Abstract
Objective. To describe working status in patients with RA, AS and PsA treated with anti-TNF therapy registered with the British Society for Rheumatology Biologics Register.
Methods. Patients with RA (n = 3291), AS (n = 229) and PsA (n = 254) treated with anti-TNF therapy were included in this study. In addition, biologic-naive patients with RA (n = 379) were included. At baseline and 3 years after registration, all patients reported their working status. Baseline characteristics between working and work-disabled patients were compared. Logistic regression analysis was applied to identify factors associated with new work disability in patients with RA.
Results. At baseline, work disability rates were already high: 49% for RA, 39% for PsA, 41% for AS and 36% for biologic-naive patients. Work-disabled patients had a higher HAQ score and worse disease activity than working patients. Working patients with a high HAQ score [odds ratio (OR) 2.79; 95% CI 1.89, 4.12] and a manual job (OR 2.31; 95% CI 1.52, 3.52) at baseline were more likely to become work disabled at follow-up, while those patients in remission 6 months after commencing anti-TNF therapy were less likely to become work disabled. However, use of anti-TNF therapy did not prevent patients with RA from becoming work disabled (OR for RA control patients vs RA anti-TNF patients 0.80; 95% CI 0.36, 1.81, adjusted for baseline variables).
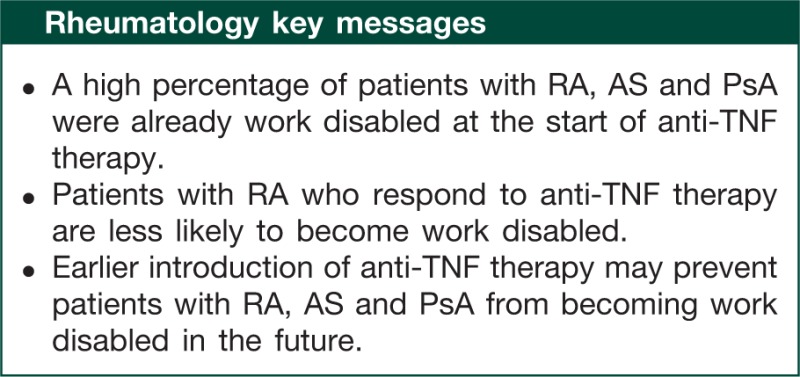
Conclusion. A high percentage of patients with RA, AS and PsA were already work disabled at the start of anti-TNF therapy. There is less future work disability in working patients with RA who responded to anti-TNF therapy.
Keywords: Rheumatoid arthritis, Ankylosing spondylitis, Psoriatic arthritis, Work disability, Anti-TNF therapy
Introduction
Work disability is one of the major economic consequences among patients with chronic inflammatory diseases such as RA, AS and PsA. In an overview of cross-sectional studies including patients with a diagnosis of RA, work disability rates ranged from 13% after a mean disease duration of 6 months to 67% after an average disease duration of 15 years [1]. In an overview among patients with AS, work disability rates were somewhat lower and ranged from 3% after 8 years to 50% after 45 years of disease [2]. Less is known about work disability as a consequence of PsA. The employment rate in patients with PsA is significantly lower than that seen in the general population, but higher than in the RA population and slightly lower than in the AS population [3]. In the studies included in these reviews, patients with RA and AS were treated with conventional DMARDs, whereas treatment of patients with AS mainly consisted of treatment with NSAIDs and physical therapy. During the past decade, a number of anti-TNF therapies have been introduced for the treatment of RA, AS and PsA. Treatment with anti-TNF agents has proved clinically effective in all three patient populations [4–10], but there are few and conflicting data available on the effect of anti-TNF agents on working status [11–17].
Since 2001, rheumatologists in the UK have been submitting clinical and demographic data to a national register [The British Society for Rheumatology Biologics Register (BSRBR)]. The primary aim of this register is to monitor the long-term safety of anti-TNF therapies [18, 19]. Using data from patients enrolled in this register, in this study we set out to compare baseline characteristics between those working and those who were classified as work disabled at the time of enrolment with the register and to describe the change in working status over 3 years among patients with RA, PsA and AS. Additionally, within the anti-TNF-treated RA cohort, we aimed to identify factors measured at baseline or within the first 6 months of anti-TNF therapy, which predicted new work disability. Finally, we compared the rates of new work disability between a group of patients with RA receiving anti-TNF therapy and a biologic-treatment-naïve group receiving standard DMARD therapy.
