Abstract
Understanding bridging behaviors of clients of female sex workers (FSWs) is important for projecting and intervening in the spread of sexually transmitted infections in Vietnam. The goals of the study were to determine HIV/STI prevalence amongst different bridging groups, identify factors associated with being potential and active bridgers, and assess the association of drug use and unsafe sex with HIV and/or STI prevalence. In April, 2007, 292 clients were anonymously interviewed at sex venues in a two-stage time-location cluster sampling survey, followed by HIV, syphilis, and HSV-2 testing. Based on condom use with both high-risk (FSWs) and low-risk (wives/girlfriends) sexual partners, clients were classified as unlikely, potential, or active bridgers. The majority of clients were potential or active bridgers (55.8%) who had a significantly higher prevalence of herpes simplex type 2 (HSV-2) (21% and 33%, respectively) than unlikely bridgers (8.7%). HIV seropositivity was 4.4-fold (95% CI 1.1–17.1) higher among those who were HSV-2-positive. Clients of FSWs may be playing a major bridging role in transmitting HIV and sexually transmitted infections (STIs) in Vietnam. An observed synergistic interaction between drug use and condom slippage/breakage emphasizes the importance of proper condom use, particularly among drug users.
Keywords: Sexual behaviors, Condoms, Bridging, Drug use, Male clients, Female sex workers (FSWs), Risk factors, Sexually transmitted infections (STIs), HIV
Introduction
The HIV/AIDS Sentinel Surveillance (HSS) was first established in Vietnam in 1994, and has demonstrated an increasing prevalence of HIV in female sex workers (FSWs). The HIV prevalence amongst FSWs was 0.57% in 1994, but increased 9-fold by the year 2006 to 4.14% (NIHE 2006). Concurrently, HIV prevalence among women attending antenatal clinics increased 19-fold, from 0.02% in 1994 to 0.38% in 2006 (NIHE 2006). In other studies, the prevalence of HIV infection among FSWs in Vietnam’s major cities was as high as 12% in Hanoi (Tran et al. 2005a) and 16.3% in Ho Chi Minh City (Nguyen et al. 2004). The FSW client population in Vietnam may play an important role in transmitting HIV from high-risk women (FSWs) to lower-risk women in the general population.
The Integrated Biological and Behavioral Surveillance (IBBS) in 2006 suggested that more than 90% of FSWs had used condoms during their last sexual encounter with both single-episode (“non-regular”) and regular clients. The proportion of consistent condom use varied from 56% to 90% with irregular clients, with a marked drop to 18–45% with regular sex partners (MOH/NIHE/FHI 2007). A study among FSWs in Hanoi revealed that consistent condom use in the past month was higher with irregular clients (62%), lower with regular clients (41%), and lowest with “love mates” (5%) (Tran et al. 2006). In addition to low consistent condom use, a significant proportion of FSWs in some areas were also drug users, 27% among high-class FSWs such as karaoke-based FSWs and 46% among low-class FSWs such as street-based FSWs (Tran et al. 2005b). Drug use places them at higher risk and amplifies that risk for their clients and the rest of society.
Approximately one-third of sexually active young Vietnamese men 15–29 years old (an estimated 1.5–3 million) have ever visited FSWs. Consistent condom use with irregular sex partners was 47.5% and 21.2% with regular sex partners (Duong et al. 2008). This implies that males who have sex with both high-risk women (defined as FSWs) and lower-risk women (defined as wives/girlfriends) and do not use condoms consistently may play a key role in spreading HIV to the general population (“bridging”).
Thus far, bridging behaviors among male clients of FSWs in Vietnam have not been adequately studied. Only one study targeted male clients of FSWs who were sampled from public sexually transmitted infection (STI) clinics, which represented the subgroup having unprotected sex with high-risk women (Thuy et al. 1999).
The goals of the study were to determine HIV/STI prevalence amongst different bridging groups, identify factors associated with being potential and active bridgers, and assess the association of drug use and unsafe sex with HIV and/or STI prevalence. We therefore investigated male clients of FSWs sampled from sex venues in Hai Phong city, a major international seaport in northern Vietnam that is actively undergoing rapid economic growth. FSWs have become established and are now numerous in this area. The Hai Phong–Do Son beach area is now famous for its inexpensive, young, beautiful FSWs. HIV prevalence amongst both FSWs and women attending antenatal clinics in this area has exceeded the average prevalence in Vietnam since 2002 (NIHE 2006).
Knowing the STI prevalence of FSWs’ clients is important. There is substantial biological evidence demonstrating that persons afflicted with STIs are more likely to both acquire and transmit HIV. Having an STI increases an individual’s susceptibility to HIV infection because genital ulcers (e.g., syphilis, herpes, or chancroids) allow entry of HIV and attract an increased number of cells that are targeted by HIV (i.e., CD4+ cells). Individuals who are infected with STIs are at least 2- to 5-fold more likely than uninfected individuals to acquire HIV through sexual contact (Wasserheit 1992). Additionally, having an STI increases a person’s infectiousness. A study conducted in Tanzania showed that individuals who were infected with both gonorrhea and HIV were more than twice as likely as those infected only with HIV to have detectable HIV genetic material in their genital secretions (Grosskurth et al. 1995). Therefore, we decided to include syphilis and herpes simplex type 2 (HSV-2), in addition to HIV, as outcomes of this study.
Methods
Subjects and Procedures
In April, 2007, 292 male clients visiting FSWs at sex venues in Hai Phong city and Do Son beach were interviewed in a cross-sectional survey, using two-stage time-location cluster sampling. In the first stage, peer educators (former or current FSWs or sex venue owners who live in the project target area and conduct outreach activities and group educational sessions for FSWs) and sex venue collaborators mapped sex venues in Do Son beach and the Thien Loi area of Hai Phong (a “red light district”), which is where more than 90% of local sex workers in Hai Phong city are located (Nguyen et al. 2005). Sex venues included places of entertainment, such as hotels, motels, guest houses, café bars, and karaoke bars, which have rental rooms available for FSWs and their clients. FSWs usually do not reside in these sex venues, and are often on-call and travel to the venues rapidly when requested. Since client numbers vary by time of day, the average number of male clients in each time slot (i.e., weekday nights, weekend afternoons, and weekend nights) was obtained. The sampling frame contained 216 time-location clusters in Do Son beach and 198 in the Thien Loi area. Thirty clusters in each area were selected with probability proportionate to average number of clients for each time slot at each venue, using C-survey software (Ariawan and Frerichs 1996).
