Abstract
Background and Objective
The Sonagachi Project in Calcutta, India, organized sex workers to improve working conditions.
Goal
To compare rates of sexually transmitted diseases between the Sonagachi Project and other areas in which only the National AIDS Control Organization (NACO) interventions were implemented.
Study
A cross-sectional survey of randomly selected female sex workers.
Results
There was no difference in the prevalence of all STDs between the 2 areas; both were lower than reported in other surveys in 1992. Analysis using propensity scores also failed to demonstrate any difference. The number of preventive activities was similar in the Sonagachi and NACO-only areas but was more prevalent than in 1992. Sex workers in the Sonagachi area had better treatment-seeking behavior and attitudes. Both the Sonagachi and NACO strategies have resulted in lower STD rates, but the Sonagachi Project also increased the proportion who had an optimistic attitude and increased prevention and treatment-seeking behavior.
Since the first report of human immunodeficiency virus (HIV) in 1986, HIV/acquired immunodeficiency syndrome (AIDS) has been spreading relentlessly in India, as in other parts of the world. In Vellore, in southern India, the prevalence of HIV among female sex workers (FSWs) increased from 1.8% in 1986 to 28.6% in 1990.1 From 1991 to 1996, the HIV prevalence among CSWs in Mumbai, the largest city in India, rose from 1% to 51%.2 Responding to the epidemic, the National AIDS Control Organization (NACO) implemented intervention measures among high-risk groups, including FSWs. NACO has designated nongovernment organizations (NGOs) to recruit and train peer workers to conduct information, education, and communication (IEC) activities and to promote condom use among FSWs. FSWs play an important role in heterosexual transmission of HIV.3 Control of sexually transmitted diseases among sex workers may have a significant impact upon the spread of HIV.4 A model has suggested that a successful sex worker intervention in India would drive the HIV/AIDS epidemic to extinction.5
Sonagachi is one of the oldest and largest red light areas in Calcutta. In 1992, the All India Institute of Hygiene and Public Health (AIIH & PH) undertook a community-based survey in Sonagachi to assess the prevalence of STDs and HIV among sex workers. After the survey, AIIH & PH initiated the Sonagachi Project, with the primary aim of organizing the sex workers to promote behavioral change to control the spread of STDs and HIV. The Project arranged for the provision of health services, including STD treatment from a central clinic and dissemination of information regarding prevention of STD/HIV transmission and promotion of condoms. The Project employed sex workers as peer educators to propagate information promoting behavioral change, to distribute and promote condoms, and to refer sex workers to clinics. Although sex workers are the main focus of the sex trade, they have the least say in matters related to it. They are controlled by the mashi (brothel owner), dalal (pimp), babu (regular customer), mastan (hooligan), and other power brokers. The Project addressed this problem and started a process of “empowerment” of the sex workers to improve their social, political, and economic conditions. The sex workers formed a forum of their own, the Durbar Mahila Samanwaya Committee, which promoted dignity and betterment of working conditions. Whenever there was a complaint regarding a sex worker, the members of the committee stood behind her and protested for her. As a result, they acquired the power to influence the powerbrokers.
The Project also included ongoing evaluations that suggested a favorable impact on awareness of STDs and HIV, use of condoms, and prevalence of STDs among sex workers. The New York Times said, “… it is the prostitutes themselves who have become the leading crusaders against AIDS.”6 The favorable impact of the Project was examined temporally among the same group of sex workers, but no comparison was made simultaneously with sex workers outside the Project. In addition, the evaluations were carried out by the Project itself, which might have a natural inclination to demonstrate a favorable impact. Sex workers in other red light areas were provided with similar services under a NACO program, with the exception of the empowerment effort. The NACO program included provision of health services, including STD treatment, and IEC regarding prevention of STD/HIV transmission, as well as promotion of condoms. These services were instituted through NGOs, 1 for each red light area. The NGOs in turn employed peer workers. The present survey was designed to compare demographic characteristics and the differences in knowledge, attitudes, and practices, as well as the prevalence of STDs between the 2 groups of sex workers, those in the Sonagachi Project and those receiving the NACO intervention only.