Patients and methods
Anti-TNF cohort
Consecutive patients with RA, PsA and AS registered with the BSRBR between 1 October 2001 and 31 December 2005 were included in this study. Patients had recently (within 6 months) started infliximab, etanercept or adalimumab at enrolment in the register. In the UK, anti-TNF therapy may be prescribed to patients with active RA {28-joint disease activity score (DAS-28) >5.1; [20]} despite previous therapy with at least two conventional DMARDs, one of which should be MTX [21]. For AS and PsA, no national guidelines were published until 2004. These guidelines now recommend that patients with AS are eligible for anti-TNF therapy if they have failed conventional treatment (i.e. >2 NSAIDs) and if they have active disease [Bath AS Disease Activity Index (BASDAI) >4 units and visual analogue scale (VAS) spinal pain >4 cm in the last week] on two occasions at least 4 weeks apart without any change of treatment. Anti-TNF therapy may be given to patients with PsA who fail two DMARDs and have active disease, defined as ≥3 tender and ≥3 swollen joints.
RA control cohort
In addition to the anti-TNF cohort, the BSRBR is recruiting a parallel cohort of biologic-naïve patients with active RA. Control patients were recruited from 20 hospitals across the UK if they had RA, were receiving a DMARD, had no history of exposure to biologic therapies and were felt to have active disease (a guide DAS-28 of at least 4.2 was recommended although patients may have had lesser disease activity). Data collection was identical to that of the anti-TNF cohort with the exception of the HAQ at baseline, which was posted directly to the patient’s home for completion and returned by post.
Clinical data
Detailed data are collected from the hospital at the start of anti-TNF therapy (or registration in the DMARD control cohort), then 6 monthly for 3 years and annually thereafter. Data collected at each time point include information on anti-rheumatic therapies, disease activity (DAS-28 for RA and PsA, and the VAS for spinal pain and the BASDAI [22] for patients with AS) and details of adverse events. In addition, patients complete a questionnaire that includes the HAQ adapted for the UK [23] at baseline and 6 monthly thereafter for 3 years.
Working status
At baseline and 3 years after inclusion into the register, all patients were sent postal questionnaires which asked two questions regarding their working status. First, patients were asked to describe their current occupation. Secondly, patients were asked to describe their working status as: (i) working full-time, (ii) working part-time, (iii) working full-time in the home, (iv) unemployed but seeking work, (v) not working due to ill health/disability (i.e. work disabled), (vi) student or (vii) retired. Since a number of patients recorded that they were retired at baseline and that they were work disabled at follow-up, we decided to re-classify these patients as work disabled at baseline. Job titles were coded using national Standard Occupational Class codes [24] and were then used to differentiate between manual (e.g. carpenter and farmer) and non-manual jobs (e.g. receptionist and civil servant).
The study was approved by the North West Multicentre Research Ethics Committee, and all subjects gave their written consent for participation.
Statistical analyses
Analysis was restricted to patients aged <62 years and those with complete data on working status at baseline and at follow-up. In each of the four patient cohorts (i.e. anti-TNF RA/AS/PsA and RA controls) baseline demographic and disease-related characteristics were compared between those who were working either full-time or part-time (i.e. working) and those who were work disabled using the t-test for normally distributed data and Mann–Whitney U-test for non-normally distributed data. Categorical data were compared using the chi-square test. Predictors of new work disability at follow-up among patients with RA in the anti-TNF therapy group, who were working at the start of anti-TNF therapy, were identified using univariate and multivariate logistic regression. Covariates included baseline age, gender, disease duration, HAQ score, job type and EULAR good response and DAS-28 remission at 6 months (DAS-28 < 2.6). Variables were included in the multiple regression model if P < 0.1 in the univariate regression analyses. Since data in the anti-TNF therapy RA group were missing at random for baseline HAQ score (4.0%), baseline disease duration (0.7%) and 6-month DAS-28 score (13%), missing data were imputed applying multiple imputation analyses (number of repeated imputations = 5) [25]. The following variables were included in the imputation analyses: age, gender, DAS-28 at baseline and at 6 months, HAQ score at baseline and at 6 months, disease duration at baseline and working status at 3 years. Subsequently, actual DAS-28 scores and imputed DAS-28 scores of missing data were then used to define whether patients were in remission (DAS-28 < 2.6 at 6 months) or had a good response to anti-TNF therapy at 6 months based on the EULAR criteria for good response (i.e. at 6 months DAS-28 < 3.2 and an improvement of DAS-28 > 1.2 after starting anti-TNF therapy) [26].
Multivariate logistic regression analysis was used to assess the relationship between treatment (conventional DMARD treatment vs anti-TNF treatment) and new work disability at follow-up in patients with RA initially working at baseline. Since baseline characteristics differed significantly between the RA anti-TNF therapy and RA control cohort, data were adjusted for those variables with P ≤ 0.1 and/or if the variable had an important influence on the effect of treatment (>10% change in OR).
Imputations were described as above to impute data missing at baseline, the imputations being performed in the RA control cohort and the RA anti-TNF therapy cohort separately. All analyses were carried out using STATA 9.0 (StataCorp, College Station, Texas, USA).
