Abstract
Introduction
Little is known about the natural history of malignant solitary pulmonary nodules (SPN). Experts’ beliefs may help fill these knowledge gaps and explain variation in clinical practices.
Methods
Using a modified Delphi process, we surveyed a group of lung cancer experts about tumor growth, disease progression and prognosis in patients with malignant SPN. After completing the first survey, experts were given the opportunity during a second survey to revise their responses in light of their peers’ beliefs.
Results
The response rate was 100% (14/14) for both surveys. There was consensus that disease progression depends on the tumor growth rate, that survival for patients with untreated lung cancer is approximated by a declining exponential function, and that treatment is delayed by approximately 1 tumor volume doubling time (TVDT) in patients who undergo a period of “watchful waiting”. Just over half of experts (8/14) agreed that lung cancer progresses in 3steps (from local to regional to distant disease), while 43% (6/14) preferred a 2-step model (from local to systemic disease). Likewise, 64% of experts (9/14) believed that malignant nodules grow exponentially, while 36% (5/14) believed that growth is slower than exponential. Experts’ estimates of the risk of disease progression during a period of observation lasting 1 TVDT varied from 1% to 50%. Estimates of 5-year survival for patients in whom diagnosis and treatment were delayed by 1 TVDT varied between 40% and 80%.
Conclusions
There is substantial variability in experts’ beliefs about the natural history of untreated, malignant SPN. Different beliefs may be partly responsible for variation in management practices.
Keywords: Lung Neoplasms, Coin lesion, pulmonary, Delphi technique, survival, disease progression, tumor growth
INTRODUCTION
The solitary pulmonary nodule (SPN) is a common and challenging clinical problem. Although evidence-based guidelines and decision analytic models have been developed to help guide clinical decisions about diagnosis and treatment of patients with SPN, these tools are limited by gaps in our current knowledge about the natural history of lung cancer.1, 2 Little is known about the natural history of untreated, malignant lung nodules. More specifically, we know little about the risk of disease progression during a period of diagnostic delay or planned observation. This limits clinicians’ ability to counsel patients about the risks associated with a strategy of “watchful waiting”. In the absence of empirical data, experts’ beliefs may be useful to clinicians and developers of decision aids by filling some knowledge gaps.
The Delphi method was developed in the 1950’s by the RAND Corporation to elicit reliable consensus opinion among a group of experts.3 The technique has been adapted in numerous ways, but centers around repeated questioning of experts, usually in the form of a survey or individual interviews, with feedback on peer responses or thought processes provided between rounds of questioning. The method aims to promote individual thinking by avoiding confrontation between experts, while guiding opinion towards a consensus. The Delphi method has been used to elicit expert consensus about a wide variety of medical topics, 4, 5 including management of spontaneous pneumothorax.6
In this study, we employed a modified Delphi technique to evaluate expert agreement with assumptions about the natural history of lung cancer, and to measure experts’ beliefs about tumor growth, disease progression and survival in patients with a malignant SPN.
METHODS
We invited leaders from the Thoracic Oncology Network of the American College of Chest Physicians (ACCP) to participate in an expert panel. Follow-up emails were sent to experts who did not respond to the initial invitation. This study was approved by the Institutional Review Board of Stanford University. All participants provided informed consent.