Materials and Methods
A comparative cross-sectional study was undertaken to assess the success of the intervention program among the sex workers in Calcutta. This study project was approved by the institutional review boards of UCLA and the National Institute of Cholera and Enteric Diseases, India. Sex workers in both the Sonagachi and NACO-only groups responded to a questionnaire that evaluated their knowledge, attitudes, and practices regarding STDs/HIV. The presence of STDs was also determined. Only brothel-based sex workers were included in the study, as floating sex workers might have a different risk level for STDs than their brothel-based counterparts. Because parental or guardian consent might not be available, those below 18 years of age were excluded. Since we had no established data about the prevalence of any STDs among sex workers outside the Project, we assumed it to have continued at the baseline level as reported from the Project in 1992, which was about 25%. Among 418 sex workers surveyed in 1992, the prevalence of candidiasis was 16.5%, 15.3% for trichomoniasis, and 4.8% for syphilis (Table 1). Considering the above facts, and to have a confidence level of 95% and power of 80%, the necessary sample size was calculated to be 308, with 154 sex workers from each of the two groups. A 25% increment was added to compensate for refusals. Thus, the final target was 400 subjects, 200 in each group.
TABLE 1.
Prevalence of Sexually Transmitted Diseases Among Sex Workers of Sonagachi Project in 1992 and 2003
| STD | 1992, % (Total No. of Subjects)11,12 | 2003, % (Total No. of Subjects) | P Value |
|---|---|---|---|
| Syphilis | |||
| Current | 4.8 (418) | 1.2 (168) | 0.04 |
| TPHA +ve | 63.0 (370) | 16.7 (168) | <0.0001 |
| Vaginal discharge | 48.3 (418) | 14.3 (168) | <0.0001 |
| Candidiasis | 16.5 (418) | 8.9 (168) | 0.02 |
| Trichomoniasis | 15.3 (418) | 3.0 (168) | <0.0001 |
| Cervical smear Gram stain +ve | 13.2 (370) | 17.3 (168) | 0.22 |
| Condyloma acuminata | 5.3 (418) | 4.2 (168) | 0.58 |
| Molluscum contagiosum | 2.4 (418) | 3.6 (168) | 0.43 |
For selection of sex workers in the Sonagachi Project, a list of red light areas under the Project was obtained from the Project managers. One red light area was selected randomly from that list. Individual brothels within the selected area were identified by their addresses, from which 20 brothels were selected randomly. Ten sex workers were selected randomly from each selected brothel.
Because all the major red light areas in Calcutta city were within the Sonagachi Project, we searched for areas on the outskirts of Calcutta, where the Project was not operating, which received the NACO intervention only. The number of sex workers in these areas was smaller. For this reason, we included all the sex workers in several of these outlying red light areas in the study to allow for refusals and to achieve a sample size of 200.
An informed verbal consent was obtained from each subject. The selected sex workers answered an anonymous structured questionnaire administered by trained social workers. The questions included demographic characteristics and knowledge, attitudes, and practices regarding STDs/HIV. No personal identifying information was asked. The subjects were then examined clinically for STDs. A smear of cervical secretion was collected for Gram stain for detection of Gram-negative diplococci, a presumptive diagnostic of Neisseria gonorrhoeae (Ng). Samples of urine and blood were also collected. Blood samples were examined by rapid plasma reagin (RPR) (Span Diagnostics Ltd., Gujarat, India) and the treponema pallidum hemagglutination assay (TPHA) (New-market Laboratories Ltd., Newmarket, England), and urine samples were examined for N gonorrhoeae and Chlamydia trachomatis (Ct) by PCR (Roche Amplicor CT/NG test kit, Germany). The TPHAs that were indeterminate were considered negative. When both RPR and TPHA were positive, the subject was considered to have active syphilis. If TPHA was negative and RPR was positive for a dilution of less than 1:8, the RPR result was regarded as a false-positive reaction. All the laboratory investigations were carried out by trained technicians at the National Institute of Cholera and Enteric Diseases, an institute of the Indian Council of Medical Research. Every batch of RPR, TPHA, and PCR testing was checked using simultaneous positive and negative controls.