Results
Baseline characteristics
The study population included 3291 consecutive patients with RA, 254 patients with PsA and 229 patients with AS who started anti-TNF therapy. In addition, 379 patients with RA were registered as DMARD controls during that same period of time. Table 1 shows the baseline characteristics of these four cohorts of patients. The AS and PsA patients tended to be younger than the RA anti-TNF cohort and the RA control cohort (median age at baseline, respectively, 43, 46, 53 and 54 years). Around three-quarters of the RA cohort and just over one-half of the PsA cohort were female. As expected, the majority of the AS cohort was male (79%). At baseline, 1236 of 3291 (37.6%) patients in the RA anti-TNF therapy cohort were working and 1627 of 3291 (49.4%) were work disabled (Table 1). Compared with the RA anti-TNF therapy cohort, a smaller proportion of patients were not able to work due to ill health and a greater proportion was working in all other patient cohorts (Table 1).
Table 1.
Baseline characteristics of patients included in the RA control cohort and the three anti-TNF therapy cohorts (RA, PsA and AS)
| Control |
Anti-TNF therapy |
|||||||
|---|---|---|---|---|---|---|---|---|
| na | RA cohort | na | RA cohort | na | PsA cohort | na | AS cohort | |
| Age | ||||||||
| Mean (s.d.), years | 379 | 52 (8) | 3291 | 50 (9) | 254 | 45 (9) | 229 | 44 (10) |
| Median (IQR) | 54 (47–58) | 53 (45–57) | 46 (39–53) | 43 (37–51) | ||||
| Gender (female), n (%) | 379 | 289 (76.3) | 3291 | 2557 (77.7) | 254 | 145 (57.1) | 229 | 48 (21.0) |
| Disease duration | ||||||||
| Mean (s.d.), years | 377 | 8 (9) | 3272 | 13 (9) | 251 | 14 (9) | 229 | 14 (10) |
| Median (IQR) | 4 (1–13) | 11 (6–18) | 13 (7–19) | 13 (6–21) | ||||
| HAQ score | ||||||||
| Mean (s.d.) | 349 | 1.3 (0.8) | 3137 | 2.0 (0.6) | 240 | 1.8 (0.7) | 118 | 4.7 (1.6) |
| Median (IQR) | 1.4 (0.8–1.9) | 2.0 (1.6–2.4) | 1.9 (1.4–2.3) | 1.5 (1.0–2.0) | ||||
| DAS-28 | ||||||||
| Mean (s.d.) | 364 | 5.0 (1.5) | 3233 | 6.6 (1.0) | 237 | 5.9 (1.3) | ||
| Median (IQR) | 5.0 (4.1–6.1) | 6.6 (5.9–7.3) | 6.0 (5.2–6.8) | |||||
| BASDAI | ||||||||
| Mean (s.d.) | 162 | 7.0 (1.8) | ||||||
| Median (IQR) | 7.2 (5.9–8.4) | |||||||
| VAS spinal pain | ||||||||
| Mean (s.d.), mm | 119 | 66 (28) | ||||||
| Median (IQR) | 75 (50–85) | |||||||
| anti-TNF therapy | 3291 | 254 | 229 | |||||
| Infliximab, n (%) | 1558 (47.3) | 152 (59.8) | 125 (54.6) | |||||
| Etanercept, n (%) | 1109 (33.7) | 71 (28.0) | 91 (39.7) | |||||
| Adalimumab, n (%) | 624 (19.0) | 31 (12.2) | 13 (5.7) | |||||
| Working status | ||||||||
| Working full-time, n (%) | 107 (28.2) | 741 (22.5) | 103 (40.6) | 99 (43.2) | ||||
| Working part-time, n (%) | 70 (18.5) | 495 (15.0) | 28 (11.0) | 26 (11.4) | ||||
| Working in the home, n (%) | 24 (6.3) | 167 (5.1) | 4 (1.6) | 2 (0.9) | ||||
| Unemployed but seeking work, n (%) | 3 (0.8) | 20 (0.6) | 2 (0.8) | 2 (0.9) | ||||
| Work disabled, n (%) | 135 (35.6) | 1627 (49.4) | 99 (39.0) | 94 (41.1) | ||||
| Student, n (%) | 3 (0.8) | 19 (0.6) | 4 (1.6) | 1 (0.4) | ||||
| Retired, n (%) | 37 (9.8) | 222 (6.8) | 14 (5.5) | 5 (2.2) | ||||
aNumber of patients with available data. IQR: interquartile range.
Work-disabled vs working patients
Table 2 shows the baseline demographic and clinical characteristics of working and work-disabled patients for each patient cohort. Except in the PsA anti-TNF therapy cohort, work-disabled patients were significantly older than working patients. In the RA and PsA anti-TNF therapy cohorts, work-disabled patients were also more likely to be women. Disease duration was similar between work-disabled and working patients in the AS and PsA anti-TNF therapy cohorts, but was significantly longer for work-disabled patients than working patients in both RA cohorts. In all patient cohorts, work-disabled patients were more disabled (higher HAQ score) and had a higher DAS, i.e. DAS-28 or BASDAI score, than working patients at baseline.
Table 2.
