Summary
This study reports trends in HIV-1 incidence in Cambodia among different target groups in the HIV-1 Sentinel Surveillance Program in 1999, 2000, and 2002, using the newly developed IgG capture BED-enzyme (HIV subtypes B, E and D) immunoassay (BED-CEIA). HIV-1-positive specimens (n = 3599) from 4 sentinel groups in the HIV-1 Sentinel Surveillance Program from 1999 to 2002—brothel-based commercial sex workers (CSWs), indirect commercial sex workers (IDSWs), police, and women attending antenatal clinics (ANCs)—were tested using the BED-CEIA. Annualized incidence rates were calculated for each group and each geographic region. Between 1999 and 2002, incidence rates declined among CSWs from 13.9% to 6.45%, among IDSWs from 5.92% to 2.87%, and among police from 1.58% to 0.26%. In the ANC group, the incidence remained stable, 0.64% in 1999, 1.11% in 2000, and 0.59% in 2002. However, there was an increasing trend among ANCs in rural areas, from 0.12 to 0.89%. In conclusion, HIV-1 incidence among CSWs, IDSWs, and police has declined between 1999 and 2002; however, the incidence has not declined in the ANC group.
Keywords: HIV-1, incidence, sentinel groups, Cambodia, recent infection, BED-CEIA
From the beginning of the HIV-1 epidemic in Cambodia, the effort to track the epidemic has relied mainly on sentinel surveillance to monitor the prevalence of HIV-1 infection.1–5
The prevalence of HIV-1 infection gives a snapshot of the magnitude of the disease burden for public health. However, incidence is the more fundamental, timely, and effective marker of the success or failure of programs aimed at preventing transmission. Over the past decade, researchers have tried to use cross-sectional specimens for the estimation of incidence.6–10
To identify acute or recent infection, different testing approaches have been used. Originally, the HIV-1 p24 antigen test or a combination of HIV-1 p24 antigen test plus the reverse transcriptase polymerase chain reaction method was used to identify recently or acutely HIV-1-infected individuals.11,12 However, these methods require testing of all the negative specimens to detect early HIV-1 infection status. In 1998, sensitive/less sensitive serologic testing strategies to identify individuals with recent infection were developed.9 However, use of commercial enzyme immunoassays (EIAs) with only subtype B antigens resulted in variable performance in different subtypes, making their application unsuitable in Southeast Asia.13,14
Recently, an IgG capture-based BED-EIA (BED-CEIA) was developed and used to detect recent HIV-1 seroconversion. 15,16 This incorporates multiple subtype antigens and has demonstrated similar performance among divergent HIV-1 subtypes. The objective of this study was to indirectly estimate the HIV-1 incidence among different HIV-1 sentinel groups in Cambodia between 1999 and 2002, using the newly developed BED-CEIA.
METHODS
This study used specimens from the HIV-1 Sentinel Surveillance (HSS) program conducted in 1999, 2000, and 2002 from 19 of 23 provinces and cities in Cambodia. There was no HSS program in 2001. Four target groups from the HSS were included in this study: women attending antenatal clinics (ANCs), direct commercial sex workers (CSWs), indirect commercial sex workers (IDSWs), and police personnel. Testing of those specimens for the HSS in Cambodia followed the World Health Organization recommended testing strategy types I and II, using the particle agglutination test (Serodia 1–2, Fujirebio, Tokyo, Japan) and enzyme-linked immunosorbent assay test (Genelavia Mixt, Pasteur Diagnostics, Marne-la-Coquette, France). HIV-1-positive specimens were retested with the BED-CEIA at the University of California, Los Angeles (UCLA) to detect recent HIV-1 seroconversion.
All HIV-1-positive specimens were tested using BED-CEIA, as described earlier, using the recommended algorithm. 15,17 Briefly, sera were diluted 1/100 and incubated on goat–antihuman IgG-coated microwell plates to allow capture of HIV and non-HIV IgG. HIV-specific IgG was detected by a multisubtype-derived branched peptide (BED-biotin), followed by streptavidin-peroxidase. The optical density values were normalized using a calibrator specimen included on every run. Specimens with an OD-n of ≤1.5 during initial BED-CEIA testing were confirmed by further testing in triplicate. An HIV-1-positive specimen for which the confirmatory BED-CEIA gave an OD-n of ≤1 was considered to be a recent HIV-1 infection, with seroconversion having occurred within the previous 168 days (95% CI, 155–184 days), based on multiple seroconverter studies15 (also unpublished data). Otherwise, the specimen was classified as long-term infection. The mean seroconversion interval will continue to be revised as more data are accumulated, but the data suggest that the format of the assay and the inclusion of multisubtype antigens identify similar seroconversion duration among various subtypes.