Knowledge about STDs/HIV was assessed by questions that included both positive and negative answers. The answers were accordingly scored, with 1 point for a correct answer and no point for an incorrect answer. Similarly, positive and negative attitudes were scored for each subject, depending on responses to specific questions.
The questionnaires were scrutinized thoroughly for consistency, and the data were entered using Epiinfo 6 software. Data were analyzed with SPSS 10.0 windows software. The Student t test was used for analysis of continuous data, the χ2 test for categorical data, and the nonparametric Kolmogorov Smirnov test7 for comparing discrete data. A logistic regression analysis was performed to determine the odds ratio for the presence of STDs among the sex workers in both of the groups, controlling for relevant risk factors that were found to be significantly (P <0.05) different between the 2 groups.
During the survey, we found that the response rate among the sex workers in the NACO-only area was unsatisfactory. Also, there were differences between the 2 groups of sex workers in demographic variables and in some risk behaviors. To achieve comparability between the 2 groups, subgroups were identified with similar propensity scores.8,9 Propensity scores are used primarily to make an adjustment for covariates while calculating the exposure effect. Using propensity analysis effectively controls for those covariates included in the propensity models by comparing subgroups with a similar distribution of the covariates. This facilitates examination of the consistency of the intervention effect across subgroups of participants and minimizes the loss of degrees of freedom in controlling for confounders. A program in the SPSS 10 Windows software was used to determine the score of an individual subject. The variables used to construct the propensity score of an individual sex worker included age, marital status, duration of sex work, number of clients per day, income per day, having regular STD check-ups, condom use, sex work outside the brothel, and attending a clinic/hospital for treatment of STDs. The χ2 test was performed between the individual subgroups to determine any differences.
Results
Of the 200 selected sex workers in the Sonagachi area, 173 (87%) took part in the survey. All sex workers in the 3 red light areas in the NACO-only intervention group, a total of 260 sex workers, needed to be recruited to reach a sample size of 169 (65%). Thus, the refusal rate was 13% in the Sonagachi area and 35% in the NACO-only area. Many of those refusing cited the fear of blood collection or speculum examination as their reasons. All the women completed the interview, but not all of them responded to all the questions asked. The demographic data are tabulated with the number of responses to each question in Table 2.
TABLE 2.
Demographic Characteristics of the Study Sample According to Group
| Characteristic | Sonagachi Group | NACO-Only Group | P Value |
|---|---|---|---|
