Abstract
Objective
To conduct a quantitative survey that focuses on oncologists' practice patterns and attitudes surrounding treatment-related infertility and fertility preservation, specifically among women of reproductive age.
Study Design
A 19-item survey was emailed to medical, pediatric, radiation and surgical oncologists at Duke University. Descriptive statistics were used.
Results
Most oncologists (61%) who responded always or usually discuss the impact treatment will have on fertility. Nearly half (45%) never refer women to reproductive specialists. Respondents who attended an educational session on fertility preservation were more likely to consider a patient's desire for fertility when planning her treatment than those who did not attend (45% vs. 33%). More than half (55%) of attendees were willing to consider a less aggressive regimen to preserve fertility, compared with 29% of those who did not attend.
Conclusion
While most oncologists recognize the importance of discussing infertility risks, many do not discuss fertility preservation routinely. Reasons for this discrepancy included poor prognosis and emergent need to start therapy. Increasing awareness through educational events may influence current practice patterns and increase collaboration between reproductive endocrinologists and oncologists.
Keywords: cancer, chemotherapy, cryopreservation, oncology, patient education
Reluctance among physicians to discuss or refer for fertility preservation has costs on patients' future fertility and morale through treatment.
The combination of improving cancer survival rates and the trend toward delayed childbearing has led to an increase in the number of women of reproductive age who are being treated for and surviving various forms of cancer.1 Although certain types of cancer treatment, for example, high doses of alkylating agents, are more likely to result in infertility via premature ovarian failure, advances in reproductive medicine provide some hope for the preservation of fertility after treatment.2 Techniques such as oocyte cryopreservation, ovarian tissue cryopreservation and ovarian suppression with gonadotropin-releasing hormone (GnRH) agonists are available at some centers. The American Society of Clinical Oncology (ASCO) and the American Society for Reproductive Medicine (ASRM) have recommended that the impact of cancer treatments on fertility be addressed with all cancer patients of reproductive age and that options for fertility preservation, such as embryo cryopreservation, be discussed routinely.2,3 Despite this strong recommendation, a large percentage of cancer patients do not recall having had a discussion related to fertility before treatment; reasons for this discrepancy are worthy of exploration.
To date, published quantitative surveys evaluating oncologists' views and practice patterns have focused on sperm cryopreservation among male patients.4,5 The purpose of this study was to quantitatively explore oncologists' practice patterns and attitudes surrounding treatment-related infertility and fertility preservation among women of reproductive age.
Materials and Methods
A 19-item survey was designed, and data were collected using the online survey tool Survey Monkey (www.surveymonkey.com). The study was reviewed and exempted by the Institutional Review Board at Duke University. The survey was sent in April 2007 via e-mail to 91 oncologists at Duke University Medical Center. Gynecologic oncologists were excluded because they are likely to have received formal education on infertility during residency training. E-mail addresses were obtained from faculty listings and the Duke University online directory. Individual responses were kept anonymous.
Primary variables for analysis included answers to the questions, “How often do you discuss the impact a female patient's condition and/or treatment will have on her future fertility?” and “Do you ever refer patients to a reproductive endocrinologist or obstetrician/gynecologist who specializes in fertility?” (Figure 1). Multiple selections were listed for those who did not always discuss the impact or refer to specialists. The questionnaire also asked respondents about designing treatment regimens, their knowledge of the impact of chemotherapeutic agents on fertility, their agreement with ASCO and ASRM recommendations and whether they attended a special seminar on fertility preservation. Question types included Yes/No, True/False, Multiple Choice, 5-Point Likert Scale (Always, Usually, Sometimes, Rarely, Never) and 3-Point Likert Scale (Very Knowledgeable Of, Aware Of, Never Heard Of). Descriptive statistics were employed to assess and present survey results.
Figure 1.