False-positive specimens will be classified as recent infections with BED-CEIA and will thus falsely elevate the HIV-1 incidence. To exclude this possibility, standard HIV serology was repeated for all specimens with an OD-n of ≤0.5 with BED-CEIA.
Sample Size
For sentinel surveillance, the sample size for each group was calculated by the HSS in Cambodia to be able to derive a 95% CI with a margin of error not >2% for ANCs and police and 6% for CSWs and IDSWs. The sample size varied according to the previous estimates of HIV prevalence in each province. The sample size for ANC was 300 in provincial capitals and 300 in remaining districts in all selected provinces. For police, in provinces where the most recent estimates of prevalence were ≤5%, the sample size was 300, and it was 100–150 in those where the prevalence was >5%. For brothel-based sex workers, the sample was 100–150. Total number of seropositive specimens from the HSS was 3685, and 3486 (94.59%) were available for testing.
Sampling Strategies
Commercial sex workers were defined as brothel-based commercial sex workers, and IDSWs were defined as women working as beer promotion girls or as bar, karaoke, or massage girls. “Take-all” or 2-stage cluster sampling was used according to the total number of sex workers in the province. Two-stage cluster sampling was also implemented among police. Pregnant women attending the designated ANC for their first visit for any pregnancy were recruited consecutively in the order in which they appeared at the sentinel sites.
Statistical Analysis
The annual incidence was calculated as I = [Nr/(Nr + Nne)] × 365/T × 100, where Nr is the total number of recent infections, Nne is the total number of uninfected persons, and T is the estimated length of mean seroconversion duration for the BED-CEIA.13 The revised estimated length of this interval is 168 days (95% CI, 155–184 days; unpublished data). Specimens that could not be retested with the peptide-based capture EIA because specimens were missing or quantity was insufficient (missing) were considered to have the same chance of being a recent infection as the ones tested. The 95% CI for estimated HIV-1 incidence was constructed using a Bonferroni procedure.9
The age- and province-standardized incidence was calculated using the female and male census population (aged 15–49 years) as the standard population for the ANC and police groups, respectively. The census of direct and indirect sex workers was used for standardization of HIV-1 incidence in these 2 groups.
Trends of HIV-1 incidence were examined separately for each target group. Odds ratios were calculated by logistic regression. HIV-1-positive specimens that were not classified as recent infection were excluded from the analysis.
HIV-1 incidences in different regions of Cambodia were also estimated. According to a consensus meeting in Cambodia in 2002, Cambodia is geographically divided into 3 regions: the western region bordering Thailand, the eastern region bordering Vietnam, and the rest as the central region.
All analyses were conducted using Statistical Analysis Software v. 8.0 (SAS Institute, Cary, NC) and EXCEL (Microsoft Office XP).
The study was approved by the Institutional Review Board at UCLA.
RESULTS
In each year from 1999 to 2002, CSWs had the highest incidence of HIV-1, followed, in decreasing order, by IDSWs, police, and ANCs. Table 1 presents the results of trend analyses controlling for demographic factors such as age, marital status, education, and location. In the CSW group, the incidence declined consistently from 13.90 per 100 person-years in 1999 to 6.45 per 100 person-years in 2002. This decline was statistically significant after controlling for demographic factors (odds ratio: 0.79, 95% CI 0.69–0.90) and was most marked in the 20- to 29-year age group. In the IDSW group, the incidence also declined from 5.08 per 100 person-years in 1999 to 2.87 per 100 person-years in 2002. The decrease was borderline significant after controlling for demographic factors (odds ratio: 0.82, 95% CI 0.66–1.03). In the police group, the incidence declined from 1.74 per 100 person-years in 1999 to 0.26 per 100 person-years in 2002. The decrease was statistically significant after controlling for demographic factors (odds ratio: 0.64, 95% CI 0.48–0.84) and most marked in the 30- to 49-year age group. In the ANC group, from 1999 to 2002, the incidence leveled off (odds ratio: 0.96, 95% CI 0.79–1.17). However, when stratified by location, the incidence in the urban areas decreased, whereas the incidence in the rural areas increased. However, neither trend was significant (data not shown).