Survey
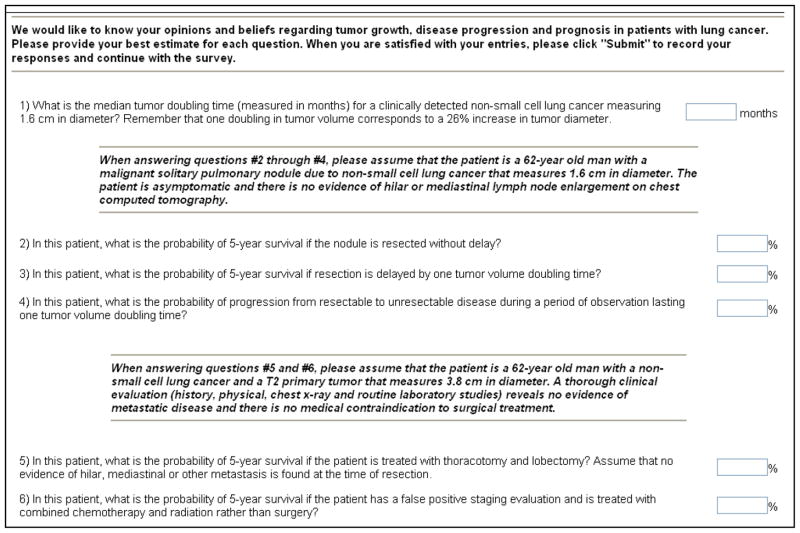
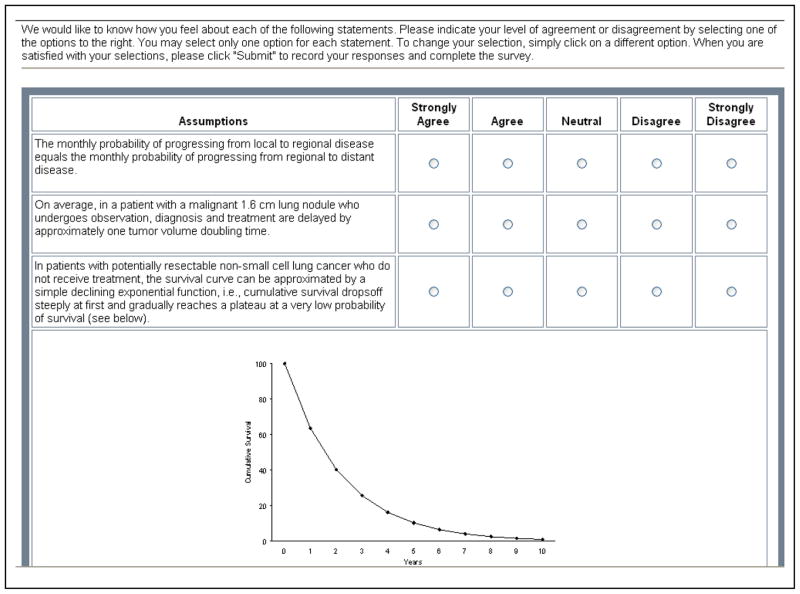
We measured experts’ beliefs about malignant SPN through two rounds of an on-line survey (Appendix). In the first round, we asked experts to provide estimates of median tumor volume doubling times (TVDT), rates of progression from resectable to unresectable disease, and 5-year survival for hypothetical patients with malignant nodules. We also asked experts to indicate their level of agreement with assumptions about tumor growth rates, disease progression and survival by using a 5 -point Likert scale. We developed survey items based on assumptions from a natural history model of lung cancer.7, 8 We emphasize that the survey was designed to measure beliefs, not to test knowledge.