In the second stage, five male clients were consecutively interviewed from the selected cluster, where they rented rooms for sexual encounters. A total of 146 clients in Do Son beach and 146 in the Thien Loi area participated. Inclusion criteria were men aged 18–60 years who had (within the past year) or were about to have sex with a FSW at a selected sex venue during the selected time slot, and were fluent in the Vietnamese language.
Male clients were initially asked by sex venue owners or pimps to participate. Clients expressing an interest were then taken to a rented interview room on-site and were screened for eligibility.
Of the 564 males visiting the selected sex venues in Thien Loi and Do Son beach, 464 (82.3%) were approached. Reasons for not being approached included sex venue owners not initially cooperating with the interview team, the client not being a Vietnamese nationale, or the person only requesting a room without being a FSW client. We excluded 49 clients who were not eligible and 25 clients who appeared to have come to the venue with the intention of participating in the study, leaving 292 eligible random clients. The proportion of eligibles approached who participated was 74.9% (71.6% in Do Son Beach and 78.5% in the Thien Loi area).
The interview team continued recruiting at each venue until completion of interviews with five clients, or returned another day to that venue at the same time slot to obtain a total of five subjects. The interview was administrated by a CD player and earphones in an anonymous manner, using a pre-tested structured questionnaire. Trained interviewers assisted clients in using the CD player and confirmed that they could use it properly. A corresponding answer sheet with no identifying information was designed for simplicity and ease of use by clients. It was checked for completeness by the interviewer (Liu et al. 1998). The intention of the study was to be completely anonymous; however, because interviewers were from the local area, there was a possibility that clients could be visually identified by the interviewers. However, interviewers were told to keep identities completely confidential if this situation occurred.
After the interview, 5 ml of venous blood was drawn, or if a client was unwilling to donate blood, oral fluid was tested for HIV. Each participant was compensated approximately $5 U.S. for the interview, and those also donating venous blood received an additional $5 U.S. In addition, participants received two coupons with their unique study identification numbers, one for a free STI examination and treatment if needed, and the other for receiving their test results and counseling at a local voluntary counseling and testing center (VCT). To assure anonymity, clients could only use their study codes to get their results. No names or addresses were recorded.
Laboratory Testing
The 5-ml venous blood specimens were drawn by a trained phlebotomist from each participant at the sex venues. Specimens were coded only by study identification numbers, and were transported weekly to the National Institute of Hygiene and Epidemiology (NIHE) in Hanoi for testing for HIV, syphilis, and HSV-2. HIV testing of clients who donated oral fluid instead was performed in the field using the Oraquick Advance Rapid HIV1/2 Antibody Test (Oral Sure Technologies, Inc.).
Utilizing strategy III for HIV testing according to WHO guidelines (WHO/GPA 1992), an ELISA test (Genscreen HIV ½ version 2, BioRad) was used, followed by a second ELISA (Murex HIV 1.2.0 of Abbott) and an agglutination test (SFD HIV½ of BioRad). Specimens positive for all three tests were classified as HIV-positive.
For HSV-2 testing, IgG antibodies to HSV-2 were detected using the HerpeSelect®2 ELISA (Focus Diagnostics, Cypress, CA).
Syphilis was tested for by repeated RPR (Rapid Plasma Reagin) and confirmed by TPHA (Treponemal Pallidum Hemaglutination Assay). Positive results from both tests confirmed positivity for syphilis. A RPR-positive but TPHA-negative result was considered indeterminate, and those with such results who returned to the VCT for their results were asked to be retested.
The study was approved by the UCLA Institutional Review Board (IRB) and the National Institute of Hygiene and Epidemiology (NIHE) Ethical Review Board.
Statistical Analysis
Data were double-entered and converted to STATA version 9.2 for analysis. Condom use with wives, girlfriends, and non-regular sex partners was gauged separately, using a Likert scale from 1 (not at all) to 5 (always), then they were dichotomized as “1” as “not always” and “0” as “always” for condom use with all three types of lower-risk sex partners (wife/girlfriend/casual sex partner). A non-regular sex partner was defined as a sex partner to whom the client was neither married nor cohabiting with at the time they had sex, and the client did not pay for having sex. If a client did not have a wife, girlfriend, or non-regular sex partner, they were assigned “0” for that type of partner. The bridging variable was created by compiling condom use with high-risk women (FSWs; always vs. not always) and low-risk women (always vs. not always), and classifying male clients into unlikely, potential, and active bridgers. Active bridgers had sex with both high- and lower-risk sex partners during the same time period and did not consistently use condoms with either type of partner, potential bridgers had sex with both high- and lower-risk sex partners during the same time period and always used condoms with high-risk sex partners but not with low-risk partners, and unlikely bridgers always used condoms with both groups or always used condoms with FSWs and had no lower-risk sex partners.
Logistic regression for survey design was used to assess the association of the bridging variable with outcome for HIV and/or syphilis, and adjusted for age, education, and income. Actual age was queried and categorized into 5 groups: less than 24 years, 25–34 years, 35–44 years, 45–54 years, and more than 55 years. Highest grade attained in school was asked and education categorized into 5 groups: graduated primary school, secondary school, high school, college or university, or higher than college. Income was categorized into 4 groups: average monthly income less than 1,000,000 VND; 1,000,000–2,000,000 VND; 2,000,000–3,000,000 VND; and more than 3,000,000 VND. Two million VND is the average monthly income for a government officer. Nominal logistic regression for survey design was used to estimate odds ratios of factors associated with being a potential or active bridger, in contrast to an unlikely bridger. Variables were selected into the multivariate model based on prior knowledge. If there was no prior knowledge, variables were selected depending on how much their presence/absence affected the confidence intervals of other variables in the model. A 10% cutoff was used, similar to that used in a study by Tran et al. (2006).