Comparison of baseline characteristics between working and work-disabled patients in the RA control cohort and within each anti-TNF therapy cohort
| Control |
Anti-TNF therapy |
|||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| RA cohort |
RA cohort |
PsA cohort |
AS cohort |
|||||||||
| Working na = 177 | Work disabled na = 135 | P-value* | Working na = 1236 | Work disabled na = 1627 | P-value* | Working na = 131 | Work disabled na = 99 | P-value* | Working na = 125 | Work disabled na = 94 | P-value* | |
| Age | ||||||||||||
| Mean (s.d.), years | 49 (9) | 54 (6) | <0.001 | 48 (9) | 52 (7) | <0.001 | 44 (9) | 46 (9) | 0.200 | 42 (10) | 45 (9) | 0.020 |
| Median (IQR)b | 52 (44–56) | 55 (51–58) | 49 (42–55) | 54 (48–57) | 45 (39–50) | 46 (38–53) | 43 (35–50) | 45 (38–53) | ||||
| Gender (female), n (%) | 130 (73) | 94 (70) | 0.458 | 913 (74) | 1267 (78) | 0.013 | 58 (44) | 71 (72) | <0.001 | 22 (18) | 22 (23) | 0.289 |
| Disease duration | ||||||||||||
| Mean (s.d.) | 7 (8) | 9 (10) | 0.013 | 12 (8) | 14 (9) | <0.001 | 13 (9) | 13 (8) | 0.827 | 14 (10) | 14 (10) | 0.656 |
| Median (IQR)b | 3 (1–10) | 5 (1–15) | 10 (5–17) | 12 (7–19) | 11 (7–19) | 13 (6–19) | 12 (5–20) | 14 (6–22) | ||||
| HAQ score | ||||||||||||
| Mean (s.d.) | 1.0 (0.7) | 1.9 (0.6) | <0.001 | 1.7 (0.6) | 2.2 (0.4) | <0.001 | 1.5 (0.6) | 2.1 (0.5) | <0.001 | 1.2 (0.8) | 1.8 (0.5) | <0.001 |
| Median (IQR)b | 1.0 (0.4–1.4) | 1.9 (1.5–2.3) | 1.8 (1.4–2.1) | 2.3 (2–2.5) | 1.5 (1–2) | 2.1 (1.9–2.5) | 1.3 (0.6–1.9) | 1.8 (1.5–2.1) | ||||
| DAS-28 | ||||||||||||
| Mean (s.d.)c | 4.6 (1.4) | 5.4 (1.5) | <0.001 | 6.4 (1.0) | 6.7 (1.0) | <0.001 | 5.8 (1.2) | 6.1 (1.2) | 0.041 | |||
| Median (IQR) | 4.7 (3.7–5.6) | 5.6 (4.4–6.5) | 6.4 (5.8–7.0) | 6.7 (6.0–7.4) | 5.9 (5.1–6.5) | 6.2 (5.4–7.0) | ||||||
| BASDAI | ||||||||||||
| Mean (s.d.) | 6.6 (2.0) | 7.6 (1.5) | 0.001 | |||||||||
| Median (IQR)b | 6.7 (5.4–8.1) | 7.5 (6.6–8.7) | ||||||||||
| VAS spinal pain | ||||||||||||
| Mean (s.d.), mm | 64 (25) | 70 (29) | 0.076 | |||||||||
| Median (IQR)b | 71 (50–80) | 78 (56–93) | ||||||||||
aNumber of patients. bMann–Whitney U-test was used for non-normally distributed data. ct-Test for normally distributed data. IQR: interquartile range. *P-value for statistical significance.
Change in working status during follow-up
At baseline, 1050 of 1669 working patients reported that they were working full-time. Seventy-six per cent of these patients were still working full-time 3 years after inclusion, ranging from 71% in the RA control cohort to 88% in the AS anti-TNF cohort (Table 3). Of the 1236 patients in the RA anti-TNF therapy group working at baseline, 996 (80.6%) were still working after 3 years and 112 (9.1%) became work disabled (Table 3). Among the 1627 patients in this group who were not working due to ill health at baseline, only 66 (4.1%) were working again 3 years after commencing anti-TNF therapy. During follow-up, 5.1% (9 of 177) of working patients in the RA control cohort became work disabled and 3.0% (4 of 135) of work-disabled patients started to work again. In the PsA and AS anti-TNF therapy cohorts, these percentages were, respectively, 6.9% (9 of 131) and 6.1% (6 of 99) in the PsA group and 4.0% (5 of 125) and 8.5% (8 of 94) in the AS cohort. Of all 135 working patients who became work disabled during follow-up, 50 (37%) had a manual job at inclusion in the register.
Table 3.