| Age, y | (n = 173) | (n = 169) | <0.0001 |
| Mean | 27 | 32 | |
| Median | 27 | 32 | |
| Range | 18 to 40 | 18 to 50 | |
| Education | (n = 173) | (n = 167) | 0.026 |
| Illiterate | 138 (80%) | 148 (89%) | |
| Up to class V | 25 (14%) | 13 (8%) | |
| Secondary | 10 (6%) | 5 (3%) | |
| Higher secondary | 0 | 1 (0%) | |
| Marital status | (n = 172) | (n = 168) | <0.0001 |
| Unmarried | 76 (44%) | 50 (30%) | |
| Married | 20 (12%) | 18 (11%) | |
| Widowed | 8 (5%) | 16 (9%) | |
| Separated | 68 (39%) | 84 (50%) | |
| Number of dependents | (n = 173) | (n = 167) | 0.17 |
| ≤2 | 75 (44%) | 85 (51%) | |
| 3 to 5 | 80 (46%) | 67 (40%) | |
| ≥5 | 18 (10%) | 15 (9%) | |
| Number of clients | (n = 173) | (n = 169) | <0.0001 |
| 1/Day | 28 (16%) | 79 (47%) | |
| 2/Day | 58 (34%) | 52 (31%) | |
| ≥3/Day | 87 (50%) | 38 (22%) | |
| Income per day (in Rs.) | (n = 172) | (n = 166) | <0.0001 |
| Mean | 166 | 77 | |
| Median | 130 | 50 | |
| Range | 30 to 1000 | 10 to 400 | |
| Duration of sex work | (n = 173) | (n = 169) | <0.0001 |
| <1 y | 39 (22%) | 20 (12%) | |
| 1 to 5 y | 76 (44%) | 36 (21%) | |
| >5 y | 58 (34%) | 113 (67%) |
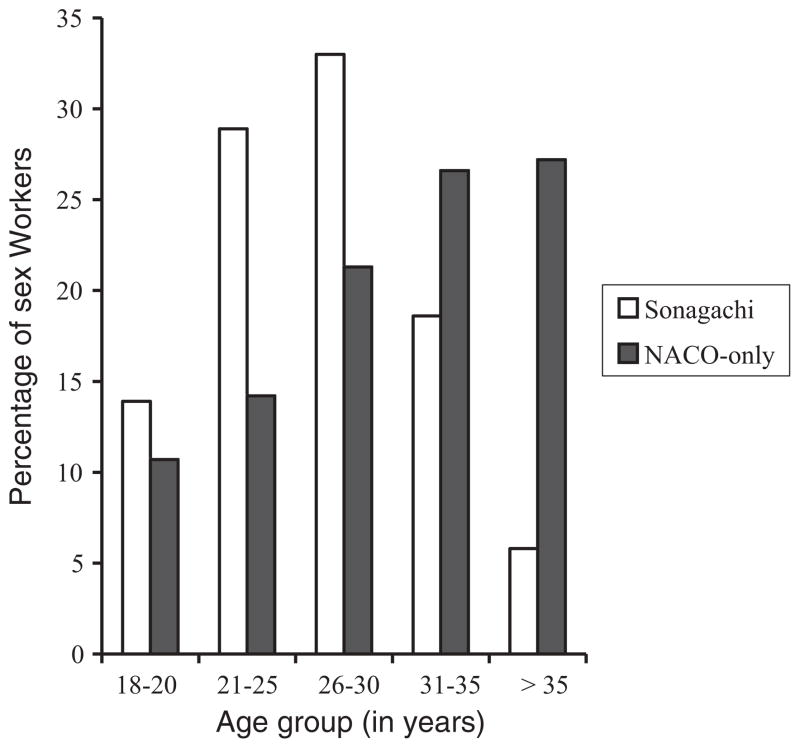
The NACO-only area sex workers were significantly older (P < 0.0001) than the Sonagachi sex workers. The mean and median ages were similar within each of the two groups. The age distribution of the 2 groups is shown in Figure 1.
Fig. 1.
Age distribution of the 2 groups.
Most of the sex workers were illiterate, 138 (80%) in the Sonagachi group and 148 (89%) in the NACO-only group (P = 0.026). The marital status also varied between the 2 groups (P < 0.0001) (Table 2). The proportion of unmarried sex workers in the Sonagachi group was significantly higher (P = 0.006) compared to NACO-only group. The Sonagachi sex workers had more clients, higher income, but shorter duration of sex work (P <0.0001) (Table 2). The NACO-only group had a higher proportion of women with no dependents (14%) than the Sonagachi group (5%) (P <0.01). There were no differences in the numbers of clients and proportion of clients who used condoms between those sex workers with and without dependents.
In both the Sonagachi and NACO-only groups, more than 70% had a knowledge score of 50% and above, and less than 10% had a score below 25% (P = 0.71). The overall scores for an optimistic attitude were higher in the Sonagachi group, with more than 77% having a score of more than 50%, while in the NACO-only group, less than 70% had a similar level (P <0.04).
A number of risk factors were found to be significantly different between the Sonagachi and NACO-only groups of sex workers (Table 3), including a higher proportion of Sonagachi sex workers who had regular STD check-ups, performed sex work only within a brothel, used a designated basket for disposal of used condoms, and preferred to visit a government clinic or hospital for treatment of STDs and were tested for HIV. Almost one-third of sex workers in both groups continued to engage in sexual intercourse during menstruation.