Results
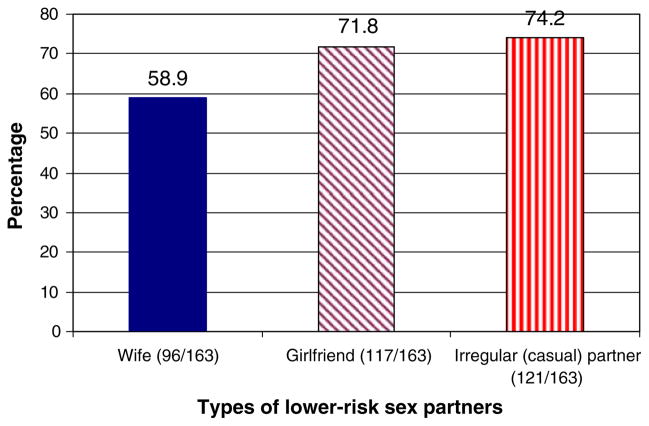
Of the 292 respondents, 147 were classified as potential bridgers (50.3%), 16 as active bridgers (5.5%), and 129 as unlikely bridgers (44.2%). Five clients who reported always using condoms with lower-risk sex partners but not always using condoms with FSWs were also classified as potential bridgers. Figure 1 shows that amongst 136 likely or active bridgers, 58.9% had a wife, 71.8% had a girlfriend(s), and 74.2% had casual sex partners. The majority (67.5%) of unlikely bridgers also had at least one type of lower-risk sex partner (wife/girlfriend/casual sex partner).
Fig. 1.
Classification of likely and active bridgers by types of lower-risk sex partners
Table 1 compares the characteristics of the three different bridging groups. Currently living with a wife or girlfriend and perceiving oneself to be at risk for becoming infected with HIV were the only significantly different characteristics between the three groups. Currently living with a wife/girlfriend was significantly more prevalent among potential and active bridgers than among unlikely bridgers (58.5% and 87.5%, respectively, vs. 38.1%; p = 0.007). Higher proportions of potential and active bridgers than unlikely bridgers perceived that they were at risk or at high risk for being infected with HIV (32.8% and 61.5%, respectively, vs. 24.8%; p = 0.056). Over one-third (38.5%) of the male clients who had unprotected sexual intercourse with high-risk women (FSWs) did not perceive themselves to be at risk for becoming infected with HIV. While there was no significant difference in HIV and syphilis prevalence among the three groups, HSV-2 seropositivity was significantly associated with risky bridging behaviors. Active and potential bridgers had a significantly higher prevalence of HSV-2 than unlikely bridgers (33.3% and 21.2%, respectively, vs. 8.77%; p = 0.043). There were no significant differences between the three bridging groups in terms of age, income, education, number of sex partners in the past month, number of sexual encounters in the past month, ever having used drugs, ever being tested for HIV, reporting STI signs/symptoms, etc.
Table 1.
Characteristics of different bridging groups, Hai Phong City, 2007
| Characteristics | Unlikely bridgers No (%) | Potential bridgers No (%) | Active bridgers No (%) | χ2 valueat valueb | p value |
|---|---|---|---|---|---|
| Number of respondents | 129 | 147 | 16 | ||
| Age | −1.24 | p1 0.212b | |||
| Mean (SD) | 30.2 (1.1) | 31.9 (0.8) | 32.8 (2.1) | −1.09 | p2 0.274b |
| Monthly income | |||||
| Mean | 3,309,908 | 5,245,891 | 3,637,500 | −0.696 | p1 0.48b |
| SD | 363,441 | 2,757,690 | 672,557 | −0.42 | p2 0.66b |
| Residence in HP city | |||||
| > 6 months | 112 (88.9%) | 124 (84.3%) | 14 (87.5%) | 1.66 | 0.437a |
| < 6 months | 14 (11.1%) | 23 (15.6%) | 2 (12.5%) | ||
| Currently living with wife/girlfriend | |||||
| Yes | 48 (38.1%) | 86 (58.5%) | 10 (62.5%) | 9.92 | 0.007a |
| No | 78 (61.9%) | 61 (41.5%) | 6 (37.5%) | ||
| Regular customer | |||||
| Yes | 68 (59.9%) | 83 (56.1%) | 8 (50%) | 0.283 | 0.868a |
| No | 58 (46%) | 65 (43.9%) | 8 (50%) | ||
| Number of sexual partners in the past month | |||||
| > 5 partners | 22 (17.5%) | 35 (23.6%) | 5 (31.3%) | 2.93 | 0.231a |
| ≤5 partners | 104 (82.5%) | 113 (76.4%) | 11 (68.7%) | ||
| Number of sexual encounters in the past month | 0.306 | p1 0.75b | |||
| Mean (SD) | 11.1 (1.1) | 10.7 (0.7) | 13.9 (2.5) | −1.025 | p2 0.31b |
| Number of sexual encounters with FSWs in the past month | |||||
| > 4 times | 34 (27%) | 42 (28.4%) | 5 (31.3%) | 0.288 | 0.866a |
| ≤4 times | 92 (73%) | 106 (71.6%) | 11 (68.7%) | ||
| Consumed alcohol before last sexual intercourse with FSW | |||||
| Yes | 89 (70.6%) | 100 (68.5%) | 12 (75%) | 0.365 | 0.833a |
| No | 37 (29.4%) | 46 (31.5%) | 4 (25%) | ||
| Had ever used drugs (heroin, ecstasy, marijuana, etc.) | |||||
| Yes | 17 (13.5%) | 19 (12.9%) | 3 (18.7%) | 0.419 | 0.811a |
| No | 109 (86.5%) | 128 (87%) | 13 (81.3%) | ||
| Used drugs before last sexual intercourse with FSW | |||||
| Yes | 8 (50%) | 10 (32.6%) | 2 (66.7%) | 0.281 | 0.869a |
| No | 8 (50%) | 9 (47.4%) | 1 (33.3%) | ||
| Ever tested for HIV | |||||
| No | 92 (73.1%) | 104 (70.7%) | 12 (75%) | 0.249 | 0.883a |
| Yes | 34 (26.9%) | 43 (29.3%) | 4 (25%) | ||
| Reported at least one sign(s)/symptom(s) of STIs in the past 12 months | |||||
| Yes | 30 (23.8%) | 31 (20.9%) | 3 (18.8%) | 2.25 | 0.325a |
| No | 96 (76.2%) | 117 (79.1%) | 13 (81.2%) | ||
| Reported at least one sign(s)/symptom(s) of STIs in the past month | |||||
| Yes | 21 (16.7%) | 31 (20.9%) | 3 (18.8%) | 1.34 | 0.513a |
| No | 105 (83.3%) | 125 (84.5%) | 13 (81.2%) | ||
| Reported condom breakage/slippage in the past month | |||||
| Yes | 28 (22.2%) | 39 (26.4%) | 6 (37.5%) | 2.32 | 0.314a |
| No | 98 (77.8%) | 109 (73.6%) | 10 (62.5%) | ||
| Perceived risk of becoming infected with HIV | |||||
| > 4, at risk or high risk | 31 (24.8%) | 48 (32.8%) | 8 (61.5%) | 5.77 | 0.056a |