Change in working status over 3 years
| Working at baseline | Work disabled at 3 years, n (%) | Work disabled at baseline | Working at 3 years, n (%) | Working full-time at baseline | Working full-time at 3 years, n (%) | ||||
|---|---|---|---|---|---|---|---|---|---|
| RA control group | 177 | → | 9 (5.1) | 135 | → | 4 (3.0) | 107 | → | 76 (71.0) |
| RA anti-TNF group | 1236 | → | 112 (9.1) | 1627 | → | 66 (4.1) | 741 | → | 545 (73.5) |
| PsA anti-TNF group | 131 | → | 9 (6.9) | 99 | → | 6 (6.1) | 103 | → | 85 (82.5) |
| AS anti-TNF group | 125 | → | 5 (4.0) | 94 | → | 8 (8.5) | 99 | → | 87 (87.9) |
Predictors of work disability
In working patients in the RA anti-TNF therapy cohort, a higher HAQ score and having a manual job at baseline, but not age, gender, disease duration or a good EULAR response at 6 months, were associated with new work disability at follow-up (Table 4). In the multivariate analyses, high HAQ score and a manual job were strong predictors of new work disability at follow-up.
Table 4.
Predictors of new work disability in patients with RA who were working at the start of anti-TNF therapy
| Univariate analysis |
Multivariate analyses |
||||
|---|---|---|---|---|---|
| OR (95% CI) | P-value | OR (95% CI) | P-value | FMI | |
| Age | 1.02 (1.00, 1.04) | 0.100 | 1.02 (0.99, 1.04) | 0.188 | 0.001 |
| Gender, female vs male | 1.01 (0.65, 1.58) | 0.961 | |||
| Disease duration at baseline | 1.01 (0.99, 1.04) | 0.232 | |||
| HAQ score | 2.79 (1.89, 4.12) | <0.001 | 2.86 (1.90, 4.30) | <0.001 | 0.016 |
| DAS-28 remission at 6 months | 0.55 (0.31, 0.99) | 0.046 | 0.75 (0.41, 1.39) | 0.361 | 0.109 |
| DAS-28 good response at 6 months | 0.66 (0.42, 1.04) | 0.073 | |||
| Manual job | 2.31 (1.52, 3.52) | <0.001 | 2.53 (1.64, 3.91) | <0.001 | 0.000 |
FMI: fraction of missing information. This measures the relative increase in the uncertainty about the coefficient of interest due to missing data. For example, had we had complete data on all subjects for all variables, the variance of the estimate of the effect of age would decrease by nearly 0.1%, whilst the variance of the estimate of the effect of DAS-28 remission would decrease by 11%. In these analyses, only those working patients at baseline (n = 1108) who were either working or work disabled at follow-up were included in the analyses.
Compared with the use of conventional DMARD therapy, the use of anti-TNF therapy did not prevent patients with RA from becoming work disabled [crude OR conventional DMARD therapy vs anti-TNF therapy 0.55; 95% CI 0.28, 1.12; P = 0.101 and adjusted OR 0.80; 95% CI 0.36, 1.81; P = 0.596 (adjusted for HAQ score, DAS-28 and manual job at baseline)]. However, patients in the anti-TNF group who were in remission 6 months after commencing anti-TNF therapy were less likely to become work disabled 3 years after inclusion in the register.
Discussion
In this study we found that, in all three anti-TNF-treated patient cohorts, work disability rates were already high at entry into the register ranging from 39 to 49%. These percentages are similar to those previously reported for populations with long-standing RA, PsA and AS [1–3]. It should be noted that this particular cohort of patients receiving anti-TNF therapy already had severe disease at entry to the study due to the UK prescribing guidelines for such therapies. In addition, after only a median disease duration of 4 years, already 36% of the DMARD control group were work disabled, again demonstrating that work disability occurs early in RA. At baseline, both functional disability and disease activity were much worse in patients who were work disabled compared with those who were working full- or part-time. This observation was seen in all four patient cohorts and resembles that found in previous publications [1].
Most previous studies investigating the effects of anti-TNF therapy on employment status were conducted in cohorts of patients with RA [11–13, 27, 28], whereas less is known about the effect of anti-TNF treatment on work disability among patients with PsA [16] or with AS [14, 17].
In a 24-week clinical trial of infliximab in patients with AS [17], there was no change in employment. On the other hand, in a small UK descriptive study of patients with AS, the use of anti-TNF therapy was associated with increased gainful employment [14]. In this latter study, 21% of work-disabled patients started to work again after anti-TNF therapy, which was higher than in our study (8.5%). This difference may, in part, be explained by the possible inclusion in our study of people who had never had a paid job and/or were not seeking a paid job in our study but described themselves as not able to work due to ill health, thus increasing the number of patients in the denominator.
In our study with a follow-up duration of 3 years, the number of working patients with PsA who became work disabled (n = 9) was slightly higher than the number of work-disabled patients who started to work again (n = 6). In a short-term study of patients with PsA, treatment with infliximab did not improve employment status or employability (i.e. patients who felt well enough to work if a job became available) [16]. However, in both this short-term study of PsA and the study of AS [17], productivity increased significantly in the anti-TNF therapy-treated group compared with the control group.