TABLE 3.
Number of Sex Workers in Each Group per Individual Risk Factor
| Risk Factor | Sonagachi Group No (%) | NACO-Only Group No (%) | P Value |
|---|---|---|---|
| 1 Ask clients to use condom | 166 (96) | 161 (95) | 0.80 |
| 2 Agree not to use condom | 81 (47) | 94 (56) | 0.11 |
| 3 Examine penis before sex | 143 (83) | 143 (85) | 0.66 |
| 4 Do not perform oral/anal sex | 161 (93) | 156 (92) | 0.78 |
| 5 Have sex during menstruation | 47 (27) | 52 (31) | 0.48 |
| 6 Sex work outside brothel | 36 (21) | 70 (41) | <0.0001 |
| 7 Dispose of condom in specific basket | 91 (53) | 50 (30) | <0.0001 |
| 8 Regular STD check-ups | 143 (83) | 82 (49) | <0.0001 |
| 9 Attend clinic/hospital for treatment of STD | 167 (97) | 127 (75) | <0.0001 |
| 10 Tested for HIV | 103 (60) | 45 (27) | <0.0001 |
| 11 Among those tested, tried to get test result | 92 (89) | 39 (87) | 0.51 |
Speculum examination was not carried out in women who were menstruating or who refused it. However, external genital examination findings were included in the analysis for those subjects who permitted it. Those who did not show any external signs of clinical STDs were not included in the analysis of outcome because a speculum examination had not been done. Five Sonagachi and 10 NACO-only group sex workers refused clinical examination, and 5 Sonagachi and 2 NACO-only group sex workers refused to give blood. Twenty-seven Sonagachi sex workers reported STD symptoms, of which 23 were clinically confirmed. The prevalence of individual STDs, presented in Table 4, was similar in both the groups.
TABLE 4.
Prevalence of STDs in the 2 Groups of Sex Workers
| Sexually Transmitted Disease | Sonagachi Group | NACO-Only Group |
|---|---|---|
| Genital ulcerative disease | 7 | 4 |
| Primary syphilis | 2 | 2 |
| Chancroid | 2 | — |
| Recurrent herpes genitalis | 3 | 1 |
| Donovanosis | — | 1 |
| Viral tumor | 13 | 7 |
| Condyloma acuminata | 7 | 4 |
| Molluscum contagiosum | 6 | 3 |
| Inguinal bubo | 2 | — |
| Lymphogranuloma venereum | 1 | — |
| Chancroid | 1 | — |
| Vaginal discharge | 24 | 31 |
| Candidiasis | 15 | 25 |
| Trichomoniasis | 5 | 4 |
| Physiological | 4 | 2 |
| Cervical discharge | 48 | 32 |
| Total with clinical STDs | 77 (46%) | 64 (39%) |
| Cervical smear Gram stain +ve | 29 (18%) | 24 (15%) |
| Serum RPR +ve | 3 | 11 |
| Serum TPHA +ve | 28 (16%) | 47 (28%) |
| Urine PCR for Ng +ve | 12 | 9 |
| Urine PCR for Ct +ve | 12 | 4 |
| Total with laboratory-proven STD | 42 (24%) | 43 (25%) |
| Total STDs | 98 (57%) | 88 (52%) |
Based on the laboratory results, 42 (24%) of the tested Sonagachi and 43 (25%) of the tested NACO-only group sex workers were found to have active STDs. The overall figures for active STDs, combining clinical and laboratory findings, were 98 for the Sonagachi and 88 for the NACO-only groups. The unadjusted odds ratio was 1.08 (95% CI: 0.68 – 1.72). Adjusting for variables such as age, number of clients, condom use, examining penis before sex work, and sex work outside brothel and during menstruation, the odds ratio was 1.07 (95% CI: 0.61–1.92). The prevalence of individual STDs did differ between the 2 groups. The Sonagachi women had a higher prevalence of chlamydia and a lower prevalence of active syphilis and candidiasis.