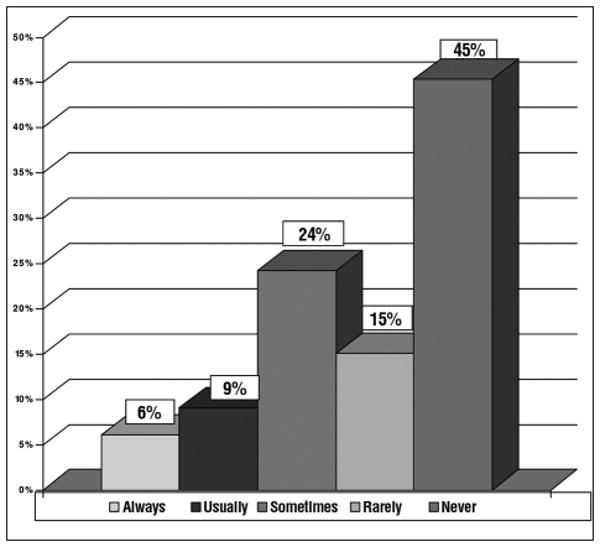
Survey question: How often do you refer patients to a reproductive endocrinologist or an OB/GYN who specializes in fertility?
Results
There was a 40% response rate (36 of 91) among physicians included in this analysis. Of respondents, 62% (22 of 36) were medical oncologists, 22% (8 of 36) pediatric oncologists and 17% (6 of 36) radiation oncologists. No surgical oncologists responded.
Results indicated that the majority of oncologists (61%) always or usually discuss the impact treatment may have on fertility. Common reasons for not discussing the impact on fertility included poor prognosis (53%), need for immediate therapy (24%) and already having children (24%). Multiple selections were allowed. Of interest, nearly half (45%) never refer women to reproductive specialists, with only 15% routinely referring (Figure 1). The most common reasons for not referring were patient disinterest in preserving fertility (39%) and limited time because of emergent need to start therapy (13%). Of oncologists who treat more than 50 women per year, 77% have referred patients to reproductive specialists compared with 43% of oncologists who treat less than 50 women per year.
The vast majority of oncologists were “aware of” or “very knowledgeable of” techniques such as in vitro fertilization (IVF) with embryo cryopreservation (97%), oocyte cryopreservation (97%), ovarian tissue cryopreservation (85%) and ovarian suppression with GnRH agonists (85%). Most (72%) knew that alkylating agents are considered the most gonadotoxic class of chemotherapeutics. All respondents agreed with ASCO and ASRM recommendations that oncologists have a responsibility to inform patients that treatments may permanently impair fertility.
Finally, respondents who attended a Duke University Medical Oncology educational session, Fertility Among Cancer Survivors, (11 of 35) were more likely to “always” or “usually” consider a patient's desire for future fertility when planning her treatment regimen compared with those who did not attend (45% vs. 33%, respectively). More than half (55%) of attendees were willing to consider a less aggressive regimen to preserve fertility, compared with 29% of those who did not attend.
Discussion
This report represents the first quantitative survey, to our knowledge, of oncologists' attitudes toward and knowledge of treatment-related infertility and fertility preservation specifically devoted to female cancer patients. Our findings indicated that nearly two-thirds of oncologists from a single academic medical center routinely discussed the impact of potentially gonadotoxic treatments on future fertility with their female patients; however, nearly half have never made referrals to reproductive specialists despite significant advances in the field.
Our findings suggest a discrepancy between physicians' beliefs and patients' preferences. Although the most common reason cited for lack of referral was patients' disinterest in preserving fertility (39%), surveys of patients have indicated widespread interest. For example, 73% of young women diagnosed with breast cancer were concerned about the possibility of becoming infertile with treatment.6 In another patient survey, 77% of men who were childless at the time of their cancer diagnosis reported that they wanted to have children in the future.7 The perceived disinterest among patients by oncologists compared with patients' apparent strong interest is deserving of continued exploration and may point to a need for further professional education.
It is interesting to note that no surgical oncologists responded to the survey. Two qualitative surveys have been published in which 24 pediatric and 16 adult oncologists were interviewed about fertility preservation.8,9 One of these surveys echoed the potential lack of interest among surgical oncologists; one commented, “I don't give the chemo [sic] and that's up to the med onc [sic] to discuss.”8 Yet the surgical oncologist may be the first physician among a multidisciplinary team to treat a newly diagnosed patient. Therefore valuable time may be lost by waiting for a medical oncologist to discuss fertility preservation and refer to reproductive specialists. Future research is necessary to explore the barriers to discussions about fertility preservation among surgical oncologists.