Among the 1108 working patients with RA in the anti-TNF therapy cohort at baseline, 996 were still working 3 years after inclusion in the register and 112 became work disabled. Patients with worse functional disability and a manual job at the start of anti-TNF therapy were more likely to become work disabled during follow-up; factors often found to be associated with work disability in patients with RA [1]. We did not perform such analyses in the PsA and the AS patient groups because of the small number of working patients at baseline who became work disabled after 3 years in these two patient cohorts.
It is unclear whether or not anti-TNF therapy is more effective in the prevention of new work disability in patients with long-standing RA when compared with standard DMARDs. In a previous study, a beneficial effect of etanercept use on the prevention of work disability in patients with RA was found comparing data from a clinical trial with that of an observational cohort [13]. In contrast, we did not find an association between anti-TNF therapy treatment and less work disability, a result similar to that of the two other observational studies of patients with long-standing RA (mean disease duration >10 years [11, 12]). It is not clear whether the discrepancies between these studies are due to differences with anti-TNF-treated cohorts (i.e. clinical trial vs observational data), the difference between DMARD control groups within each study or residual confounding.
Previous studies have shown that severe joint damage is associated with irreversible disability and the ability to improve this disability declines with disease duration [29]. Even if patients with long-standing RA respond to anti-TNF therapy, the likelihood of regaining employment is very low [30–32]. Therefore, it is important to investigate the effect of anti-TNF therapy in patients with early arthritis. In two published clinical trials, one performed in the UK [15, 28] and one international study, of anti-TNF therapy in early RA (mean disease duration <1 year) employment/job loss rates did not differ between the placebo plus MTX group and the anti-TNF plus MTX treatment group. However, patients in the anti-TNF therapy groups lost fewer workdays, increased productivity and were more likely to be employable. The results from the international clinical trial showed that, in multivariate regression analyses, treatment did not predict employability, whereas response to treatment did. In our study, we also found an association between response to treatment and reduced work disability in the anti-TNF therapy group. It must, however, be noted that the proportion of missing information was relatively high (i.e. 10%) for the covariate DAS-28 remission at 6 months.
Since the results of our study are based on self-reported data, some of the results must be interpreted with caution. Unfortunately, we do not know the underlying cause of the patients’ inability to work because we did not ask specifically about arthritis-related work disability. Patients were considered to be work disabled if they described themselves as not able to work due to ill health at baseline, and therefore may include patients who were on temporary sick leave, or patients who reported that they were retired at baseline and not able to work due to ill health at follow-up. Thus, the percentage of work disability presented in this study might be overestimated. On the other hand, patients who reported that they were retired at baseline may have retired early because of their disease. It is also possible that patients who recorded that they were not working due to ill health had never had a paid job before the onset of their disease, a population often excluded from analyses to estimate work disability rates in previous studies. In addition, since data for this study were obtained over a 5-year period, we do not know whether changes in the economic climate had any influence on the change in working status of the patients.
In summary, there is less future work disability in working patients with RA who respond to anti-TNF therapy. Unfortunately, a high percentage of patients with RA, AS and PsA were already work disabled at the start of anti-TNF therapy and had worse disease activity and more functional disability than patients who were working. Earlier introduction of anti-TNF therapy, resulting in a better response and prevention of irreversible joint damage, may prevent patients with RA, AS and PsA from becoming work disabled in the future.
Acknowledgements
The authors acknowledge the enthusiastic collaboration of all consultant rheumatologists and their specialist nurses in the UK in providing the data. In addition, we acknowledge the support from Ian Griffiths (Past) and David Isenberg (Current), Chairs of the BSRBR Management Committee, Gabriel Panayi, David G. I. Scott, Andrew Bamji and Deborah Bax, Presidents of the BSR during the period of data collection, for their active role in enabling the Register to undertake its tasks and to Samantha Peters (CEO of the BSR), Mervyn Hogg, Nia Taylor and members of the BSRBR Scientific Steering Committee. We also acknowledge the seminal role of the BSR Clinical Affairs Committee in establishing the national biologic guidelines and recommendations for such a Register. Finally, we would like to acknowledge the substantial contribution of Andy Tracey and Katie McGrother in database design and manipulation and Alan Silman in his prior role as a principal investigator of the BSRBR. The BSR commissioned the BSRBR as a UK-wide national project to investigate the safety of biologic agents in routine medical practice. D.P.M.S. and K.L.H. are principal investigators of the BSRBR. The BSR receives restricted income from UK pharmaceutical companies, presently Abbott Laboratories, Biovitrum, Schering Plough, Wyeth Pharmaceuticals and Roche. This income finances a wholly separate contract between the BSR and the University of Manchester, who provide and run the BSRBR data collection, management and analysis services. The principal investigators and their team have full academic freedom and are able to work independently of pharmaceutical industry influence. All decisions concerning analyses, interpretation and publication are made autonomously of any industrial contribution. Members of the Manchester team, BSR trustees, committee members and staff completed an annual declaration in relation to conflicts of interest.