| ≤ 3, average or low risk | 94 (75.2%) | 98 (67.2%) | 5 (38.5%) | ||
| HIV prevalence | |||||
| Prevalence | 4.76% | 4.05% | 6.25% | 0.206 | 0.902a |
| 95% CI | 0.29–9.23% | 1.0–7.1% | 0–18.6% | ||
| Syphilis prevalence | |||||
| Prevalence | 1.58% | 1.35% | 0% | 0.269 | 0.874a |
| 95% CI | 0–3.77% | 0–3.23% | 0 | ||
| HSV-2 prevalence | |||||
| Prevalence | 8.77% | 21.16% | 33.33% | 6.29 | 0.043a |
| 95% CI | 3.71–13.83% | 12.96–29.36% | 10.1–56.5% | ||
Note: Totals do not add to 100% for some variables due to missing values
Chi square test
t-test obtaining p<0.05, compared means of potential bridgers vs. unlikely bridgers (p1) and active bridgers vs. unlikely bridgers (p2) Estimates of prevalence and SD for cluster survey design
Unadjusted associations of different factors with bridging behaviors are presented in Table 2. Potential bridgers were 2.32-fold more likely than unlikely bridgers to be currently living with a wife/girlfriend (95% CI 1.29–4.16). Believing condom use is not necessary when having sex with wives/girlfriends was 1.7-fold more frequent among potential bridgers (95% CI 1.05–2.74) and 3.45-fold more frequent among active bridgers (95% CI 1.17–10.14) compared to unlikely bridgers. Not believing that condoms are effective in preventing HIV/STIs was significantly associated with potential bridging behaviors (OR = 1.88, 95% CI 1.05–3.36). Perceived risk of oneself becoming infected with HIV was more frequent among potential (OR = 1.18, 95% CI 1.02–1.37) and active (OR = 1.36, 95% CI 0.98–1.87) bridgers.
Table 2.
Unadjusted odd ratios (UORs) of bridging behaviors among potential and active bridgers vs. unlikely bridgers
| Associated factors | Potential bridgers UOR (95% CI) | Active bridgers UOR (95% CI) |
|---|---|---|
| Regular customer of the sex venue | ||
| Yes vs. no | 1.09 (0.65–1.81) | 0.85 (0.34–2.1) |
| p-value | 0.739 | 0.725 |
| Currently living with wife/girlfriend | ||
| Yes vs. no | 2.32 (1.29–4.16) | 2.77 (0.77–10.0) |
| p-value | 0.005 | 0.117 |
| Number of sex partners in the past month | ||
| > 5 partners vs. ≤5 partners | 1.46 (0.78–2.74) | 2.1 (0.59–7.8) |
| p-value | 0.230 | 0.24 |
| Number of sex encounters with FSWs in the past month | ||
| ≥4 times vs. < 4 times | 0.99 (0.93–1.05) | 1.04 (0.95–1.14) |
| p-value | 0.832 | 0.330 |
| Had ever used drugs (heroin, ecstasy, marijuana, etc.) | ||
| Yes vs. no | 0.95 (0.48–1.86) | 1.47 (0.39–5.57) |
| p-value | 0.883 | 0.557 |
| Ever tested for HIV | ||
| No vs. yes | 0.89 (0.51–1.56) | 1.1 (0.33–3.7) |
| p-value | 0.689 | 0.866 |
| Reported at least one sign(s)/symptom(s) of STIs | ||
| Past 12 months | ||
| Yes vs. no | 0.84 (0.67–1.04) | 0.95 (0.6–1.5) |
| p-value | 0.116 | 0.84 |
| Past month | ||
| Yes vs. no | 0.96 (0.73–1.27) | 1.18 (0.78–1.78) |
| p-value | 0.789 | 1.03 |
| Reported condom breakage/slippage in the past month | ||
| Yes vs. no | 1.25 (0.71–2.19) | 2.1 (0.57–7.67) |
| p-value | 0.427 | 0.256 |
| Believed condom use is NOT necessary when having sex with wife/girlfriend | ||
| Yes vs. no | 1.7 (1.05–2.74) | 3.45 (1.17–10.14) |
| p-value | 0.029 | 0.025 |
| Don’t believe in effectiveness of condoms for STI prevention | ||
| Yes vs. low or average | 1.88 (1.05–3.36) | 1.05 (0.22–4.9) |
| p-value | 0.033 | 0.943 |
| Perceived risk of becoming infected with HIV | ||
| Increase from 1 to 5 (1 = low to 5 = high risk) | 1.18 (1.02–1.37) | 1.36 (0.98–1.87) |
| p-value | 0.027 | 0.062 |
95% CI, 95% confidence interval. 95% CI adjusted for cluster survey using nominal logistic regression, comparison group was unlikely bridgers
The five STI sign/symptoms are abnormal discharge, pain during urination, ulcer on the penis, itching of the penis, other abnormalities of the penis
UOR, unadjusted odds ratio
Table 3 shows the final optimal multivariate regression model based on the best fit model, which included the minimal number of explanatory variables in the model. Age, income, and education were considered potential confounders, and were included in the model based on prior knowledge, since that would affect condom use behavior but would not be affected by currently living with a wife/girlfriend, not believing in the necessity of condom use, and own perceived risk of becoming infected with HIV. After adjustment, living with a wife/girlfriend, believing in the necessity of condom use when having sex with a wife/girlfriend, and own perceived risk of being infected with HIV were statistically significantly associated with bridging behaviors. Compared to unlikely bridgers, currently living with a wife/girlfriend was 2.56-fold (95% CI 1.39–4.6) more frequent among potential bridgers and 1.52-fold among active bridgers. Not believing in the necessity of using condoms when having sexual intercourse with a wife/girlfriend was 1.78-fold (95% CI 1.05–3.03) more frequent among potential bridgers and 4.34-fold (95% CI 1.35–14.28) among active bridgers. Perceiving one’s own risk for being infected with HIV was 1.4-fold more frequent among active bridgers (95% CI 1.02–1.9) than among unlikely bridgers.
