INTRODUCTION
Altered synaptic and structural plasticity has been proposed as one of the mechanisms of depression (Duman, 2002; Manji et al., 2001). Neurotrophins participate in the regulation of structural and morphological plasticity of central nervous system neurons as well as in synaptic connectivity and neurotransmission (McAllister et al., 1999; Thoenen, 2000). Among the neurotrophins, variations in the brain derived neurotrophic factor (BDNF) have been identified in several psychiatric disorders including mood disorders, schizophrenia, obsessive compulsive disorder, and Alzheimer's disease (Licinio and Wong, 2002). These observations suggest that BDNF has pleiotropic action relevant to complex behavioral disorders including depression.
BDNF has been implicated in the pathogenesis of depression and the mechanism of action of antidepressant agents (Dwivedi, 2009). Animal studies have shown that antidepressant agents increase the expression of the BDNF gene in hippocampal structures, areas related to regulation of affect and of other functions that are abnormal during depression (Nibuya et al., 1995). Further, infusion of BDNF in the dentate gyrus of the hippocampus has led to antidepressant responses in the forced swim and the learned helplessness animal models of depression (Shirayama et al., 2002). Human autopsy studies showed that antidepressants increase BDNF immunoreactivity in the dentate gyrus, hilus and supragranular regions (Chen et al., 2001). Moreover, antidepressants normalize serum BDNF levels (Aydemir et al., 2005; Gonul et al., 2005) that are reduced during depression (Karege et al., 2002). Emerging literature suggests that BDNF allelic status may influence the response of depression to antidepressants (Choi et al., 2006; Licinio et al., 2009).
BDNF is expressed by a gene on chromosome 11p13 that encodes a BDNF precursor peptide. The BDNF precursor is accumulated in the Golgi apparatus, where sortilin facilitates its correct folding into a mature domain, and after binding with carboxypeptidase E, it is sorted into a secretory pathway (Dwivedi, 2009; Lu et al., 2005). While several BDNF polymorphisms have been studied in their relationship to antidepressant response, this study focused on the single nucleotide polymorphism (rs6265) at nucleotide position 196/758 consisting of a valine (val) to methionine (met) substitution at codon 66 in the prodomain (Bath and Lee, 2006; Egan et al., 2003). There are three reasons for this choice. First, the BDNFmet polymorphism is common (The International HapMap Project, 2003). Second, the BDNFmet genotype has been identified as a risk factor for geriatric depression (Hwang et al., 2006; Taylor et al., 2007). Third, BDNFmet affects activity-dependent BDNF secretion, critical for dendritic trafficking (Bath and Lee, 2006; Chen et al., 2004; Egan et al., 2003), and synaptic plasticity (Martinowich et al., 2007). Rats transfected with BDNFmet have impaired BDNF production and distribution in several brain areas compared to rats with BDNFval/val genotype (Egan et al., 2003).
Late-life depression is often accompanied by white matter abnormalities (Alexopoulos, 2005). It has been proposed that white matter abnormalities compromising frontolimbic circuitry may predispose to geriatric depression and interfere with its response to pharmacotherapy (Alexopoulos, 2005) . BDNF polymorphisms may influence white matter integrity in older adults since BDNF influences neuron survival, neurogenesis, and synaptic connectivity in the adult brain (Bath and Lee, 2006; Carlson et al., 2006; Egan et al., 2003). Moreover, BDNF is expressed in areas related to mood regulation, including the frontal cortex, hippocampus, striatum, and thalamus (Bath and Lee, 2006). Thus a critical question is whether promoting white matter changes is a mechanism by which BDNF allelic status influences the response of geriatric depression to antidepressants.
This analysis focused on remission rates of the subset of depressed elderly Caucasian patients participating in an escitalopram treatment trial (Alexopoulos et al., 2008) who also had genotypic characterization. Remission was selected as the outcome variable because it is viewed as the optimal target of the acute treatment of depression. Depressed patients who achieve remission are left with less disability and are three times less likely to relapse than depressed patients left with residual symptoms (Judd et al., 1998). The objectives of this analysis were: 1) To test the hypothesis that BDNFval/met allelic status influences the remission rate of late-life depression; 2) to explore whether the relationship between BDNF allelic status and remission of late-life depression is influenced by the presence of microstructural white matter abnormalities.
METHOD
Subjects
The subjects were consecutively recruited individuals aged 60 years and older, who met DSM-IV criteria for unipolar major depression without psychotic features and had a score of 18 or greater on the 24-item Hamilton Depression Rating Scale (HDRS) (Hamilton, 1960) . After description of the study in lay terms, subjects signed written informed consent approved by the IRBs of Weill-Cornell Medical College and the Nathan Kline Institute.