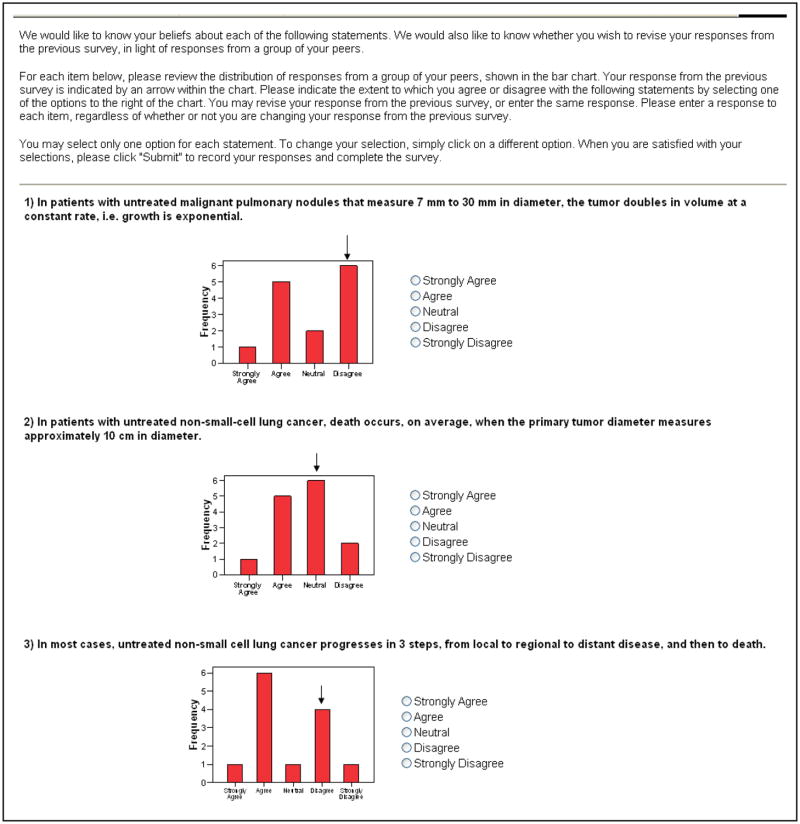
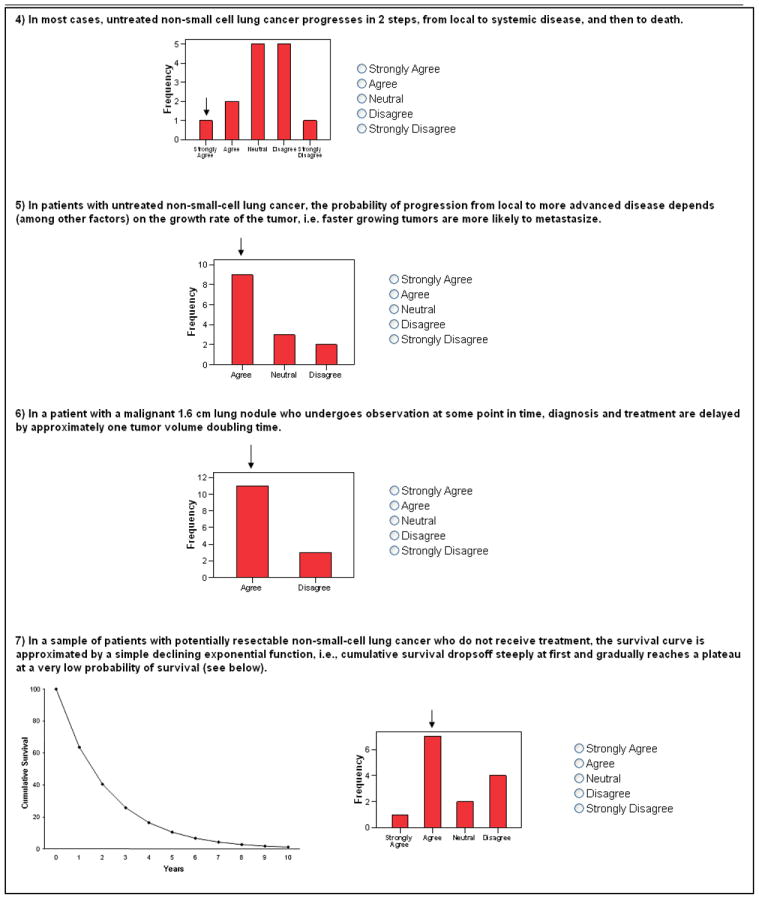
In the second round of the survey, we again asked experts to indicate their agreement with the assumptions, this time while considering their peers’ responses from the previous round. Adjacent to each item, we embedded a bar chart depicting the distribution of first-round responses and an arrow indicating where the participant’s previous response fell within that distribution (Appendix). To maintain confidentiality, each participant was sent a unique round 2 survey with only his or her own responses indicated. Participants could keep their responses the same, or revise them in light of their peers’ responses.