To date, there have been few surveys addressing oncologists' knowledge and practices regarding fertility preservation. Two published surveys of oncologists focused on sperm cryopreservation for male cancer patients.4,5 These surveys indicated that fewer than half routinely offered sperm banking and only 26% were aware of intracytoplasmic sperm injection. Additionally, a survey conducted among pediatric oncology providers regarding fertility issues in pediatric cancer patients found that only 35% of providers currently consulted with reproductive specialists whereas 93% indicated a desire to do so in the future.10 A recent study in the United Kingdom reviewed data forms for over 1,000 patients collected prospectively from pediatric oncologists.11 Although the effect of cancer treatments on fertility was discussed with 63% of patients regardless of gender, only 1% of newly diagnosed girls were referred to a reproductive specialist. Studies featuring interviews of pediatric and adult oncologists on their opinions regarding fertility preservation indicated that referrals for fertility preservation are not routinely made.8,9
Reluctance among physicians to discuss or refer for fertility preservation has costs on patients' future fertility and morale through treatment. Several surveys, reported from the patient's perspective, have addressed the reproductive concerns of cancer patients.6,7,12-14 The fear of infertility and the possibility of chemotherapy-related effects on offspring are commonly listed as concerns by patients, and these concerns can have an impact on their quality of life.12 One study found that 73% of breast cancer survivors were at least somewhat concerned about fertility. Even among those who had already conceived, 56% wished to have more children. However, only 17% had met with an infertility specialist.6 Another survey of female cancer survivors of reproductive age revealed that only 57% recalled receiving information about treatment-related risks, indicating that this important message is not reaching all patients at risk and is consistent with the results reported herein.13
In addition to the benefits for future fertility, counseling on fertility preservation options may be important in helping patients cope with their condition and therapy. One study, for example, found that men who banked their sperm felt it was a positive factor in coping emotionally with cancer.14 A physician's recommendation was a strong predictor of whether a patient banked his sperm.7
Our results indicate that although most oncologists recognize the importance of discussing infertility risks with female patients, in practice many do not discuss fertility preservation routinely. Reasons given for not discussing fertility preservation included poor prognosis, emergent need to start therapy and the fact that many of these women may have already had children before their cancer diagnosis. Surveys of patients have shown that some of these reasons, specifically already having children, may not be valid because some women may have a strong desire to complete a family or may have a new partner.6 Discussing fertility and taking fertility-preserving measures may boost patients' morale as they undergo chemotherapy and radiation therapy.7
Our results also suggest that increasing awareness through educational events addressing fertility preservation may influence current practice patterns. We found that oncologists who attended a fertility preservation seminar were more likely to consider a patient's desire for future fertility and to consider less aggressive regimens. Given the small sample size, these results were not statistically significant. Larger studies are indicated to evaluate the impact of educational programs.
This study has several limitations. Because we surveyed physicians from a single academic center, these results may not reflect the views of oncologists in different practice settings and geographic locations. In some areas, for example, reproductive services are not readily available. Our response rate of 40% was slightly better than the 24% and 28% response rates in the surveys focusing on sperm cryospreservation.4,5 It is possible that physicians who are more interested in fertility preservation, and thus perhaps more knowledgeable about current techniques, may have been more likely to respond. However, response rates were similar among those who attended an educational session on fertility preservation and those who did not attend, 41% (12 of 29) vs. 39% (24 of 62). Despite these limitations, this survey illustrates an ability to survey oncologists regarding fertility preservation among women and highlights interesting trends deserving further exploration with a geographically and professionally diverse physician population.
Infertility is of paramount concern among a majority of female patients as they face a cancer diagnosis and treatment plan, many of which will compromise future fertility. Although both ASCO and ASRM state that the impact of cancer treatments on fertility and options for fertility preservation should be addressed with all cancer patients of reproductive age, our results indicate that this important message is reaching approximately half of the intended population in one academic center. To better understand the barriers to care and most appropriate interventions, a larger scale, nationwide survey of oncologists is needed to determine whether the trends identified in this pilot survey are more broadly applicable. The overall goal is to facilitate communication between oncologists and reproductive endocrinologists to improve the care of women with cancer.
Acknowledgments
The authors would like to thank Anne D. Lyerly, M.D., for her suggestions after reviewing this manuscript.