Exclusion criteria were: 1) History of other axis I psychiatric disorders prior to the onset of depression; 2) presence of delirium, history of stroke, head trauma, multiple sclerosis, or brain degenerative diseases; 3) metastatic cancer, brain tumors, unstable cardiac, hepatic, or renal disease, myocardial infarction, or stroke within the 3 months preceding the study; 4) lymphoma, pancreatic cancer, or endocrinopathies other than diabetes; 5) treatment with steroids, alpha-methyl-dopa, clonidine, reserpine, tamoxifen, or cimetidine; 6) Mini-Mental State Examination score < 24 (Folstein et al., 1975), and 7) metal implants.
Assessment
DSM-IV diagnosis was based on the SCID-R, administered at entry to the study. Depressive symptoms were assessed using the 24-item HDRS. Cognitive impairment was rated with the Mini Mental State Examination (MMSE) (Folstein et al., 1975) and disability with the World Health Organization Disability Assessment Scale (WHODAS-II) (Epping-Jordan and Ustun, 2000).
Treatment
The subjects had a 2-week, single-blind, placebo drug-wash-out phase at the end of which they had an MRI scan. Subjects who still met DMS-IV criteria for major depression and had HDRS≥18 received controlled treatment with escitalopram 10 mg daily for 12 weeks. Subjects received their medication in one-week supply blisters.
Depressed subjects were assessed weekly. Follow-up meetings consisted of a rating session with a research assistant followed by a brief session with a research psychiatrist. Research assistants administered the HDRS, obtained vital signs, questioned the subjects about medication adherence and inspected the escitalopram blister package. No subject received psychotherapy. Remission was defined as HDRS≤7 for two consecutive weeks and absence of DSM-IV diagnosis of depression.
Genotyping
Genomic DNA was isolated from whole blood samples using the QIAamp DNA blood kit (Qiagen) according to the manufacturer's standard protocol. The BDNF Val66Met polymorphism (rs6265) was genotyped using a commercially available Taqman 5’-exonuclease real-time PCR assay (ABI; C__11592758_10). All reaction were run using an ABI 7900HT using both real time detection of amplification of each allele and endpoint reading of allelic ratios. Genotypes were called by visual inspection of the real time traces and automated genotype calling of endpoint data. All samples which did not meet quality criteria for automated genotype calling and/or gave discordant genotype calls in the real-time were re-run in duplicate. All samples that required re-run provided concordant genotypes on re-run. The genotype distribution at rs6265 was in Hardy-Weinberg equilibrium.
MRI scans were obtained with the 1.5T Siemens Vision Scanner housed at the Nathan Kline Institute Center for Advanced Brain Imaging. Patients received a magnetization prepared rapidly acquired gradient echo (MPRAGE) scan (TR=11.6ms, TE=4.9ms, matrix=256x256, FOV=320mm, NEX=1, slice thickness = 1.25 mm, 172 slices, no gap), as well as a turbo dual spin echo scan (TSE; TR=ms, TE=22/90ms, matrix=256x256, FOV=240mm, slice thickness = 5mm, 26 slices, no gap), and a diffusion tensor imaging scan (TR=6000ms, TE=100ms, matrix=128x128, FOV=320mm, NEX=7, slice thickness = 5mm, 19 slices, no gap). For the DTI scan, eight diffusion sensitization directions were used (with b=1000 s/mm2 along with an image with no diffusion weighting (b=0 s/mm2). The TSE and DTI scans were acquired in an oblique axial plane parallel to the anterior commissure–posterior commissure axis.
We examined FA in specific regions of interest (ROIs) using the Reproducible Object Quantification Scheme (ROQS) software that operates on non-normalized data sets. ROQS relies on fiber orientation information calculated from the diffusion tensor to define the boundary of anatomically distinct white matter tracts in a semi-automated manner (Niogi et al., 2007). The user chooses a seed pixel within the structure of interest and an algorithm uses the properties of this pixel to determine the appropriate boundary. Once the boundary of the white matter tract is determined, mean and standard deviation values of FA from pixels within the boundary are automatically determined for each ROI. The ROQS technique has been shown to be more reproducible and more reliable than hand-drawn ROIs (Niogi et al., 2007).
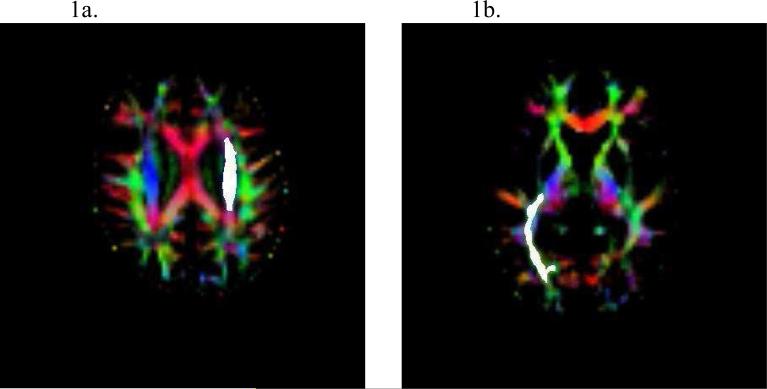
The following white matter ROIs were examined: the centrum semiovale, the cingulum, the superior and anterior corona radiata, the superior and inferior longitudinal fasciculi, the posterior limb of the internal capsule, the body, genu, and splenium of the corpus callosum and the uncinate fasciculus. Figure 1 shows examples of the superior corona radiata and the inferior longitudinal fasciculus. Both intra and inter-rater reliability were established for each ROI using 10 randomly selected brains from our sample. The intraclass correlation formula for two random raters (2) (Shrout and Fleiss, 1979) was used, and the resulting intra- and inter-rater reliability estimates for all ROIs exceeded 0.90. All structures were measured separately for each hemisphere.