TABLE 1.
HIV-1 Incidence Trends in Different Sentinel Surveillance Groups, 1999–2002
| 1999 | 2000 | 2002 | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Group | Age Group |
Pop. at Risk |
Inc. 100 Person Years* |
Pop. at Risk |
Inc. 100 Person Years* |
Pop. at Risk |
Inc. 100 Person Years* |
OR | 95% CI | P Value |
| ANC | 14–19 | 516 | 1.26 | 556 | 0.00 | 1590 | 0.91 | 1.17 | 0.64–2.14 | 0.61 |
| 20–29 | 2798 | 0.55 | 3248 | 1.52 | 4404 | 0.61 | 0.9 | 0.70–1.17 | 0.44 | |
| 30–39 | 1470 | 0.81 | 1754 | 0.66 | 2230 | 0.72 | 0.97 | 0.66–1.41 | 0.88 | |
| 40–49 | 216 | 0.00 | 341 | 0.00 | 344 | 0.63 | — | — | — | |
| Overall | 0.72† | 1.11† | 0.59† | 0.96‡ | 0.79–1.17 | 0.69 | ||||
| CSW | ||||||||||
| 14–19 | 488 | 9.38 | 350 | 8.57 | 355 | 6.54 | 0.87 | 0.67–1.13 | 0.29 | |
| 20–29 | 993 | 13.02 | 998 | 7.68 | 1123 | 6.17 | 0.76 | 0.65–0.89 | 0.0007 | |
| 30–39 | 99 | 8.78 | 109 | 12.17 | 93 | 2.42 | 0.7 | 0.39–1.26 | 0.24 | |
| Overall | 13.90† | 9.02† | 6.45† | 0.79§ | 0.69–0.90 | 0.0003 | ||||
| IDSW | ||||||||||
| 14–19 | 340 | 5.08 | 392 | 5.26 | 221 | 3.27 | 0.82 | 0.53–1.29 | 0.39 | |
| 20–29 | 848 | 6.82 | 997 | 2.77 | 768 | 3.64 | 0.78 | 0.60–1.02 | 0.07 | |
| 30–39 | 62 | 0.00 | 86 | 2.53 | 78 | 0.00 | 0.64 | 0.07–5.66 | 0.69 | |
| Overall | 5.08† | 5.08† | 2.87† | 0.82§ | 0.66–1.03 | 0.09 | ||||
| Police | ||||||||||
| 20–29 | 866 | 2.00 | 718 | 0.91 | 563 | 1.16 | 0.87 | 0.53–1.44 | 0.59 | |
| 30–39 | 1893 | 1.18 | 2,191 | 0.89 | 2,152 | 0.22 | 0.59 | 0.37–0.93 | 0.02 | |
| 40–49 | 796 | 2.26 | 912 | 1.48 | 1,067 | 0.49 | 0.58 | 0.35–0.98 | 0.04 | |
| ≥50 | 121 | 1.80 | 184 | 0.00 | 242 | 0.00 | — | — | — | |
| Overall | 1.74† | 1.30† | 0.26† | 0.64§ | 0.48–0.84 | 0.001 | ||||
Incidence per 100 person-years.
Adjusted for the provincial population size.
Odds ratio adjusted for age, marital status, location, and schooling.
Odds ratio adjusted for age, marital status, and schooling.