Funding: Funding to pay the open access charges for this article was provided by the British Society for Rheumatology.
Disclosure statement: The authors have declared no conflicts of interest.
References
- 1.Verstappen SM, Bijlsma JW, Verkleij H, et al. Overview of work disability in rheumatoid arthritis patients as observed in cross-sectional and longitudinal surveys. Arthritis Rheum. 2004;51:488–97. doi: 10.1002/art.20419. [DOI] [PubMed] [Google Scholar]
- 2.Boonen A. A review of work-participation, cost-of-illness and cost-effectiveness studies in ankylosing spondylitis. Nat Clin Pract Rheumatol. 2006;2:546–53. doi: 10.1038/ncprheum0297. [DOI] [PubMed] [Google Scholar]
- 3.Mau W, Listing J, Huscher D, Zeidler H, Zink A. Employment across chronic inflammatory rheumatic diseases and comparison with the general population. J Rheumatol. 2005;32:721–8. [PubMed] [Google Scholar]
- 4.Maini R, St Clair EW, Breedveld F, et al. Infliximab (chimeric anti-tumour necrosis factor alpha monoclonal antibody) versus placebo in rheumatoid arthritis patients receiving concomitant methotrexate: a randomised phase III trial. ATTRACT Study Group. Lancet. 1999;354:1932–9. doi: 10.1016/s0140-6736(99)05246-0. [DOI] [PubMed] [Google Scholar]
- 5.Klareskog L, van der Heijde D, de Jager JP, et al. Therapeutic effect of the combination of etanercept and methotrexate compared with each treatment alone in patients with rheumatoid arthritis: double-blind randomised controlled trial. Lancet. 2004;363:675–81. doi: 10.1016/S0140-6736(04)15640-7. [DOI] [PubMed] [Google Scholar]
- 6.Weinblatt ME, Keystone EC, Furst DE, et al. Adalimumab, a fully human anti-tumor necrosis factor alpha monoclonal antibody, for the treatment of rheumatoid arthritis in patients taking concomitant methotrexate: the ARMADA trial. Arthritis Rheum. 2003;48:35–45. doi: 10.1002/art.10697. [DOI] [PubMed] [Google Scholar]
- 7.Kavanaugh A, Antoni C, Krueger GG, et al. Infliximab improves health related quality of life and physical function in patients with psoriatic arthritis. Ann Rheum Dis. 2006;65:471–7. doi: 10.1136/ard.2005.040196. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Antoni C, Krueger GG, de VK, et al. Infliximab improves signs and symptoms of psoriatic arthritis: results of the IMPACT 2 trial. Ann Rheum Dis. 2005;64:1150–7. doi: 10.1136/ard.2004.032268. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Baraliakos X, Brandt J, Listing J, et al. Outcome of patients with active ankylosing spondylitis after two years of therapy with etanercept: clinical and magnetic resonance imaging data. Arthritis Rheum. 2005;53:856–63. doi: 10.1002/art.21588. [DOI] [PubMed] [Google Scholar]
- 10.Haibel H, Rudwaleit M, Brandt HC, et al. Adalimumab reduces spinal symptoms in active ankylosing spondylitis: clinical and magnetic resonance imaging results of a fifty-two-week open-label trial. Arthritis Rheum. 2006;54:678–81. doi: 10.1002/art.21563. [DOI] [PubMed] [Google Scholar]
- 11.Wolfe F, Allaire S, Michaud K. The prevalence and incidence of work disability in rheumatoid arthritis, and the effect of anti-tumor necrosis factor on work disability. J Rheumatol. 2007;34:2211–7. [PubMed] [Google Scholar]
- 12.Allaire S, Wolfe F, Niu J, Zhang Y, Zhang B, LaValley M. Evaluation of the effect of anti-tumor necrosis factor agent use on rheumatoid arthritis work disability: the jury is still out. Arthritis Rheum. 2008;59:1082–9. doi: 10.1002/art.23923. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Yelin E, Trupin L, Katz P, Lubeck D, Rush S, Wanke L. Association between etanercept use and employment outcomes among patients with rheumatoid arthritis. Arthritis Rheum. 2003;48:3046–54. doi: 10.1002/art.11285. [DOI] [PubMed] [Google Scholar]
- 14.Keat AC, Gaffney K, Gilbert AK, Harris C, Leeder J. Influence of biologic therapy on return to work in people with work disability due to ankylosing spondylitis. Rheumatology. 2008;47:481–3. doi: 10.1093/rheumatology/ken010. [DOI] [PubMed] [Google Scholar]
- 15.Bejarano V, Quinn M, Conaghan PG, et al. Effect of the early use of the anti-tumor necrosis factor adalimumab on the prevention of job loss in patients with early rheumatoid arthritis. Arthritis Rheum. 2008;59:1467–74. doi: 10.1002/art.24106. [DOI] [PubMed] [Google Scholar]