Figure 1.
Left superior corona radiata ROI (Fig 1a). Right inferior longitudinal fasciculus ROI (Fig 1b) as estimated by ROQS. Images are in radiological view.
Data Analysis
Initially, t-tests and chi-square tests were used to identify demographic and clinical variables distinguishing depressed subjects who achieved remission from those who remained symptomatic. The hypothesis related to remission rates between depressed, met allele carriers and val homogygotes was tested with logistic regression using as covariates variables with different distribution in remitters and non-remitters. To pursue hypotheses on the relationship of BDNF allele status and microstructural white matter abnormalities, first, we compared FA of specific brain regions between remitters and non-remitters using t-tests. Then, we constructed hierarchical logistic regression models predictive of remission in which we entered BDNF allele status and age of onset first, followed by FA of regions associated with remission status. Finally, the BDNF allele status by FA region interaction was entered in the regression model in order to ascertain whether the relationship of BDNF allele status to remission was influenced by FA. Two tailed significance tests were used in all comparisons.
RESULTS
A total of 43 depressed elderly subjects met selection criteria, signed informed consent and entered the study. After the single-blind, drug washout placebo phase, 34 continued to meet DSM-IV criteria for major depression, had an HDRS score equal to or higher than 18 and entered the escitalopram treatment phase. There were no significant differences in age, education, severity of depression (HDRS) at baseline, index episode duration, age of first depressive episodes, or number of previous episodes between subjects who responded to placebo and those who remained symptomatic and entered the escitalopram trial.
Of the 34 subjects, two had one week of treatment and exited the study (one did not see the need to continue antidepressant treatment, and one due to inter-current medical events). Of the 32 subjects who completed the treatment phase, 17 achieved remission and 15 continued to experience significant depressive symptoms and signs. There were no significant differences in demographic or clinical characteristics between depressed patients who achieved remission and those who remained depressed (Table 1).
TABLE 1.
Baseline Demographic and Clinical Data of 32 Elderly Patients with Major Depression Treated with Escitalopram 10 mg Daily.
| Variable |
Remitters (N=17) |
Non-Remitters (N=15) |
Wilcoxon Statistics |
|||
|---|---|---|---|---|---|---|
| Mean | SD | Mean | SD | Z | p | |
| Age (years) | 69.2 | 6.0 | 71.7 | 7.4 | −0.81 | 0.43 |
| Education (years) | 16.4 | 3.1 | 15.5 | 4.7 | −0.08 | 0.94 |
| Baseline HDRS* | 21.9 | 4.3 | 21.6 | 2.4 | −0.50 | 0.63 |
| Anxiety Psychic | 2.2 | 0.95 | 2.1 | 1.0 | −0.06 | 0.97 |
| Anxiety Somatic | 1.2 | 1.0 | 1.67 | 0.72 | −1.51 | 0.17 |
| Agitation | 0.29 | 0.59 | 0.13 | 0.35 | −0.78 | 0.60 |
| Hypochondriasis | 0.41 | 0.62 | 0.33 | 0.62 | −0.47 | 0.71 |
| Anxiety Factor of HDRS** | 4.1 | 1.9 | 4.2 | 1.3 | −0.30 | 0.79 |
| Age of Onset (years) | 56.6 | 16.0 | 53.6 | 17.7 | −0.57 | 0.58 |
| Number of Previous Episodes | 2.4 | 1.5 | 2.7 | 1.4 | −0.65 | 0.53 |
| DRS Total | 136.8 | 5.7 | 133.8 | 8.1 | −1.50 | 0.14 |
| Mini Mental State Examination | 28.7 | 1.5 | 27.8 | 1.9 | −1.51 | 0.14 |
24-item Hamilton Depression Rating Scale
Sum of HDRS items psychic anxiety, somatic anxiety, agitation, and hypochondriasis
Among patients who completed the escitalopram treatment trial, 17 were met allele carriers (1 met/met and 16 val/met) and 15 were val allele homozygotes. There were no significant differences in age, gender, education, severity of depression at entry (HDRS), index episode duration, and number of previous episodes. However, val homogygotes (BDNFval/val) had a later age of illness onset (mean: 64.7 years, SD: 6.9) than met allele carriers (BDNFmet mean: 46.7 years, SD: 19.0; z=2.3, p<0.01). For this reason, subsequent comparisons used age of onset as covariate.