The prevalence of the individual STDs among the Sonagachi sex workers in 1992 and 2003 is shown in Table 1. There was a significant decline in the prevalence of syphilis, vaginal discharge, candidiasis, and trichomoniasis. The prevalence of a Gram-positive cervical smear, condyloma acuminate, and molluscum contagiosum did not change.
Age was shown to be an important risk factor for STDs, with an odds ratio of 2.7 and 2.2 for age groups 18 to 25 years and 26 to 35 years, respectively, relative to the age group over 35 years, when adjusting for group, number of clients, and other risk factors. The practice of not examining the penis before sex work had an OR of 1.9 for STDs (P < 0.047; 95% CI: 1.0 – 3.7).
The subjects of the 2 groups were categorized according to similarity of propensity scores into 5 subclasses, with approximately 20% of the total subjects in each subclass (Table 5). As there were missing values for certain variables for 39 sex workers, we could not obtain propensity scores for them. Eleven (28%) of those missing values were in the Sonagachi group, and 28 were in the NACO-only group. There was no significant difference between the Sonagachi and NACO-only groups in the proportion of STDs within any of the 5 subclasses (Table 6).
TABLE 5.
Distribution of Sonagachi and NACO-Only Sex Workers Assigned to Subclasses According to Their Propensity Scores
| Subclass | Propensity Score Range | Number of Subjects Sonagachi NACO-Only | Total Number (%) | |
|---|---|---|---|---|
| 1 | 0.03 to 0.21 | 6 | 53 | 59 (19.5) |
| 2 | <0.21 to 0.48 | 20 | 37 | 57 (18.8) |
| 3 | <0.48 to 0.63 | 33 | 27 | 60 (19.8) |
| 4 | <0.63 to 0.80 | 50 | 14 | 64 (21.1) |
| 5 | <0.80 to 1.00 | 53 | 10 | 63 (20.8) |
| Total | 162 | 141 | 103 (100) | |
TABLE 6.
Frequency of STDs in the Propensity Subclasses
| Subclass | STD Status | Intervention, No. (%) | Control, No. (%) | Total, No. (%) | P Value |
|---|---|---|---|---|---|
| 1 | Present | 3 (50) | 24 (47.1) | 27 (47.4) | 0.61 |
| Absent | 3 (50) | 27 (52.9) | 30 (52.6) | ||
| 2 | Present | 13 (65) | 19 (59.4) | 32 (61.5) | 0.68 |
| Absent | 7 (35) | 13 (40.6) | 20 (38.5) | ||
| 3 | Present | 21 (67.7) | 18 (75) | 39 (70.9) | 0.56 |
| Absent | 10 (32.3) | 6 (25) | 16 (29.1) | ||
| 4 | Present | 25 (53.2) | 6 (50) | 31 (52.5) | 0.84 |
| Absent | 22 (46.8) | 6 (50) | 28 (47.5) | ||
| 5 | Present | 30 (56.6) | 6 (60) | 36 (57.1) | 0.84 |
| Absent | 23 (43.4) | 4 (40) | 27 (42.9) |
Subclassification of propensity scores produced an unequal distribution of sex workers from the 2 groups within each subclass. The numbers of subjects in subclasses 2 and 3 were somewhat similar in both the groups. These 2 groups were merged to increase the number of subjects in the group and were tested for any difference in STD prevalence. None was found (P = 0.94).
Discussion
There were numerous difficulties encountered in performing this comparison. The sex workers in the Sonagachi area were younger than in the NACO-only area (P <0.0001). Sex workers are usually sold to the brothel owners in Calcutta when they are young. The mean age of sex workers reported at the baseline survey of the Sonagachi Project in 1992 was 23 years, with 85% of them in the 15-to 29-year age group. The lowest age was 13 years.10 The present survey did not include sex workers below the age of 18 years. The observed mean age of sex workers in the Project area was 27 years, with 76% in the 18- to 30-year age group. Thus, the age distribution among sex workers within the Project had not changed.
