer. These data suggested that 2 doses of the VN04 ca vaccine may be required for optimal protection. More work is needed to understand the protective immune responses induced by H5N1 LAIV and to correlate the preclinical studies of animals with the clinical studies of humans. Because of the inherent properties of the HA protein of the H5N1 VN04 ca vaccine, it may be very difficult to find an H5N1 LAIV that confers broad cross-protective immunity to diverse H5N1 viruses using systemic antibody responses as standards for predicting vaccine efficacy. Our data indicate that the improvement of the VN04 ca vaccine-induced immune responses requires not only the removal of the 158N glycosylation but also the binding to the human-like receptor. Since the recent H5N1 viruses in clade 2.2 have evolved to have receptor binding specificity to α2,6SAL due to the loss of glycosylation at residue 158 and the acquisition of the 193R residue (24), vaccine strains for use against these recent H5N1 viruses should also be evaluated to further understand the roles contributed by 158N glycosylation and HA receptor binding specificity in virus immunogenicity.
Acknowledgments
We thank Scott Jacobson, Kim Ngo, Stephanie Gee, Brett Pickell, Nick Nguyen, and other staff in the animal care facility for helping with the ferret studies, Winnie Chan and Celia Santos for excellent technical assistance, Chin-Fen Yang and Dan Ye for sequencing analyses of adaptive mutations, Daniel Perez of the University of Maryland for providing the protocol for resialylation of cRBCs and α2-6(N)-sialyltransferase, Yang He and Lilly Yang for providing tissue culture cells, members of Hong Jin's group for discussions and assistance, and Chris Ambrose, Glenn Byrd, and Gary Van Nest for critical reviews of the manuscript.
This work was supported in part by the Intramural Research Program of NIAID, NIH.
Footnotes
Published ahead of print on 28 April 2010.
REFERENCES
- 1.Ayora-Talavera, G., H. Shelton, M. A. Scull, J. Ren, I. M. Jones, R. J. Pickles, and W. S. Barclay. 2009. Mutations in H5N1 influenza virus hemagglutinin that confer binding to human tracheal airway epithelium. PLoS One 4:e7836. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Chen, H., G. J. Smith, K. S. Li, J. Wang, X. H. Fan, J. M. Rayner, D. Vijaykrishna, J. X. Zhang, L. J. Zhang, C. T. Guo, C. L. Cheung, K. M. Xu, L. Duan, K. Huang, K. Qin, Y. H. Leung, W. L. Wu, H. R. Lu, Y. Chen, N. S. Xia, T. S. Naipospos, K. Y. Yuen, S. S. Hassan, S. Bahri, T. D. Nguyen, R. G. Webster, J. S. Peiris, and Y. Guan. 2006. Establishment of multiple sublineages of H5N1 influenza virus in Asia: implications for pandemic control. Proc. Natl. Acad. Sci. U. S. A. 103:2845-2850. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Chen, Z., W. Wang, H. Zhou, A. L. Suguitan, Jr., C. Shambaugh, L. Kim, J. Zhao, G. Kemble, and H. Jin. 2010. Generation of live attenuated novel influenza A/California/7/09 (H1N1) vaccines with high yield in embryonated chicken eggs. J. Virol. 84:44-51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Connor, R. J., Y. Kawaoka, R. G. Webster, and J. C. Paulson. 1994. Receptor specificity in human, avian, and equine H2 and H3 influenza virus isolates. Virology 205:17-23. [DOI] [PubMed] [Google Scholar]
- 5.Deshpande, K. L., V. A. Fried, M. Ando, and R. G. Webster. 1987. Glycosylation affects cleavage of an H5N2 influenza virus hemagglutinin and regulates virulence. Proc. Natl. Acad. Sci. U. S. A. 84:36-40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Glaser, L., J. Stevens, D. Zamarin, I. A. Wilson, A. Garcia-Sastre, T. M. Tumpey, C. F. Basler, J. K. Taubenberger, and P. Palese. 2005. A single amino acid substitution in 1918 influenza virus hemagglutinin changes receptor binding specificity. J. Virol. 79:11533-11536. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Govorkova, E. A., J. E. Rehg, S. Krauss, H. L. Yen, Y. Guan, M. Peiris, T. D. Nguyen, T. H. Hanh, P. Puthavathana, H. T. Long, C. Buranathai, W. Lim, R. G. Webster, and E. Hoffmann. 2005. Lethality to ferrets of H5N1 influenza viruses isolated from humans and poultry in 2004. J. Virol. 79:2191-2198. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Haque, A., D. Hober, and L. H. Kasper. 2007. Confronting potential influenza A (H5N1) pandemic with better vaccines. Emerg. Infect. Dis. 13:1512-1518. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8a.Hensley, S. E., S. R. Das, A. L. Bailey, L. M. Schmidt, H. D. Hickman, A. Jayaraman, K. Viswanathan, R. Raman, R. Sasisekharan, J. R. Bennink, and J. W. Yewdell. 2009. Hemagglutinin receptor binding avidity drives influenza A virus antigenic drift. Science 326:734-736. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Hoffmann, E., A. S. Lipatov, R. J. Webby, E. A. Govorkova, and R. G. Webster. 2005. Role of specific hemagglutinin amino acids in the immunogenicity and protection of H5N1 influenza virus vaccines. Proc. Natl. Acad. Sci. U. S. A. 102:12915-12920. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Hoffmann, E., G. Neumann, Y. Kawaoka, G. Hobom, and R. G. Webster. 2000. A DNA transfection system for generation of influenza A virus from eight plasmids. Proc. Natl. Acad. Sci. U. S. A. 97:6108-6113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Jin, H., B. Lu, H. Zhou, C. Ma, J. Zhao, C. F. Yang, G. Kemble, and H. Greenberg. 2003. Multiple amino acid residues confer temperature sensitivity to human influenza virus vaccine strains (FluMist) derived from cold-adapted A/Ann Arbor/6/60. Virology 306:18-24. [DOI] [PubMed] [Google Scholar]
- 12.Karron, R. A., K. Callahan, C. Luke, B. Thumar, J. McAuliffe, E. Schappell, T. Joseph, K. Coelingh, H. Jin, G. Kemble, B. R. Murphy, and K. Subbarao. 2009. A live attenuated H9N2 influenza vaccine is well tolerated and immunogenic in healthy adults. J. Infect. Dis. 199:711-716. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Leroux-Roels, I., A. Borkowski, T. Vanwolleghem, M. Drame, F. Clement, E. Hons, J. M. Devaster, and G. Leroux-Roels. 2007. Antigen sparing and cross-reactive immunity with an adjuvanted rH5N1 prototype pandemic influenza vaccine: a randomised controlled trial. Lancet 370:580-589. [DOI] [PubMed] [Google Scholar]
- 14.Maines, T. R., X. H. Lu, S. M. Erb, L. Edwards, J. Guarner, P. W. Greer, D. C. Nguyen, K. J. Szretter, L. M. Chen, P. Thawatsupha, M. Chittaganpitch, S. Waicharoen, D. T. Nguyen, T. Nguyen, H. H. Nguyen, J. H. Kim, L. T. Hoang, C. Kang, L. S. Phuong, W. Lim, S. Zaki, R. O. Donis, N. J. Cox, J. M. Katz, and T. M. Tumpey. 2005. Avian influenza (H5N1) viruses isolated from humans in Asia in 2004 exhibit increased virulence in mammals. J. Virol. 79:11788-11800. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Matrosovich, M., A. Tuzikov, N. Bovin, A. Gambaryan, A. Klimov, M. R. Castrucci, I. Donatelli, and Y. Kawaoka. 2000. Early alterations of the receptor-binding properties of H1, H2, and H3 avian influenza virus hemagglutinins after their introduction into mammals. J. Virol. 74:8502-8512. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Matrosovich, M., N. Zhou, Y. Kawaoka, and R. Webster. 1999. The surface glycoproteins of H5 influenza viruses isolated from humans, chickens, and wild aquatic birds have distinguishable properties. J. Virol. 73:1146-1155. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Murphy, B. R., and K. Coelingh. 2002. Principles underlying the development and use of live attenuated cold-adapted influenza A and B virus vaccines. Viral Immunol. 15:295-323. [DOI] [PubMed] [Google Scholar]
- 18.Neumann, G., T. Noda, and Y. Kawaoka. 2009. Emergence and pandemic potential of swine-origin H1N1 influenza virus. Nature 459:931-939. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Nobusawa, E., H. Ishihara, T. Morishita, K. Sato, and K. Nakajima. 2000. Change in receptor-binding specificity of recent human influenza A viruses (H3N2): a single amino acid change in hemagglutinin altered its recognition of sialyloligosaccharides. Virology 278:587-596. [DOI] [PubMed] [Google Scholar]
- 20.Paulson, J. C., and G. N. Rogers. 1987. Resialylated erythrocytes for assessment of the specificity of sialyloligosaccharide binding proteins. Methods Enzymol. 138:162-168. [DOI] [PubMed] [Google Scholar]
- 21.Rogers, G. N., J. C. Paulson, R. S. Daniels, J. J. Skehel, I. A. Wilson, and D. C. Wiley. 1983. Single amino acid substitutions in influenza haemagglutinin change receptor binding specificity. Nature 304:76-78. [DOI] [PubMed] [Google Scholar]