BDNFval/val subjects had lower remission rates (40.0%) than BDNFmet carriers (64.7%) in a model taking age of onset into account (BDNF allele Wald □2=4.1, df=1, p<0.043; onset Wald □2=2.33, p<0.13). Earlier studies (Alexopoulos et al., 2002), showed that failure to achieve remission is associated with microstructural white matter abnormalities in various brain areas. In this sample, depressed elderly patients who failed to achieve remission had lower fractional anisotropy (FA) than those who achieved remission in three areas: body of the corpus callosum (mean: 0.43, SD: 0.05 vs. 0.46, SD: 0.05, t=1.87, df=30, p<0.07), left superior corona radiata (mean: 0.42, SD: 0.04 vs. 0.46, SD: 0.04, t=2.61, df=30, p<0.014) and right inferior longitudinal fasciculum (mean: 0.40, SD: 0.03 vs. 0.43, SD: 0.03, t=2.15, df=30, P<0.04).
To determine whether the effect of BDNF alleles on remission is influenced by white matter microstructural abnormalities (FA), hierarchical regression was conducted in which BDNF alleles and age of onset were entered first, followed by the FA values of brain areas associated with non-remission (Table 2). The model that included the corpus callosum FA predicted 35 percent of the variance in remission rates. A similar percentage of the variance in remission rates (32 percent) was predicted by the model that included FA in the left superior corona radiata. However, a lower percentage of the variance (24 percent) was predicted by the model that included FA of the right inferior longitudinal fasciculum FA. In each of the three models, the interaction between BDNF alleles and the FA variable did not contribute to the variance in predicting remission.
Table 2.
BDNF Allele and Fractional Anisotropy: Relationship to Remission in 32 Elderly Patients with Major Depression Treated with Escitalopram.
| Variables | Likelihood Ratio χ2 | p |
|---|---|---|
| Model A 1 | ||
| BDNF Genotype | 5.5 | 0.019 |
| Age of Onset† | 2.4 | 0.120 |
| Corpus Callosum FA | 4.9 | 0.027 |
| Model B 2 | ||
| BDNF Genotype | 3.6 | 0.056 |
| Age of Onset† | 3.9 | 0.049 |
| Left Superior Corona Radiata FA | 4.0 | 0.046 |
| Model C 3 | ||
| BDNF Genotype | 2.5 | 0.115 |
| Age of Onset† | 2.4 | 0.119 |
| Right Inferior Longitudinal Fasciculum FA | 2.1 | 0.146 |
Proportional Hazards Likelihood Ratio χ2=12.35, df=3, p<0.063 (R2=35)
Proportional Hazards Likelihood Ratio χ2=11.18, df=3, p<0.011 (R2=32)
Proportional Hazards Likelihood Ratio χ2=7.94, df=3, p<0.047 (R2=24)
Age of onset of first depressive episode
DISCUSSION
The principal finding of this study is that depressed older Caucasian patients with the BDNFmet carriers were more likely to achieve remission than BDNFval/val homozygotes after 12 weeks of treatment with escitalopram 10 mg daily. Microstructural abnormalities in the body of the corpus callosum, the left superior corona radiata, and the right inferior longitudinal fasciculum were also associated with lower remission rate. However, there were no significant interactions between BDNF allele status and microstructural abnormalities in predicting remission of geriatric depression.
This is the first study, to our knowledge, to identify a relationship between BDNF-gene Val66Met polymorphism and remission of late-life depression and to investigate the role of white matter abnormalities. However, the relationship of BDNF val66met genotype and remission of geriatric depression is consistent with findings in younger Asian populations. Specifically, a study of Korean younger depressed adults observed that those with the BDNFval/met genotype were more likely to respond to citalopram than subjects with the BDNFval/val genotype (Choi et al., 2006). Similar findings were reported in Japanese younger adults treated with antidepressants over 6 weeks (Yoshida et al., 2007). In this study, depressed patients with the BDNFval/met polymorphism had greater improvement of depressive symptoms compared to patients with other BDNF polymorphisms (Yoshida et al., 2007). Finally, a trend towards greater response to fluoxetine was noted in depressed, Taiwanese younger adults with the BDNFval/met genotype (Tsai, 2003). Nonetheless, a study in Spanish sample failed to demonstrate an association between the BDNF val66met polymorphism and remission of depression in younger adults (Gratacos et al., 2008).
This study has several limitations, including the likelihood that clinical factors may influence remission rates, the focus on a single BDNF polymorphism, and the small number of subjects. In this sample, demographic and clinical factors were similarly distributed among remitters and non-remitter with the exception of age of onset of first depressive episode. Age of onset was taken into account in analyses of predictors of remission. There are reports of numerous polymorphisms at the BDNF locus in human populations some of which have been associated with depression and antidepressant response (Licinio et al., 2009). We have focused on the val66met polymorphism in this study because it is common, influences BDNF secretion, and is the only BDNF polymorphism with a known molecular phenotype (Chen et al., 2004; Egan et al., 2003). Finally, the small number of subjects mandates that our findings should be viewed as preliminary.