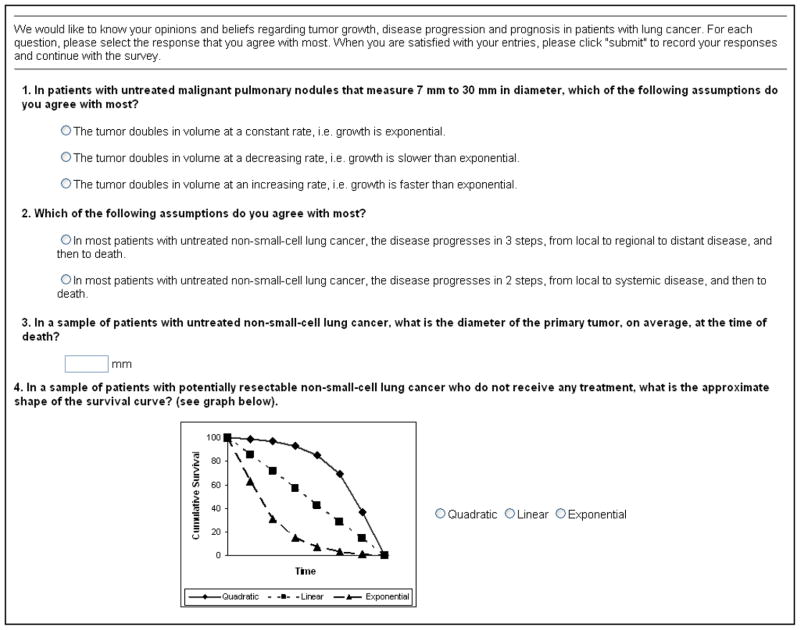
We also asked multiple choice -type questions about several assumptions in the second round survey. We asked experts to choose between several models of tumor growth (constant, increasing or decreasing rate), disease progression (3-step, from local to regional to distant, or 2-step, from local to systemic), and survival (quadratic, linear or exponential curves). We also asked experts to estimate the approximate tumor diameter at which death would occur, on average, in a sample of patients with untreated non-small-cell lung cancer (NSCLC).
Statistical Analyses
For Likert scale items, we report the number of experts that agreed or disagreed with each assumption. For estimates, we report range and median values. When we asked experts to estimate values under two different conditions, we calculated the difference between each expert’s estimates. We rep ort ranges and median values of these differences. We report detailed results from the second and final survey round only, unless otherwise noted.
RESULTS
The response rate was 100% (14/14) in both rounds of the survey. The panel included 9 specialists in pulmonary medicine, 4 thoracic surgeons, and 1 pathologist.
Tumor Growth
There was limited consensus among the experts regarding growth of malignant nodules. In the first survey round, a clear majority of experts (12/14) agreed that a 1 cm nodule has doubled in volume 30 times, an assumption consistent with exponential growth. When asked explicitly whether they believed that tumor growth was exponential, 67% (8/12) favored this model (Figure). When asked to select the tumor growth model with which they most agreed, a majority (9/14) chose exponential growth (corresponding to doubling in volume at a constant rate), buta sizable minority (5/14) believed that the rate of growth decreased over time.
Figure. Expert Panel Agreement with Assumptions, Round 2.
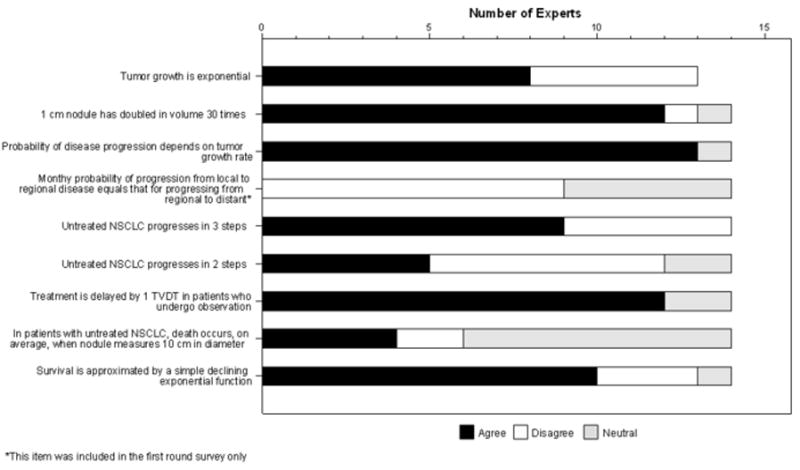
Expert agreement with assumptions about tumor growth, disease progression and survival in patients with NSCLC, after the second survey round. Responses of “Agree” and “Strongly Agree” were combined, as were responses of “Disagree” and “Strongly Disagree.” One expert did not provide a response to the final assumption
NSCLC – Non-small cell lung cancer
TVDT – Tumor volume doubling time
Disease Progression
There was clear consensus that the probability of disease progression depends on the tumor growth rate, but none of the experts agreed that the monthly probability of progression from local to regional disease equals that for progression from regional to distant disease (Figure). Experts appeared to favor a 3-step model of disease progression, with which 9/14 agreed. When forced to choose between the 3-step and 2-stepmodels, a slim majority (8/14) selected the 3 -step model as the most appropriate, while a sizable minority (6/14) selected the 2-step model. In subsequent discussions with several panel members, they suggested that lung cancer progression may be a 2-step or 3-step process in different patients.