Table 3.
Adjusted odd ratios (AORs) of factors associated with being a potential or active bridger compared to being an unlikely bridger in Hai Phong city, 2007
| Associated factors | Potential bridgers AOR (95% CI) | Active bridgers AOR (95% CI) |
|---|---|---|
| Currently living with wife/girlfriend | ||
| Yes vs. no | 2.56 (1.39–4.6) | 1.52 (0.30–8.33) |
| p-value | 0.003 | 0.595 |
| Believed that condom use is NOT necessary when having sex with wife/girlfriend | ||
| Yes vs. no | 1.78 (1.05–3.03) | 4.34 (1.35–14.28) |
| p-value | 0.031 | 0.015 |
| Perceived risk of becoming infected with HIV | ||
| Increase from 1 to 5 (1 = low to 5 = high risk) | 1.14 (0.97–1.35) | 1.4 (1.02–1.9) |
| p-value | 0.09 | 0.036 |
95% CI, 95% confidence interval
95% CI adjusted for cluster survey using nominal logistic regression, comparison group was unlikely bridgers
AORs, adjusted odds ratios for age, education, income, and other variables in the model
Because the percentage of respondents reporting always using condoms with FSWs was very high (94.5%), the variable itself was not associated with the outcome of HIV and/or syphilis seropositivity (OR ≈ 1, 95% CI was wide and included one), but condom breakage/slippage became a strong predictor for HIV and/or syphilis seropositivity. Condom breakage/slippage results in unintentional unprotected sex. Although male clients might always use condoms with FSWs (potential or unlikely bridgers), breakage/slippage placed them at risk for being infected with HIV and/or syphilis; an unprotected sex variable was created as an indicator for bridging behavior by combining those who did not always use a condom with FSWs plus those who experienced condom breakage/slippage. Table 4 shows the single and joint associations of unprotected sex upon the likelihood of being HIV- and/or syphilis-seropositive. The purpose of this analysis was to determine the extent to which drug use, having unprotected sex (the majority due to condom misuse/defects), or both were associated with being HIV/syphilis-seropositive, whether there was an interaction association between the two factors, and the single association of each factor. The reference group had never used drugs nor had unprotected sex. The association alone of having ever used drugs was compared between the group having used drugs but not having unprotected sex and the reference group. Similarly, the association alone of having unprotected sex was calculated by comparing the association between the group that had unprotected sex but had not used drugs and the reference group. The joint association was obtained by comparing the group that had both used drugs and had unprotected sex vs. the reference group. The associations were adjusted for clients’ age, income, and education as potential confounders by prior knowledge. Confidence intervals were adjusted for the design effect required for cluster survey analysis.
Table 4.
Combined contributions of unprotected sex in the past month and drug use with being HIV/syphilis-seropositive
| AORs | Unprotected sex (intentional and unintentional) |
||
|---|---|---|---|
| Yes | No | ||
| Ever used drugs | Yes | AOR11 = 14.4 (95% CI 3.9–53.3) | AOR01 = 5.2 (95% CI 1.8–15.7) |
| No | AOR10 = 2.8 (95% CI 1.2–6.3) | AOR00 = 1 | |
AOR, adjusted odds ratio
Adjusted for age, education, and income
Drug use alone increased the likelihood of being HIV- and/or syphilis-seropositive 5.2-fold (95% CI 1.8–15.7), while having unprotected sex alone increased the likelihood of being HIV- and/or syphilis-seropositive 2.8-fold (95% CI 1.2–6.3). The joint adjusted odds ratio was 14.4 (95% CI 3.9–53.3) higher than the additive of the two (5.2 + 2.8 − 1). Assuming that the prevalence of HIV and/or syphilis is low (e.g., less than 5%), the assumption can be made that the odds ratios ≈ risk ratios (ORs ≈ RRs) can therefore be tested for additivity (Rothman and Greenland 1998a).