The relationship of BDNF to antidepressant response is complex. The effects of BDNF in the brain vary depending on the location in which it is expressed. In the ventral tegmental area and the nucleus accumbens, direct administration of BDNF increased behaviors associated with enhanced response to reward, including locomotor activity and conditioned reward to cocaine (Horger et al., 1999). However, administration of BDNF in the ventral tegmental area exerts a depressogenic effect in animal models and blockade of BDNF action in the nucleus accumbens has an antidepressant-like effect (Eisch et al., 2003). Similarly, selective ablation of the BDNF gene in the rat nucleus accumbens reduces depression-like behavior in response to social defeat stress (Berton et al., 2006). Unlike the ventral tegmental area and the nucleus accumbens, where BDNF may promote depression-like behavior, BDNF may be related to antidepressant action in the hippocampus. Specifically, antidepressants induce the expression of BDNF in the hippocampus, an effect thought to reverse neuronal atrophy and cell death and promote antidepressant response (Duman and Monteggia, 2006). However, BDNF is not necessary for antidepressant-like response in animal models (Conti et al., 2002).
The opposite effects of BDNF on the one hand in the ventral tegmental area and the nucleus accumbens and on the other in the hippocampus pose a challenge to understanding the relationship of the BDNFmet genotype to remission of geriatric depression. The treatment trial in this study consisted of a selective serotonin reuptake inhibitor. Complex interactions between BDNF and the serotonin system have been identified. These include promotion by BDNF of the function, growth and sprouting of serotonin neurons (Mamounas et al., 2000), increase of serotonin synthesis (Siuciak et al., 1998) and decrease of serotonin uptake (Mossner et al., 2000). Therefore, further serotonin uptake inhibition by escitalopram may not have been helpful in BDNFval/val depressed patients in whom BDNF is adequately expressed. Such patients may require antidepressants with a different mode of action assuming that depression is driven by factors other than serotonin deregulation in some of them. An alternative hypothesis is that the expression of BDNF in the ventral tegmental area and the nucleus accumbens of BDNFval/val has a depressogenic effect that may not be adequately corrected through enhancement of the serotonin system. Nonetheless, these hypotheses need to be tested with specifically designed studies.
Along with genetic factors, aging related changes compromising frontolimbic circuitry may contribute to geriatric depression and its treatment response (Alexopoulos, 2005). Depressed elders have microstructural (Nobuhara et al., 2006) and macromolecular (Gunning-Dixon et al., 2008; Kumar et al., 2004) white matter abnormalities in frontolimbic pathways. White matter hyperintensities have been associated with chronicity of geriatric depression (Simpson et al., 1998), although some disagreement exists (Salloway et al., 2002). Depressed elderly patients who remained symptomatic after treatment with SSRIs (Alexopoulos et al., 2002; Alexopoulos et al., 2008) had more microstructural white matter abnormalities in several frontolimbic white matter areas compared to depressed elders who achieved remission.
In this study, microstructural white matter abnormalities in several areas were associated with low remission rate. Our expectation was that the BDNFval/val polymorphism would have a protective effect and reverse the adverse effect of white matter abnormalities on outcomes of depression. Our reason was based on findings suggesting that BDNFval/val is associated with higher dendritic complexity and increased number of both neuronal and glia cells perhaps by enhancing neurogenesis or decreasing cell death (Bath and Lee, 2006; Vicario-Abejon et al., 1998) and repair after injury (Lu et al., 2005). However, the lack of interaction between BDNF allele status and white matter abnormalities in predicting remission did not support our expectation.
Acknowledgments
The authors thank Raj Sangoi RT ( R ) MR for his work as chief MR technologist and Dean Catalano for his work with MRI acquisition and data management.
Role of Funding Source
Personnel and imaging cost of this work was supported by NIMH grants R01 MH079414, R01 MH065653, P030 MH085943, T32 MH019132 (GSA), K23 MH067702 (CFM), K23 MH074818 (FGD), the Sanchez Foundation, and TRU Foundation. Escitalopram and placebo were provided free of cost by Forest Pharmaceuticals, Inc.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Disclosure/Conflict of Interest
Dr. Alexopoulos has received research grants by Forest Pharmaceuticals, Inc. and Cephalon and participated in scientific advisory board meetings of Forest Pharmaceuticals and Sanofi Aventis. He has given lectures supported by Forest, Bristol Meyers Squibb, Janssen, and Lilly and owns equity of Johnson and Johnson.
Drs. Gunning, Murphy, Glatt, Kelly, Lim, Morimoto and Hoptman, and Ms. Kanellopoulos report no competing interests.