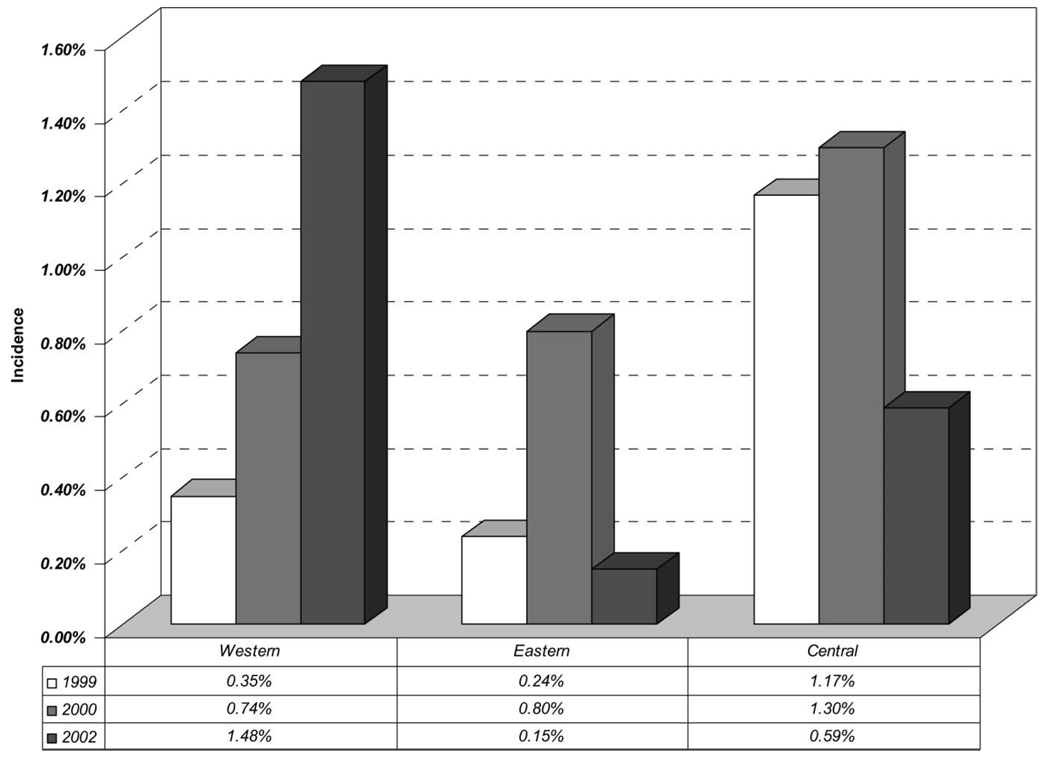
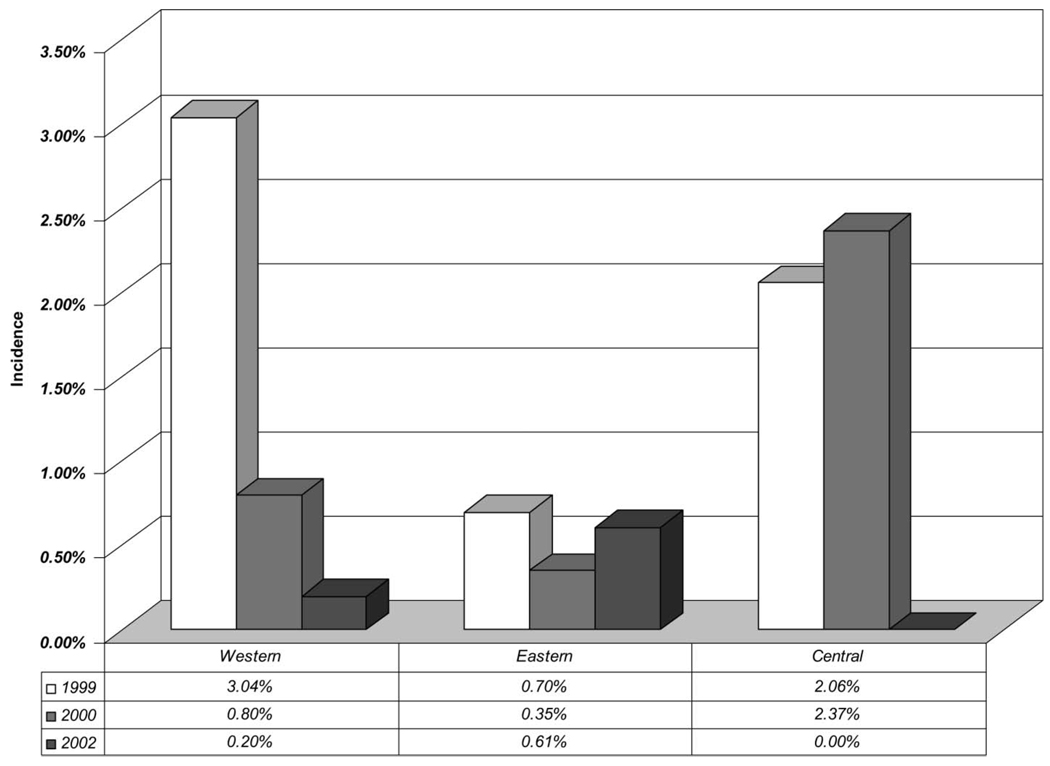
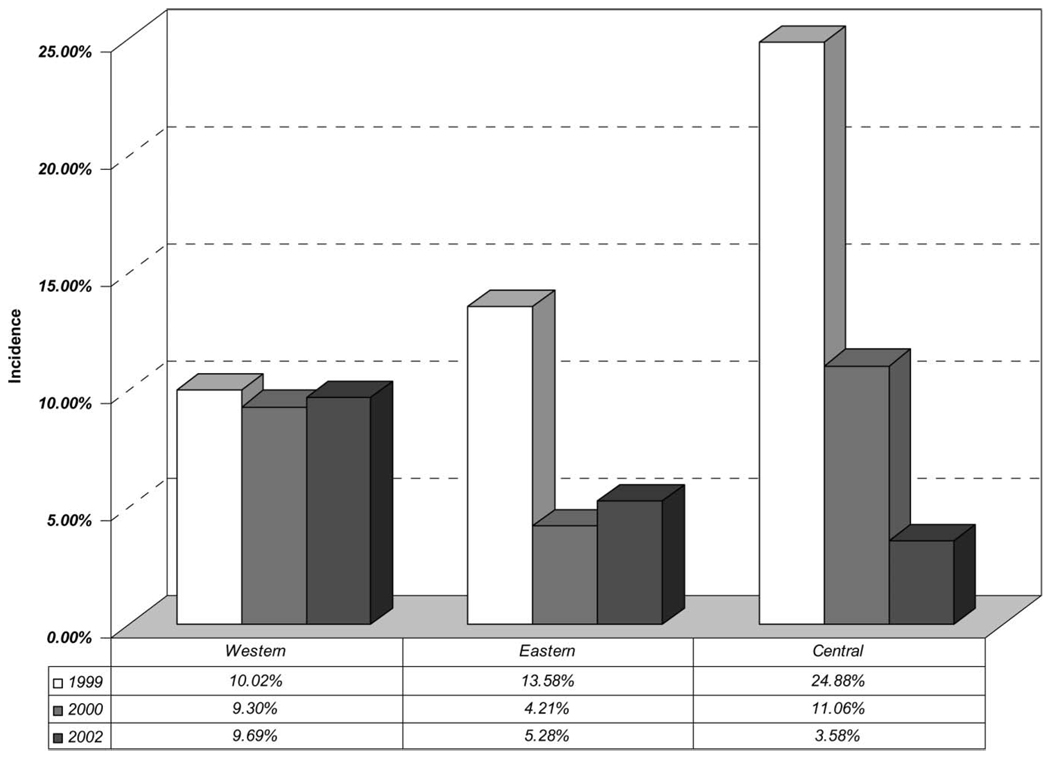
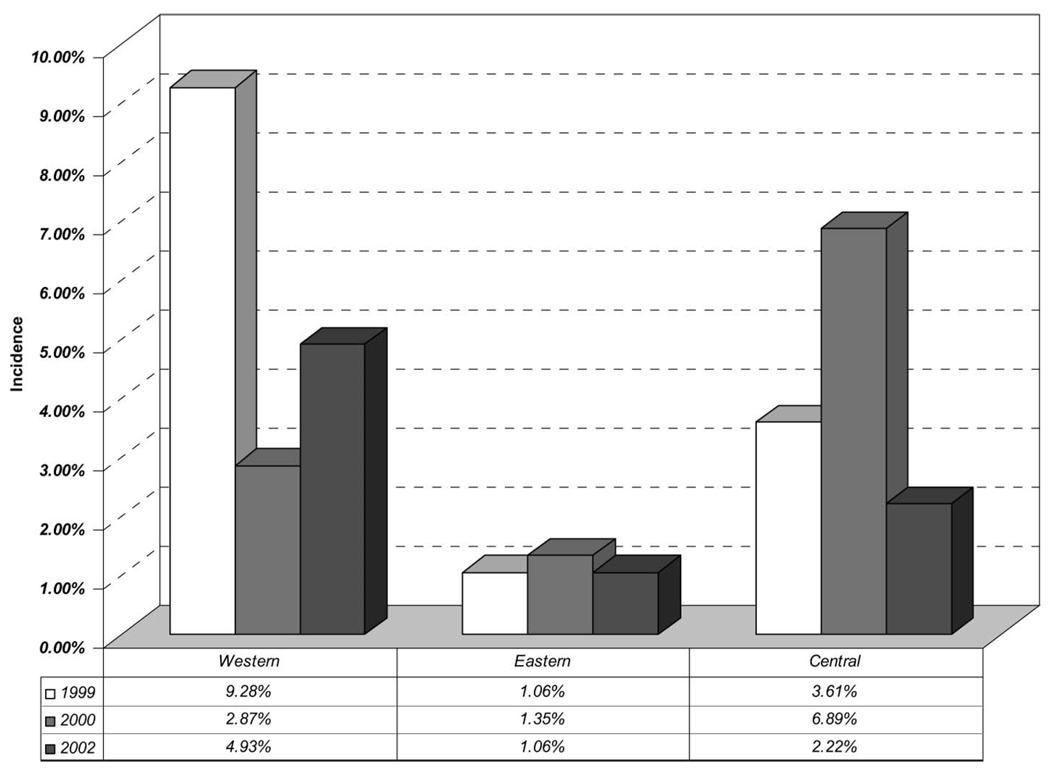
Analyzing the incidence by different regions of the country, the incidence was higher in the western region (Figs. 1–4). Even though the overall trend of HIV-1 incidence in pregnant women showed a stable incidence from 1999 to 2002, we observed a declining trend among pregnant women in the central and eastern parts of the country and a significant increase in incidence in the western region (Fig. 1). CSWs in the western region had a stable rate of HIV-1 incidence, whereas there was a declining trend in the other 2 regions (Fig. 2). Among IDSWs, only the western region showed a significantly decreasing trend (Fig. 3). In police, the western and central regions had a declining trend, whereas the eastern region had a stable rate of HIV-1 incidence during these years (Fig. 4).
FIGURE 1.
Trend of HIV-1 incidence among ANCs in different regions in Cambodia.
FIGURE 4.
Trend of HIV-1 incidence among police in different regions in Cambodia.
FIGURE 2.
Trend of HIV-1 incidence among CSWs in different regions in Cambodia.
FIGURE 3.
Trend of HIV-1 incidence among IDSWs in different regions in Cambodia.
DISCUSSION