Discussion
This study classified bridging into three different bridging groups: unlikely, potential, and active. Potential and active bridgers comprised 55.8% of the total male client sample. Clearly, a significant proportion of clients of sex workers in Hai Phong were bridgers who put their lower-risk sex partners at risk for infection with HIV and STIs, leading to transmission of STIs, including HIV, to low-risk groups of women. Table 1 shows that 26.4% of potential bridgers experienced condom breakage/slippage; therefore, they were considered active bridgers. Of the estimated 1.5–3 million young sexually active Vietnamese men aged 15–24 years who have visited FSWs, 837,000–1,670,000 men are estimated to be potential or active bridgers, assuming our study population was representative of all male clients in Vietnam. Considering the average of 4.6 sexual partners in the past month (95% CI 3.8–5.5) (data not shown) and using the lower estimate of 837,000 men visiting FSWs, as many as 3,850,200 women in Vietnam would be placed at risk for being infected with HIV/STIs (95% CI 3,180,600–4,603,500). Using the higher estimate of 1,670,000 male clients, the number of women at risk might be 7,682,000 (95% CI 6,346,000–9,185,000).
Several factors were associated with being a “bridger”. Bridgers were more likely to be currently living with regular partners such as a wife or girlfriend and to be infected with HSV-2. Although awareness and perception of one’s own risk for HIV/STIs was high among active bridgers and higher still amongst potential bridgers, they still engaged in unsafe sexual behaviors. The multivariate logistic regression model revealed that NOT believing in the necessity of using condoms when having sexual intercourse with a wife/girlfriend was significantly associated with being a potential or active bridger (1.78- and 4.34-fold, respectively). Thus, current condom promotion campaigns are clearly inadequate in reaching the men most likely to transmit disease.
Our definitions of bridging groups differed from those used by other researchers. In a study in Cambodia, Gorbach et al. (2000) had a similar definition of active bridgers, but defined potential bridgers as men who always used condoms with all high-risk partners or with all low-risk partners or with both, but did have sex with both types of partners during the same 3-month period. A U.S. study of STI patients practicing bridging behavior indicated that active bridgers were persons infected with an STI, and potential bridgers were persons not infected with an STI (Aral et al. 1999; Gorbach et al. 2000). Tabet et al. (2002) defined bridgers as men who had sex with both men and women in the past year, and Jennings et al. (2007) defined an age-bridger as a person who, within 2 months, had had at least two sexual partners who differed from him in age by 2 years or more. Definitions of bridging varied by time frame, target population, and purpose of analysis. Our study targeted male clients of FSWs. For public health purposes, classifying a male client who has no lower-risk sex partner but visits FSWs as an unlikely bridger is appropriate.
HSV-2 prevalence was significantly increased among active and potential bridgers compared to unlikely bridgers (33.3% and 21.16%, respectively, vs. 8.77%; p = 0.043), and higher among active than potential bridgers. Less consistent condom use and having more sex partners might be reasons for the significant pattern of increasing HSV-2 prevalence among them. HSV-2 increases the probability of acquiring HIV infection. A nested case-control study in Tanzania documented that HSV-2 infection increased risk for acquisition of HIV 6-fold (95% CI 2.5–14.9) among participants who were HSV-2-infected at baseline, and 16.8-fold (95% CI 6–46) if subjects had acquired HSV-2 during the study (del Mar Pujades Rodriguez et al. 2002). Lama et al. (2006) reported that HSV-2 seropositivity was associated with 5.6-fold higher prevalence of HIV infection in a survey among men who have sex with men. The population attributable risk percent for HIV acquisition due to prevalent and incident HSV-2 infection was 42% among women in Uganda and 65% in Zimbabwe (Brown et al. 2007). In our study, HIV prevalence amongst HSV-2-seropositive subjects was 12.8%, while HIV prevalence among HSV-2-negative clients was only 3.7% (OR = 4.4, 95% CI 1.1–17.1). Thus, active and potential bridgers were more likely to be HSV-2-positive, and according to our data, over 4-fold more likely to be HIV-positive, and thus more likely to transmit HIV.
We believe that the time-space-venue and two-stage PPS cluster sampling survey produced a representative sample of male clients in Hai Phong city. Behavioral data were obtained by a survey administered by CD player/earphones in an anonymous manner, which would be more likely to elicit valid information about sexual and drug use behaviors (Liu et al. 1998). Thus, the study results may be more representative of the male client population that visits direct FSWs in Hai Phong city, and might be applied to other similar big cities in Vietnam than studies using interviewer-administered strategies.
Table 2 indicates that unlikely bridgers had 4.76%, 1.58%, and 8.77% prevalence of HIV, syphilis, and HSV-2, respectively. There are several reasons why unlikely bridgers became infected. First, the question about consistent condom use was asked for a life-time frame (ever); however, clients might not have remembered their life-long sexual practices and only answered according to their current condom use behaviors, leading to misclassification of clients into different bridging groups. Current unlikely clients might have been infected with HIV/syphilis in the past when they engaged in unprotected sex. The questionnaire was designed with the intention of keeping the questions short; therefore, the more precise tool of quantifying condom use behavior was not used. Another explanation could be that condom slippage/breakage caused unlikely bridgers to become infected (22.2% of 129 unlikely bridgers reported experiencing condom breakage/slippage). Furthermore, clients could have become infected with HIV via another route, such as sharing needles and syringes if they were injection drug users. Seventeen of the 129 unlikely bridgers admitted to ever using drugs; of these, 5/17(29.4%) were HIV-positive.
The problem of reporting bias cannot be completely eliminated, even though a CD player/earphone strategy was used to administer the questionnaire. The data suggest there was no significant difference in HIV and syphilis seroprevalence among the three groups, while there was a significant difference in HSV-2 prevalence among the three. Our data did not support any reasonable explanation for this lack of observed difference. It might be due to the small sample size of the study that could not detect the significant differences of a low prevalence (<5%); a cross-sectional survey cannot identify clients with long vs. short duration of practicing unsafe sex leading to seroconversion. Another explanation could be that the observed significant difference of HSV-2 prevalence but not prevalence of HIV and syphilis among the three groups reflects the greater transmissibility of HSV-2 compared to HIV and syphilis. However, our study also has the usual limitations of cross-sectional studies.
The study suggests that intervention strategies are needed to overcome the observed lack of association between knowledge and action. The discrepancy of always using condoms among different types of sexual partners indicates that condom use has been accepted and implemented with commercial sexual partners much more than with regular and casual sex partners. This discrepancy is similar to that found in a study of sexual bridging by Cambodian men (Gorbach et al. 2000) and a study on sexual risks and bridging behaviors among young people in Hai Phong, Vietnam (Duong et al. 2008).