Footnotes
Financial Disclosure: The authors have no connection to any companies or products mentioned in this article.
Presented as a poster at the 63rd Annual Meeting of the American Society for Reproductive Medicine, Washington, D.C., October 13-17, 2007.
References
- 1.Marhhom E, Cohen I. Fertility preservation options for women with malignancies. Obstet Gynecol Surv. 2007;62:58–72. doi: 10.1097/01.ogx.0000251029.93792.5d. [DOI] [PubMed] [Google Scholar]
- 2.Lee SJ, Schover LR, Partridge AH, et al. American Society of Clinical Oncology recommendations on fertility preservation in cancer. J Clin Oncol. 2006;24:2917–2931. doi: 10.1200/JCO.2006.06.5888. [DOI] [PubMed] [Google Scholar]
- 3.Ethics Committee of the American Society for Reproductive Medicine: Fertility preservation and reproduction in cancer patients. Fertil Steril. 2005;83:1622–1628. doi: 10.1016/j.fertnstert.2005.03.013. [DOI] [PubMed] [Google Scholar]
- 4.Schover LR, Brey K, Lichtin A, et al. Oncologists' attitudes and practices regarding banking sperm before cancer treatment. J Clin Oncol. 2002;20:1890–1897. doi: 10.1200/JCO.2002.07.174. [DOI] [PubMed] [Google Scholar]
- 5.Zapzalka DM, Redmon JB, Pryor JL. A survey of oncologists regarding sperm cryopreservation and assisted reproductive techniques for male cancer patients. Cancer. 1999;86:1812–1817. doi: 10.1002/(sici)1097-0142(19991101)86:9<1812::aid-cncr24>3.0.co;2-l. [DOI] [PubMed] [Google Scholar]
- 6.Partridge AH, Gelber S, Peppercorn J, et al. Web-based survey of fertility issues in young women with breast cancer. J Clin Oncol. 2004;22:4174–4183. doi: 10.1200/JCO.2004.01.159. [DOI] [PubMed] [Google Scholar]
- 7.Schover LR, Brey K, Lichtin A, et al. Knowledge and experience regarding cancer, infertility, and sperm banking in younger male survivors. J Clin Oncol. 2002;20:1880–1889. doi: 10.1200/JCO.2002.07.175. [DOI] [PubMed] [Google Scholar]
- 8.Quinn GP, Vadaparampil ST, Gwede CK, et al. Discussion of fertility preservation with newly diagnosed patients: Oncologists' views. J Cancer Surviv. 2007;1:146–155. doi: 10.1007/s11764-007-0019-9. [DOI] [PubMed] [Google Scholar]
- 9.Vadaparampil S, Quinn G. Barriers to fertility preservation among pediatric oncologists. Patient Educ Couns. 2008;72:402–410. doi: 10.1016/j.pec.2008.05.013. [DOI] [PubMed] [Google Scholar]
- 10.Goodwin T, Oosterhuis BE. Attitudes and practices of pediatric oncology providers regarding fertility issues. Pediatr Blood Cancer. 2007;48:80–85. doi: 10.1002/pbc.20814. [DOI] [PubMed] [Google Scholar]
- 11.Anderson RA, Weddel A, Spoudeas HA, et al. Do doctors discuss fertility issues before they treat young patients with cancer? Hum Reprod. 2008;23:2246–2251. doi: 10.1093/humrep/den252. [DOI] [PubMed] [Google Scholar]
- 12.Wenzel L, Dogan-Ates A, Habbal R, et al. Defining and measuring reproductive concerns of female cancer survivors. J Natl Cancer Inst Monogr. 2005;34:94–98. doi: 10.1093/jncimonographs/lgi017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Schover LR, Rybicki LA. Having children after cancer: A pilot survey of survivors' attitudes and experiences. Cancer. 1999;86:697–709. doi: 10.1002/(sici)1097-0142(19990815)86:4<697::aid-cncr20>3.0.co;2-j. [DOI] [PubMed] [Google Scholar]
- 14.Saito K, Suzuki K, Iwasaki A, et al. Sperm cryopreservation before cancer chemotherapy helps in the emotional battle against cancer. Cancer. 2005;104:521–524. doi: 10.1002/cncr.21185. [DOI] [PubMed] [Google Scholar]