To our knowledge, this is the first application of the BED-CEIA to estimate HIV-1 incidence from HIV-1 sentinel surveillance data in southeast Asia in general and in Cambodia in particular. Our results suggest that there has been significant decline in incidence from 1999 to 2002 in 2 target groups: CSWs and police. IDSWs showed the same trend, but it was highly significant in only the western region. ANCs were the only group for which the overall trend did not show any decline. These results are also consistent with the trends of HIV-1 prevalence in the sentinel surveillance program in Cambodia4 and the temporal trends of key risk behaviors in the behavioral surveillance program in Cambodia.18
The decline in incidence among CSWs, IDSWs, and police personnel may reflect the effectiveness of the intervention program to reduce heterosexual transmission from the high-risk population to the bridge population through the 100% condom campaign.19 It is not unexpected that this intervention program has had little or no impact on the transmission from those who are already infected to their usual sexual partners and wives, since testing and counseling are not widely available and condom use is low with wives and girlfriends.18
The overall HIV-1 incidence in the western region showed an alarming increase among pregnant women and no decline among CSWs. This trend could be due to the high internal migration to this region. The high HIV-1 incidence rate among CSWs in Cambodia makes this population well suited for HIV-1 prevention research, including vaccine trials.
Several biases influence the estimation of incidence due to the design of the HSS program. First, wide coverage of the surveillance program, coupled with some rotation in personnel supervisors, makes it difficult to keep the standard operating procedure comparable over subsequent years.1–4 Second, the rate of refusal varied from year to year, and the characteristics of those who refused to participate in the study are not known. If those who refused to participate in the study had higher risk behaviors than those who participated, this estimate may have been biased and thus may have affected the analyses of HIV-1 incidence trends. Third, it was assumed that the ANC group was representative of all pregnant women. This may not be true in Cambodia, because poor women are more likely to use ANCs (as opposed to private clinics), if at all. According to the Demographic Health Survey in Cambodia in 2000, only one-third of Cambodian women who had given birth over the previous 5 years received antenatal care from a medically trained person.20 A study conducted in Cambodia comparing HIV-1 prevalence data from the HIV-1 sentinel surveillance to a population-based survey of women in the catchment area showed that HIV-1 prevalence among ANCs provides an overestimate of the general population of women in rural areas.21 Therefore, any attempt to use data from pregnant women to represent the general female population should take this factor into account. Finally, since the younger women were oversampled in 2002 and younger infected women are more likely to be recently infected than older women, the results may have been biased.