REFERENCES
- The International HapMap Project Nature. 2003;426:789–796. doi: 10.1038/nature02168. [DOI] [PubMed] [Google Scholar]
- Alexopoulos GS. Depression in the elderly. Lancet. 2005;365:1961–1970. doi: 10.1016/S0140-6736(05)66665-2. [DOI] [PubMed] [Google Scholar]
- Alexopoulos GS, Kiosses DN, Choi SJ, Murphy CF, Lim KO. Frontal white matter microstructure and treatment response of late-life depression: a preliminary study. Am J Psychiatry. 2002;159:1929–1932. doi: 10.1176/appi.ajp.159.11.1929. [DOI] [PubMed] [Google Scholar]
- Alexopoulos GS, Murphy CF, Gunning-Dixon FM, Latoussakis V, Kanellopoulos D, Klimstra S, Lim KO, Hoptman MJ. Microstructural white matter abnormalities and remission of geriatric depression. Am J Psychiatry. 2008;165:238–244. doi: 10.1176/appi.ajp.2007.07050744. [DOI] [PubMed] [Google Scholar]
- Aydemir O, Deveci A, Taneli F. The effect of chronic antidepressant treatment on serum brain-derived neurotrophic factor levels in depressed patients: a preliminary study. Prog Neuropsychopharmacol Biol Psychiatry. 2005;29:261–265. doi: 10.1016/j.pnpbp.2004.11.009. [DOI] [PubMed] [Google Scholar]
- Bath KG, Lee FS. Variant BDNF (Val66Met) impact on brain structure and function. Cogn Affect Behav Neurosci. 2006;6:79–85. doi: 10.3758/cabn.6.1.79. [DOI] [PubMed] [Google Scholar]
- Berton O, McClung CA, Dileone RJ, Krishnan V, Renthal W, Russo SJ, Graham D, Tsankova NM, Bolanos CA, Rios M, Monteggia LM, Self DW, Nestler EJ. Essential role of BDNF in the mesolimbic dopamine pathway in social defeat stress. Science. 2006;311:864–868. doi: 10.1126/science.1120972. [DOI] [PubMed] [Google Scholar]
- Carlson PJ, Singh JB, Zarate CA, Jr., Drevets WC, Manji HK. Neural circuitry and neuroplasticity in mood disorders: insights for novel therapeutic targets. NeuroRx. 2006;3:22–41. doi: 10.1016/j.nurx.2005.12.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen B, Dowlatshahi D, MacQueen GM, Wang JF, Young LT. Increased hippocampal BDNF immunoreactivity in subjects treated with antidepressant medication. Biol Psychiatry. 2001;50:260–265. doi: 10.1016/s0006-3223(01)01083-6. [DOI] [PubMed] [Google Scholar]
- Chen ZY, Patel PD, Sant G, Meng CX, Teng KK, Hempstead BL, Lee FS. Variant brain-derived neurotrophic factor (BDNF) (Met66) alters the intracellular trafficking and activity-dependent secretion of wild-type BDNF in neurosecretory cells and cortical neurons. J Neurosci. 2004;24:4401–4411. doi: 10.1523/JNEUROSCI.0348-04.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Choi MJ, Kang RH, Lim SW, Oh KS, Lee MS. Brain-derived neurotrophic factor gene polymorphism (Val66Met) and citalopram response in major depressive disorder. Brain Res. 2006;1118:176–182. doi: 10.1016/j.brainres.2006.08.012. [DOI] [PubMed] [Google Scholar]
- Conti AC, Cryan JF, Dalvi A, Lucki I, Blendy JA. cAMP response element-binding protein is essential for the upregulation of brain-derived neurotrophic factor transcription, but not the behavioral or endocrine responses to antidepressant drugs. J Neurosci. 2002;22:3262–3268. doi: 10.1523/JNEUROSCI.22-08-03262.2002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Duman RS. Pathophysiology of depression: the concept of synaptic plasticity. Eur Psychiatry. 2002;17(Suppl 3):306–310. doi: 10.1016/s0924-9338(02)00654-5. [DOI] [PubMed] [Google Scholar]
- Duman RS, Monteggia LM. A neurotrophic model for stress-related mood disorders. Biol Psychiatry. 2006;59:1116–1127. doi: 10.1016/j.biopsych.2006.02.013. [DOI] [PubMed] [Google Scholar]
- Dwivedi Y. Brain-derived neurotrophic factor: role in depression and suicide. Neuropsychiatr Dis Treat. 2009;5:433–449. doi: 10.2147/ndt.s5700. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Egan MF, Kojima M, Callicott JH, Goldberg TE, Kolachana BS, Bertolino A, Zaitsev E, Gold B, Goldman D, Dean M, Lu B, Weinberger DR. The BDNF val66met polymorphism affects activity-dependent secretion of BDNF and human memory and hippocampal function. Cell. 2003;112:257–269. doi: 10.1016/s0092-8674(03)00035-7. [DOI] [PubMed] [Google Scholar]
- Eisch AJ, Bolanos CA, de Wit J, Simonak RD, Pudiak CM, Barrot M, Verhaagen J, Nestler EJ. Brain-derived neurotrophic factor in the ventral midbrain-nucleus accumbens pathway: a role in depression. Biol Psychiatry. 2003;54:994–1005. doi: 10.1016/j.biopsych.2003.08.003. [DOI] [PubMed] [Google Scholar]