- 22.Shinya, K., M. Hatta, S. Yamada, A. Takada, S. Watanabe, P. Halfmann, T. Horimoto, G. Neumann, J. H. Kim, W. Lim, Y. Guan, M. Peiris, M. Kiso, T. Suzuki, Y. Suzuki, and Y. Kawaoka. 2005. Characterization of a human H5N1 influenza A virus isolated in 2003. J. Virol. 79:9926-9932. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Skehel, J. J., D. J. Stevens, R. S. Daniels, A. R. Douglas, M. Knossow, I. A. Wilson, and D. C. Wiley. 1984. A carbohydrate side chain on hemagglutinins of Hong Kong influenza viruses inhibits recognition by a monoclonal antibody. Proc. Natl. Acad. Sci. U. S. A. 81:1779-1783. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Stevens, J., O. Blixt, L. M. Chen, R. O. Donis, J. C. Paulson, and I. A. Wilson. 2008. Recent avian H5N1 viruses exhibit increased propensity for acquiring human receptor specificity. J. Mol. Biol. 381:1382-1394. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Stevens, J., O. Blixt, L. Glaser, J. K. Taubenberger, P. Palese, J. C. Paulson, and I. A. Wilson. 2006. Glycan microarray analysis of the hemagglutinins from modern and pandemic influenza viruses reveals different receptor specificities. J. Mol. Biol. 355:1143-1155. [DOI] [PubMed] [Google Scholar]
- 26.Stevens, J., O. Blixt, J. C. Paulson, and I. A. Wilson. 2006. Glycan microarray technologies: tools to survey host specificity of influenza viruses. Nat. Rev. Microbiol. 4:857-864. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Stevens, J., O. Blixt, T. M. Tumpey, J. K. Taubenberger, J. C. Paulson, and I. A. Wilson. 2006. Structure and receptor specificity of the hemagglutinin from an H5N1 influenza virus. Science 312:404-410. [DOI] [PubMed] [Google Scholar]
- 28.Suguitan, A. L., Jr., M. P. Marino, P. D. Desai, L. M. Chen, Y. Matsuoka, R. O. Donis, H. Jin, D. E. Swayne, G. Kemble, and K. Subbarao. 2009. The influence of the multi-basic cleavage site of the H5 hemagglutinin on the attenuation, immunogenicity and efficacy of a live attenuated influenza A H5N1 cold-adapted vaccine virus. Virology 395:280-288. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Suguitan, A. L., Jr., J. McAuliffe, K. L. Mills, H. Jin, G. Duke, B. Lu, C. J. Luke, B. Murphy, D. E. Swayne, G. Kemble, and K. Subbarao. 2006. Live, attenuated influenza A H5N1 candidate vaccines provide broad cross-protection in mice and ferrets. PLoS Med. 3:e360. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Thanh, T. T., H. R. van Doorn, and M. D. de Jong. 2008. Human H5N1 influenza: current insight into pathogenesis. Int. J. Biochem. Cell Biol. 40:2671-2674. [DOI] [PubMed] [Google Scholar]
- 31.Tumpey, T. M., C. F. Basler, P. V. Aguilar, H. Zeng, A. Solorzano, D. E. Swayne, N. J. Cox, J. M. Katz, J. K. Taubenberger, P. Palese, and A. Garcia-Sastre. 2005. Characterization of the reconstructed 1918 Spanish influenza pandemic virus. Science 310:77-80. [DOI] [PubMed] [Google Scholar]
- 32.Vines, A., K. Wells, M. Matrosovich, M. R. Castrucci, T. Ito, and Y. Kawaoka. 1998. The role of influenza A virus hemagglutinin residues 226 and 228 in receptor specificity and host range restriction. J. Virol. 72:7626-7631. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Wei, C. J., L. Xu, W. P. Kong, W. Shi, K. Canis, J. Stevens, Z. Y. Yang, A. Dell, S. M. Haslam, I. A. Wilson, and G. J. Nabel. 2008. Comparative efficacy of neutralizing antibodies elicited by recombinant hemagglutinin proteins from avian H5N1 influenza virus. J. Virol. 82:6200-6208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Weis, W. I., A. T. Brunger, J. J. Skehel, and D. C. Wiley. 1990. Refinement of the influenza virus hemagglutinin by simulated annealing. J. Mol. Biol. 212:737-761. [DOI] [PubMed] [Google Scholar]
- 35.Yen, H. L., J. R. Aldridge, A. C. Boon, N. A. Ilyushina, R. Salomon, D. J. Hulse-Post, H. Marjuki, J. Franks, D. A. Boltz, D. Bush, A. S. Lipatov, R. J. Webby, J. E. Rehg, and R. G. Webster. 2009. Changes in H5N1 influenza virus hemagglutinin receptor binding domain affect systemic spread. Proc. Natl. Acad. Sci. U. S. A. 106:286-291. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Yen, H. L., A. S. Lipatov, N. A. Ilyushina, E. A. Govorkova, J. Franks, N. Yilmaz, A. Douglas, A. Hay, S. Krauss, J. E. Rehg, E. Hoffmann, and R. G. Webster. 2007. Inefficient transmission of H5N1 influenza viruses in a ferret contact model. J. Virol. 81:6890-6898. [DOI] [PMC free article] [PubMed] [Google Scholar]