Several other factors should also be considered in interpreting the results of HIV-1 testing. We found that among those samples that were brought to UCLA, some were false positives. It is then important to know what the false-negative rate would be among those negative samples; however, this is not known. The findings from current data analyses assumed that there were no false negatives among those negative samples. If this is not true, the incidence estimated here would reflect an underestimation of the incidence in each sentinel group. Another important assumption was that the rates of false positives and recent infections were similar between those specimens that were tested by the BED-CEIA and those not tested (5.4%). A sensitivity analysis was performed assuming 3 different scenarios: all missing specimens were not recent infections; all missing specimens have the same proportion of recent infections as the ones tested; and all missing specimens are recent infections. The sensitivity analysis showed that the trends were basically the same.
Lastly, some precautions need to be taken when interpreting the results of the BED-CEIA used in this study. The absolute estimate of incidence depends on the accuracy of the seroconversion interval. In trend analysis of populations, the error introduced by any inaccuracy of this interval would be systematic, and trends analyses are therefore likely to be valid. However, continued validation of BED-CEIA in cross-sectional specimens with known HIV-1 incidence will be important to assess the findings of this study. Four percent of the persons at the end stage of AIDS may be falsely classified by BED-CEIA as recent infections.14 However, persons with end-stage AIDS are less likely to participate in the surveillance program and would probably already be symptomatic.
When estimating the incidence from the prevalence of recent infections, an important assumption was made that the population was in a steady state, with no net case migration from the pool of prevalent cases, which was conditional on age at migration and age at disease onset. Since the duration of the infection detected by BED-CEIA was only 168 days, the theoretical condition of “stationary population with no net migration” as described here is likely to hold true.
In conclusion, the study found that HIV-1 incidence rates among 3 sentinel groups, CSWs, IDSWs, and police, declined over the study period between 1999 and 2002. These declines may reflect the effectiveness of the intervention programs Cambodia has implemented. However, this study also showed that the epidemic persists in pregnant women in Cambodia and in the western region. Further studies should focus on strategies to protect at-risk women in Cambodia.
ACKNOWLEDGMENTS
The authors thank the National Center for HIV/AIDS, Dermatology and STDs (NCHADS) for the use of their HIV-1 Sentinel Surveillance Program 1999 to 2002 data. The authors also wish to acknowledge Drs. Anthony Butch, Najib Aziz, and Carlos Garibay in the Department of Pathology and Laboratory Medicine at UCLA for their laboratory support. In addition, the authors would like to thank Drs. Kaoeun Chettra, Mun Phalkun, Theng Thithara, and Lim Yi, and all the provincial AIDS program staff members for their tireless efforts to collect the data and specimens that made this study possible. We also thank Wendy Aft for preparation of the manuscript.
Partly funded by NIH/Fogarty International Center grant TW000013.
REFERENCES
- 1.Report on Sentinel Surveillance in Cambodia, 1998. Cambodia: Phnom Penh; 1999. National Center for HIV/AIDS, Dermatology and STD Control, Cambodia. [Google Scholar]
- 2.Report on HIV Sentinel Surveillance in Cambodia, 1999. Cambodia: Phnom Penh; 2000. National Center for HIV/AIDS, Dermatology and STD Control, Cambodia. [Google Scholar]
- 3.Report on HIV Sentinel Surveillance in Cambodia, 2000. Cambodia: Phnom Penh; 2001. National Center for HIV/AIDS, Dermatology and STD Control, Cambodia. [Google Scholar]
- 4.Dissemination Workshop of HIV-1 Sentinel Surveillance Cambodia, 2002. Cambodia: Phnom Penh; 2002. National Center for HIV-1/AIDS, Dermatology and STDs Control, Cambodia. [Google Scholar]