Although 94.5% of the sampled male clients reported always using condoms with FSWs, 24.8% experienced condom breakage/slippage, suggesting that condom use was less effective with FSWs due to either improper use or the poor quality of condoms, which could cause potential and unlikely bridgers to become active bridgers. Our study suggests that drug users are more likely to use condoms improperly, presenting a particularly high risk to their partners. Thus, condom promotion needs to target drug users, especially with messages about proper condom use. Instruction of proper condom use should be an essential component of drug substitution treatment and needle exchange programs, as well as other intervention programs targeting drug users.
Study Limitations
The study might have had potential selection bias due to the relatively high proportion of refusals (participation proportion was 74.8%). Male clients who served in the military or police, who were married, or who had higher income were more likely to refuse participation. In addition, the study might not have recruited clients who went to sex venues at 1–2 a.m. or later, because the quota of five clients per venue was usually met before midnight. Seven selected time-space clusters did not allow us to conduct our study at their venues, so we substituted the nearest cooperative venues with similar estimated numbers of clients. Therefore, selection biases might have occurred, because bridging behaviors might have been different among clients at cooperating venues than clients at non-cooperating venues or who were not approached.
The study is subject to social desirability bias, resulting in over-reporting of condom use. Although 94.5% reported having always used condoms with FSWs, when asked if they had used a condom with a FSW during their last sexual encounter, only 84.9% reported doing so (95% CI 79.5–90.2). If there was similar over-reporting of condom use with wives/girlfriends, the study would be subject to misclassification of bridging groups. A significant proportion of male clients who reported not engaging in bridging behaviors might actually be active bridgers. Unfortunately there was no way to validate the variable of always using condoms with wives/girlfriends. This bias, however, would reduce the probability of observing a difference, and was therefore a conservative bias (Rothman and Greenland 1998b). This classification is based on the assumption that wives, girlfriends, and irregular sexual partners are actually lower-risk sex partners. However, the conclusions might differ if these women or a proportion of them were actually at higher risk due to injection drug use or had sexual intercourse with others in addition to their sexual encounters with the male participants of this study.
Self-perceived risk of becoming infected with HIV/STIs was significantly different between the three groups, and was 1.4-fold more common among active bridgers. However, because this was a cross-sectional design, we cannot determine whether male clients who perceived that they were at high risk for HIV infection did so because of their active bridging behavior, or that since they perceived that they were already at high risk for HIV infection (such as drug injection, etc.), they disregard the dangers of unsafe sex.
The implication of an observed synergistic relationship between condom breakage/slippage and ever having used drugs might not have been applicable for other settings having a higher prevalence of HIV and/or syphilis (e.g., 5%), because the assumption required to assume OR ≈ RR was not met.
Conclusions
Almost 60% of male clients of sex workers in Hai Phong may be transmitting HIV and/or STIs to their non-commercial sex partners. A high proportion of clients were infected with HSV-2, which increases the risk of acquiring HIV and subsequently transmitting it to their low-risk partners. Their attitudes about condom use emphasize that current intervention methods are ineffective. Thus, there is a need for more effective condom promotion activities to reach this group of probable core transmitting bridgers. The observed synergistic interaction between condom slippage/breakage and drug use emphasizes the need for condom promotion and education campaigns that target drug users, especially with messages about proper condom use. Instruction about proper condom use should be an essential component of drug substitution treatment and needle and syringe exchange programs, as well as other intervention programs for drug users. In addition, the quality of condoms should be strictly controlled to minimize condom breakage.
Acknowledgments
This study was funded by a grant from the National Institute of Health/Fogarty International Center (D43 TW000013). We especially thank Drs. Ralph Frerichs, Donald Morisky, and Pamina Gorbach, who reviewed manuscript and provided thoughtful suggestions and relevant literature. Special thanks to Family Health International colleagues for advice and support for the conduct of the study. We are grateful to the research team members and staff of the Vietnam Administration of Preventive Medicine of the Ministry of Health, Hai Phong Health Services, the Hai Phong HIV/AIDS Prevention Center, the Hoa Phuong Club, and the World Vision project in Hai Phong for their contributions to the success of the study. Sincere thanks to Dr. Tran Quang Vinh for field work organization, and to Wendy Aft for assistance in preparing this manuscript.
Contributor Information
Nhu T. Nguyen, Family Health International, Vietnam Country Office, Hanoi, Vietnam
Hien T. Nguyen, National Institute of Hygiene and Epidemiology, Hanoi, Vietnam
Huan Q. Trinh, Ministry of Health, Hanoi, Vietnam
Stephen J. Mills, Family Health International, Vietnam Country Office, Hanoi, Vietnam
Roger Detels, Email: Detels@ucla.edu, Department of Epidemiology, UCLA School of Public Health, 71-269 CHS, Los Angeles, CA 90095-1772, USA.