The education status of women in India, particularly in the villages, is low; about 80% of the sex workers were illiterate. Without education, these women cannot compete for better jobs. The 1992 survey of the Project reported that 84% of sex workers were illiterate,10 which is similar to our finding of 80% illiteracy among sex workers in the Project area. Similarly, the number of clients in 1992 varied between 2 and 10 per day, with an average of 3,10 while the current figures are 1 to 10, with a median of 3. These figures indicate that although many of the basic characteristics of the sex workers within the Project had not changed between 1992 and the current study, the prevalence of syphilis, vaginal discharge, candidiasis, and trichomoniasis had significantly declined in the Sonagachi sex workers.
It is not uncommon in India, particularly among people in the lower economic strata, for husbands to abandon their wives and children and not take care of them. The data showed that about half of the intervention and control sex workers were the victims of such a situation. These unfortunate women, additionally handicapped by illiteracy, are compelled to support themselves and their children through sex work.
The knowledge level of STDs/HIV did not differ between the Sonagachi and NACO-only groups of sex workers. Learning activities were provided to both of the groups by the West Bengal State AIDS Control Society, under the National AIDS Control Program. Only the scores for an optimistic attitude were marginally higher (P = 0.04) in the Sonagachi group. It is possible that the process of empowerment in the Sonagachi area influenced the attitudes of the sex workers.
Sex workers in the NACO-only group had fewer regular STD check-ups, more frequently visited hotels or customers’ homes for sex work, and more often did not dispose of used condoms properly. These factors would tend to increase the risk of STDs among sex workers in the control area. On the other hand, they had fewer clients.
Most sex workers of both the groups asked their clients to use condoms. However, because of the competitive market and the fear of losing the client, half in both groups agreed to unprotected sex if forced or offered extra money. The frequency of unprotected sex was similar in the 2 groups. However, at the 1992 survey before intervention, only 1% of sex workers reported regular use of condoms10; assuming both areas were similar in 1992, there has been considerable improvement in reported condom use in the 2 groups. The Sonagachi group was successful in promoting STD treatment and HIV testing, both of which are under the control of the sex workers. In negotiating with the client about condom use when she is alone, the Sonagachi sex workers were neither more nor less successful than the NACO-only sex workers.
No difference existed between the 2 groups in regards to the prevalence of all STDs combined, although active syphilis was higher in the NACO area, whereas laboratory-proven chlamydia and gonorrhea were higher in the Sonagachi area. However, the prevalence of STDs was low in both areas compared to the rates reported in 1992 in Sonagachi, as well as in red light areas in other parts of India or in other developing countries.11–14 The IEC activities and promotion of condoms instituted by the West Bengal State AIDS Control Society through NGOs might be responsible for this low prevalence of STDs among this high-risk group. The NACO also reported a low prevalence in the state of West Bengal in comparison to many other states of India.15
Stratified analysis grouping by propensity score was useful to reduce the problem of noncomparability of the total sample.8,9 The difference in STD prevalence in none of the similar individual subclasses was found to be significant. Even merging of subclasses to increase the number of subjects in each group failed to reveal any difference (P = 0.94).
Strong points of the current study were random sampling, a high number of cases in each group, evaluation of the status of the subjects through a standard questionnaire, and inclusion of laboratory studies, in addition to clinical reports. The prevalence of STDs considered in the calculation of sample size, however, was much higher than the observed prevalence. Thus, the power of the study was lower than originally calculated. Further, the participation of the sex workers from the NACO-only area was low. These sex workers might have been aware of their STD status and avoided participation. On the other hand, the opportunity of getting examined and treated anonymously by senior doctors at no cost should have encouraged them to participate. Therefore, the awareness of STD status might have affected the observed STD rates either up or down. There is always a possibility of misclassification of disease status in both clinical and laboratory reporting, but it should have been nondifferential, resulting only in a reduced probability of observing a difference.
In conclusion, the current study found the prevalence of all STDs among sex workers in Calcutta was the same in both the Sonagachi and NACO-only areas but was much lower than that observed in 1992. Thus, both the Sonagachi intervention and the West Bengal NACO intervention appear to have been successful. The Sonagachi intervention, however, appears to have had the additional benefit of significantly improving the treatment-seeking behavior and optimistic attitude of sex workers.