- 5.WHO/UNAIDS. AIDS Epidemic Update. Geneva, Switzerland: 2002. [Google Scholar]
- 6.Brookmeyer R, Quinn T, Shepherd M, et al. The AIDS epidemic in India: a new method for estimating current human immunodeficiency virus (HIV-1) incidence rates. Am J Epidemiol. 1995;142:709–713. doi: 10.1093/oxfordjournals.aje.a117700. [DOI] [PubMed] [Google Scholar]
- 7.Brookmeyer R, Quinn TC. Estimation of current human immunodeficiency virus incidence rates from a cross-sectional survey using early diagnostic tests. Am J Epidemiol. 1995;141:166–172. doi: 10.1093/oxfordjournals.aje.a117404. [DOI] [PubMed] [Google Scholar]
- 8.Cleghorn FR, Jack N, Murphy JR, et al. Direct and indirect estimates of HIV-1 incidence in a high-prevalence population. Am J Epidemiol. 1998;147:834–839. doi: 10.1093/oxfordjournals.aje.a009536. [DOI] [PubMed] [Google Scholar]
- 9.Janssen RS, Satten GA, Stramer SL, et al. New testing strategy to detect early HIV-1 infection for use in incidence estimates and for clinical and prevention purposes. JAMA. 1998;280:42–48. doi: 10.1001/jama.280.1.42. [DOI] [PubMed] [Google Scholar]
- 10.Mehendale SM, Rodrigues JJ, Brookmeyer RS, et al. Incidence and predictors of human immunodeficiency virus type 1 seroconversion in patients attending sexually transmitted disease clinics in India. J Infect Dis. 1995;172:1486–1491. doi: 10.1093/infdis/172.6.1486. [DOI] [PubMed] [Google Scholar]
- 11.Kinloch-De Loes S, Hirschel BJ, Hoen B, et al. A controlled trial of zidovudine in primary human immunodeficiency virus infection. N Engl J Med. 1995;333:408–413. doi: 10.1056/NEJM199508173330702. [DOI] [PubMed] [Google Scholar]
- 12.Schacker T, Collier AC, Hughes J, et al. Clinical and epidemiologic features of primary HIV-1 infection. Ann Intern Med. 1996;125:257–264. doi: 10.7326/0003-4819-125-4-199608150-00001. [DOI] [PubMed] [Google Scholar]
- 13.Parekh BS, Hu DJ, Vanichseni S, et al. Evaluation of a sensitive/less-sensitive testing algorithm using the 3A11-LS assay for detecting recent HIV-1 seroconversion among individuals with HIV-1-1 subtype B or E infection in Thailand. AIDS Res Hum Retroviruses. 2001;17:453–458. doi: 10.1089/088922201750102562. [DOI] [PubMed] [Google Scholar]
- 14.Young CL, Hu DJ, Byers R, et al. Evaluation of a sensitive/less sensitive testing algorithm using the bioMerieux Vironostika-LS assay for detecting recent HIV-1-1 subtype B’ or E infection in Thailand. AIDS Res Hum Retroviruses. 2003;19:481–486. doi: 10.1089/088922203766774522. [DOI] [PubMed] [Google Scholar]
- 15.Parekh BS, Kennedy MS, Dobbs T, et al. Quantitative detection of increasing HIV type 1 antibodies after seroconversion: a simple assay for detecting recent HIV-1 infection and estimating incidence. AIDS Res Hum Retroviruses. 2002;18:295–307. doi: 10.1089/088922202753472874. [DOI] [PubMed] [Google Scholar]
- 16.Hu DJ, Vanichseni S, Mock PA, et al. HIV-1 incidence estimates by detection of recent infection from a cross-sectional sampling of injection drug users in Bangkok: use of the IgG capture BED enzyme immuno-assay. AIDS Res Hum Retroviruses. 2003;19:727–730. doi: 10.1089/088922203769232511. [DOI] [PubMed] [Google Scholar]
- 17.Dobbs T, Kennedy S, Pau CP, et al. Performance characteristics of the immunoglobulin G-capture BED-enzyme immunoassay, an assay to detect recent human immunodeficiency virus type 1 seroconversion. J Clin Microbiol. 2004;42:2623–2628. doi: 10.1128/JCM.42.6.2623-2628.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Gorbach P, Sopheab H, Leng HB, et al. National Center for HIV/AIDS, Dermatology and STDs. Cambodia: Phnom Penh; 2002. BSSV: Sexual Behavior Among Urban Sentinel Groups, Cambodia, 2001. [Google Scholar]
- 19.World Health Organization/Western Pacific Region. Report on 100% condom use. 2001 [Google Scholar]
- 20.National Institute of Statistics. (Ministry of Planning, Directorate General for Health (Ministry of Health.) Cambodia: Phnom Penh; Cambodia Demographic Health Survey, 2000. 2003
- 21.Saphonn V, Leng HB, Ly SP, et al. How well do antenatal clinic (ANC) attendees represent the general population? A comparison of HIV-1 prevalence from ANC sentinel surveillance sites with a population-based survey of women aged 15–49 in Cambodia. Int J Epidemiol. 2002;31:449–455. [PubMed] [Google Scholar]