- 16.Kavanaugh A, Antoni C, Mease P, et al. Effect of infliximab therapy on employment, time lost from work, and productivity in patients with psoriatic arthritis. J Rheumatol. 2006;33:2254–9. [PubMed] [Google Scholar]
- 17.van der Heijde D, Han C, DeVlam K, et al. Infliximab improves productivity and reduces workday loss in patients with ankylosing spondylitis: results from a randomized, placebo-controlled trial. Arthritis Rheum. 2006;55:569–74. doi: 10.1002/art.22097. [DOI] [PubMed] [Google Scholar]
- 18.Silman A, Symmons D, Scott DG, Griffiths I. British Society for Rheumatology Biologics Register. Ann Rheum Dis. 2003;62(Suppl. 2):ii28–9. doi: 10.1136/ard.62.suppl_2.ii28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Hyrich K, Symmons D, Watson K, Silman A. Baseline comorbidity levels in biologic and standard DMARD treated patients with rheumatoid arthritis: results from a national patient register. Ann Rheum Dis. 2006;65:895–8. doi: 10.1136/ard.2005.043158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Prevoo ML, van‘t Hof MA, Kuper HH, van Leeuwen MA, van de Putte LB, van Riel PL. Modified disease activity scores that include twenty-eight-joint counts. Development and validation in a prospective longitudinal study of patients with rheumatoid arthritis. Arthritis Rheum. 1995;38:44–8. doi: 10.1002/art.1780380107. [DOI] [PubMed] [Google Scholar]
- 21.Ledingham J, Deighton C. Update on the British Society for Rheumatology guidelines for prescribing TNFalpha blockers in adults with rheumatoid arthritis (update of previous guidelines of April 2001) Rheumatology. 2005;44:157–63. doi: 10.1093/rheumatology/keh464. [DOI] [PubMed] [Google Scholar]
- 22.Garrett S, Jenkinson T, Kennedy LG, Whitelock H, Gaisford P, Calin A. A new approach to defining disease status in ankylosing spondylitis: the Bath Ankylosing Spondylitis Disease Activity Index. J Rheumatol. 1994;21:2286–91. [PubMed] [Google Scholar]
- 23.Kirwan JR, Reeback JS. Stanford Health Assessment Questionnaire modified to assess disability in British patients with rheumatoid arthritis. Br J Rheumatol. 1986;25:206–9. doi: 10.1093/rheumatology/25.2.206. [DOI] [PubMed] [Google Scholar]
- 24.National Office of Statistics, Standard Occupational Classification 2000 (SOC2000) 2000 [Google Scholar]
- 25.van Buuren S, Boshuizen HC, Knook DL. Multiple imputation of missing blood pressure covariates in survival analysis. Stat Med. 1999;18:681–94. doi: 10.1002/(sici)1097-0258(19990330)18:6<681::aid-sim71>3.0.co;2-r. [DOI] [PubMed] [Google Scholar]
- 26.van Gestel AM, Haagsma CJ, van Riel PL. Validation of rheumatoid arthritis improvement criteria that include simplified joint counts. Arthritis Rheum. 1998;41:1845–50. doi: 10.1002/1529-0131(199810)41:10<1845::AID-ART17>3.0.CO;2-K. [DOI] [PubMed] [Google Scholar]
- 27.Farahani P, Levine M, Gaebel K, Wang EC, Khalidi N. Community-based evaluation of etanercept in patients with rheumatoid arthritis. J Rheumatol. 2006;33:665–70. [PubMed] [Google Scholar]
- 28.Smolen JS, Han C, van der Heijde D, et al. Infliximab treatment maintains employability in patients with early rheumatoid arthritis. Arthritis Rheum. 2006;54:716–22. doi: 10.1002/art.21661. [DOI] [PubMed] [Google Scholar]
- 29.Aletaha D, Strand V, Smolen JS, Ward MM. Treatment-related improvement in physical function varies with duration of rheumatoid arthritis: a pooled analysis of clinical trial results. Ann Rheum Dis. 2008;67:238–43. doi: 10.1136/ard.2007.071415. [DOI] [PubMed] [Google Scholar]
- 30.Han C, Smolen J, Kavanaugh A, St Clair EW, Baker D, Bala M. Comparison of employability outcomes among patients with early or long-standing rheumatoid arthritis. Arthritis Rheum. 2008;59:510–4. doi: 10.1002/art.23541. [DOI] [PubMed] [Google Scholar]
- 31.Smolen JS, Aletaha D. Patients with rheumatoid arthritis in clinical care. Ann Rheum Dis. 2004;63:221–5. doi: 10.1136/ard.2003.012575. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Kavanaugh A, Han C, Bala M. Functional status and radiographic joint damage are associated with health economic outcomes in patients with rheumatoid arthritis. J Rheumatol. 2004;31:849–55. [PubMed] [Google Scholar]