Acknowledgments
This research was supported by the NIH Fogarty AIDS International Training and Research Program (D43 TW000013).
References
- 1.Sharma VK, Bhargav R, Kar HK, et al. Global and national overview of HIV/AIDS epidemic. In: Sharma VK, editor. Textbook of Sexually Transmitted Diseases. New Delhi, India: Viva Books Pvt Ltd; 2003. pp. 68–76. [Google Scholar]
- 2.Jayasekera D. [Accessed December 18, 2004];AIDS becomes a serious health problem in India [World Socialist Web site] Available at: http://www.wsws.org/articles/2001/may2001/aids-m04.shtml.
- 3.Ford K, Wirawan DN, Reed BD, et al. The Bali STD/AIDS Study: evaluation of an intervention for sex workers. Sex Transm Dis. 2002;29:50–58. doi: 10.1097/00007435-200201000-00009. [DOI] [PubMed] [Google Scholar]
- 4.Bhave G, Lindan CP, Hudes ES, et al. Impact of an intervention on HIV, sexually transmitted diseases, and condom use among sex workers in Bombay, India. AIDS. 1995;9(suppl 1):S21–S30. [PubMed] [Google Scholar]
- 5.Nagelkerke NJ, Jha P, de Vlas SJ, et al. Modelling HIV/AIDS epidemics in Botswana and India: impact of interventions to prevent transmission. Bull World Health Organ. 2002;80:419–420. [PMC free article] [PubMed] [Google Scholar]
- 6.Dugger CW. Going brothel to brothel, prostitutes preach about using condoms. [Accessed December 18, 2004];New York Times. 1999 January 4; Available at: http://www.nytimes.com/library/world/asia/010499india-aids.htm.
- 7.Kirkwood BK. Essentials of Medical Statistics. Oxford, England: Blackwell Scientific Publications; 1988. p. 148. [Google Scholar]
- 8.Rosenbaum PR, Rubin DB. The central role of the propensity score in observational studies for causal effects. Biometrika. 1983;70:41–55. [Google Scholar]
- 9.Rosenbaum PR, Rubin DB. Reducing bias in observational studies using subclassification on the propensity score. J Am Stat Assoc. 1984;79:516–524. [Google Scholar]
- 10.Chakraborty AK, Jana S, Das A, et al. Community based survey of STD/HIV infection among commercial sex workers in Calcutta (India), part I: some social features of commercial sex workers. J Commun Dis. 1994;26:161–167. [PubMed] [Google Scholar]
- 11.Das A, Jana S, Chakraborty AK, et al. Community based survey of STD/HIV infection among commercial sex workers in Calcutta (India), part III: clinical findings of sexually transmitted diseases (STD) J Commun Dis. 1994;26:191–196. [PubMed] [Google Scholar]
- 12.Pal NK, Chakraborty MS, Das A, et al. Community based survey of STD/HIV infection among commercial sex workers in Calcutta (India), part IV: sexually transmitted diseases and related risk factors. J Commun Dis. 1994;26:197–202. [PubMed] [Google Scholar]
- 13.Desai VK, Kosambiya JK, Thakor HG, et al. Prevalence of sexually transmitted infections and performance of STI syndromes against aetiological diagnosis, in female sex workers of red light area in Surat, India. Sex Transm Infect. 2003;79:111–115. doi: 10.1136/sti.79.2.111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.van den Hoek A, Yuliang F, Dukers NH, et al. High prevalence of syphilis and other sexually transmitted diseases among sex workers in China: potential for fast spread of HIV. AIDS. 2001;15:753–759. doi: 10.1097/00002030-200104130-00011. [DOI] [PubMed] [Google Scholar]
- 15.National AIDS Control Organization (NACO) Observed HIV prevalence levels statewise: 1998–2004. http://www.nacoonline.og/facts_statewise.htm.