There was clear consensus that treatment is delayed by approximately 1 TVDT in patients who undergo a period of observation, or “watchful waiting,” during their evaluation for lung cancer (Figure). However, opinion varied widely as to the consequences of such a delay. Experts’ estimates of the probability of progressing from resectable to unresectable disease during a delay lasting 1 TVDT ranged from 1 to 50% (Table).
Table.
Estimates of Tumor Growth, Disease Progression and Survival
| Estimate | n | Median | Range |
|---|---|---|---|
| Median tumor doubling time (months)1 | 14 | 4 | 1.5–14 |
| Probability of progression from resectable to unresectable disease during delay of 1 TVDT2 | 14 | 10% | 1–50% |
| Average diameter (cm) of primary tumor at time of death3 | 13 | 5 | 1–10 |
| Probability of 5-year survival if nodule resected without delay2 | 14 | 70% | 60–80% |
| Probability of 5-year survival if resection delayed by 1 TVDT2 | 14 | 65% | 40–80% |
TVDT – Tumor volume doubling time
NSCLC – Non-small cell lung cancer
CT – computed tomography
For clinically-detected 1.6 cm NSCLC.
For a 62 year old asymptomatic man with a 1.6 cm malignant solitary pulmonary nodule due to NSCLC. No evidence of hilar or mediastinal lymph node enlargement on chest CT.
For a sample of patients with untreated NSCLC.
Survival
There was consensus that in a sample of patients with potentially resectable NSCLC, survival is approximated by a simple declining exponential function (Figure). Four experts reported that survival was best approximated by a quadratic function, and none chose a linear function to describe survival. Estimates of the probability of 5-year survival with and without prompt treatment varied widely (Table). The median difference between estimates of 5-year survival with and without delayed treatment was 5% (range 0 to 20%).
In an untreated patient with NSCLC, the median tumor diameter at the time of death was believed to be 5 cm (range1 to 10 cm) (Table). Only4 participants believed that the average tumor diameter at the time of death was 10 cm (Figure).
In general, responses changed only slightly from round 1 to round 2. In four out of seven questions that were asked in both rounds, the median response (weak agreement) did not change, but a small number of panelists modified their response by moving closer to the median value. In one item (death after 40 doublings in volume), 4 respondents moved closer to the median response (neutral) and 1 moved away. In another item (lung cancer progresses in two steps), 3 respondents moved away from the median response (neutral) and 4 actually reversed their positions (2 from agreement to disagreement and 2 from disagreement to agreement). In one item (exponential growth), the median value changed from neutral to weak agreement after 3 participants modified their responses.
DISCUSSION
These results offer a first look at experts’ beliefs about the natural history of malignant SPN. Although some consensus existed among this small panel of experts, we observed substantial variability in their beliefs. This variability is likely explained in part by gaps in our current knowledge about tumor biology and the natural history of lung cancer.
One simple model of natural history assumes that a tumor begins as a single cell that measures 10 μm in diameter and grows exponentially (i.e. it doubles in volume at a constant rate), and that on average, in the absence of treatment, death occurs after 40 doublings in tumor volume, at which time the tumor measures 10 cm in diameter.7, 8 Our results suggest that the face validity of this model is limited.
Our most striking finding is the variability in experts’ estimates of the risk of disease progression during a period of observation lasting 1 TVDT, which ranged from 1% to 50%. Estimates of 5-year survival for patients in whom diagnosis and treatment were delayed also varied greatly (range 40% to 80%). Other areas of important disagreement include beliefs about growth rates (exponential versus slower than exponential) and disease progression (3-stepsversus 2-steps).
This study is limited by its small sample size, and the results may not be generalizable to other groups of experts or practicing clinicians. In most cases, we measured beliefs by using a single item, and while items were note formally validated, we believe that face validity was excellent.
In the absence of empirical data, beliefs about tumor growth and disease progression may play a role in guiding decisions about patient care. For example, clinicians who believe that malignant nodules are likely to progress from resectable to unresectable disease if diagnosis is delayed may be more likely to refer for prompt surgical resection, rather than performing a biopsy or recommending follow-up with serial imaging tests. Further research is needed to test this hypothesis and to explore the relationship between physicians’ beliefs and practices. In particular, future work should examine beliefs about tumor growth, disease progression and survival in a sample of practicing clinicians. In addition, this work should be coupled with ongoing bench and translational research into the biology of tumor growth and promoters of tumor spread.