- Epping-Jordan J, Ustun T. The WHODAS-II: leveling the playing field for all disorders. WHO Mental Health Bulletin. 2000;6:5–6. [Google Scholar]
- Folstein MF, Folstein SE, McHugh PR. “Mini-mental state”. A practical method for grading the cognitive state of patients for the clinician. J Psychiatr Res. 1975;12:189–198. doi: 10.1016/0022-3956(75)90026-6. [DOI] [PubMed] [Google Scholar]
- Gonul AS, Akdeniz F, Taneli F, Donat O, Eker C, Vahip S. Effect of treatment on serum brain-derived neurotrophic factor levels in depressed patients. Eur Arch Psychiatry Clin Neurosci. 2005;255:381–386. doi: 10.1007/s00406-005-0578-6. [DOI] [PubMed] [Google Scholar]
- Gratacos M, Soria V, Urretavizcaya M, Gonzalez JR, Crespo JM, Bayes M, de Cid R, Menchon JM, Vallejo J, Estivill X. A brain-derived neurotrophic factor (BDNF) haplotype is associated with antidepressant treatment outcome in mood disorders. Pharmacogenomics J. 2008;8:101–112. doi: 10.1038/sj.tpj.6500460. [DOI] [PubMed] [Google Scholar]
- Gunning-Dixon FM, Hoptman MJ, Lim KO, Murphy CF, Klimstra S, Latoussakis V, Majcher-Tascio M, Hrabe J, Ardekani BA, Alexopoulos GS. Macromolecular White Matter Abnormalities in Geriatric Depression: A Magnetization Transfer Imaging Study. Am J Geriatr Psychiatry. 2008 doi: 10.1097/JGP.0b013e3181602a66. [DOI] [PubMed] [Google Scholar]
- Hamilton M. A rating scale for depression. Journal of Neurological Neurosurgery in Psychiatry. 1960;23:56–62. doi: 10.1136/jnnp.23.1.56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Horger BA, Iyasere CA, Berhow MT, Messer CJ, Nestler EJ, Taylor JR. Enhancement of locomotor activity and conditioned reward to cocaine by brain-derived neurotrophic factor. J Neurosci. 1999;19:4110–4122. doi: 10.1523/JNEUROSCI.19-10-04110.1999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hwang JP, Tsai SJ, Hong CJ, Yang CH, Lirng JF, Yang YM. The Val66Met polymorphism of the brain-derived neurotrophic-factor gene is associated with geriatric depression. Neurobiol Aging. 2006;27:1834–1837. doi: 10.1016/j.neurobiolaging.2005.10.013. [DOI] [PubMed] [Google Scholar]
- Judd LL, Akiskal HS, Maser JD, Zeller PJ, Endicott J, Coryell W, Paulus MP, Kunovac JL, Leon AC, Mueller TI, Rice JA, Keller MB. Major depressive disorder: a prospective study of residual subthreshold depressive symptoms as predictor of rapid relapse. J Affect Disord. 1998;50:97–108. doi: 10.1016/s0165-0327(98)00138-4. [DOI] [PubMed] [Google Scholar]
- Karege F, Perret G, Bondolfi G, Schwald M, Bertschy G, Aubry JM. Decreased serum brain-derived neurotrophic factor levels in major depressed patients. Psychiatry Res. 2002;109:143–148. doi: 10.1016/s0165-1781(02)00005-7. [DOI] [PubMed] [Google Scholar]
- Kumar A, Gupta RC, Albert Thomas M, Alger J, Wyckoff N, Hwang S. Biophysical changes in normal-appearing white matter and subcortical nuclei in late-life major depression detected using magnetization transfer. Psychiatry Res. 2004;130:131–140. doi: 10.1016/j.pscychresns.2003.12.002. [DOI] [PubMed] [Google Scholar]
- Licinio J, Dong C, Wong ML. Novel sequence variations in the brain-derived neurotrophic factor gene and association with major depression and antidepressant treatment response. Arch Gen Psychiatry. 2009;66:488–497. doi: 10.1001/archgenpsychiatry.2009.38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Licinio J, Wong ML. Brain-derived neurotrophic factor (BDNF) in stress and affective disorders. Mol Psychiatry. 2002;7:519. doi: 10.1038/sj.mp.4001211. [DOI] [PubMed] [Google Scholar]
- Lu B, Pang PT, Woo NH. The yin and yang of neurotrophin action. Nat Rev Neurosci. 2005;6:603–614. doi: 10.1038/nrn1726. [DOI] [PubMed] [Google Scholar]
- Mamounas LA, Altar CA, Blue ME, Kaplan DR, Tessarollo L, Lyons WE. BDNF promotes the regenerative sprouting, but not survival, of injured serotonergic axons in the adult rat brain. J Neurosci. 2000;20:771–782. doi: 10.1523/JNEUROSCI.20-02-00771.2000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Manji HK, Drevets WC, Charney DS. The cellular neurobiology of depression. Nat Med. 2001;7:541–547. doi: 10.1038/87865. [DOI] [PubMed] [Google Scholar]