References
- Aral SO, Hughes JP, Stoner B, Whittington W, Handsfield HH, Anderson RM, et al. Sexual mixing patterns in the spread of gonococcal and chlamydial infections. American Journal of Public Health. 1999;89(6):825–833. doi: 10.2105/ajph.89.6.825. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ariawan I, Frerichs RR. CSurvey 1.5. A cluster sampling utility program for IBM-compatible microcomputers. Los Angeles, CA: University of Calfornia; 1996. [Google Scholar]
- Brown JM, Wald A, Hubbard A, Rungruengthanakit K, Chipato T, Rugpao S, et al. Incident and prevalent herpes simplex virus type 2 infection increases risk of HIV acquisition among women in Uganda and Zimbabwe. AIDS (London, England) 2007;21(12):1515–1523. doi: 10.1097/QAD.0b013e3282004929. [DOI] [PubMed] [Google Scholar]
- del Mar Pujades Rodriguez M, Obasi A, Mosha F, Todd J, Brown D, Changalucha J, et al. Herpes simplex virus type 2 infection increases HIV incidence: A prospective study in rural Tanzania. AIDS (London, England) 2002;16(3):451–462. doi: 10.1097/00002030-200202150-00018. [DOI] [PubMed] [Google Scholar]
- Duong CT, Nguyen TH, Hoang TT, Nguyen VV, Do TM, Pham VH, et al. Sexual risk and bridging behaviors among young people in Hai Phong, Vietnam. AIDS and Behavior. 2008;2(4):643–651. doi: 10.1007/s10461-007-9265-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gorbach PM, Sopheab H, Phalla T, Leng HB, Mills S, Bennett A, et al. Sexual bridging by Cambodian men: Potential importance for general population spread of STD and HIV epidemics. Sexually Transmitted Diseases. 2000;27(6):320–326. doi: 10.1097/00007435-200007000-00004. [DOI] [PubMed] [Google Scholar]
- Grosskurth H, Mosha F, Todd J, Mwijarubi E, Klokke A, Senkoro K, et al. Impact of improved treatment of sexually transmitted diseases on HIV infection in rural Tanzania: Randomised controlled trial. Lancet. 1995;346(8974):530–536. doi: 10.1016/S0140-6736(95)91380-7. [DOI] [PubMed] [Google Scholar]
- Jennings JM, Luo RF, Lloyd LV, Gaydos C, Ellen JM, Rietmeijer CA. Age-bridging among young, urban, heterosexual males with asymptomatic Chlamydia trachomatis. Sexually Transmitted Infections. 2007;83(2):136–141. doi: 10.1136/sti.2006.023556. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lama JR, Lucchetti A, Suarez L, Laguna-Torres VA, Guanira JV, Pun M, et al. Association of herpes simplex virus type 2 infection and syphilis with human immunodeficiency virus infection among men who have sex with men in Peru. The Journal of Infectious Diseases. 2006;194(10):1459–1466. doi: 10.1086/508548. [DOI] [PubMed] [Google Scholar]
- Liu H, Xie J, Yu W, Song W, Gao Z, Ma Z, et al. A study of sexual behavior among rural residents of China. Journal of Acquired Immune Deficiency Syndromes and Human Retrovirology. 1998;19(1):80–88. doi: 10.1097/00042560-199809010-00013. [DOI] [PubMed] [Google Scholar]
- Ministry of Health/National Institute of Hygiene and Epidemiology/Family Health International. Results from the HIV/STI Integrated Biological and Behavioral Surveillance (IBBS) in Vietnam, 2005–2006. Hanoi, Vietnam: Ministry of Health/National Institute of Hygiene and Epidemiology/Family Health International; 2007. [Google Scholar]
- National Institute of Hygiene and Epidemiology (NIHE) HIV/AIDS Sentinel Surveillance Data Report, 1994 to 2006. Hanoi, Vietnam: NIHE; 2006. [Google Scholar]
- Nguyen AT, Nguyen TH, Pham KC, Le TG, Bui DT, Hoang TL, et al. Intravenous drug use among street-based sex workers: A high-risk behavior for HIV transmission. Sexually Transmitted Diseases. 2004;31(1):15–19. doi: 10.1097/01.OLQ.0000105002.34902.B5. [DOI] [PubMed] [Google Scholar]
- Nguyen AT, Vu DTB, Nguyen DD. Report coverage and reaching survey among female sex workers and injecting drug users in Hai Phong, Vietnam. Hanoi, Vietnam: Family Health International; 2005. [Google Scholar]
- Rothman KJ, Greenland S. Modern epidemiology. New York: Lippincott Williams and Wilkins; 1998a. Concepts of interaction; pp. 341–342. [Google Scholar]
- Rothman KJ, Greenland S. Modern epidemiology. New York: Lippincott Williams and Wilkins; 1998b. Precision and validity in epidemiologic studies; p. 127. [Google Scholar]
- Tabet S, Sanchez J, Lama J, Goicochea P, Campos P, Rouillon M, et al. HIV, syphilis and heterosexual bridging among Peruvian men who have sex with men. AIDS (London, England) 2002;16(9):1271–1277. doi: 10.1097/00002030-200206140-00010. [DOI] [PubMed] [Google Scholar]
- Thuy NT, Lindan CP, Phong TH, Van Dat T, Nhung VT, Barclay J, et al. Predictors of visits to commercial sex workers by male attendees at sexually transmitted disease clinics in southern Vietnam. AIDS (London, England) 1999;13(6):719–725. doi: 10.1097/00002030-199904160-00013. [DOI] [PubMed] [Google Scholar]
- Tran TN, Detels R, Lan HP. Condom use and its correlates among female sex workers in Hanoi, Vietnam. AIDS and Behavior. 2006;10(2):159–167. doi: 10.1007/s10461-005-9061-7. [DOI] [PubMed] [Google Scholar]
- Tran TN, Detels R, Long HT, Lan HP. Drug use among female sex workers in Hanoi, Vietnam. Addiction (Abingdon, England) 2005a;100(5):619–625. doi: 10.1111/j.1360-0443.2005.01055.x. [DOI] [PubMed] [Google Scholar]
- Tran TN, Detels R, Long HT, Van Phung L, Lan HP. HIV infection and risk characteristics among female sex workers in Hanoi, Vietnam. Journal of Acquired Immune Deficiency Syndromes and Human Retrovirology. 2005b;39(5):581–586. [PMC free article] [PubMed] [Google Scholar]
- Wasserheit JN. Epidemiological synergy. Interrelationships between human immunodeficiency virus infection and other sexually transmitted diseases. Sexually Transmitted Diseases. 1992;19(2):61–77. [PubMed] [Google Scholar]
- World Health Organization/Global Programme on AIDS. Acquired immunodeficiency syndrome (chapter 24) [Accessed March 2008.];Blood safety and clinical technology: Guidelines on standard operating procedures for microbiology. 1992 http://www.searo.who.int/en/Section10/Section17/Section53/Section482_1809.htm.