In conclusion, this study represents the first survey, to our knowledge, of experts’ beliefs about lung cancer growth, progression and prognosis. Our results show that experts hold different beliefs about the natural history of lung cancer and suggest the possibility that these differences may partially explain variation in practices for managing patients with SPN.
Acknowledgments
We are grateful for the assistance of Raphael Fleishman in creating the on-line surveys, and for the participation of members of our expert panel.
This work was supported by a grant from the National Cancer Institute (RO1 CA117340-2). The views expressed in this paper are those of the authors and do not necessarily represent the views of the Department of Veterans Affairs or the National Cancer Institute.
Appendix
First Round Survey—Page 1
First Round Survey—Page 2
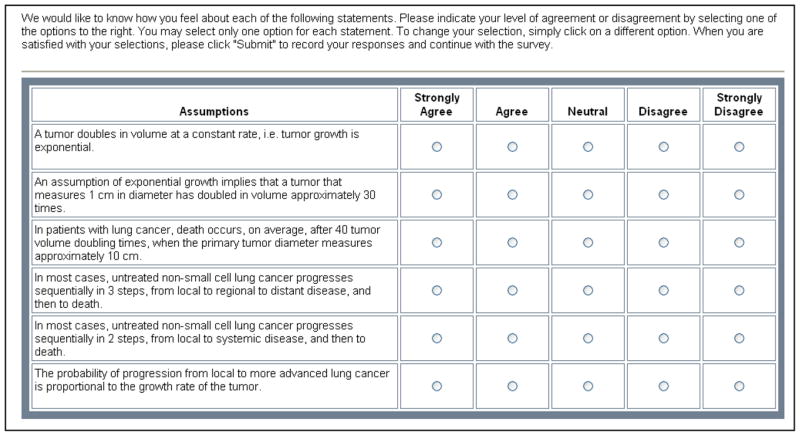
First Round Survey—Page 3
Second Round Survey—Page 1
Round 2 Survey—Page 2
Each member of the expert panel received a unique round 2 survey with only his or her responses indicated by an arrow above the bar charts. The screen shots below represent one example:
References
- 1.Gould M, Fletcher J, Iannettoni M, et al. Evaluation of patients with pulmonary nodules: When is it lung cancer? ACCP evidence-based clinical practice guidelines (2nd edition) Chest. 2007;132:108S–130S. doi: 10.1378/chest.07-1353. [DOI] [PubMed] [Google Scholar]
- 2.Gould M, Sanders G, Barnett P, et al. Cost-effectiveness of alternative management strategies for patients with solitary pulmonary nodules. Annals of Internal Medicine. 2003;138(9):724–735. doi: 10.7326/0003-4819-138-9-200305060-00009. [DOI] [PubMed] [Google Scholar]
- 3.Dalkey N, Helmer O. An experimental application of the Delphi method to the use of experts. Management Science. 1963;9(3):458–467. [Google Scholar]
- 4.Jones J, Hunter D. Qualitative research: Consensus methods for medical and health services research. British Medical Journal. 1995;311:376–380. doi: 10.1136/bmj.311.7001.376. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Murphy MK, Black NA, Lamping DL, et al. Consensus development methods, and their use in clinical guideline development. Health Technology Assessment. 1998;2(3):i–iv. 1–88. [PubMed] [Google Scholar]
- 6.Baumann MH, Strange C, Heffner JE, et al. Management of spontaneous pneumothorax: An American college of chest physicians Delphi consensus statement. Chest. 2001;119(2):590–602. doi: 10.1378/chest.119.2.590. [DOI] [PubMed] [Google Scholar]
- 7.Nathan M, Collins V, Adams R. Differentiation of benign and malignant pulmonary nodules by growth rate. Radiology. 1962;79:221–231. doi: 10.1148/79.2.221. [DOI] [PubMed] [Google Scholar]
- 8.Geddes D. The natural history of lung cancer: A review based on rates of tumor growth. British Journal of Diseases of the Chest. 1979;73:1–17. [PubMed] [Google Scholar]