- Martinowich K, Manji H, Lu B. New insights into BDNF function in depression and anxiety. Nat Neurosci. 2007;10:1089–1093. doi: 10.1038/nn1971. [DOI] [PubMed] [Google Scholar]
- McAllister AK, Katz LC, Lo DC. Neurotrophins and synaptic plasticity. Annu Rev Neurosci. 1999;22:295–318. doi: 10.1146/annurev.neuro.22.1.295. [DOI] [PubMed] [Google Scholar]
- Mossner R, Daniel S, Albert D, Heils A, Okladnova O, Schmitt A, Lesch KP. Serotonin transporter function is modulated by brain-derived neurotrophic factor (BDNF) but not nerve growth factor (NGF). Neurochem Int. 2000;36:197–202. doi: 10.1016/s0197-0186(99)00122-9. [DOI] [PubMed] [Google Scholar]
- Nibuya M, Morinobu S, Duman RS. Regulation of BDNF and trkB mRNA in rat brain by chronic electroconvulsive seizure and antidepressant drug treatments. J Neurosci. 1995;15:7539–7547. doi: 10.1523/JNEUROSCI.15-11-07539.1995. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Niogi SN, Mukherjee P, McCandliss BD. Diffusion tensor imaging segmentation of white matter structures using a Reproducible Objective Quantification Scheme (ROQS). Neuroimage. 2007;35:166–174. doi: 10.1016/j.neuroimage.2006.10.040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nobuhara K, Okugawa G, Sugimoto T, Minami T, Tamagaki C, Takase K, Saito Y, Sawada S, Kinoshita T. Frontal white matter anisotropy and symptom severity of late-life depression: a magnetic resonance diffusion tensor imaging study. J Neurol Neurosurg Psychiatry. 2006;77:120–122. doi: 10.1136/jnnp.2004.055129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Salloway S, Boyle PA, Correia S, Malloy PF, Cahn-Weiner DA, Schneider L, Krishnan KR, Nakra R. The relationship of MRI subcortical hyperintensities to treatment response in a trial of sertraline in geriatric depressed outpatients. Am J Geriatr Psychiatry. 2002;10:107–111. [PubMed] [Google Scholar]
- Shirayama Y, Chen AC, Nakagawa S, Russell DS, Duman RS. Brain-derived neurotrophic factor produces antidepressant effects in behavioral models of depression. J Neurosci. 2002;22:3251–3261. doi: 10.1523/JNEUROSCI.22-08-03251.2002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shrout PE, Fleiss JL. Intraclass correlations: uses in assessing rater reliability. Psychol Bull. 1979;86:420–428. doi: 10.1037//0033-2909.86.2.420. [DOI] [PubMed] [Google Scholar]
- Simpson S, Baldwin RC, Jackson A, Burns AS. Is subcortical disease associated with a poor response to antidepressants? Neurological, neuropsychological and neuroradiological findings in late-life depression. Psychol Med. 1998;28:1015–1026. doi: 10.1017/s003329179800693x. [DOI] [PubMed] [Google Scholar]
- Siuciak JA, Clark MS, Rind HB, Whittemore SR, Russo AF. BDNF induction of tryptophan hydroxylase mRNA levels in the rat brain. J Neurosci Res. 1998;52:149–158. doi: 10.1002/(SICI)1097-4547(19980415)52:2<149::AID-JNR3>3.0.CO;2-A. [DOI] [PubMed] [Google Scholar]
- Taylor WD, Zuchner S, McQuoid DR, Steffens DC, Speer MC, Krishnan KR. Allelic differences in the brain-derived neurotrophic factor Val66Met polymorphism in late-life depression. Am J Geriatr Psychiatry. 2007;15:850–857. doi: 10.1097/JGP.0b013e318050c9d5. [DOI] [PubMed] [Google Scholar]
- Thoenen H. Neurotrophins and activity-dependent plasticity. Prog Brain Res. 2000;128:183–191. doi: 10.1016/S0079-6123(00)28016-3. [DOI] [PubMed] [Google Scholar]
- Tsai SJ. Brain-derived neurotrophic factor: a bridge between major depression and Alzheimer's disease? Med Hypotheses. 2003;61:110–113. doi: 10.1016/s0306-9877(03)00141-5. [DOI] [PubMed] [Google Scholar]
- Vicario-Abejon C, Collin C, McKay RD, Segal M. Neurotrophins induce formation of functional excitatory and inhibitory synapses between cultured hippocampal neurons. J Neurosci. 1998;18:7256–7271. doi: 10.1523/JNEUROSCI.18-18-07256.1998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yoshida K, Higuchi H, Kamata M, Takahashi H, Inoue K, Suzuki T, Itoh K, Ozaki N. The G196A polymorphism of the brain-derived neurotrophic factor gene and the antidepressant effect of milnacipran and fluvoxamine. J Psychopharmacol. 2007;21:650–656. doi: 10.1177/0269881106072192. [DOI] [PubMed] [Google Scholar]